Abstract
Study Objective
In this study, we evaluated (1) trauma under-triage by age group; (2) the association between age and serious injury after accounting for other field triage criteria and confounders; and (3) the potential impact of a mandatory age triage criterion for field triage.
Methods
This was a retrospective cohort study of injured children and adults transported by 48 EMS agencies to 105 hospitals in 6 regions of the Western U.S. from 2006 through 2008. We used probabilistic linkage to match EMS records to hospital records, including: trauma registries, state discharge databases and emergency department databases. The primary outcome measure was serious injury, as measured by an Injury Severity Score (ISS) ≥ 16. We assessed under-triage (ISS ≥ 16 and triage-negative or transport to a non-trauma center) by age decile and used multivariable logistic regression models to estimate the association (linear and non-linear) between age and ISS ≥ 16, adjusted for important confounders. We also evaluated the potential impact of age on triage efficiency and trauma center volume.
Results
260,027 injured patients were evaluated and transported by EMS over the 3-year study period. Under-triage increased for patients over 60 years of age, reaching approximately 60% for those older than 90 years. There was a strong non-linear association between age and ISS ≥ 16. For patients not meeting other triage criteria, the probability of serious injury was most notable after 60 years. A mandatory age triage criterion would have decreased under-triage at the expense of over-triage, with one ISS ≥ 16 patient identified for every 60–65 additional patients transported to major trauma centers.
Conclusion
Trauma under-triage increases in patients older than 60 years. While the probability of serious injury increases among triage-negative patients with increasing age, the use of a mandatory age triage criterion appears inefficient for improving field triage.
INTRODUCTION
Background
Field triage plays a critical role in directing seriously injured patients to major trauma centers, which improve survival and functional outcomes.1 The process of field triage is guided by a triage algorithm originally developed by the American College of Surgeons Committee on Trauma (ACSCOT) and revised under the auspices of the Centers for Disease Control and Prevention (CDC).2,3 Starting in 1987, the Field Triage Decision Scheme included age (< 5 or > 55 years)4 as a “special consideration” criterion to identify vulnerable populations potentially benefitting from care in major trauma centers. However, there is little empiric evidence demonstrating the utility of age as a field triage criterion for identifying patients with serious injuries. Complicating this issue are several studies suggesting that under-triage (the proportion of patients with serious injuries not meeting field triage criteria and/or treated in non-trauma centers) is notably higher among elders5–8 and possibly children.9
Importance
Several studies have demonstrated advanced age to be a risk factor for adverse outcomes in trauma.10–17 The criterion specifying age < 5 or > 55 years as a reason to transport to a major trauma center was based on early studies demonstrating increased in-hospital mortality among injured patients in these age ranges.10,18,19 However, evidence supporting the use of specific age cut-points to guide appropriate field triage is sparse, especially for patients not already identified by other triage criteria. Adding importance to this topic is the suggestion that under-triage differs by age5–9 and the possibility that outcomes may be worse in seriously injured patients at the extremes of age due to lack of access to appropriate trauma care. Whether modifying the age criterion in the field triage guidelines would reduce age-specific under-triage practices, improve access to trauma care and reduce morbidity and mortality without adversely impacting major trauma centers remains unknown.
Goals of This Investigation
We analyzed a large, multi-site, population-based, out-of-hospital injury cohort to evaluate under-triage in multiple age groups, including children and elders. We also examined the association between age and serious injury (Injury Severity Score [ISS] ≥ 16) after accounting for other triage criteria to potentially identify an appropriate field triage criterion for age. Finally, we evaluated the implications of different mandatory age triage criteria on trauma centers and trauma systems. While we have previously evaluated the diagnostic value of the field triage criteria,8 this study represents a more detailed assessment of age in the field triage of injured persons.
METHODS
Study Design
This was a multi-site retrospective cohort study. Fourteen Institutional Review Boards at 6 sites approved this protocol and waived the requirement for informed consent.
Setting
The study included injured children and adults who were evaluated and transported by 48 EMS agencies to 105 hospitals (12 Level I, 5 Level II, 3 Level III, 4 Level IV, 1 Level V and 80 community/private/federal hospitals) in 6 regions across the Western U.S. over a 3-year period (January 1, 2006 through December 31, 2008). The 6 regions included: Portland, OR/Vancouver, WA (4 counties); King County, WA; Sacramento, CA (2 counties); San Francisco, CA; Santa Clara, CA (2 counties); and Denver, CO. These regions are part of the Western Emergency Services Translational Research Network (WESTRN), a research consortium of geographic regions, EMS agencies and hospitals linked through Clinical and Translational Science Award centers. Each region consisted of a pre-specified geographic “footprint” corresponding to EMS agency service areas typically including a central metropolitan area (urban) and the surrounding region (suburban with some outlying rural and frontier areas).
Selection of Participants
The study sample included all injured patients (children and adults) for whom the 9-1-1 EMS system was activated and there was transport to an acute care hospital (trauma and non-trauma centers) within the 6 predefined geographic regions. Injured patients were identified by an EMS provider primary impression recorded as “injury” or “trauma.” Specifying the sample in this manner allowed for a population-based, out-of-hospital injury cohort of patients with both minor and serious injuries, as perceived by EMS providers. We excluded interhospital transfers without an initial presentation involving EMS; EMS runs listed as “cancelled,” “no patient found” or “stand by”; non-transported patients; and deaths in the field. In regions where multiple EMS agencies care for the same patient, we used probabilistic linkage20–22 to merge EMS records.
Methods and Measurements
The primary predictor variable of interest was patient age (in years). We also collected: sex, field procedures (intubation attempt, intravenous line placement), initial field vital signs (systolic blood pressure [SBP] in mmHg; Glasgow Coma Scale [GCS] score; respiratory rate in breaths per minute); hospital type; and region. Acute care hospitals were categorized as major trauma centers (Level I and II trauma hospitals) versus lower level trauma centers (Level III – V) and non-trauma hospitals. We grouped lower level trauma centers (Level III – V) with non-trauma hospitals because not all regions categorize Level III-V trauma centers and because Level I/II hospitals have the most rigorous evidence base to support outcome differences when caring for seriously injured patients.
We collected all triage criteria listed in the ACSCOT Field Triage Decision Scheme,3,4 as recorded by EMS providers. Due to variability in local implementation and retention of criteria from older versions of the triage scheme, we also included triage criteria from past versions of the decision scheme (e.g., rollover motor vehicle crash) still in use. Because missing values for individual triage criteria were common in EMS records, triage-positive patients and the use of individual criteria were determined as follows: trauma triage criteria specified in the EMS chart; EMS provider documented “trauma system entry” (or similar charting, depending on local terminology); EMS-recorded trauma identification number (used at some sites as a mechanism for tracking injured patients entered into the trauma system); a matched record from a local trauma registry specifying “scene” origin (i.e., EMS-identified trauma patient); or other surrogate charting markers in EMS records of triage-positive patients specific to each region.
