Abstract
Successful management of temporomandibular joint (TMJ) ankylosis depends on adequate gap arthroplasty and interpositional graft; the objective is to produce a functioning pseudoarthrosis that prevents reankylosis and provides adequate mobility. Several interpositional grafts have been used for the treatment of temporomandibular joint ankylosis such as indigenous pterygomasseteric sling, temporalis muscle/fascia, auricular cartilage, fat and dermis-fat. Lateral thigh fascia lata (LTFL) graft is commonly used in neurosurgical practice and in other surgical specialities. We present a case of lateral thigh fascia lata used as interpositional graft for the treatment of a unilateral fibrous temporomandibular joint ankylosis.
Keywords: Temporomandibular joint, Ankylosis, Lateral thigh fascia lata
Introduction
Ankylosis release is the oldest form of TMJ surgery, and it has evolved from simple bone division to separate the ramus from the cranial base to complex arthroplasty [1]. The goals of surgery for TMJ ankylosis should be to establish movement, function in the jaw, prevent relapse, restore appearance, and achieve normal growth and occlusion in the child. The management of these patients is by gap arthroplasty with interpositional grafting [2]. Different interpositional grafts have been used, such as indigenous pterygomasseteric slings, temporomandibular meniscus, temporalis muscle/fascia, skin, auricular cartilage, fat and dermis-fat. Flaps of temporalis muscle and/or fascia were first described by Yolovine in 1898 and first used by Murphy in 1914 for surgery of the temporomandibular joint [2] and it has become the most popular interpositional grafting technique because of its simplicity and close proximity to the surgical site [1].
Lateral thigh fascia lata serves as an excellent dural substitute and is commonly used in neurosurgical practice. Fascia lata is strong, pliable, and easily sutured to native tissues. It is homologous tissue with no risk of foreign body reaction and a very low risk of infection [3]. Lateral thigh fascia lata is widely used in a large variety of surgical specialties when autologous graft tissue is desired, including cardiac surgery [4], orthopedic surgery [5], ophthalmology [6], urology [7], general surgery [8] and plastic and reconstructive surgery [9, 10]. We present a case of a unilateral temporomandibular joint ankylosis managed with gap arthroplasty and lateral thigh fascia lata as interpositional graft.
Case Report
A 30-year-old man with history of right temporomandibular joint trauma during a basket ball game was referred to our oral and maxillofacial department. Trauma had occurred 6 months before with no signs of mandibular fracture at any site. The chief complaint was a progressive decrease on mouth opening. Physical examination revealed a maximum mouth opening of 13 mm (Fig. 1). Panoramic x-ray showed signs of right temporomandibular joint ankylosis. Computed tomography showed images compatible with a right fibrous temporomandibular joint ankylosis with limitation of movements of right mandibular condyle during mouth opening (Fig. 2a, b). With these clinical and radiographic findings a diagnosis of a right fibrous TMJ ankylosis was done.
Fig. 1.

Preoperative maximum mouth opening of 13 mm
Fig. 2.
a Three-dimensional computed tomography with mouth closed. b Three-dimensional computed tomography during mouth opening, notice the limitation of movements of the right mandibular condyle and the presence of fibrous tissue between condyle and glenoid fossa
Under general anesthesia a right preauricular approach with Al-Kayat and Bramley modification was achieved and gap arthroplasty was performed by excision of the ankylosed mass beginning from the condylar neck and getting a final gap of 10 mm between ramus and skull base (Fig. 3).
Fig. 3.

Gap arthroplasty through a preauricular approach. A 10 mm gap arthroplasty was created
Once the ankylosed tissue was excised we proceeded to harvest lateral thigh fascia lata to use it as interpositional graft.
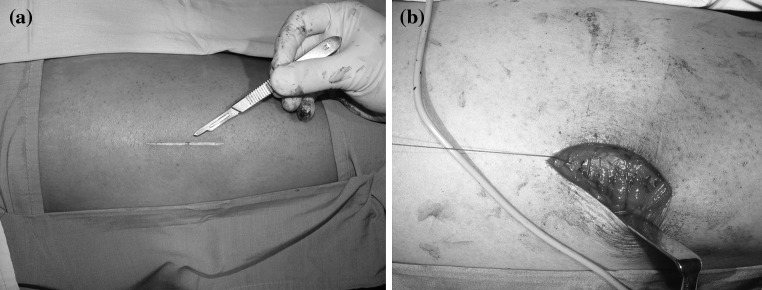
Harvesting Technique for Lateral Thigh Fascia Lata
A soft roll was placed beneath the buttock of the patient and the lower extremity was gently internally rotated. A linear incision was made on the side of the thigh using the iliotibial groove as a guide. The length of the incision depends on the size of the graft required in this case we used a 5 cms linear incision (Fig. 4a). After the incision was done, dissection was carried down through the subcutaneous fat and the fascia lata was exposed. This thick fascia lata arises superiorly from the tensor fascia lata and gluteus medius and Maximus muscles and inserts distally on the lateral condyle of the tibia. A fasciotomy incision was created parallel to the skin incision as posteriorly as possible on the graft. With an index finger, careful blunt dissection was used to separate the fascia from the underlying muscle, this finger dissection was made in order to avoid inadvertent trauma to the muscle with other instruments. The fasciotomy incision can be lengthened as desired to accommodate the size of the graft needed.
