Abstract
Aims and Objectives
This comparative study compares the primary and secondary healing after surgical removal of impacted mandibular third molars, evaluating and monitoring the extent of swelling and severity of pain and trismus.
Materials and Methods
60 patients (37 females, 23 males; age range 18–40 years) were included in the series. The patients were randomly subdivided into 2 groups of 30 each. All the patients were operated by the same operator under same clinical conditions. Group 1 had 30 patients who underwent primary closure. Group 2 had 30 patients who underwent secondary closure. Pain, swelling and trismus were evaluated for 1st, 3rd and 7th days after surgery with a VAS scale.
Results
An analysis of immediate findings showed that the patients with primary closure experienced significantly greater pain, swelling and trismus than that was experienced by patients with secondary closure. When the subsequent findings were analyzed there was statistically significant difference in pain, swelling and trismus experienced between both the groups.
Conclusion
The findings of this study suggest that the procedure of choice after removal of impacted mandibular third molars is a secondary closure and healing by secondary intention. A secondary closure appears to minimize the postoperative edema, pain and trismus and thus contributes to enhanced patient comfort.
Keywords: Third molar surgery, Primary wound closure, Secondary wound closure
Introduction
The removal of lower third molars is one of the most frequently performed procedures in oral and maxillofacial surgery. Mandibular third molar removal often causes considerable post operative discomfort.
Many methods and drugs have been tried in order to relieve this post operative discomfort so that the patient does not loose working man hours and the quality of life is not affected.
Different anti-inflammatory and antibacterial drugs have been tried on the mandibular third molar surgery model to asses relief in post operative complications [1–7]. Authors have also compared the insertions of cones [8] or drains [9, 10] saturated with antimicrobial agents in third molar sockets with primary closure and found that in most studies there was a significant decrease in post operative discomfort in the medicated group. Studies show that the amount of post operative discomfort is also related to the type of wound closure [10–12]. From the standpoint of rationalizing health service expenditure, it has been calculated that the cost incurred by convalescence and temporary inability to work increase the total expenditure for removal of third molars by 25% [13, 14]. Apart from economic implications, third molar surgery gives rise to a significant morbidity, in the form of pain, trismus and swelling that may be severe enough to interfere with normal activities. Reducing or minimizing these post operative sequelae after third molar surgery seems a laudable goal, particularly if clinical healing is not compromised [5]. One of the factors most closely linked to the intensity of post operative pain and swelling is type of healing of the surgical wound [10–12].
In secondary healing, the socket remains in communication with the oral cavity whereas, in primary healing, the socket is covered and sealed hermetically by a mucosa flap [12]. A primary closure is preferred by Howe, Archer, Giralnick, Kruger, Thoma and Killey and Kay [11]. Other authors like Bourgoyne, Blair, Ivy, Padgett and Mead prefer the wounds to heal by secondary closure [11]. On the other hand, Clark and Winter indicate that the wounds may be treated by either method. The use of surgical drain has also been suggested [9, 10]. Woodward advocates the use of a small opening posterior to the second molar to facilitate post operative irrigation of the wound. [11].
Our study compares the primary and secondary healing after surgical removal of impacted mandibular third molars, evaluating the incidence of post operative infection and monitoring the extent of swelling and severity of pain and trismus.
Materials and Methods
60 patients (37 females, 23 males; age range 18–40 years) were included in the series. The patients were randomly subdivided into 2 groups of 30 each. Group 1 had 30 patients who underwent primary closure. Group 2 had 30 patients who underwent secondary closure. Prior to the surgery, the patients were told that two equally acceptable surgical closure techniques would be used and written consent was taken.
Selection Criteria All healthy patients with no abusive habits, within the age group of 18–40 years, irrespective of gender with mesioangularly impacted asymptomatic mandibular third molars were selected.
Both the groups required osteotomy and sectioning of the tooth. The selected patients were not allergic to the local anesthetic used. All patients were operated by the same operator, given the same postoperative instructions and medication.
The patients were examined on the 1st, 3rd, and 7th postoperative days, for pain, swelling and trismus using a VAS scale.