Outcome Measures
The primary outcome measure in this study was an Injury Severity Score (ISS) ≥ 16, a commonly used measure of “serious injury” defining the subset of patients most likely to benefit from trauma center care.1,2,23–27 To obtain ISS, we used probabilistic linkage (LinkSolv v8.2, Strategic Matching, Inc., Morrisonville, NY) to match EMS records to hospital records from trauma registries, emergency department (ED) databases and state discharge databases. This methodology has been used to link EMS data to hospital records in previous studies22,28 and has been validated for matching ambulance records to trauma registry data.28 Because ISS is not included in administrative data sources, we used a mapping function (ICDPIC .ado module http://ideas.repec.org/c/boc/bocode/s457028.html for Stata v11, StataCorp, College Station, TX) and ICD9 diagnoses from all linked hospital records to generate ISS.29 Previous studies have validated software for mapping administrative diagnosis codes to anatomic injury scores30,31 and we have separately validated the use of ICDPIC to generate ISS.32
We used two different definitions of “under-triage”: (1) patients with ISS ≥ 16 and not meeting any field triage criteria, regardless of transport destination and (2) patients with ISS ≥ 16 and initial transport to a non-Level I/II hospital (i.e., Level III-V trauma centers and non-trauma centers), regardless of triage criteria. Each of these definitions represents a different perspective on under-triage: field-based identification of seriously injured patients (using triage criteria) versus appropriate transport destination regardless of field-recognition of serious injury.
Primary Data Analysis
We used descriptive statistics to characterize injured patients and to describe under-triage by age group in 10-year increments. We then used multivariable logistic regression to investigate the association between age and ISS ≥ 16 using models both unadjusted and adjusted for additional covariates to assess whether adding confounders would change the relationship between age and serious injury. Covariates were selected a priori based on known or plausible relationships between age and serious injury, including: prehospital Glasgow Coma Scale score, prehospital systolic blood pressure ≤ 90 mmHg, prehospital intubation attempt, prehospital intravenous line placement, mechanism of injury and site. We used both the full sample and a subgroup restricted to patients who did not meet field triage criteria (“triage-negative patients”) in separate models. As the triage-negative subgroup was intended to represent patients for whom the age triage criterion would be among the final factors considered in determining need for trauma center care (i.e., step 4 in the Field Triage Decision Scheme2,3), we kept patients specified by EMS personnel as meeting only the age triage criterion in the “triage-negative” subgroup. Figure 1 details how we constructed the triage-negative subgroup from the overall sample.
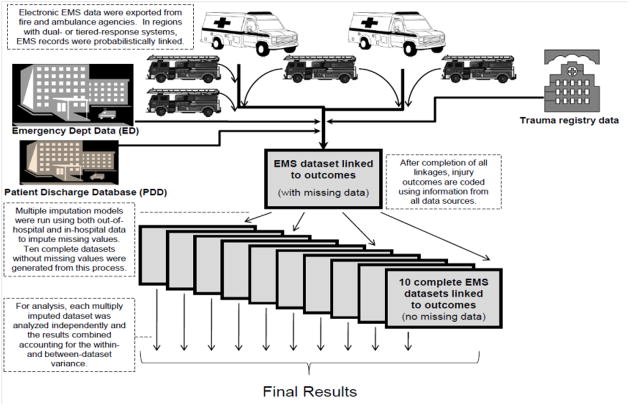
Figure 1.
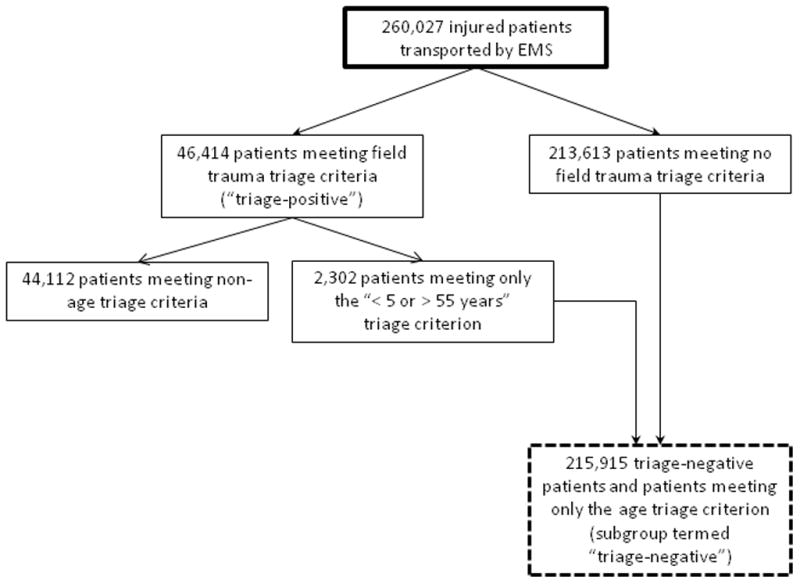
Schematic of the primary sample and “triage-negative” subgroup.
To test non-linear associations between age and ISS ≥ 16, we used fractional polynomials and polytomous categorical terms for age in separate logistic regression models. We initially modeled age as a best-fit fractional polynomial.33–35 Fractional polynomials provide a method for assessing non-linear associations by transforming continuous variables into higher-order terms (44 different first- and second-order variables) that can be compared to a linear term using a standardized algorithm, both unadjusted and adjusted for other covariates.33 We also modeled age as a polytomous categorical variable to provide another analytic method for testing the association between age and serious injury across a variety of age groups. We assessed model fit using the Hosmer-Lemeshow goodness of fit test for all models.
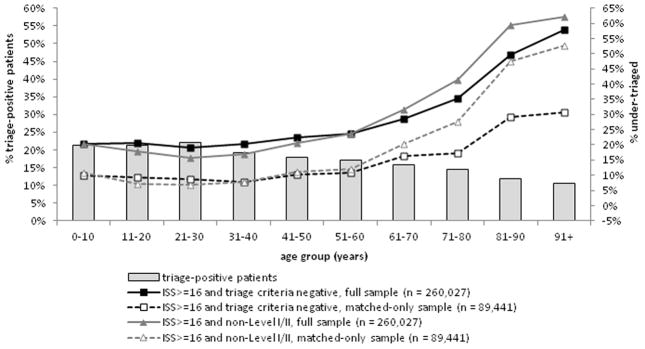
To minimize bias, preserve the population-based sampling design and maximize study power, we used multiple imputation to handle missing values.36 We have previously demonstrated the validity of multiple imputation for imputing missing out-of-hospital values and trauma data under a variety of conditions.37,38 We have also evaluated the use of multiple imputation to impute ISS across a range of conditions and proportions of missing data in this sample.39 We used flexible chains regression models for multiple imputation (IVEware, Survey Methodology Program, Survey Research Center, Institute for Social Research, University of Michigan, MI)40 with generation of 10 multiply imputed datasets, each analyzed independently and combined using Rubin’s rules to appropriately account for variance within- and between-datasets.36 As a sensitivity analysis, we replicated all analyses using the non-imputed sample. A schematic depicting creation of the database for this project, including use of probabilistic linkage and multiple imputation, is illustrated in Figure 2.
