SUMMARY
Objective
The quality of life (QOL) for individuals with schizophrenia is determined by a number of factors, not limited to symptomatology. The current study examined lack of insight as one such factor that may influence subjective QOL or functional capacity. It was hypothesized that insight would significantly interact with symptom severity to influence subjective QOL. Insight was not expected to influence the relation between symptom severity and functional capacity.
Methods
Participants were middle-aged and older outpatients who met diagnostic criteria for schizophrenia or schizoaffective disorder, and subsyndromal depression. Insight, psychopathology, and subjective QOL were assessed via semi-structured interviews and functional capacity was assessed via performance-based measures.
Results
Insight interacts with negative symptom severity to predict subjective QOL. Severity of negative symptoms and insight contribute directly to functional capacity.
Conclusions
Individuals with intact insight may be better able to manage their symptoms, resulting in improved QOL. Treatment implications for improving the QOL of middle age and older adults with schizophrenia are discussed.
Keywords: schizophrenia, insight, quality of life
INTRODUCTION
In a chronic illness like schizophrenia, symptom reduction is only one of several desirable outcomes. Quality of life (QOL) has increasingly been viewed as an important indicator of functioning (Meltzer, 1999). Symptom reduction is assumed to play a role in improving QOL (Packer et al., 1997), although results regarding this relation are inconsistent. Researchers have demonstrated a relation between QOL and positive (Heselgrave et al., 1997; Lysaker et al., 1998; Cechnicki and Valdes, 2003; Hofer et al., 2006) and negative (Browne et al., 1996b; Heselgrave et al., 1997; Packer et al., 1997; Ho et al., 1998; Ritsner et al., 2000; Huppert et al., 2001; Cechnicki and Valdes, 2003; Strejilevich et al., 2005; Bozikas et al., 2006; Hofer et al., 2006) symptoms, such that greater symptom severity is associated with decreased QOL. Others have found no relation to positive (Browne et al., 1996b; Packer et al., 1997; Ho et al., 1998; Smith et al., 1999; Bozikas et al., 2006) or negative (Lysaker et al., 1998; Smith et al., 1999) symptoms.
A more consistent relation is found between QOL and depression (Packer et al., 1997; Dickerson et al., 1998; Smith et al., 1999; Ritsner et al., 2000; Huppert et al., 2001; Cechnicki and Valdes, 2003; Hofer et al., 2006), although exceptions remain (Bozikas et al., 2006). Furthermore, with the exceptions of Browne et al. (1996b) and Bozikas et al. (2006) these associations are moderate at best (Cechnicki and Valdes, 2003; Hofer et al., 2006), suggesting QOL is a complex construct likely influenced by multiple factors.
The absence of a consistently demonstrated relation between QOL and psychopathology may be due to distorted perceptions of QOL among some individuals with schizophrenia. When subjective QOL is assessed via self-report, these ratings are often higher than expected on the basis of objective living conditions (Nillson and Levander, 1997). Such distorted perceptions may be due to poor insight (Atkinson et al., 1997). Two studies have shown subjective and objective measures of functioning are significantly correlated among individuals with high insight, though not related among individuals with low insight (Doyle et al., 1999; Whitty et al., 2004).
We propose insight moderates the relation between symptom severity and subjective QOL. Although an interaction is suggested by researchers who comment on the complexity of QOL (Packer et al., 1997; Ritsner et al., 2000; Cechnicki and Valdes, 2003; Hofer et al., 2006), to our knowledge this has not been explored. Although insight is expected to moderate the relation between psychopathology and subjective QOL, it is not expected to moderate the relation between psychopathology and functional capacity.
