Abstract
Background
In the present study, 20 patients with mandibular fracture were included to evaluate the versatility of titanium 3D plate in comparison with conventional titanium miniplate fixation.
Methods
The patients were alternatively allocated to either the 3D plate group or Miniplate group. The patients were evaluated for the clinical assessment of mobility after fixation, pre and post-surgical occlusal relationship, adequacy of reduction on post operative radiograph and any post surgical complications.
Results
All 25 fractures in 20 patients were found to be adequately fixed when checked intra-operatively. No post-operative IMF was required in either of the groups. The mean radiographic score at post operative time interval in Miniplate group was found to be 2.80 ± 0.42 and in 3D Plate was found to be 2.90 ± 0.32. The mean radiographic score at 3 months time interval in Miniplate group was found to be 2.70 ± 0.48 and in 3D Plate was found to be 2.70 ± 0.48. Radiolucency at 3 months period was found in 1 patient (10%) in the miniplate group and it was not found in any patients in the 3D plate group. None of the patients in both the groups had complications of non-union or mal-union. In miniplate group, 2 patients (20%) had infections and in 3D plate group 1 patient (10%) had infection. 3 patients in miniplate group had occlusal discrepancies (30%) and 1 patient in 3D plate group had occlusal discrepancies (10%). Overall, complications were found in 6 patients (60%) in miniplate group and 2 patients (20%) in 3D plate group. The data when compared was statistically significant (P < 0.05).
Conclusion
The 3D plating system was found to be advantageous over conventional miniplates. It uses lesser foreign material, reduces the operation time and overall cost of the treatment. Thus 3D plate can be used as an alternative to conventional miniplates. The system is reliable and effective treatment modality for mandibular fractures.
Keywords: Mandible fracture, Miniplates, 3D plates
Introduction
Techniques for open reduction of mandibular fractures have changed and diversified enormously in recent decades and achieved new horizons. Various plating systems using either an intra-oral approach or an extra-oral approach have been described for stable internal fixation and improved management of mandibular fractures [1].
Recently miniplates and modifications in miniplates based on champy’s principle like titanium 3D plating system have been developed to meet the requirements of semi rigid fixation with lesser complications.
The basic concept of 3D fixation is that a geometrically closed quadrangular plate secured with bone screws creates stability in three dimensions. The principle of the 3D fixation is further based on the idea that the plate is not positioned along the trajectories but over the weak structure lines. The fixation points of the plate remain in the vicinity of the fracture or osteotomy line [2] (Fig. 1). The newly introduced 3D plating system provides definite advantages over conventional miniplates. The 3D plating system uses fewer plates and screws as compared to conventional miniplates to stabilize the bone fragments [1, 2].
Fig. 1.
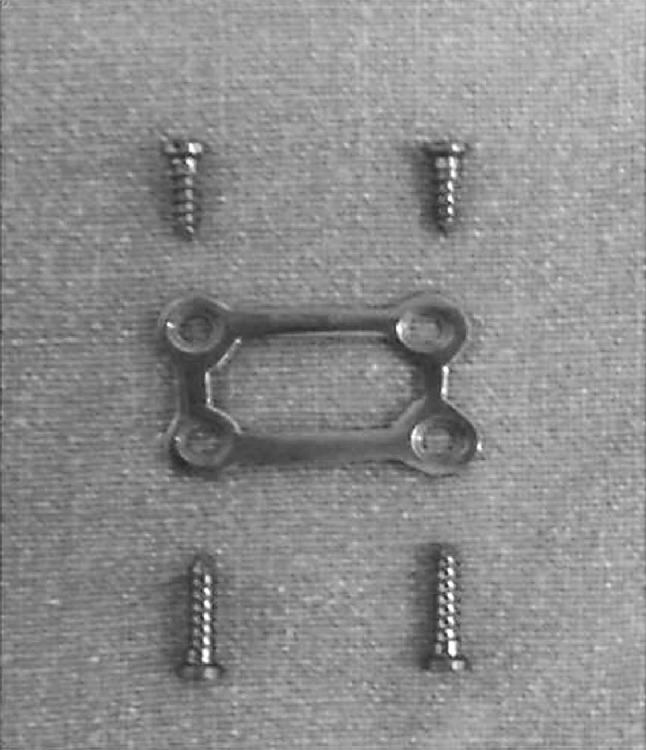
3D plate
The 3D plating system has a compact design and is easy to use. The 1.0 mm thick 3D plate is as stable as much thicker 2–0 mm miniplate (Fig. 2). This offers better bending stability and more resistance to out of plane movement or torque [1]. Adjustments is easy because of the thin connecting arms of the plate even in case of 1 mm standard plate. The screws adapt each part of the plate separately without any tension to the bone. There is no need for the exact adaption of the plate as is necessary with thicker plates [2] (Fig. 3).