Figure 2.
Schematic of constructing the database at each of 6 sites
*This figure represents a slightly modified version of a figure from Newgard CD et al. Evaluating the Use of Existing Data Sources. Probabilistic Linkage and Multiple Imputation to Build Population-Based Injury Databases Across Phases of Trauma Care Acad Emerg Med(In Press).39 Reprinted with permission from Academic Emergency Medicine
Database management and data analysis were performed using SAS (v. 9.2, SAS Institute, Cary, NC). We used SAS-callable IVEware (Survey Methodology Program, Survey Research Center, Institute for Social Research, University of Michigan, MI) for multiple imputation and Stata (v.10, StataCorp, College Station, TX) to assess and compare fractional polynomials.
RESULTS
There were 260,027 injured persons evaluated and transported by EMS during the study period, of whom 8,007 (3.1%) had ISS ≥ 16 and 46,414 (17.9%) met field triage criteria for trauma center transport by EMS personnel. Of triage-positive patients, 6,026 (13.0%) were recorded as meeting the age < 5 or > 55 years field triage criterion. Characteristics of the sample are listed in Table 1, by age group.
Table 1.
Clinical characteristics of injured patients transported by EMS in 6 regions, by age group (full sample n = 260,027, matched-only sample n = 89,441).
| 0–10 years | 11–20 years | 21–30 years | 31–40 years | 41–50 years | 51–60 years | 61–70 years | 71–80 years | 81–90 years | 91+ years | |
|---|---|---|---|---|---|---|---|---|---|---|
| n | 11,303 | 30,543 | 42,204 | 33,283 | 36,443 | 29,995 | 17,993 | 19,537 | 29,012 | 9,715 |
| n for matched- only records* | 3,516 | 9,749 | 12,851 | 10,065 | 11,492 | 10,404 | 6,829 | 8,374 | 12,100 | 3,772 |
| Demographics: | ||||||||||
| Female | 41.8% | 40.5% | 38.5% | 40.2% | 41.1% | 45.8% | 54.8% | 63.8% | 69.7% | 75.4% |
| Out-of-hospital physiology and procedures: | ||||||||||
| SBP (mmHg) – mean | 110.9 | 125.6 | 129.0 | 131.8 | 135.6 | 139.8 | 143.6 | 146.0 | 147.5 | 147.8 |
| SBP < 90 mmHg | 14.6% | 3.0% | 2.8% | 2.4% | 2.1% | 2.4% | 2.4% | 2.1% | 1.6% | 1.6% |
| GCS – mean | 14.5 | 14.6 | 14.5 | 14.5 | 14.5 | 14.5 | 14.6 | 14.6 | 14.5 | 14.5 |
| GCS ≤ 8 | 1.3% | 1.2% | 1.9% | 1.4% | 1.2% | 1.1% | 0.9% | 0.7% | 0.5% | 0.5% |
| Respiratory rate (breaths/minute) – mean | 22.1 | 18.5 | 18.2 | 18.1 | 18.0 | 17.9 | 17.9 | 17.8 | 17.7 | 17.7 |
| Intubation attempt | 0.6% | 0.9% | 1.3% | 1.0% | 0.8% | 0.6% | 0.6% | 0.4% | 0.2% | 0.2% |
| Intravenous line placement | 16.4% | 32.5% | 35.1% | 32.7% | 31.6% | 31.7% | 33.1% | 34.8% | 33.2% | 30.7% |
| Mechanism of Injury: | ||||||||||
| Gunshot wound | 0.4% | 1.8% | 1.7% | 1.0% | 0.6% | 0.5% | 0.3% | 0.2% | 0.2% | 0.2% |
| Stabbing | 1.8% | 3.5% | 4.2% | 3.5% | 2.8% | 1.7% | 0.9% | 0.5% | 0.3% | 0.3% |
| Assault | 4.5% | 13.7% | 17.4% | 15.1% | 13.8% | 7.3% | 3.0% | 1.2% | 0.5% | 0.5% |
| Fall | 36.2% | 15.5% | 14.8% | 21.9% | 30.5% | 43.5% | 58.2% | 73.4% | 82.3% | 85.4% |
| Motor vehicle crash | 27.4% | 37.9% | 41.0% | 36.3% | 30.1% | 26.6% | 20.1% | 11.3% | 5.8% | 3.6% |
| Bicycle | 2.2% | 2.7% | 1.9% | 2.0% | 2.1% | 1.9% | 1.2% | 0.5% | 0.2% | 0.1% |
| Pedestrian vs. auto | 3.7% | 3.1% | 2.4% | 2.3% | 2.4% | 2.4% | 2.0% | 1.2% | 0.5% | 0.4% |
| Other | 23.9% | 21.9% | 16.7% | 18.1% | 17.7% | 16.1% | 14.4% | 11.8% | 10.1% | 9.6% |
| Hospital measures: | ||||||||||
| Initial transport to Level I/II | 39.1% | 44.7% | 51.9% | 48.5% | 46.0% | 40.0% | 31.9% | 23.3% | 17.3% | 14.9% |
| Interhospital transfer | 2.8% | 1.8% | 1.7% | 1.7% | 2.0% | 2.2% | 2.2% | 2.2% | 1.9% | 1.6% |
| Injury Severity Score – mean | 3.6 | 3.8 | 4.0 | 4.0 | 4.0 | 4.1 | 4.1 | 4.1 | 4.2 | 4.3 |
| ISS ≥ 16 | 2.3% | 3.0% | 3.4% | 3.1% | 3.2% | 3.4% | 3.6% | 3.0% | 2.6% | 2.4% |
| n, ISS ≥ 16 | 265 | 917 | 1,412 | 1,019 | 1,155 | 1,030 | 646 | 583 | 751 | 230 |
| n, ISS ≥ 16 for matched-only records* | 180 | 662 | 1,017 | 706 | 826 | 769 | 483 | 410 | 477 | 114 |
Among the matched-only sample, age was missing in 289 (0.3%) records and ISS missing in 180 (0.2%) records.