METHODS
Participants
Participants were recruited for participation in a larger study from VA Medical Centers, outpatient settings, board and care facilities, independent/assisted living facilities, and the general community in two areas of the country, with the intent of recruiting an ethnically diverse sample. All met DSM-IV (American Psychological Association, 1994) criteria for schizophrenia or schizoaffective disorder. Additional inclusion criteria included: (1) positive endorsement of 2–4 DSM-IV symptoms of major depression; (2) baseline score of 8 or greater on the 17-item Hamilton Depression Rating Scale (Hamilton, 1960); (3) at least 40 years old; (4) adequate decisional capacity; and (5) presence of a caregiver. Participants with a diagnosed dementia disorder or active substance abuse were excluded in order to meet the goals of the larger randomized trial (Zisook et al., 2006), which examined the effectiveness of SSRI augmentation in middle-aged and older individuals with schizophrenia and subsyndromal depression. Participants could have a diagnosis of schizoaffective disorder, either depressed or bipolar type, provided they had no active major depression or mania within the past month.
Measures
The Positive and Negative Syndrome Scale
(PANSS; Kay et al., 1987). The PANSS is a 30-item clinician-rated scale designed to assess positive, negative, and global symptomatology. The current study uses the Positive Scale (seven items), Negative Scale (seven items), and one item to assess insight and judgment on a seven-point scale. This item encompasses several of the key insight dimensions (Lysaker et al., 2003) and significantly correlates with the total score of lengthier measures (Sanz et al., 1998). Higher scores indicate insight deficits or greater symptom severity.
The Calgary Depression Rating Scale
(CDRS; Addington et al., 1992). The CDRS assesses severity of depressive symptoms; higher scores indicate greater symptom severity.
The Heinrichs Quality of Life Scale
(QLS; Heinrichs et al., 1984). The QLS assesses subjective QOL with regard to interpersonal relations, instrumental role functioning, intrapsychic foundations, and common objects and activities. Items are rated on a seven-point scale; higher scores indicate better quality of life.
The UCSD Performance-based Skills Assessment
(UPSA; Patterson et al., 2001a). The UPSA objectively measures functional capacity in: (1) money management; (2) writing a check; (3) communication (e.g. use of telephone to dial emergency); (4) following a recipe; (5) transportation (e.g. following a bus schedule); and (6) planning an outing. Participants are rated on their performance in role-plays, which require approximately 45 min. The interrater reliability of this instrument is high (ICC=0.91). Concurrent validity is evidenced by significant correlations with negative symptom severity and cognitive impairment.
The Social Skills Performance Assessment
(SSPA; Patterson et al., 2001b). The SSPA assess participants' social skills as demonstrated in two 3-min role-plays presenting social problem situations (e.g. a tenant meeting a new neighbor). Estimates of inter-rater and test–retest reliability are high: 0.90 and 0.92, respectively. Concurrent validity is evidenced by significant differences in performance between patients with schizophrenia and normal controls, and significant correlations with negative symptom severity and cognitive impairment.
The Medication Management Ability Assessment
(MMAA; Patterson et al., 2002). The MMAA is a role-play task similar in complexity to medication regimens to which older adults or people with chronic illnesses are likely to follow. Participants are given four pill bottles with varying labeled instructions and a verbal description of the medications. They are tested 1 h later on how to take the pills throughout the day; pill bottles are available for reference during the testing. MMAA role-plays require 10 min to complete and reliability estimates range from 0.94 to 0.98. Compared to normal controls, patients were found to make more errors, and were more likely to be classified as non-adherent. Performance was significantly related to negative symptom severity, cognitive impairment, prescription refill records, performance-based measures of everyday functioning and self-reported quality of life.
Procedure
Written informed consent and data regarding demographics, psychopathology, quality of life, and functional capacity were collected at baseline. All data were collected before participants began the treatment phase of the study.
Data analysis
As preliminary analyses revealed between-site differences on several demographic variables, site was included as a covariate in all analyses. Multiple regression was used to test the interaction between insight and psychopathology. In each model, a QOL or functioning variable was predicted by insight, a measure of psychopathology, and their interaction.
RESULTS
Demographic data by site are presented in Table 1.
Table 1.