Surgical Protocol
All the 60 mandibular third molars were surgically removed under local anesthesia using the Ward’s incision (Fig. 1), ostectomy was done, the tooth was delivered and after achieving hemostasis a primary or secondary closure was done randomly.
In group 1 (primary healing) the flap was repositioned hermetically with 3–0 black silk sutures (Fig. 2).
In group 2 (secondary healing), a wedge of mucosa 5–6 mm wide was removed from the buccal flap and was repositioned and sutured using 3–0 black silk (Fig. 3). No dressing was applied to open socket.
Fig. 1.

Ward’s Incision
Fig. 2.

Primary closure of the wound
Fig. 3.

Secondary closure of the wound
Evaluation Criteria
Patients were evaluated for pain, swelling and trismus on 1st, 3rd, and 7th postoperative day, the pain was measured by the patient using a Visual analogue scale (VAS) of 0 to 5 (Table 1). The swelling was assessed by the patient using a VAS of 0 to 5 (Table 2). Trismus was evaluated using simple graduated metallic scale.
Table 1.
| Score | ||
|---|---|---|
| 0 | No pain | The patient feels well |
| 1 | Slight pain | If the patient is distracted he or she does not feel the pain |
| 2 | Mild pain | The patient feels the pain even if concentrating on some activity |
| 3 | Severe pain | The patient is very disturbed but nevertheless can continue with normal activities |
| 4 | Very severe pain | The patient is forced to abandon normal activities |
| 5 | Extremely severe pain | The patient must abandon every type of activity and feels the need to lie down |
Table 2.
| Score | ||
|---|---|---|
| 0 | No swelling | The patient does not detect the slightest swelling |
| 1 | Slight swelling | The patient detects a slight swelling but it is not very noticeable |
| 2 | Mild swelling | The swelling is noticeable but does not interfere with normal mastication and swallowing |
| 3 | Severe swelling | The swelling is evident and hinders normal mastication |
| 4 | Very severe swelling | The swelling is marked. Mastication is hindered but there is no reduction in mouth opening (no trismus) |
| 5 | Extremely severe swelling | The swelling is very evident and mouth opening is reduced (trismus) |
Statistical Methods
The VAS scale values at each visit in the two groups are showed as mean, standard error, minimum and maximum. Mean differences between the two groups are presented with a 95% confidence interval. A suitable analysis of variance model for repeated measures was used to compare the variation of VAS scale values reported on each of the 7 days in the two groups. The F value of ANOVA for repeated measures are showed in the Results section as Fn,d (where n: numerator degree of freedom and d: denominator degree of freedom). Differences with P < 0.05 were considered statistically significant. To avoid an excessive Beta error, no correction for multiple comparisons was applied to the significance levels presented.
Result
There was a significant difference in the severity of pain between the two groups, at all times recorded. Intensity of pain was greater in Group 1 patients (primary healing) on 1st, 3rd, and 7th postoperative days. There was a statistically significant difference in swelling between the two groups on 1st, 3rd and 7th postoperative days. Swelling was more severe in Group 1, the peak of swelling being on day 3. In Group 2, the severity of swelling had a much smaller peak, again on day 3. There was significant difference in the degree of mouth opening in the 2 groups, with more trismus associated with primary closure.
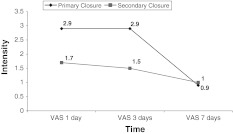
Pain
Highly significant differences were observed between the days with F′ value of 61.0 with a probability of 0.000 and between closures with F value of 68.53 with probability of 0.000. At primary closure, on 1st day VAS, pain was observed at a mean value of 2.9 with a minimum of 1.0 and maximum of 5.0 with standard deviation of 0.92, while on 3rd day VAS, the mean value of 2.9 with 1.0 and 4.0 minimum and maximum respectively. At 7th day VAS, the mean value was 1.0 with a minimum of 0.0 and maximum of 2.0 with standard deviation of 0.61.
At secondary closure, on 1st day VAS, pain was observed at a mean value of 1.7 with a minimum of 1.0 and maximum of 4.0 with standard deviation of 0.92, while on 3rd day VAS, the mean value of 1.5 with 1.0 and 3.0 minimum and maximum, respectively. At 7th day VAS, the mean value was 0.9 with a minimum of 0.0 and maximum of 2.0 with standard deviation of 0.61.