Use of field triage criteria and under-triage by age group are presented in Figure 3. The proportion of patients meeting field triage criteria steadily declined after 30 years of age. Conversely, under-triage was relatively steady through age 60 years, then increased with increasing age to a high of 58.0 – 62.2% (depending on the definition of under-triage) in patients older than 90 years. There was no indication of increased under-triage in children relative to adults. Findings were consistent between the full (imputed) versus matched-only (non-imputed) samples and when defining under-triage by field triage status versus hospital destination. However, under-triage rates were lower across all age groups and had greater divergence by how under-triage was defined (triage status versus hospital destination) in the non-imputed sample. Among patients greater than 60 years, under-triage was higher when defined by hospital destination, demonstrating that a portion of seriously injured elders are identified by field triage criteria, but still transported to non-Level I/II hospitals.
Figure 3.
Age-based evaluation of under-triage among injured patients transported by EMS *
*We defined “under-triage” two ways: (1) the percentage of patients with serious injury (ISS ≥ 16) that did not meet field trauma triage criteria and (2) the percentage of patients with ISS ≥ 16 that were not transported to a Level I/II trauma center. Results were qualitatively similar when transport destination (Level I/II) included subsequent interhospital transfers. The full sample (n = 260,027) includes all injured patients transported by EMS with use of multiple imputation to impute missing ISS for patients without a matched hospital record The matched-only sample (n = 89,441) includes only patients that matched to a hospital record.
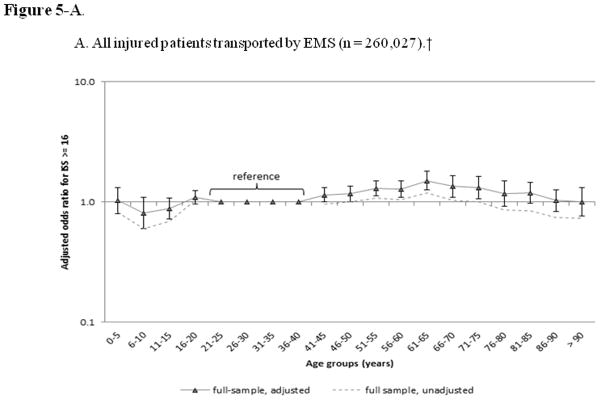
Age was a strong predictor of serious injury in multivariable regression models, with evidence of a non-linear association in the full sample and the triage-negative sample (p < .0001 and p = .007 for tests of fractional polynomial vs. linear age terms in each sample, respectively). Using best-fit fractional polynomials, there were different curves produced for the association between age and serious injury in the two patient populations (Figure 4). Among the full sample (i.e., patients meeting and not meeting field triage criteria), the probability of serious injury was highest among patients in the mid-age range and notably less for patients at the ends of the age spectrum. Among triage-negative patients, the probability of serious injury began to increase at age 30, becoming greater with increasing age. However, there was no single age with a distinct, abrupt increase in the probability of serious injury. The exception to this trend was children under 5 years of age, who had a higher probability of serious injury, though these results were not consistent across all models. Categorical age models yielded similar findings (Figure 5), though without an increased association with serious injury among young children. In the triage-negative sample, patients over 60 years demonstrated increased odds of ISS ≥ 16. Findings from the age models were qualitatively similar when analyzed using the matched-only (non-imputed) sample, with notably smaller sample sizes and wider 95% confidence intervals (data not shown). Goodness of fit differed between models that included all confounders versus more limited (parsimonious) models, with limited models generally yielding better fit. However, all models produced similar findings between age and serious injury.
Figure 4.
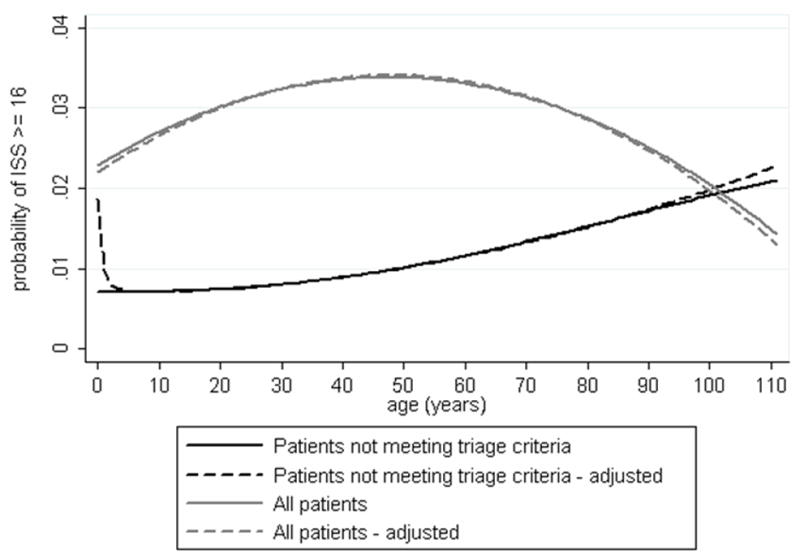
Unadjusted and adjusted probability of Injury Severity Score (ISS) ≥ 16 by age for all injured patients (n = 260,027) and for patients not meeting triage criteria (n = 215,915).
*Multivariable logistic regression models (adjusted estimates) included the following variables age, prehospital Glasgow Coma Scale score, prehospital systolic blood pressure ≤ 90 mmHg, intubation attempt, prehospital intravenous line placement, mechanism of injury and site.
Figure 5.
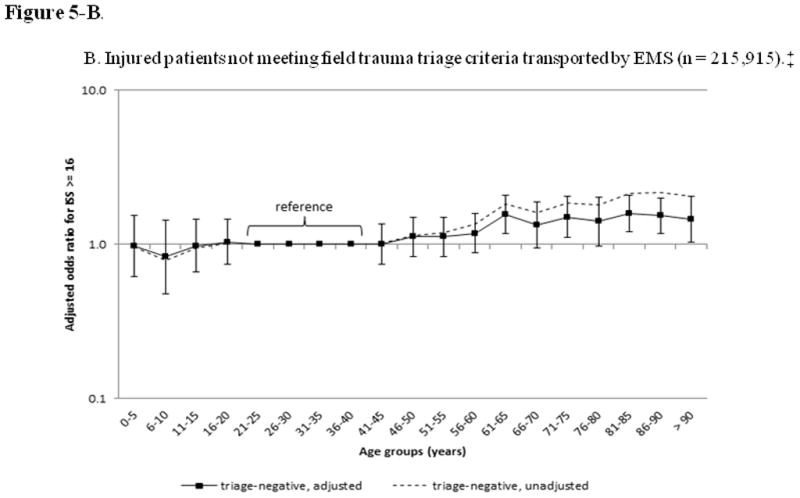
Figure 5-A. Unadjusted and adjusted odds ratios for Injury Severity Score (ISS) ≥ 16 by age group for all injured patients and for patients not meeting field trauma triage criteria.