Demographic and diagnostic information
| Variable | Site 1 (n=81) |
Site 2 (n=63) |
t or χ2 |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| Current age | 50.21 (5.88) | 54.45 (7.15) | 3.88** |
| Age at onset | 26.10 (9.77) | 24.26 (15.00) | 0.72 |
| Diagnoses (%) | 3.99* | ||
| Schizophrenia | 71.60 | 55.56 | |
| Schizoaffective | 28.40 | 44.44 | |
| Education level (years) | 12.04 (2.24) | 11.87 (2.04) | 0.45 |
| Gender (% male) | 72.84 | 88.89 | 5.66* |
| Marital status (%) | 8.15 | ||
| Married/cohabitating | 12.35 | 15.88 | |
| Divorced/separated | 33.33 | 38.10 | |
| Widowed | 2.47 | 11.11 | |
| Never married | 51.85 | 34.92 | |
| Race (%) | 18.14* | ||
| Caucasian | 59.26 | 49.21 | |
| African-American | 22.22 | 49.21 | |
| Hispanic | 11.11 | 0.00 | |
| Othera | 7.40 | 1.59 |
Includes Native American (n=1), Native Hawaiian/Pacific Islander (n=4), and Other (n=2).
p<0.05.
p<0.001.
Participants at site 1 were younger and more likely to be female and diagnosed with schizophrenia, as opposed to schizoaffective disorder. The sample at site 1 was primarily Caucasian, while the sample at site 2 had equal proportions of Caucasian and African-American participants.
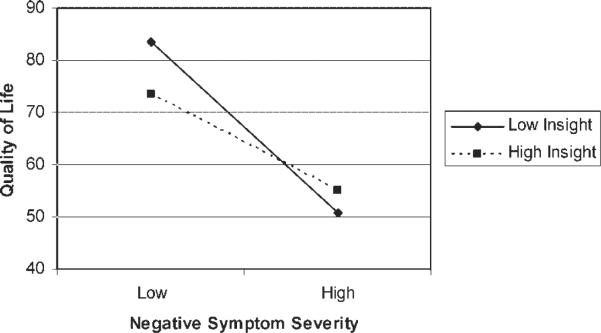
Regarding subjective QOL, a significant interaction between insight and negative symptom severity was observed. As seen in Figure 1, intact insight appears to function as a protective factor against the deleterious effects of negative symptom severity on QOL. Neither positive nor depressive symptom severity significantly contributed to the prediction of QLS scores.
Figure 1.
The effect of insight and negative symptom severity on subjective QOL.
Regarding functional capacity, results indicated no significant interaction between insight and symptom severity. Negative symptom severity exerted a significant main effect on functional capacity, such that greater symptom severity was associated with poorer performance on the UPSA, SSPA, and MMAA. When negative symptom severity was not included in the model, insight emerged as a significant predictor of UPSA and SSPA scores. This is consistent with the significant correlation between insight and negative symptom severity, and the nonsignficant correlation between insight and depression, as seen in Table 2.
Table 2.
Correlation matrix of all independent and dependent variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|
| 1. Pos | — | |||||||
| 2. Neg | 0.16 | — | ||||||
| 3. Dep | 0.19* | 0.11 | — | |||||
| 4. Insight | 0.38*** | 0.21* | −0.03 | — | ||||
| 5. QLS | −0.20* | −0.58*** | −0.19* | −0.17* | — | |||
| 6. UPSA | −0.15 | −0.36*** | 0.05 | −0.21* | 0.23** | — | ||
| 7. SSPA | −0.08 | −0.42*** | 0.04 | −0.17* | 0.42*** | 0.53*** | — | |
| 8. MMAA | 0.06 | 0.22** | −0.05 | 0.10 | −0.11 | −0.34*** | −0.21* | — |
p<0.05.
p<0.01.
p<0.001.
All values are partial correlations controlling for site.
Dep=Calgary Rating Scale for Depression; MMAA=Medication Management Ability Assessment; Neg=PANSS Negative Symptoms; Pos=PANSS Positive Symptoms; QLS=Quality of Life Scale; SSPA=Social Skills Performance Assessment; UPSA=UCSD Performance-Based Skills Assessment.