The confidence interval of 95% was observed at VAS 1st day of 2.10 and 2.54 and 1.96 to 2.40 at VAS 3rd day and 0.73 to 1.17 at VAS 7th day. (Table 3 and Graph 1).
Table 3.
Pain statistical analysis of data
| Class | VAS | VAS | VAS | Classes | F′ | d.f. | P value | |
|---|---|---|---|---|---|---|---|---|
| 1 day | 3 days | 7 days | ||||||
| Primary closure (Group 1) | N | 30 | 30 | 30 | Between closures | 68.53 | 1,174 | 0.000 |
| Mean | 2.9 | 2.9 | 1.0 | Between days | 61.00 | 2,174 | 0.000 | |
| SE | 0.92 | 0.71 | 0.61 | Closure × days | 11.97 | 2,174 | 0.000 | |
| Minimum | 1.0 | 1.0 | 0.0 | |||||
| Maximum | 5.0 | 4.0 | 2.0 | |||||
| Secondary closure (Group 2) | N | 30 | 30 | 30 | ||||
| Mean | 1.7 | 1.5 | 0.9 | |||||
| SE | 0.91 | 0.57 | 0.68 | |||||
| Minimum | 1.0 | 1.0 | 0.0 | |||||
| Maximum | 4.0 | 3.0 | 2.0 | |||||
| Difference between means | 1.2 | 1.4 | 0.1 | |||||
| CI 95% | Lower | 2.10 | 1.96 | 0.73 | ||||
| Upper | 2.54 | 2.40 | 1.17 | |||||
Graph 1.
Comparison of pain between primary and secondary closure
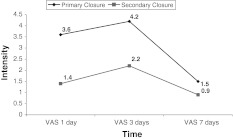
Swelling
Highly significant differences were observed between days with F′ value of 159.2 with a probability of 0.000 and between closures with F value of 318.60 with a probability of 0.000. At primary closure, on 1st day VAS, swelling was observed at a mean value of 3.6 with a minimum of 2.0 and maximum of 5.0 with standard deviation of 0.67, while on 3rd day VAS, the mean value of 4.2 with 3.0 and 5.0 minimum and maximum, respectively. At 7th day VAS, the mean value was 1.5 with a minimum of 0.0 and maximum of 3.0 with standard deviation of 0.63.
At secondary closure, on 1st day VAS, swelling was observed at a mean value of 1.4 with a minimum of 1.0 and maximum of 2.0 with standard deviation of 0.50, while on 3rd day VAS, the mean value of 2.2 with 1.0 and 3.0 minimum and maximum, respectively. At 7th day VAS, the mean value was 0.9 with a minimum of 0.0 and maximum of 2.0 with standard deviation of 0.55. The confidence interval of 95% was observed at VAS 1st day of 2.35 and 2.67 and 1.05 to 3.32 at VAS 3rd day and 1.05 to 1.37 at VAS 7th day. (Table 4; Graph 2).
Table 4.
Swelling statistical analysis of data
| Class | VAS | VAS | VAS | Classes | F′ | d.f. | P value | |
|---|---|---|---|---|---|---|---|---|
| 1 day | 3 days | 7 days | ||||||
| Primary closure (Group 1) | N | 30 | 30 | 30 | Between closures | 318.6 | 1,174 | 0.000 |
| Mean | 3.6 | 4.2 | 1.5 | Between days | 159.2 | 2,174 | 0.000 | |
| SE | 0.67 | 0.70 | 0.63 | Closure × days | 30.2 | 2,174 | 0.000 | |
| Minimum | 2.0 | 3.0 | 0.0 | |||||
| Maximum | 5.0 | 5.0 | 3.0 | |||||
| Secondary closure (Group 2) | N | 30 | 30 | 30 | ||||
| Mean | 1.4 | 2.2 | 0.9 | |||||
| SE | 0.50 | 0.59 | 0.55 | |||||
| Minimum | 1.0 | 1.0 | 0.0 | |||||
| Maximum | 2.0 | 3.0 | 2.0 | |||||
| Difference between means | 2.2 | 2.0 | 0.6 | |||||
| CI 95% | Lower | 2.35 | 3.00 | 1.05 | ||||
| Upper | 2.67 | 3.32 | 1.37 | |||||
Graph 2.