Figure 5-B. Unadjusted and adjusted odds ratios for Injury Severity Score (ISS) ≥ 16 by age group for all injured patients and for patients not meeting field trauma triage criteria.
*Odds ratio for age categories are adjusted for the following covariates prehospital Glasgow Coma Scale score, prehospital systolic blood pressure ≤ 90 mmHg intubation attempt, prehospital intravenous line placement, mechanism of injury and site.
† For unadjusted odds ratios, the 95% confidence interval reaches statistical significance (does not cross one) for patients 0–15 years, 61–65 years and over 75 years; error bars are omitted for clarity.
‡ For unadjusted odds ratios, the 95% confidence interval reaches statistical significance (does not cross one) for all patients over 55 years; error bars are omitted for clarity.
Table 2 lists sensitivity and specificity estimates for the current field triage guidelines and hypothetical scenarios using different mandatory age triage criteria for both the imputed and non-imputed samples. The resulting changes in trauma center volume, additional patients with ISS ≥ 16 identified and number needed to treat (number of additional patients with minor injuries considered triage-positive with the new age criteria required to identify one previously under-triaged patient) are also included in Table 2. The use of mandatory age criteria for transport to a trauma center reduced the specificity of field triage (increased over-triage) and increased trauma center volume by 511 to 992 patients per year, the majority of whom had non-serious injuries. Under the different scenarios tested, one additional patient with ISS ≥ 16 would be identified for every 60 to 65 additional patients with non-serious injuries triaged to major trauma centers.
Table 2.
Triage accuracy, trauma center volume and number needed to treat using different age-specific field triage criteria.*
| Fully imputed sample (overall n = 260,027; ISS ≥ 16 n = 8,007) | Non-imputed, matched-only sample (n overall = 89,441; ISS ≥ 16 n = 5,711)† | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| % meeting triage criteria | Sens | 95%CI | Spec | 95%CI | Sens | 95%CI | Spec | 95%CI | Annual addit. ISS≥16 patients | Annual increase in transports to Level I/II trauma centers | Average annual volume increase per Level I/II trauma center | NNT‡ | |
| Current practice‡ | 17.9% | 73.6% | (72.4–74.8) | 83.9% | (83.8–84.1) | 87.5% | (86.6–88.3) | 62.8% | (62.4–63.1) | - | - | - | - |
| Current practice, without age criterion | 17.0% | 71.1% | (70.0–72.3) | 84.8% | (84.6–84.9) | 85.1% | (84.1–86.0) | 64.3% | (64.0–64.7) | - | - | - | - |
| Scenarios of mandatory age criterion for trauma triage: | |||||||||||||
| ≤15, ≥55 years | 55.2% | 88.0% | (87.1–88.8) | 45.9% | (45.7–46.1) | 94.6% | (94.0–95.2) | 27.3% | (27.0–27.6) | 384 | 24,793 | 992 | 65 |
| ≤5, ≥55 years | 50.5% | 87.0% | (86.1–87.9) | 50.7% | (50.5–50.9) | 94.3% | (93.7–94.9) | 30.2% | (29.9–30.5) | 357 | 22,119 | 885 | 62 |
| ≥ 55 years | 48.7% | 86.6% | (85.7–87.5) | 52.5% | (52.3–52.7) | 94.0% | (93.4–94.6) | 31.3% | (30.9–31.6) | 347 | 21,064 | 843 | 61 |
| ≥ 60 years | 44.1% | 85.1% | (84.2–86.0) | 57.2% | (57.0–57.4) | 93.3% | (92.6–93.9) | 35.0% | (34.7–35.3) | 307 | 18,428 | 737 | 60 |
| ≥ 65 years | 40.7% | 83.8% | (82.8–84.7) | 60.7% | (60.5–60.9) | 92.5% | (91.8–93.2) | 37.9% | (37.5–38.2) | 272 | 16,341 | 654 | 60 |
| ≥ 70 years | 38.0% | 82.7% | (81.8–83.7) | 63.4% | (63.2–63.6) | 91.9% | (91.2–92.6) | 40.5% | (40.1–40.8) | 244 | 14,621 | 585 | 60 |
| ≥ 75 years | 35.3% | 81.5% | (80.5–82.6) | 66.2% | (66.0–66.4) | 91.2% | (90.5–92.0) | 43.4% | (43.1–43.7) | 212 | 12,778 | 511 | 60 |
Estimates based on actual triage criteria use and transport patterns in this sample.
Triage sensitivity and specificity estimates of current practice for the matched-only sample have been previously published.8
NNT = number needed to treat. This metric represents the ratio of additional patients with minor injury (ISS < 16) considered triage-positive with the new age criteria to identify one previously under-triaged patient with serious injury (ISS ≥ 16).
LIMITATIONS
This study used a retrospective cohort study design and is subject to the standard limitations that accompany such research, including the possibility of unmeasured confounding and bias. Unmeasured factors, such as comorbid conditions, patient preference regarding transport destination and lack of uniformity in the application of trauma triage criteria could have theoretically altered our findings. We attempted to minimize selection bias by using population-based data from multiple sites and EMS agencies, as well as tracking patients regardless of hospital destination. To account for potential misclassification bias in triage status, we used a comprehensive approach and triangulated multiple data sources to maximize identification of triage-positive patients. We have no reason to suspect that such misclassification would have differed based on age.
When calculating estimates of trauma center volume and metrics of triage efficiency, we considered age as a criterion for transport to a Level I/II trauma center. However, the Field Triage Decision Scheme allows for flexibility in transport decision making for patients meeting step 4 criteria (including age), stating “consider transport to a trauma center or a specific resource hospital.”3 If only a portion of patients meeting mandatory age triage criteria were transported to major trauma centers, our estimates would over-estimate the impact of an age criterion on triage sensitivity, major trauma center volume and system efficiency.
While we demonstrate that under-triage increases as age increases, our study does not discern reasons for this finding. It remains unclear whether the triage criteria are less sensitive in older populations (i.e., that revised criteria may improve sensitivity), that the criteria are applied differently by field providers in older patients (e.g., provider bias), that older patients more frequently request transport to non-trauma hospitals (patient preference) or that there are other inherent differences in identifying elders with serious injuries. These are important areas to explore with further research. In addition, we defined under-triage based on an ISS ≥ 16 and triage-negative or transport to non-Level I/II trauma centers, although some may consider using a lower ISS value in older age groups. Such a modification would result in higher proportions of under-triage, with our results providing conservative estimates. Furthermore, these definitions of under-triage may be overly restrictive in rural and frontier regions due to practical limitations with geography, transport distances, weather, resources and other factors affecting rural trauma care.