DISCUSSION
The quality of life (QOL) for individuals with schizophrenia is likely determined by several factors (Awad, 1992; Awad and Hogan, 1994). The current study supports the hypothesis that insight is one such factor. Poor insight was found to adversely influence patients' perception of their QOL. Although decreased subjective QOL was associated with increased negative symptom severity for all patients, the magnitude of this relation is stronger for those individuals with poor insight. Individuals with high insight are more likely to be compliant with medication (David et al., 1992; Amador et al., 1993; Garavan et al., 1998; Cabeza et al., 2000; Yen et al., 2005; Watson et al., 2006) and may be better able to manage their symptoms, thereby resulting in higher psychosocial functioning.
Although insight influenced the relation between subjective QOL and negative symptom severity, it did not moderate the relation between subjective QOL and positive or depressive symptom severity. This is consistent with research that has indicated negative symptoms have a greater impact on QOL (Meltzer et al., 1990; Browne et al., 1996b; Pinikahana et al., 2002). Negative symptoms may be especially influential among individuals with chronic schizophrenia, as in the current sample. Less responsive to treatment (Packer et al., 1997), negative symptoms often predominate the chronic phase of schizophrenia, whereas the positive symptoms may become less florid over time (Ho et al., 1998).
Researchers have expressed concern about the reliability with which individuals with schizophrenia assess their subjective QOL (Atkinson et al., 1997; Doyle et al., 1999; Cechnicki and Valdes, 2003; Whitty et al., 2004), making objective assessments of functioning important outcome variables. The current study used three performance-based measures to objectively assess functioning. Consistent with our hypotheses, the relation between psychopathology and functional capacity was not influenced by level of insight. The pattern of results indicates negative symptom severity is the strongest predictor of functional capacity. When negative symptom severity is not included in the model, insight retains enough partial correlation to predict functioning.
There were several examined relations that did not reach statistical significance, but showed a trend in the expected direction. For example, the interaction between insight and negative symptom severity predicted medication management with p=0.057, suggesting inadequate power may be a limitation of the current study. Future studies with a larger sample size or more powerful measure of insight may reveal more significant relations and interactions.
Additional limitations are as follows. First, the study was cross-sectional and results cannot be used to infer causality. Second, the generalizability of results is limited to samples of middle-aged and older adults with subsyndromal depression. Also, the inclusion of veterans may have created a selection bias during recruitment, resulting in a sample with a higher age of onset of schizophrenia because, in order to qualify for military service, individuals could not have had a serious mental illness earlier in life. Lastly, there were site differences in terms of race, gender, age, and diagnosis. Whereas the differences in race reflect actual differences between the two metropolitan areas where the study was conducted, the reason for site differences in terms of gender, age, and diagnoses are unclear.
Treatment implications
The development of insight may not be a therapeutic goal per se, but rather a vehicle for improving adherence, quality of life, and functioning (McGorry, 1995). Interventions aimed at improving insight have been primarily psychoeducational (McGorry and McConville, 1999) and appear effective in improving overall well-being (Pekkala and Merinder, 2002). Our results, however, suggest that improvements in insight will not necessarily translate to improvements in functional capacity. Interventions aimed directly at improving functional capacity (e.g. Patterson et al., 2006) or comprehensive rehabilitation programs that include a psychoeducational component and training in social skills and activities of daily living (e.g. Browne et al., 1996a) may prove most beneficial in improving the lives of middle-aged and older individuals with chronic schizophrenia.
KEY POINTS
Insight moderates the relation between negative symptom severity and subjective QOL for individuals with schizophrenia.
Negative symptom severity contributes directly to functional capacity.
ACKNOWLEDGEMENTS
This research was supported by RO-1 MH 063931-04 Citalopram Augmentation of Older Patients with Schizophrenia (S. Zisook, PI), the National Institute of Mental Health grants MH66248, MH19934, and the Department of Veterans Affairs. J. Kasckow was supported by R01 MH6398, the VISN 4 MIRECC, and a VISN 4 CPPF award.