Comparison of swelling between primary and secondary closure
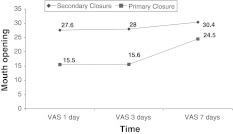
Trismus
Highly significant differences were observed between days with F′ value of 73.3 with a probability of 0.000 and between closures with F value of 507.8 with a probability of 0.000. At primary closure, on 1st day VAS, Trismus was observed at a mean value of 27.6 with a minimum of 20 and maximum of 32 with standard deviation of 2.79, while on 3rd day VAS, the mean value of 28 with 20 and 32 minimum and maximum, respectively. At 7th day VAS, the mean value was 30.4 with a minimum of 27 and maximum of 33 with standard deviation of 1.25.
At secondary closure, on 1st day VAS, Trismus was observed at a mean value of 15.5 with a minimum of 9.0 and maximum of 20.0 with standard deviation of 3.77, while on 3rd day VAS, the mean value of 15.6 with 9.0 and 22 minimum and maximum, respectively. At 7th day VAS, the mean value was 24.5 with a minimum of 20.0 and maximum of 29.0 with standard deviation of 2.91.
The confidence interval of 95% was observed at VAS 1st day of 20.62 and 22.40 and 20.91 to 22.69 at VAS 3rd day and 26.54 to 28.32 at VAS 7th day. (Table 5; Graph 3).
Table 5.
Trismus statistical analysis of data
| Class | VAS | VAS | VAS | Classes | F′ | d.f. | P value | |
|---|---|---|---|---|---|---|---|---|
| 1 day | 3 days | 7 days | ||||||
| Primary closure (Group 1) | N | 30 | 30 | 30 | Between closures | 507.8 | 1,174 | 0.000 |
| Mean | 15.5 | 15.6 | 24.5 | Between days | 73.3 | 2,174 | 0.000 | |
| SE | 3.77 | 4.00 | 2.91 | Closure × days | 21.9 | 2,174 | 0.000 | |
| Minimum | 9.0 | 9.0 | 20.0 | |||||
| Maximum | 2.0 | 22.0 | 29.0 | |||||
| Secondary closure (Group 2) | N | 30 | 30 | 30 | ||||
| Mean | 27.6 | 28.0 | 30.4 | |||||
| SE | 2.79 | 2.60 | 1.25 | |||||
| Minimum | 20.0 | 20.0 | 27.0 | |||||
| Maximum | 32.0 | 32.0 | 33.0 | |||||
| Difference between means | 12.1 | 12.4 | 5.9 | |||||
| CI 95% | Lower | 20.62 | 20.91 | 26.54 | ||||
| Upper | 22.40 | 22.69 | 28.32 | |||||
Graph 3.
Comparison of trismus between primary and secondary closure
An analysis of immediate findings showed that the patients with primary closure experienced significantly greater pain than that was experienced by patients with secondary closure. When the subsequent findings were analyzed there was statistically significant difference in pain experienced between both the groups. An analysis of immediate findings showed that swelling in patients with primary closure was significantly greater than in patients with secondary closure. An analysis of subsequent findings showed that the swelling in patients with primary closure was significantly greater as compared to patients with secondary closure.
An analysis of immediate findings showed that trismus was significantly greater in patients with primary closure. An analysis of subsequent findings showed that trismus was significantly greater in patients with primary closure as compared to patients with secondary closure.
Discussion
Acute inflammation is the immediate and early response to injury. A critical function of the response is to deliver leucocytes to the site of injury, where they can help clear the invading bacteria, as well as degrade the necrotic tissues resulting from damage.
Healing of the Wounds can be Accomplished in One of the Following 2 Ways
Healing by primary intention
Healing by secondary intention
Healing by Primary Intention
Immediately after injury, the space between the approximated surfaces of incised wound is filled with blood which then clots and seals the wound against dehydration and infection. Acute inflammatory response occurs within 24 h with the appearance of neutrophils from the margins of the incision. By the 3rd day, polymorphs are replaced by macrophages. The basal cells of epidermis from both the cut margins start proliferating and migrating towards incisional space in the form of epithelial spurs. A well approximated wound is covered by layer of epithelium in 48 h. By the 5th day, a multilayered new epithelium is formed which is differentiated into superficial and deeper layers. By 3rd day, fibroblasts also invade the wound area. By 5th day, new collagen fibrils start forming which dominate till healing is completed [16].