Fig. 2.
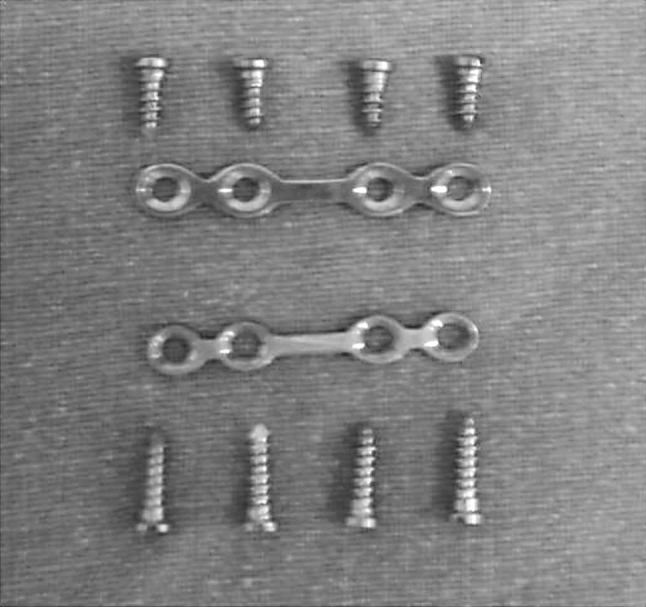
Miniplate
Fig. 3.

3D plate and miniplate
Various researches show that the 3D plating system offers more favorable biomechanical behavior than the conventional miniplates in terms of stability and strain resistance in different regions of mandible [1, 3, 4]. The 1 mm standard 3D plate can withstand traction forces with value of 690 N which are almost the value of maximum load capacity of the mandible [2].
So in the present prospective study, an attempt has been made to assess the versatility of titanium 3D plate in mandibular fractures in comparison with conventional titanium miniplate fixation by
Evaluating the incidence of complications.
Evaluating stability of 3D plating system over conventional miniplates.
Studying advantages and disadvantages over conventional miniplates.
Materials and Methods
This is a randomized prospective study conducted on patients visiting Department of Oral and Maxillofacial Surgery, Government Dental College and Research Institute, Bangalore with diagnosis of mandibular fractures. All the patients were treated on in-patient basis.
All patients with insignificant medical history were involved in the study. The selected cases were treated by open reduction and internal fixation. The study was designed to evaluate the versatility of titanium 3D plate in comparison with conventional titanium miniplate fixation. The sample size was 20 with 10 patients in each group. One group received 3D plate and other received miniplates. The patients with non-comminuted, non-infected mandibular fractures in symphysis, parasymphysis, body, and angle region indicated for open method were included.
Fractures associated with condyle, coronoid process, and ramus were excluded from the study. The study was approved by institutional ethical committee, and informed consent was obtained from the patients before their inclusion in the study. After the inclusion and exclusion criteria were met before the treatment patients were alternatively allocated to receive either of two types of plating system for treatment and randomization. All patients were treated and observed by the same surgeon.
Titanium 4-holed miniplates with gap having a thickness of 2.0 mm were used. The screws used were of 6.0 and 8.0 mm length. The plates were fixed in accordance with champy’s principle (Fig. 4).
Fig. 4.

Patient with miniplate
A 4-holed rectangular titanium 3D plate was used in this study. A single plate was used in case of symphysis, parasymphysis, and body as well as angle region; fixed with 6.0 and 8.0 mm screws. In the parasymphysis and body region, 3D plate was fixed above the level of mandibular canal. The lower border screws were fixed first followed by upper border screws. The 3D plate was placed in such a way so that horizontal cross bars are perpendicular to the fracture line and vertical cross bars are parallel to fracture line (Fig. 5).
Fig. 5.