Institutions at which research was conducted: Veterans Health Administration National Center for Organization Development; San Diego Veterans Affairs Health Service Center Department of Psychiatry, University of California San Diego.
Footnotes
CONFLICT OF INTEREST None known.
REFERENCES
- Addington D, Addington J, Maticka-Tyndale E, Joyce J. Reliability and validity of a depression rating scale for schizophrenics. Schizophr Res. 1992;6:201–208. doi: 10.1016/0920-9964(92)90003-n. [DOI] [PubMed] [Google Scholar]
- Amador XF, Strauss DH, Yale SA, et al. Assessment of insight in psychosis. Am J Psychiatry. 1993;50(6):873–879. doi: 10.1176/ajp.150.6.873. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th edn American Psychiatric Association; Washington, DC: 1994. [Google Scholar]
- Atkinson M, Zibin S, Chuang H. Characterizing quality of life among patients with chronic mental illness: a critical examination of the self-report methodology. Am J Psychiatry. 1997;154(1):99–105. doi: 10.1176/ajp.154.1.99. [DOI] [PubMed] [Google Scholar]
- Awad AG. Quality of life of schizophrenic patients on medications and implications for new drug trials. Hosp Community Psychiatry. 1992;43:262–265. doi: 10.1176/ps.43.3.262. [DOI] [PubMed] [Google Scholar]
- Awad AG, Hogan TP. Subjective response to neuroleptics and the quality of life: implications for treatment outcome. Acta Psychiatr Scand. 1992;89:27–31. doi: 10.1111/j.1600-0447.1994.tb05828.x. [DOI] [PubMed] [Google Scholar]
- Bozikas VP, Kosmidis MH, Kafantari A, et al. Community dysfunction in schizophrenia: rate-limiting factors. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30:463–470. doi: 10.1016/j.pnpbp.2005.11.017. [DOI] [PubMed] [Google Scholar]
- Browne S, Roe M, Lane A, et al. A preliminary report on the effect of a psychosocial and educative rehabilitation programme on quality of life and symptomatology in schizophrenia. Eur Psychiatry. 1996a;11:386–389. doi: 10.1016/S0924-9338(97)82574-6. [DOI] [PubMed] [Google Scholar]
- Browne S, Roe M, Lane A, et al. Quality of life in schizophrenia: relationship to sociodemographic factors, symptomatology and tardive dyskenisia. Acta Psychiatr Scand. 1996b;94:118–124. doi: 10.1111/j.1600-0447.1996.tb09835.x. [DOI] [PubMed] [Google Scholar]
- Cabeza IG, Amador MS, Lopez CA, de Chavez MG. Subjective response to antipsychotics in schizophrenic patients: clinical implications and related factors. Schizophr Res. 2000;41:349–355. doi: 10.1016/s0920-9964(99)00079-1. [DOI] [PubMed] [Google Scholar]
- Cechnicki A, Valdes M. Relation between schizophrenic patients' quality of life and symptom severity. Arch Psychiatry Psychother. 2003;5(3):55–68. [Google Scholar]
- David AS, Buchanan A, Reed A, Almeida OP. The assessment of insight in psychosis. Br J Psychiatry. 1992;161:599–602. doi: 10.1192/bjp.161.5.599. [DOI] [PubMed] [Google Scholar]
- Dickerson FB, Ringel NB, Parente F. Subjective quality of life in outpatients with schizophrenia: clinical and utilization correlates. Acta Psychiatr Scand. 1998;98:124–127. doi: 10.1111/j.1600-0447.1998.tb10053.x. [DOI] [PubMed] [Google Scholar]
- Doyle M, Flanagan S, Browne S, et al. Subjective and external assessments of quality of life in schizophrenia: relationship to insight. Acta Psychiatr Scand. 1999;99:466–472. doi: 10.1111/j.1600-0447.1999.tb00994.x. [DOI] [PubMed] [Google Scholar]