Healing by Secondary Intention
After removal of the tooth, the blood which fills the socket coagulates, within first 24–48 h after extraction, there is vasodilatation and engorgement of blood vessels in the remnants of the periodontal ligament and mobilization of leucocytes to the immediate area around the clot. Within the first week after tooth extraction, proliferation of fibroblasts from connective tissue cells in the remnants of periodontal ligament is evident, and these fibroblasts begin to grow into the clot around the periphery. This clot forms an actual scaffold upon which cells associated with healing process may migrate. It is only a temporary structure, however, and is gradually replaced by granulation tissue. The epithelium at the periphery of the wound exhibits evidence of proliferation in the form of mild mitotic activity even at this time. The crest of alveolar bone which makes up the margin of the socket exhibits beginning of the osteoclastic activity. Endothelial cell proliferation signalling the beginning of capillary ingrowth may be seen. During this period, the blood clot begins to undergo organization by the ingrowth around the periphery of the fibroblasts and occasional small capillaries from the residual periodontal ligament. An extremely thick layer of leucocytes forms over the surface of the clot, and the edge of the wound continues to exhibit epithelial proliferation [17].
The extent of swelling, the severity of pain and trismus are the chief indicators of patient discomfort during the post operative period after third molar removal. The purpose of this study was to compare the closure by primary intention and the closure that used a window, with healing by secondary intention. The effectiveness of the techniques was evaluated relative to degree of patient comfort and postoperative condition of the surgical site.
This study determined that the secondary healing is more comfortable for the patients with regard to these three parameters. Swelling and pain were evaluated with the VAS scale, which is considered to be an efficacious tool to evaluate clinical parameters that influence the subjective experience of an individual, such as pain. Trismus was measured by measuring the interincisal mouth opening [12, 18].
Photographic techniques and computerised tomography scanning have also been proposed to measure anatomical changes in the profile of patients subjected to third molar surgery [19]. Stereophotographic techniques, proposed by Pedersen and Mearsk-Moller [12, 20] are probably the most sophisticated method described to date, but are too complex for clinical use.
Henrikson et al. [21] proposed the use of the VAS scale to measure swelling, and compared the effects of two drugs on the post operative course following third molar surgery in his study.
From a review of the findings, it is evident that the sample size provided a means for detecting statistically significant differences in the patients’ responses to the closure technique.
The degree of edema, severity of pain and trismus are primary indicators of patient’s discomfort. Our findings suggest that during 1st, 3rd and 7th postoperative days, the patients with secondary closure were more comfortable. During the immediate postoperative period, there was greater degree of hematoma and edema formation in the patients with primary closure.
The results obtained in the present study indicate that secondary closure of the socket causes less inconvenience for the patient as it appears to minimize post-extraction swelling, pain and trismus.
The results obtained are in agreement with many of those reported in the literature [10–12, 22].
In a split-mouth study on 56 patients, Dubois et al. [11] extracted both mandibular third molars simultaneously. Closure was primary on the left; on the right, the mucosa distal to the second molar was incised so as to create a window of approximately 6 mm circumference and leave the socket open for secondary healing. Secondary closure was found to minimise swelling and pain in the immediate post operative period, helping to reduce patient discomfort.
Holland and Hindle [22] showed that post operative pain and swelling were more marked in “closed” than in “open” healing, and that the technique of election should be “open” healing. This despite their finding that at 1 month from surgery the wound appeared to have healed better in “closed” healing.
Brabander and Cattaneo [10] evaluated two different types of wound closure after removing mandibular third molars impacted in the mucosa. In the test group a portion of mucosa distal to the second molar was removed and a drain, in the form of vaselined gauze, was inserted into the socket to ensure secondary closure of the surgical wound. In the control group they utilised the same surgical procedure but without drainage. Secondary closure was found to be preferable as it reduces pain and swelling post-surgery, but insertion of a vaselined gauze drain did not influence these parameters.