Fig. 4.
a Harvesting lateral thigh fascia lata. A 5 cms linear incision is done on the side of the right thigh. b Closure of the lateral thigh incision in layers after LTFL was grafted
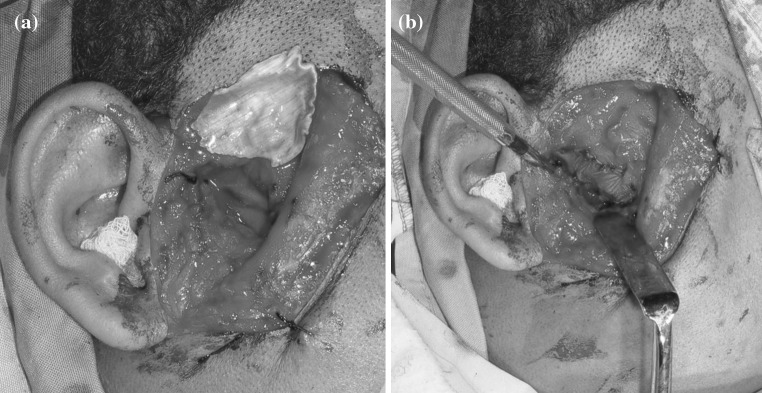
Since the ankylosed tissue had been already removed, a template of the amount of graft needed was done with latex of surgical gloves, then this was transposed to the fascia lata and the tissue was grafted. After harvesting, the graft was draped with a wet dressing until used. Even though this fascial defect can be left unreconstructed, we used a 2/0 Vicryl suture to correlate and approximate fascia lata as much as possible. Skin was closed in layers using subcutaneous interrupted 3/0 Vicryl sutures and 3/0 Nylon sutures for skin (Fig. 4b). Finally an elastic wrap was placed on the thigh to eliminate dead space during healing. Lateral thigh fascia lata was secured laterally, medially, anteriorly, and posteriorly between mandibular ramus and skull base with 3/0 vicryl suture (Fig. 5a, b). The preauricular incision was closed in layers. Physiotherapy was started from the first postoperative day. Patient has been followed up for 3 years without any sign of reankylosis and no complications after LTFL graft. Patient’s actual maximum mouth opening is 32 mm (Fig. 6).
Fig. 5.
a LTFL graft. b LTFL graft sutured laterally, medially, anterior and posterior between mandibular ramus and skull cranial base
Fig. 6.

Maximum mouth opening of 32 mm after 3 years from initial surgery
Discussion
Functional activity of the ankylosed TMJ relies primarily on the ostectomy created and the choice of interpositional material [11]. Arthroplasty without interpositional graft requires a gap of 10 to 20 mm and often results in mouth deviation and has a high recurrence rate of about 53%. For this reason it seems better to create a minimal gap greater than 5 mm and then perform interpositional graft to prevent recurrence caused by osteoblastic growth between the abraded surfaces [2]. The rationale behind interpositional arthroplasty is that the presence of dead space after extensive resection of callus leads to hematoma formation with subsequent organization. Local pluripotent stem cells may then be induced to differentiate into fibroblast and osteoblast, with deposition of collagen and bone. A decrease in vascularity and oxygen tension occurs in the surrounding tissues, favoring the transformation of fibrous tissue into cartilage and bone. The objective is to create a functioning pseudoarthrosis that prevents recurrence and provides adequate mobility [11].
No ideal interpositional graft is available because the problems encountered with the various available materials are that the temporalis muscle shows some degree of degeneration or atrophy and becomes fibrosed, which aggravates the trismus, fascia lacks of bulk, cartilage tends to fibrose and calcify, and alloplastic implants under functional loads disintegrate and cause foreign body giant cell reaction [2].
Lateral thigh fascia lata envelopes the muscles of the upper leg. Laterally, this fascia coalesces to a much thicker iliotibial band. This fascial band runs from ilial crest to the tibia. It is narrow distally and much broader proximally. Several muscles in the upper leg have fibrous attachments to this fascial band. The planes just superficial and deep to this band are essentially avascular. The iliotibial band lies under the subcutaneous tissue. LTFL is widely used in a large variety of surgical specialties.