- Garavan J, Browne S, Gervin M, et al. Compliance with neuroleptic medication in outpatients with schizophrenia; relationship to subjective response to neuroleptics; attitudes to medication and insight. Compr Psychiatry. 1998;39(4):215–219. doi: 10.1016/s0010-440x(98)90063-3. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinrichs DW, Hanlon TE, Carpenter WT. The Quality of Life Scale: an instrument for rating the schizophrenic deficit syndrome. Schizophr Bull. 1984;10(3):388–398. doi: 10.1093/schbul/10.3.388. [DOI] [PubMed] [Google Scholar]
- Heselgrave RJ, Awad AG, Voruganti LNP. The influence of neurocognitive deficits and symptoms on quality of life in schizophrenia. J Psychiatry Neurosci. 1997;22(4):235–243. [PMC free article] [PubMed] [Google Scholar]
- Ho BC, Nopoulos P, Flaum M, et al. Two year outcome in first episode schizophrenia: predictive value of symptoms for quality of life. Am J Psychiatry. 1998;155:1196–1201. doi: 10.1176/ajp.155.9.1196. [DOI] [PubMed] [Google Scholar]
- Hofer A, Rettenbacher MA, Widschwendter CG. Correlates of subjective and functional outcomes in outpatient clinic attendees with schizophrenia and schizoaffective disorder. Eur Arch Psychiatry Clin Neurosci. 2006;256(4):246–255. doi: 10.1007/s00406-005-0633-3. [DOI] [PubMed] [Google Scholar]
- Huppert JD, Weiss KA, Lim R, et al. Quality of life in schizophrenia: contributions of anxiety and depression. Schizophr Res. 2001;51:171–180. doi: 10.1016/s0920-9964(99)00151-6. [DOI] [PubMed] [Google Scholar]
- Kay SR, Fizbein A, Opler LA. Positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13:261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Lysaker PH, Bell MD, Bryson GJ, Kaplan F. Personality as a predictor of the variability of insight in schizophrenia. J Nerv Ment Dis. 1998;187:119–122. doi: 10.1097/00005053-199902000-00011. [DOI] [PubMed] [Google Scholar]
- Lysaker PH, Lancaster RS, Davis LW, Clements CA. Patterns of neurocognitive deficits and unawareness of illness in schizophrenia. J Nerv Ment Dis. 2003;191(1):38–44. doi: 10.1097/00005053-200301000-00007. [DOI] [PubMed] [Google Scholar]
- McGorry PD. Psychoeducation in first episode psychosis: a therapeutic process. Psychiatry. 1995;58:329–344. doi: 10.1080/00332747.1995.11024736. [DOI] [PubMed] [Google Scholar]
- McGorry PD, McConville SB. Insight in psychosis: an elusive target. Compr Psychiatry. 1999;40(2):131–142. doi: 10.1016/s0010-440x(99)90117-7. [DOI] [PubMed] [Google Scholar]
- Meltzer HY, Burnett S, Bastani B, Ramirez LF. Effects of six months of clozapine treatment on the quality of life of chronic schizophrenic patients. Hosp Community Psychiatry. 1990;41(8):892–897. doi: 10.1176/ps.41.8.892. [DOI] [PubMed] [Google Scholar]
- Meltzer HY. Outcome in schizophrenia: beyond symptom reduction. J Clin Psychiatry. 1999;60:3–7. [PubMed] [Google Scholar]
- Nilsson L, Levander S. Quality of life and schizophrenia: no subjective differences among four living conditions. Nordic J Psychiatry. 1997;52:277–283. [Google Scholar]
- Packer S, Husted J, Cohen S, Tomlinson G. Psychopathology and quality of life in schizophrenia. J Psychiatry Neurosci. 1997;22(4):231–234. [PMC free article] [PubMed] [Google Scholar]
- Patterson T, Goldman S, McKibbin C, et al. UCSD performance-based skills assessment: development of a new measure of everyday functioning for severely mentally ill adults. Schizophr Bull. 2001a;27(2):235–245. doi: 10.1093/oxfordjournals.schbul.a006870. [DOI] [PubMed] [Google Scholar]