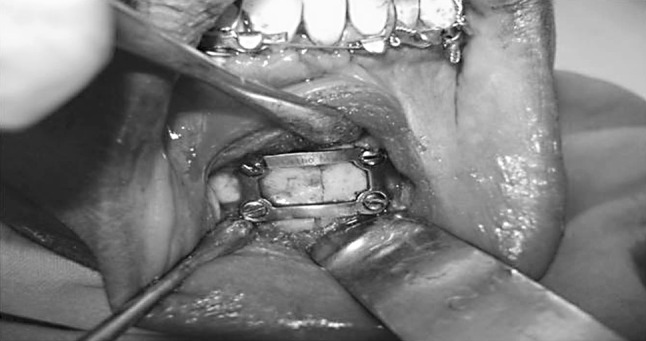
Patient with 3D plate
The patients were followed up for a period of 6 weeks initially for every week and later at a period of 3 months. All the parameters used were assessed at various recall visits and recorded. Postoperative OPG was taken in all the cases as early as possible after surgery and later at a period of 3 months. Additional OPG was taken if required.
Assessment of Patients
The patients were evaluated for the location, type and number of fractures; presence of tooth in fracture line, time elapsed between the presentation of the patient after trauma, operating time, clinical assessment of mobility after fixation, pre and post-surgical occlusal relationship, adequacy of reduction on post operative radiograph and any post surgical complications.
Evaluation Criteria
Intra-Operative
1. Adequacy of Fracture Fixation
Adequacy of fracture fixation was checked immediately after fixation by clinical manipulations in three dimensions. In case of adequate fixation, no further treatment was done while in fractures found to be inadequately fixed further intervention was done.
Post-Operative
1. Radiological Assessment
Post-operative Radiographs i.e. OPG Post-operative radiographs were taken as early as possible after the surgical procedure. These were assessed using a score from 1 to 3.
Score 3: Radiological evidence of precise anatomic reduction in the fracture site.
Score 2: Reduced fractures that were slightly displaced but had a satisfactory occlusion.
Score 1: Poorly reduced fractures that required a second operation to correct poor alignment and unacceptable occlusion.
The radiographic score of all the patients in both the plating systems was added and total score of each system was obtained. The higher value indicated better plating system.
Radiograph after 3 months The radiograph at a period of 3 months was taken because normal fracture healing process takes approximately 3 months. The OPGs were scored as done previously. OPGs were also assessed for radiographic changes around the plating system.
2. Complications
Assessed up to 3 months.
Non-union: Persistent mobility between fracture segments on clinical manipulations.
Mal-union: Based on clinical and radiographic assessment.
Infections: Case to be considered infected having discharge with positive culture test.
Occlusal discrepancies: Based on clinical examination and information obtained from the patient.
All the complications were managed accordingly. The above described findings were recorded in each patient and the final data thus obtained compared to other group.
The statistical formulas used in the study are t test and z test.
Results
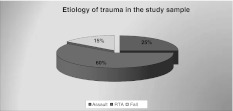
The mean age of the patients participating in this study was 29 ± 5.8 years (Graph 1; Table 1). There were 20 (100%) male patients of Asian origin, with road traffic accident (RTA) being the most common cause of etiology 12 (60%), followed by assault 5 (25%), and work related or self fall 3 (15%) (Graph 2; Table 2).
Graph 1.
Age distribution of study population
Table 1.
Age distribution of the study population
| Age | N | % |
|---|---|---|
| 10–20 Years | 1 | 5.00 |
| 21–30 Years | 13 | 65.00 |
| 31–40 Years | 6 | 30.00 |
| 41–50 Years | 0 | 0.00 |
| Total | 20 | 100 |
Graph 2.
Etiology of trauma of study population
Table 2.
Etiology of trauma
| Cause of injury | N | % |
|---|---|---|
| RTA | 12 | 60.00 |
| Work related/fall | 3 | 15.00 |
| Assault | 5 | 25.00 |
| Sports injury | 0 | 0.00 |
| Miscellaneous | 0 | 0.00 |
| Total | 20 | 100 |
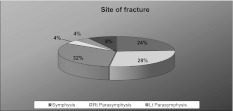
Fracture distribution consisted of 15 parasymphysis (60%), 6 symphysis (24%), 1 body (4%) and 3 angle (12%) fractures with a total of 25 fracture sites in the 20 cases selected (Graph 3; Table 3).
Graph 3.
Site of fratcture
Table 3.
Location of fracture
| Site of fracture | N | % |
|---|---|---|
| Symphysis | 6 | 24 |
| Rt. parasymphysis | 7 | 28 |
| Lt. parasymphysis | 8 | 32 |
| Rt. body | 1 | 4 |
| Lt. body | – | – |
| Rt. angle | 1 | 4 |
| Lt. angle | 2 | 8 |
| Total | 25 | 100 |
The fractures were treated ranging from 1 to 5 days with a mean of 3.1 ± 1.21 days from the time of injury.