LTFL graft has some advantages for its usage in this surgery: it is strong, pliable, and easily sutured to native tissues, it is easily harvested and no important nerves or vessels are encountered during surgical approach, the harvesting time should take about 15 to 20 min, no additional scar is done over temporalis muscle avoiding trismus secondary to degeneration, atrophy or fibrosis of temporalis muscle. Some of the complications of LTFL graft reported are: hematoma, dehiscence, nerve injury (distal branches of latero cutaneous nerve), muscle herniation [3, 12]. None of these complications were seen in our case. This case has 3 years of follow up to the date with no complications of the donor site and with no reankylosis. Actually the patient has a maximum mouth opening of 32 mm with mandibular deviation to the operative side while opening. The 32 mm of maximum mouth opening of our patient is almost on the lower scale reported by Kaban et al. in 1990 reporting excellent results with his protocol for treating TMJ ankylosis, with a maximal incisal opening of 37.5 ± 3.90 mm at 1 year in 14 patients with 18 affected joints [13]. In a more recent retrospective analysis of 11 children younger than 16 years of age treated by Kaban’s protocol he reports a mean maximal incisal opening of 38.2 mm with a range of 15 to 49 mm. Ten of the eleven patients had a maximal incisal opening greater than 30 mm [14]. Even though we just report one case, for us the usage of LTFL graft was safe and easy.
References
- 1.Dimitroulis G. The interpositional dermis-fat graft in the management of temporomandibular joint ankylosis. Int J Oral Maxillofac Surg. 2004;33(8):755–760. doi: 10.1016/j.ijom.2004.01.012. [DOI] [PubMed] [Google Scholar]
- 2.Bulgannawar BA, Rai BD, Nair MA, Kalola R. Use of temporalis fascia as an interpositional arthroplasty in temporomandibular joint ankylosis: analysis of 8 cases. J Oral Maxillofac Surg. 2011;69(4):1031–1035. doi: 10.1016/j.joms.2010.02.043. [DOI] [PubMed] [Google Scholar]
- 3.Link MJ, Converse LD, Lanier WL. A new technique for single-person fascia lata harvest. Neurosurgery. 2008;63(4 Suppl 2):359–361. doi: 10.1227/01.NEU.0000327035.12333.E3. [DOI] [PubMed] [Google Scholar]
- 4.Kohanna FH, Adams PX, Cunningham JN, Jr, Spencer FC. Use of autologous fascia lata as a pericardial substitute following open-heart surgery. J Thorac Cardiovasc Surg. 1977;74(1):14–19. [PubMed] [Google Scholar]
- 5.Kartus J, Movin T, Karlsson J. Donor-site morbidity and anterior knee problems after anterior cruciate ligament reconstruction using autografts. Arthroscopy. 2001;17(9):971–980. doi: 10.1053/jars.2001.28979. [DOI] [PubMed] [Google Scholar]
- 6.Bashshur Z, Ma’luf R, Najjar D, Noureddin B. Scleral fixation of posterior chamber intraocular lenses using fascia lata to cover the knots. Ophthalmic Surg Lasers. 2002;33(6):445–449. [PubMed] [Google Scholar]
- 7.Kargi E, Yeşilli C, Akduman B, Babucçu O, Hoşnuter M, Mungan A. Fascia lata grafts for closure of secondary urethral fistulas. Urology. 2003;62(5):928–931. doi: 10.1016/j.urology.2003.07.012. [DOI] [PubMed] [Google Scholar]
- 8.Vries Reilingh TS, Bodegom ME, Goor H, Hartman EH, Wilt GJ, Bleichrodt RP. Autologous tissue repair of large abdominal wall defects. Br J Surg. 2007;94(7):791–803. doi: 10.1002/bjs.5817. [DOI] [PubMed] [Google Scholar]
- 9.Rose EH. Autogenous fascia lata grafts: clinical applications in reanimation of the totally or partially paralyzed face. Plast Reconstr Surg. 2005;116(1):20–32. doi: 10.1097/01.PRS.0000169685.54862.18. [DOI] [PubMed] [Google Scholar]
- 10.Karaaltin MV, Orhan KS, Demirel T. Fascia lata graft for nasal dorsal contouring in rhinoplasty. J Plast Reconstr Aesthet Surg. 2009;62(10):1255–1260. doi: 10.1016/j.bjps.2008.03.053. [DOI] [PubMed] [Google Scholar]
- 11.Thangavelu A, Santhosh Kumar K, Vaidhyanathan A, Balaji M, Narendar R. Versatility of full thickness skin-subcutaneous fat grafts as interpositional material in the management of temporomandibular joint ankylosis. Int J Oral Maxillofac Surg. 2011;40(1):50–56. doi: 10.1016/j.ijom.2010.06.025. [DOI] [PubMed] [Google Scholar]
- 12.Amir A, Gatot A, Zucker G, Sagi A, Fliss DM. Harvesting large fascia lata sheaths: a rational approach. Skull Base Surg. 2000;10(1):29–34. [PMC free article] [PubMed] [Google Scholar]
- 13.Kaban LB, Perrott DH, Fisher K. A protocol for management of temporomandibular joint ankylosis. J Oral Maxillofac Surg. 1990;48:1145–1151. doi: 10.1016/0278-2391(90)90529-B. [DOI] [PubMed] [Google Scholar]
- 14.Kaban LB, Bouchard C, Troulis MJ. A protocol for managemento of temporomandibular joint ankylosis in children. J Oral Maxillofac Surg. 2009;67:1966–1978. doi: 10.1016/j.joms.2009.03.071. [DOI] [PubMed] [Google Scholar]