Rakprasitkul and Pairuchvej [18] compared primary healing associated to the insertion of a small drainage tube, removed on day 3, with primary healing alone. They found no significant difference with regard to severity of pain in the two groups, but swelling was significantly less in patients with drainage. In the drainage group, reduction of mouth opening was also less marked and there was less bleeding.
In a similar splitmouth study, Saglam [12] compared test side (surgical extraction, primary closure and drainage for 72 h) with control side (surgical extraction and primary closure alone). The results obtained by Rakprasitkul and Pairuchvej [18] were confirmed, and swelling, pain and trismus were significantly less severe on the test side. The use of drainage is recommended when the primary closure technique is employed. The results obtained in the present study enable us to conclude that, open healing of the surgical wound after removal of impacted third molars produces less post operative swelling, pain and trismus than occurs with closed healing, by hermetically suturing the socket.
Perhaps the English dentist, Mr Hunter, was correct in his text, “it is also a common practice, to close the gum as it is termed; this is more for show than use; for the gum cannot be made to close as to unite by the first intention.”[23].
Summary and Conclusion
The findings of this study suggest that the procedure of choice after removal of impacted mandibular third molars is a secondary closure and healing by secondary intention. A secondary closure appears to minimize the postoperative edema, pain and trismus and thus contributes to enhanced patient comfort.
Acknowledgment
Thanks to Mr. Sai Prasad for compiling the statistics and graphs of the study.
References
- 1.Curran JB, Kennett S, Young AR. An assessment of the use of prophylactic antibiotic in third molar surgery. Int J Oral Surg. 1974;3:1–6. doi: 10.1016/S0300-9785(74)80030-X. [DOI] [PubMed] [Google Scholar]
- 2.MacGregor AJ, Hutchinson D. The effect of sulfonamides on pain and swelling following removal of ectopic third molars. Int J Oral Surg. 1975;4:184–190. doi: 10.1016/S0300-9785(75)80024-X. [DOI] [PubMed] [Google Scholar]
- 3.Petersen JK. Anti-inflammatory and analgetic effects of indomethacin following removal of impacted mandibular third molars. Int J Oral Surg. 1975;4:267–276. doi: 10.1016/S0300-9785(75)80044-5. [DOI] [PubMed] [Google Scholar]
- 4.Svenn K, Gilhuus-Moe O. Paracetamol/Codeine in relieving pain following removal of impacted mandibular third molars. Int J Oral Surg. 1975;4:258–266. doi: 10.1016/S0300-9785(75)80043-3. [DOI] [PubMed] [Google Scholar]
- 5.MacGregor AJ, Addy A. Value of penicillin in the prevention of pain, swelling and trismus following the removal of ectopic mandibular third molars. Int J Oral Surg. 1980;9:166–172. doi: 10.1016/S0300-9785(80)80015-9. [DOI] [PubMed] [Google Scholar]
- 6.Troullos ES, Hargreaves KM, Butler DP, Dionne RA. Comparison of nonsteroidal anti-inflammatory drugs, ibuprofen and flurbiprofen, with methylprednisolone and placebo for acute pain, swelling and trismus. J Oral Maxillofac Surg. 1990;48:945–952. doi: 10.1016/0278-2391(90)90007-O. [DOI] [PubMed] [Google Scholar]
- 7.Schultze-Mosgau S, Schmelzeisen R, Frolich JC, Schmele H. Use of ibuprofen and methylprednisolone for prevention of pain and swelling after removal of impacted third molars. J Oral Maxillofac Surg. 1995;53:2–7. doi: 10.1016/0278-2391(95)90486-7. [DOI] [PubMed] [Google Scholar]
- 8.Nordenram A, Sydnes G, Odegaard J. Neomycin-bacitracin cones in impacted third molar sockets. Int J Oral Surg. 1973;2:279–283. doi: 10.1016/S0300-9785(73)80023-7. [DOI] [PubMed] [Google Scholar]