We used a single outcome (ISS ≥ 16) representing the patient population shown to benefit from trauma center care,1,2, 23–27 rather than assessing other potential outcome metrics (e.g., mortality, resource use, AIS ≥ 3). Because not all patients in the sample had matched hospital records, we relied on multiple imputation to handle missing values, preserve sample size and sampling design. We have demonstrated multiple imputation to remain robust to relatively high proportions of missing values for ISS across a variety of conditions, but not for categorical variables or ordinal data with a narrow range of values (e.g., AIS).38,39 Therefore, using an ISS-based outcome allowed us to effectively integrate multiple imputation to handle missing values. As a sensitivity analysis, we replicated the analyses using the non-imputed sample (complete case analysis) with qualitatively similar results.
DISCUSSION
In this study, we demonstrate that under-triage increases with age for patients older than 60 years and that among patients not meeting other triage criteria, there is no single age (or combination of ages) that could be used as a triage criterion to effectively reduce under-triage without large increases in over-triage and the volume of patients with minor injuries transported to major trauma centers. We also demonstrate that current use of the age-specific triage criterion is selective (i.e., not universally applied to all eligible patients) and likely used for patients meeting the age criteria who are also suspected of having a serious injury.
The use of age as a field trauma triage criterion has been part of the national triage guidelines for more than two decades, but largely without empirical research demonstrating the value of age in identifying patients with serious injuries. The age cut point of > 55 years was supported by data from the Major Trauma Outcome Study, which showed that in-hospital mortality rose among admitted patients starting at 55 years across all levels of injury severity, mechanisms of injury and body regions of injury.10 Similarly, early pediatric trauma studies suggested that children younger than 5 years were at increased mortality risk, particularly from motor vehicle crashes.18,19 While these were pivotal studies in defining age-specific mortality risk, they were not designed to assess age as a field criterion for trauma triage. Many subsequent studies (almost exclusively in adults) demonstrated age to be an independent risk factor for mortality and poor outcome among injured patients10–17 independent of pre-existing illness.13,41,42 However, mortality is a crude marker for triage purposes. As opposed to serious anatomic injury, mortality is influenced by many extraneous post-injury factors and does not necessarily identify patients most likely to benefit from trauma center care. The most recent version of the field triage guidelines draws further attention to “older adults,” noting the increased risk of injury and death after 55 years, a more liberal definition for hypotension (systolic blood pressure < 110 mmHg) in patients over 65 years and the possibility of low impact mechanisms causing severe injury in this population.43 Our findings suggest that for patients not meeting other triage criteria, increasing age is associated with an increased likelihood of serious injury, but that an independent, mandatory age triage criterion (e.g., > 60 years) is likely to be inefficient for improving field triage.
Our results were mixed for children. While the multivariable model using fractional polynomials for age suggested that young children (< 5 years) may be at increased risk of serious injury, this finding was not consistent across all analyses. Children are clearly different than adults regarding injury patterns, propensity for different types of injury, physiologic response to injury and outcomes, and therefore require pediatric-specific care following injury. However, our findings do not clearly delineate a lower end of the age spectrum that could be independently used to identify children with serious injuries in the field, particularly for those not meeting other triage criteria. The specific age criteria (e.g., < 5 years) to use for field triage in children was removed in the 2006 guidelines, in favor of a more general statement that children “should be triaged preferentially to pediatric-capable trauma centers.”2 This statement was retained in the 2011 field triage guidelines using a definition of less than 15 years for “children.”43
For injured adults, there is no universally accepted definition of “elderly” or “geriatric.” Age cut-offs ranging from ≥ 55 to ≥ 80 years have been suggested.17 Per the World Health Organization, most developed countries have accepted the chronological age of 65 years as a definition of “elderly.”44 Others have suggested age over 70 years as a criterion for hospital-based trauma team activation11 and development of geriatric-specific trauma triage criteria.12 Our findings demonstrate several key age-specific findings among adults. First, we did not identify a single, independent age cut-point to reliably identify seriously injured elders without substantially increasing over-triage rates to major trauma centers. Second, patients over 60 years were commonly under-triaged and had the highest probability of serious injury (for patients not meeting other triage criteria). Third, we demonstrate that the association between age and serious injury is not linear. Finally, our findings show that among the full, heterogeneous sample of injured patients (triage-positive and triage-negative), those at the ends of the age spectrum were less likely to have serious injury, illustrating the importance of accounting for other triage criteria when addressing the utility of age in field triage.
There are multiple studies suggesting increased rates of under-triage and poor access to trauma care among elders5–8 and potentially among children.9 Our results were similar among patients older than 60 years, but not among children. Under-triage rates in this sample were notably higher than those recommended by ACSCOT3 though similar to previous research evaluating access to trauma center care among seriously injured elders.6 Reasons for under-triage among injured elders remain poorly understood. Several studies have shown that seriously injured elders often fail to meet standard physiologic criteria.11,45–48 However, even among samples including children and younger adults, the physiologic criteria only identify a minority of seriously-injured patients,8 suggesting that changes to the physiologic criteria in isolation are unlikely to resolve the under-triage issue. Elders may incur serious injuries from low velocity mechanisms (e.g., ground level falls), greater anatomic and physiologic fragility (e.g., osteoporosis, cortical atrophy, greater propensity for hemorrhage) and other factors that increase the probability of occult injury, which require a high level of suspicion to recognize.
In this study, we also present data on the potential implications of using mandatory age-based triage criteria to reduce under-triage. While some trauma systems have considered (or already implemented) mandatory age triage criteria, the implications regarding over-triage and impact on trauma centers have remained poorly understood. We demonstrate that mandatory age criteria for directing injured patients to trauma centers would have major implications, including marked increases in over-triage and a considerable number of patients with minor to moderate injuries being re-directed to major trauma centers. These findings suggest that while such a strategy would reduce under-triage, the volume shifts are likely untenable for most trauma centers and may attenuate the potential benefits from capturing a few more seriously injured individuals. In addition, there may be unintended consequences for non-trauma hospitals, including financial losses, disruption in continuity of care and decreased patient volume. An age criterion may also infringe on patient autonomy when choosing a destination hospital for their care, particularly when the suspicion for serious injury is low. Further complicating this issue is previous research that has failed to demonstrate improved survival, better functional outcomes or cost-effectiveness from treating seriously injured elders in major trauma centers.1,49 Our findings indicate there are continued opportunities to develop more inclusive trauma systems with improved secondary triage processes and to explore additional ideas for improving the triage, care and outcomes among injured elders.
CONCLUSIONS
In this population-based, multi-site investigation, we demonstrate that under-triage of injured patients increases incrementally in patients over 60 years. Among those not meeting field triage criteria, the probability of serious injury increases with increasing age, becoming more notable after 60 years, but without an abrupt increase at any specific age. The use of mandatory age-based triage criteria would be expected to reduce under-triage at the expense of increases in over-triage and volume of minimally injured patients transported to major trauma centers.