Adequacy of fracture fixation was checked immediately after fixation by clinical manipulations in three dimensions. Postoperative OPG was taken in all the cases as early as possible after surgery and later at a period of 3 months. The patients were followed up for a period of 6 weeks initially for every week and later at a period of 3 months.
All fractures were found to be adequately fixed when checked intra-operatively after fixation. No post-operative IMF was required in either of the groups.
The mean radiographic score at post operative time interval in miniplate group was found to be 2.80 ± 0.42 with a median score of 3.00. The mean radiographic score in 3D plate was found to be 2.90 ± 0.32 with a median score of 3.00 (Graph 4; Table 4). The median difference between the two groups was not statistically significant (P > 0.05).
Table 4.
Comparison of radiographic scores at post op time interval in the groups
| Group | N | Mean | Std. dev. | Median | Z | P value |
|---|---|---|---|---|---|---|
| Miniplate | 10 | 2.80 | 0.42 | 3.00 | −0.610 | 0.542 |
| 3D plate | 10 | 2.90 | 0.32 | 3.00 |
The mean radiographic score at 3 months time interval in miniplate group was found to be 2.70 ± 0.48 with a median score of 3.00. The mean radiographic score in 3D plate was found to be 2.90 ± 0.32 with a median score of 3.00 (Graph 4; Table 5). The median difference between the two groups was not statistically significant (P > 0.05).
Graph 4.
Comparison of radiographic scores between miniplate and 3D plate group postoperatively and at 3 months interval
Table 5.
Comparison of radiographic scores at 3 months time interval in the groups
| Group | N | Mean | Std. dev. | Median | Z | P value |
|---|---|---|---|---|---|---|
| Miniplate | 10 | 2.70 | 0.48 | 3.00 | −1.090 | 0.276 |
| 3D plate | 10 | 2.90 | 0.32 | 3.00 |
Radiolucency at 3 months period was found in 1 patient (10%) in the miniplate group and it was not found in any patients in the 3D plate group (Table 6). But the difference in the proportion of patients with radiolucency, between the groups was not statistically significant (P > 0.05). The patient with radiolucency in miniplate group was asymptomatic and no active intervention was done in this case.
Table 6.
Comparison of complications in two groups
| Complications | Miniplate | 3D plate | Z | P value | ||
|---|---|---|---|---|---|---|
| Present | Absent | Present | Absent | |||
| Radiolucency | 1 | 9 | 0 | 10 | 1.03 | 0.305 |
| Non-union | 0 | 10 | 0 | 10 | – | – |
| Mal-union | 0 | 10 | 0 | 10 | – | – |
| Infections | 2 | 8 | 1 | 9 | 0.63 | 0.531 |
| Occlusal discrepancies | 3 | 7 | 1 | 9 | 1.12 | 0.264 |
None of the patients in both the groups had complications of non-union or mal-union (Table 6).
In miniplate group, 2 patients (20%) had infections and in 3D plate group 1 patient (10%) had infection. But the difference in the proportion of patients having infection, between the two groups was not statistically significant (P > 0.05). The infections in both the groups were treated with antibiotics and resolved uneventfully (Table 6).
3 patients in miniplate group had occlusal discrepancies (30%) and 1 patient in 3D plate group had occlusal discrepancies (10%). However, the difference in the proportion of patients with occlusal discrepancies between the two groups were not statistically significant (P > 0.05). The use of intermaxillary elastics helped to solve the problem in all such cases (Table 6).
Overall, complications were found in 6 patients (60%) in miniplate group and 2 patients (20%) in 3D plate group. The data when compared was statistically significant (P < 0.05) (Table 7).
Table 7.
Comparison of the overall complications in two groups
| Complications | Miniplate | 3D plate | Z | P value |
|---|---|---|---|---|
| Present | 6 | 2 | 2.13 | 0.031 |
| Absent | 4 | 8 |
Discussion
The objectives in the treatment of mandibular fracture are to re-establish normal occlusion and masticatory function with minimal disability and complications.
Conservative treatment to achieve this is performed by immobilizing the mandible for the healing period by intermaxillary fixation which is achieved by dental wiring, arch bars, cap splints, and gunning splints. Operative treatment of mandibular fractures involves intra or extraoral opening of the fracture site and direct osteosynthesis with transosseous wires, lag screws, or bone plates [5]. A number of fixation methods have been advocated for the treatment of mandibular fractures [6].