- Patterson T, Lacro J, McKibbin C, et al. Medication management ability assessment: results from a performance-based measure in older outpatients with schizophrenia. J Clin Psycho-pharmacol. 2002;22(1):11–19. doi: 10.1097/00004714-200202000-00003. [DOI] [PubMed] [Google Scholar]
- Patterson T, Mausbach B, McKibbin G, et al. Functional Adaptation Skills Training (FAST): a randomized trial of a psychosocial intervention for middle-aged and older patients with chronic psychotic disorders. Schizophr Res. 2006;86(1):291–299. doi: 10.1016/j.schres.2006.05.017. [DOI] [PubMed] [Google Scholar]
- Patterson T, Moscona S, McKibbin C, et al. Social skills performance assessment among older patients with schizophrenia. Schizophr Res. 2001b;48(2):351–360. doi: 10.1016/s0920-9964(00)00109-2. [DOI] [PubMed] [Google Scholar]
- Pekkala E, Merinder L. Psychoeducation for schizophrenia. Cochrane Database Syst Rev. 2002;(2):CD002831. doi: 10.1002/14651858.CD002831. [DOI] [PubMed] [Google Scholar]
- Pinikahana J, Happell B, Hope J, Keks N. Quality of life in schizophrenia: a review of the literature from 1995 to 2000. Int J Ment Health Nurs. 2002;11:103–111. doi: 10.1046/j.1440-0979.2002.00233.x. [DOI] [PubMed] [Google Scholar]
- Ritsner M, Modai I, Endicott J, et al. Differences in quality of life domains and psychopathologic and psychosocial factors in psychiatric patients. J Clin Psychiatry. 2000;61:880–889. doi: 10.4088/jcp.v61n1113. [DOI] [PubMed] [Google Scholar]
- Sanz M, Constable G, Lopez-Ibor I, et al. A comparative study of insight scales and their relationship to psychopathological and clinical variables. Psychol Med. 1998;28:437–466. doi: 10.1017/s0033291797006296. [DOI] [PubMed] [Google Scholar]
- Smith TE, Hull JW, Goodman M, et al. The relative influence of symptoms, insight, and neurocognition on social adjustment in schizophrenia and schizoaffective disorder. J Nerv Ment Dis. 1999;187(2):102–108. doi: 10.1097/00005053-199902000-00006. [DOI] [PubMed] [Google Scholar]
- Strejilevich SA, Palatnik A, Avila R, et al. Lack of extra-pyramidal side effects predicts quality of life in outpatients treated with clozapine or typical antipsychotics. Psychiatry Res. 2005;133:277–280. doi: 10.1016/j.psychres.2004.10.009. [DOI] [PubMed] [Google Scholar]
- Watson PWB, Garety PA, Weinman J, et al. Emotional dysfunction in schizophrenia spectrum psychosis: the role of illness perceptions. Psychol Med. 2006;36:761–770. doi: 10.1017/S0033291706007458. [DOI] [PubMed] [Google Scholar]
- Whitty P, Browne S, Clarke M, et al. Systematic comparison of subjective and objective measures of quality of life at 4-year follow-up subsequent to a first episode of psychosis. J Nerv Ment Dis. 2004;12:805–809. doi: 10.1097/01.nmd.0000146733.26005.bd. [DOI] [PubMed] [Google Scholar]
- Yen C, Chen C, Ko C, et al. Relationships between insight and medication adherence in outpatients with schizophrenia and bipolar disorder: prospective study. Psychiatry Clin Neurosci. 2005;59:403–409. doi: 10.1111/j.1440-1819.2005.01392.x. [DOI] [PubMed] [Google Scholar]
- Zisook S, Nyer M, Kasckow J, et al. Depressive symptom patterns in patients with chronic schizophrenia and subsyndromal depression. Schiz Res. 2006;86:226–233. doi: 10.1016/j.schres.2006.03.047. [DOI] [PubMed] [Google Scholar]