Acknowledgments
FUNDING
This project was supported by the Robert Wood Johnson Foundation Physician Faculty Scholars Program; the Oregon Clinical and Translational Research Institute (grant #UL1 RR024140); UC Davis Clinical and Translational Science Center (grant #UL1 RR024146); Stanford Center for Clinical and Translational Education and Research (grant #1UL1 RR025744); University of Utah Center for Clinical and Translational Science (grant #UL1-RR025764 and C06-RR11234); and UCSF Clinical and Translational Science Institute (grant #UL1 RR024131). All Clinical and Translational Science Awards are from the National Center for Research Resources, a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research.
We want to acknowledge and thank all the participating EMS agencies, EMS medical directors, trauma registrars, and state offices that supported and helped provide data for this project.
Footnotes
Author contributions:
YN and CDN conceived of and designed the study. CDN, EMB, RYH, NCM, JFH, KS and ML assisted with acquisition of data. CDN performed all database management and statistical analyses. All authors helped interpret the data and results. CDN and MD provided oversight, guidance and mentorship during the project. YN drafted the manuscript and all authors participated in critical revision of the manuscript. CDN and YN take responsibility for the data, results and manuscript as a whole.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. NEJM. 2006;354:366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Guidelines for Field Triage of Injured Patients: Recommendations of the National Expert Panel on Field Triage. MMWR. 2009;58:1–35. [PubMed] [Google Scholar]
- 3.Resources for the Optimal Care of the Injured Patient. Chicago, IL: American College of Surgeons; 2006. [Google Scholar]
- 4.Mackersie RC. History of trauma field triage development and the American College of Surgeons criteria. Prehospital Emergency Care. 2006;10:287–294. doi: 10.1080/10903120600721636. [DOI] [PubMed] [Google Scholar]
- 5.Hsia RY, Wang E, Torres H, et al. Disparities in trauma center access despite increasing utilization: data from California, 1999 to 2006. J Trauma. 2010;68:217–24. doi: 10.1097/TA.0b013e3181a0e66d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vassar MJ, Holcroft JJ, Knudson MM, Kizer KW. Fractures in access to and assessment of trauma systems. J Am Coll Surg. 2003;197:717–725. doi: 10.1016/S1072-7515(03)00749-X. [DOI] [PubMed] [Google Scholar]
- 7.Scheetz LJ. Effectiveness of prehospital trauma triage guidelines for the identification of major trauma in elderly motor vehicle crash victims. J Emerg Nurs. 2003;29:109–115. doi: 10.1067/men.2003.59. [DOI] [PubMed] [Google Scholar]
- 8.Newgard CD, Zive D, Holmes JF, et al. A Multi-Site Assessment of the ACSCOT Field Triage Decision Scheme For Identifying Seriously Injured Children and Adults. J Am Coll Surg. 2011;213:709–21. doi: 10.1016/j.jamcollsurg.2011.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang NE, Saynina O, Kuntz-Duriseti K, et al. Variability in pediatric utilization of trauma facilities in California: 1999 to 2005. Ann Emerg Med. 2008;52:607–615. doi: 10.1016/j.annemergmed.2008.05.011. [DOI] [PubMed] [Google Scholar]
- 10.Finelli F, Jonsson J, Champion H, et al. A case control study for major trauma in geriatric patients. J Trauma. 1989;29:541–548. doi: 10.1097/00005373-198905000-00001. [DOI] [PubMed] [Google Scholar]
- 11.Demetriades D, Sava J, Alo K, et al. Old age as a criterion for trauma team activation. J Trauma. 2001;51:754–7. doi: 10.1097/00005373-200110000-00022. [DOI] [PubMed] [Google Scholar]
- 12.Caterino J, Valasek T, Werman H. Identification of an age cutoff for increased mortality in patients with elderly trauma. AM J of Emerg Med. 2010;28:151–158. doi: 10.1016/j.ajem.2008.10.027. [DOI] [PubMed] [Google Scholar]
- 13.Morris JA, Jr, MacKenzie EJ, Damiano AM, et al. Mortality in trauma patients: the interaction between host factors and severity. J Trauma. 1990;30:1476–82. [PubMed] [Google Scholar]
- 14.Johnson CL, Margulies DR, Kearney TJ, Hiatt JR, Shabot MM. Trauma in the elderly: an analysis of outcomes based on age. Am Surg. 1994 Nov;60(11):899–902. [PubMed] [Google Scholar]
- 15.Van der Sluis CK, Klasen HJ, Eisma WH, ten Duis HJ. Major trauma in young and old: what is the difference? J Trauma. 1996 Jan;40(1):78–82. doi: 10.1097/00005373-199601000-00015. [DOI] [PubMed] [Google Scholar]
- 16.Perdue PW, Watts DD, Kaufmann CR, Trask AL. Differences in mortality between elderly and younger adult trauma patients: geriatric status increases risk of delayed death. J Trauma. 1998 Oct;45(4):805–10. doi: 10.1097/00005373-199810000-00034. [DOI] [PubMed] [Google Scholar]
- 17.Jacobs DG, Plaisier BR, Barie PS, et al. Practice management guidelines for geriatric trauma. Allentown, PA: Eastern Association for the Surgery of Trauma; 2001. Available at http://www.east.org/tpg/geriatric.pdf. [Google Scholar]
- 18.Baker SP. Motor vehicle occupant deaths in young children. Pediatrics. 1979 Dec;64(6):860–1. [PubMed] [Google Scholar]
- 19.Monthly Vital Statistics Report: Advance Report, Final Mortality Statistics 1979. 1, supplement Vol. 28. Hyattsville, Md: US National Center for Health Statistics; 1979. [Google Scholar]
- 20.Clark DE. Practical introduction to record linkage for injury research. Injury Prevention. 2004;10:186–191. doi: 10.1136/ip.2003.004580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jaro MA. Probabilistic linkage of large public health data files. Statistics in Medicine. 1995;14:491–498. doi: 10.1002/sim.4780140510. [DOI] [PubMed] [Google Scholar]
- 22.Dean JM, Vernon DD, Cook L, et al. Probabilistic linkage of computerized ambulance and inpatient hospital discharge records: a potential tool for evaluation of emergency medical services. Ann Emerg Med. 2001;37:616–626. doi: 10.1067/mem.2001.115214. [DOI] [PubMed] [Google Scholar]