- 9.NzubeChukwuneke F, Oji C, Saheeb DB. A comparative study of the effect of using a rubber drain on postoperative discomfort following lower third molar surgery. Int J Oral Maxillofac Surg. 2008;37:341–344. doi: 10.1016/j.ijom.2007.11.016. [DOI] [PubMed] [Google Scholar]
- 10.Brabander EC, Cattaneo G. Effect of surgical drain together with a secondary closure technique on postoperative trismus, swelling and pain after mandibular third molar surgery. Int J Oral Maxillofac Surg. 1988;17:119–121. doi: 10.1016/S0901-5027(88)80164-4. [DOI] [PubMed] [Google Scholar]
- 11.Dubois DD, Pizer ME, Chinnis RJ. Comparison of primary and secondary closure techniques after removal of impacted mandibular third molars. J Oral Maxillofac Surg. 1982;40:631–634. doi: 10.1016/0278-2391(82)90111-2. [DOI] [PubMed] [Google Scholar]
- 12.Pasqualini D, Cocero N, Castella A, Mela L, Bracco P. Primary and secondary closure of the surgical wound after removal of impacted mandibular third molars: a comparative study. Int J Oral Maxillofac Surg. 2005;34:52–57. doi: 10.1016/j.ijom.2004.01.023. [DOI] [PubMed] [Google Scholar]
- 13.Shugars DA, Benson K, White RP, Simpson KN, Bader JD. Developing a measure of patient perceptions of short term outcomes of third molar surgery. J Oral Maxillofac Surg. 1996;54:1402–1408. doi: 10.1016/S0278-2391(96)90253-0. [DOI] [PubMed] [Google Scholar]
- 14.Ruta DA, Bissias E, ogston S, Ogdan GR. Assessing health outcomes after extraction of third molars: the postoperative symptom severity scale. Br J Oral Maxillofac Surg. 2000;38:480–487. doi: 10.1054/bjom.2000.0339. [DOI] [PubMed] [Google Scholar]
- 15.Holland CS. The development of a method of assessing swelling following third molar surgery. Br J Oral Surg. 1979;17(2):104–114. doi: 10.1016/S0007-117X(79)80037-2. [DOI] [PubMed] [Google Scholar]
- 16.Mohan H. Healing of tissues. In: Mohan H, editor. Essential pathology for dental students. 3. New Delhi: Jaypee Brothers Medical Publishers (P) Ltd; 2005. pp. 135–144. [Google Scholar]
- 17.Sivapathasundharam B. Healing of oral wounds. In: Shafer G, Hine MH, Levy BM, editors. Shafer’s textbook of oral pathology. 5. Delhi: Elsevier a Division of Reed Elsevier India Private Limited; 2008. pp. 816–842. [Google Scholar]
- 18.Rakprasitkul S, Pairuchvej V. Mandibular third molar surgery with primary closure and tube drain. Int J Oral Maxillofac Surg. 1997;26:187–190. doi: 10.1016/S0901-5027(97)80817-X. [DOI] [PubMed] [Google Scholar]
- 19.Gool AV, Ten Bosch JJ, Boering G. A photographic method of assessing swelling following third molar removal. Int J Oral Surg. 1975;4:121–129. doi: 10.1016/S0300-9785(75)80004-4. [DOI] [PubMed] [Google Scholar]
- 20.Ucok C. Stereophotogrammetric assessment of the effect of tenoxicam on facial swelling subsequent to third molar surgery. Int J Oral Maxillofac Surg. 1997;26:380–382. doi: 10.1016/S0901-5027(97)80802-8. [DOI] [PubMed] [Google Scholar]
- 21.Henrikson PA, Thilander H, Wahlander LA. Voltaren as an analgesic after surgical removal of a lower wisdom tooth. Int J Oral Surg. 1985;14:333–338. doi: 10.1016/S0300-9785(85)80022-3. [DOI] [PubMed] [Google Scholar]
- 22.Holland CS, Hindle MO. The influence of closure or dressing of third molar sockets on postoperative swelling and pain. Br J Oral Maxillofac Surg. 1984;22:65–71. doi: 10.1016/0266-4356(84)90011-1. [DOI] [PubMed] [Google Scholar]
- 23.Waite PD, Cherala S. Surgical outcomes for suture-less surgery in 366 impacted third molar patients. J Oral Maxillofac Surg. 2006;64:669–673. doi: 10.1016/j.joms.2005.12.014. [DOI] [PubMed] [Google Scholar]