Currently, open reduction with internal fixation is the norm and tiny titanium plates are used to immobilize fragments of the jaw. Morbidity of the procedure is low with the advantage that the patient returns to normal function within days of treatment [5]. The intraoral approach is preferred unless indicated otherwise as it is time saving and less traumatic [7]. The miniplates are applied close to tension zone of mandible. The screws are monocortical to prevent injury to dentition and alveolar nerve [8–11].
The titanium is the metal of choice for fixation plates; mainly because of its high biocompatibility and ease of manipulation [4, 12, 13]. Modification of miniplates like titanium 3D plating system was developed by Farmand [2] to meet the requirements of semi rigid fixation with lesser complications.
The 3D miniplates is a misnomer as the plates are not three dimensional but hold the fracture fragments rigidly by resisting the forces in three dimensions namely shearing, bending and torsional forces [2]. The basic concept of 3D fixation as explained by Farmand [2] is that a geometrically closed quadrangular plate secured with bone screws creates stability in three dimensions. The stability is gained over a defined surface area and is achieved by its configuration and not by thickness or length. The large free areas between the plate arms and minimal dissection permit good blood supply to the bone [2].
The newly introduced 3D plating system provides definite advantages over conventional miniplates. The 3D plating system uses fewer plates and screws as compared to conventional miniplates to stabilize the bone fragments. Thus it uses lesser foreign material, reduces the operation time and overall cost of the treatment as described by Zix et al. and Farmand [1, 2, 14].
The 3D plating system has a compact design and is easy to use. The 1.0 mm thick 3D plate is as stable as the much thicker 2–0 mm miniplate. This offers better bending stability and more resistance to out of plane movement or torque [1].
Whether one method is superior to another or not, it is difficult to determine. Zix et al. [1] concluded that 3D plating system is an easy to use alternative to conventional miniplates to treat mandibular angle fractures. Various researches show that the 3D plating system offers more favorable biomechanical behavior than the conventional miniplates in terms of stability and strain resistance in different regions of mandible [1, 3, 4, 14, 15].
In this study, 25 fractures were observed in the 20 patients selected, which were divided into two groups. All fractures were found to be adequately fixed when checked intra-operatively after fixation. No post-operative IMF was required in either of the groups. None of the patients in both the groups had complications of non-union or mal-union. The mean radiographic score at post operative time interval in miniplate group was found to be 2.80 ± 0.42 and in 3D plate was found to be 2.90 ± 0.32.
The mean radiographic score at 3 months time interval in miniplate group was found to be 2.70 ± 0.48, while in 3D plate was found to be 2.70 ± 0.48. Radiolucency at 3 months period was found in 1 patient (10%) in the miniplate group and it was not found in any patients in the 3D plate group. The patient with radiolucency in miniplate group was asymptomatic and no active intervention was required.
Overall, complications were found in 6 patients (60%) in miniplate group and 2 patients (20%) in 3D plate group. The data when compared was statistically significant (P < 0.05). There are no in vivo studies done on comparison of two groups as such, while evaluating the efficacy of 3D miniplates, our results go well with those described by Zix et al. [1]; Farmand [2]; Meyer et al. [3]; Alkan et al. [4]; Farmand and Dupoirieux [14]; and Wittenberg et al. [16].
In the present study, it is seen that 3D titanium miniplates are effective in the treatment of mandibular fractures and overall complication rates are lesser as compared to conventional miniplates. Both the systems are equally stable when used to treat mandibular fractures.
In the symphysis and parasymphysis region, 3D plating system uses lesser foreign material, as only one plate and four screws are used as compared to two plates and eight screws in case of conventional miniplates. This reduces the overall cost of the treatment to almost half for 3D plate as compared to conventional miniplates of the same manufracturer. However in other areas of mandible hardware used is the same with comparable cost of both the systems. Also there is reduction in the operation time for 3D plate in the symphysis and parasymphysis region.
Thus 3D plate can be used as an alternative to conventional miniplates. The system is reliable and effective treatment modality for mandibular fractures as the traditional miniplates. Further, the use of 3D plating system in various procedures of maxillofacial region needs to be explored.
Conclusion
The findings of this prospective analysis indicate that 3D titanium miniplates are effective in the treatment of mandibular fractures and overall complication rates are lesser as compared to conventional miniplates. Both the systems have adequate stability after fixation of fracture. The stability of 3D plate is gained over a defined surface area and is achieved by its configuration and not by thickness or length. The large free areas between the plate arms and minimal dissection permit good blood supply to the bone. The 3D system is easy to use and cost effective. Further it uses lesser hardware as compared to conventional miniplates. Thus 3D plate can be used as an alternative to conventional miniplates. The system is reliable and effective treatment modality for mandibular fractures.