- 23.Mullins RJ, Veum-Stone J, Helfand M, et al. Outcome of hospitalized injured patients after institution of a trauma system in an urban area. JAMA. 1994;271:1919–1924. doi: 10.1001/jama.1994.03510480043032. [DOI] [PubMed] [Google Scholar]
- 24.Mullins RJ, Veum-Stone J, Hedges JR, et al. Influence of a statewide trauma system on location of hospitalization and outcome of injured patients. J Trauma. 1996;40:536–545. doi: 10.1097/00005373-199604000-00004. [DOI] [PubMed] [Google Scholar]
- 25.Mullins RJ, Mann NC. Population-based research assessing the effectiveness of trauma systems. J Trauma. 1999;47:S59–66. doi: 10.1097/00005373-199909001-00013. [DOI] [PubMed] [Google Scholar]
- 26.Jurkovich GJ, Mock C. Systematic review of trauma system effectiveness based on registry comparisons. J Trauma. 1999;47:S46–55. doi: 10.1097/00005373-199909001-00011. [DOI] [PubMed] [Google Scholar]
- 27.Hulka F, Mullins RJ, Mann NC, et al. Influence of a statewide trauma system on pediatric hospitalization and outcome. J Trauma. 1997;42:514–519. doi: 10.1097/00005373-199703000-00020. [DOI] [PubMed] [Google Scholar]
- 28.Newgard CD. Validation of probabilistic linkage to match de-identified ambulance records to a state trauma registry. Acad Emerg Med. 2006;13:69–75. doi: 10.1197/j.aem.2005.07.029. [DOI] [PubMed] [Google Scholar]
- 29.Clark DE, Osler TM, Hahn DR. ICDPIC: Stata Module to Provide Methods for Translating International Classification of Diseases (Ninth Revision) Diagnosis Codes into Standard Injury Categories and/or Scores. Boston: Boston College, Department of Economics; 2009. [Google Scholar]
- 30.MacKenzie EJ, Steinwachs DM, Shankar BS, Turney SZ. An ICD-9CM to AIS conversion table: development and application. Proc AAAM. 1986;30:135–151. [Google Scholar]
- 31.MacKenzie EJ, Steinwachs DM, Shankar B. Classifying trauma severity based on hospital discharge diagnoses. Validation of an ICD-9CM to AIS-85 conversion table. Med Care. 1989;27:412–422. doi: 10.1097/00005650-198904000-00008. [DOI] [PubMed] [Google Scholar]
- 32.Fleischman R, Mann NC, Wang NE, et al. Validating The Use Of ICD9 Codes To Generate Injury Severity Score: The ICDPIC Mapping Procedure. [Abstract] Acad Emerg Med. 2012 (In Press) [Google Scholar]
- 33.Royston P, Altman DG. Regression using fractional polynomials of continuous covariates: parsimonious parametric modeling. Appl Statist. 1994;43:429–467. [Google Scholar]
- 34.Royston P, Sauerbrei W. Stability of multivariable fractional polynomial models with selection of variables and transformations: a bootstrap investigation. Statist Med. 2003;22:639–659. doi: 10.1002/sim.1310. [DOI] [PubMed] [Google Scholar]
- 35.Sauerbrei W, Meier-Hirmer C, Benner A, Royston P. Multivariable regression model building by using fractional polynomials: description of SAS, STATA and R programs. Computational Statistics & Data Analysis. 2006;50:3464–3485. [Google Scholar]
- 36.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: John Wiley & Sons, Inc; 1987. [Google Scholar]
- 37.Newgard CD. The validity of using multiple imputation for missing prehospital data in a state trauma registry. Acad Emerg Med. 2006;13:314–324. doi: 10.1197/j.aem.2005.09.011. [DOI] [PubMed] [Google Scholar]
- 38.Newgard CD, Haukoos J. Missing data in clinical research – part 2: Multiple imputation. Acad Emerg Med. 2007;14:669–678. doi: 10.1197/j.aem.2006.11.038. [DOI] [PubMed] [Google Scholar]
- 39.Newgard CD, Malveau S, Staudenmayer K, Wang NE, Hsia RY, Mann NC, Holmes JF, Kuppermann N, Haukoos JS, Bulger EM, Dai M, Cook LJ. Evaluating the Use of Existing Data Sources, Probabilistic Linkage and Multiple Imputation to Build Population-Based Injury Databases Across Phases of Trauma Care. Acad Emerg Med. doi: 10.1111/j.1553-2712.2012.01324.x. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Raghunathan T, Lepkowski, Van Hoewyk J, Solenberger P. A multivariate technique for multiply imputing missing values using a sequence of regression models. Survey Methodology. 2001;27:85–95. [Google Scholar]
- 41.Hollia S, Lecky F, Yates DW, et al. The effect of pre-existing medical conditions and age on mortality after injury. J Trauma. 2006;61:1255–60. doi: 10.1097/01.ta.0000243889.07090.da. [DOI] [PubMed] [Google Scholar]
- 42.Perdue PW, Watts DD, Kaufmann CR, et al. Differences in mortality between elderly and younger adult trauma patients: geriatric status increase risk of delayed death. J Trauma. 1998;45:805–10. doi: 10.1097/00005373-199810000-00034. [DOI] [PubMed] [Google Scholar]
- 43.Sasser SM, Hunt RC, Faul M, et al. Guidelines for Field Triage of Injured Patients: Recommendations of the National Expert Panel on Field Triage, 2011. MMWR. 2012;61:1–20. [PubMed] [Google Scholar]
- 44.World Health Organization. Available at http://www.who.int/healthinfo/survey/ageingdefnolder/en/index.html.
- 45.Phillips S, Rond PC, III, Kelly SM, et al. The failure of triage criteria to identify geriatric patients with trauma: results from the Florida trauma triage study. J Trauma. 1996;40:278–283. doi: 10.1097/00005373-199602000-00018. [DOI] [PubMed] [Google Scholar]
- 46.Scalea TM, Simon HM, Duncan AO, et al. Geriatric blunt multiple trauma: improved survival with early invasive monitoring. J Trauma. 1990;30:129–36. [PubMed] [Google Scholar]
- 47.Demetriades D, Karaiskakis M, Velmahos G, et al. Effect on outcome of early intensive management of geriatric trauma patients. Br J Surg. 2002;89:1319–22. doi: 10.1046/j.1365-2168.2002.02210.x. [DOI] [PubMed] [Google Scholar]
- 48.Lehamann Ryan, Beekley Alec, Casey Linda, et al. The impact of advanced age on trauma triage decisions and outcomes: A statewide analysis. Am J of Surgery. 2009;197:571–575. doi: 10.1016/j.amjsurg.2008.12.037. [DOI] [PubMed] [Google Scholar]
- 49.MacKenzie EJ, Weir S, Rivara FP, et al. The value of trauma center care. J Trauma. 2010;69:1–10. doi: 10.1097/TA.0b013e3181e03a21. [DOI] [PubMed] [Google Scholar]