References
- 1.Zix J, Lieger O, Iizuka T. Use of straight and curved 3-dimensional titanium miniplates for fracture fixation at the mandibular angle. J Oral Maxillofac Surg. 2007;65:1758–1763. doi: 10.1016/j.joms.2007.03.013. [DOI] [PubMed] [Google Scholar]
- 2.Farmand M. Three dimensional plate fixation of fractures and osteotomies. Facial Plast Surg Clin North Am. 1995;3(1):39–56. [Google Scholar]
- 3.Meyer C, Serhir L, Boutemi P. Experimental evaluation of three osteosynthesis devices used for stabilizing condylar fractures of the mandible. J Craniomaxillofac Surg. 2006;34:173–181. doi: 10.1016/j.jcms.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 4.Alkan A, et al. Biomechanical comparison of different plating techniques in repair of mandibular angle fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:752–756. doi: 10.1016/j.tripleo.2007.03.014. [DOI] [PubMed] [Google Scholar]
- 5.Mukerji R, Mukerji G, McGurk M. Mandibular fractures: historical perspective. Br J Oral Maxillofac Surg. 2006;44:222–228. doi: 10.1016/j.bjoms.2005.06.023. [DOI] [PubMed] [Google Scholar]
- 6.Eberad K, Schilli W. Oral and maxillofacial traumatology. Chicago: Quintessence Pub. Co.; 1982. pp. 308–370. [Google Scholar]
- 7.Raveh J, Vuillemin T, Ladrach K, Sutter F. Plate osteosynthesis of 367 mandibular fractures. The unrestricted indication for intraoral approach. J Craniomaxillofac Surg. 1987;15(5):244–253. doi: 10.1016/S1010-5182(87)80061-6. [DOI] [PubMed] [Google Scholar]
- 8.Kroon HMF, Mathisson M, Cordey JR, Rahn BA. The use of miniplates in mandibular fractures. J Craniomaxillofac Surg. 1991;19:199–204. doi: 10.1016/S1010-5182(05)80547-5. [DOI] [PubMed] [Google Scholar]
- 9.Moreno JC, Ferncindez A, Ortiz JA, Montalvo JJ. Complication rates associated with different treatments for mandibular fractures. J Oral Maxillofac Surg. 2000;58:273–280. doi: 10.1016/S0278-2391(00)90051-X. [DOI] [PubMed] [Google Scholar]
- 10.Shumrick KA. Complications of facial plating. Oper Tech Otolaryngol Head Neck Surg. 1995;6(2):135–141. doi: 10.1016/S1043-1810(05)80025-9. [DOI] [Google Scholar]
- 11.Feller KU, et al. Analysis of complications in fractures of the mandibular angle—a study with finite element computation and evaluation of data of 277 patients. J Oral Maxillofac Surg. 2003;31:290–295. doi: 10.1016/s1010-5182(03)00015-5. [DOI] [PubMed] [Google Scholar]
- 12.Rosenberg A, Gratz KW, Sailer HF. Should titanium miniplates be removed after bone healing is complete? Int J Oral Maxillofac Surg. 1993;22:185–188. doi: 10.1016/S0901-5027(05)80249-8. [DOI] [PubMed] [Google Scholar]
- 13.Matthew IR, Frame JW, Browne RM, Millar BG. In vivo surface analysis of titanium and stainless steel miniplates and screws. Int J Oral Maxillofac Surg. 1996;25:463–468. doi: 10.1016/S0901-5027(96)80085-3. [DOI] [PubMed] [Google Scholar]
- 14.Farmand M, Dupoirieux L. The value of 3-dimensional plates in maxillofacial surgery. Rev Stomatol Chir Maxillofac. 1992;93(6):353–357. [PubMed] [Google Scholar]
- 15.Fonseca RJ. Oral and maxillofacial trauma. 3. Philadelphia: Elsevier Saunders Company; 2005. pp. 1132–1164. [Google Scholar]
- 16.Wittenberg JM, Mukherjee DP, Smith BR, Kruse RN. Biomechanical evaluation of new fixation devices for mandibular angle fractures. Int J Oral Maxillofac Surg. 1997;26:68–73. doi: 10.1016/S0901-5027(97)80852-1. [DOI] [PubMed] [Google Scholar]