Abstract
The gold standard for surgical correction of both uni- and bilateral coronal synostosis remains to this day, the “standardised bilateral fronoto-orbital advancement and reshaping” based on the “tongue in groove” technique developed by Tessier. It consists of bilateral frontal craniotomy for suture release and decompression, combined with creation of a “supraorbital bar” as a bilateral orbital complex by osteotomising the orbital roof (anterior cranial base), supraorbital ridge and upper lateral orbital rims bilaterally. This is followed by a bilateral advancement and remodelling of the frontal region as well as the orbital region bilaterally which is then rigidly fixed in position, the supraorbital bar to the face (at the fronto-zygomatic region and the fronto-nasal region) and the reconstructed forehead to the supraorbital bar. In this study, a slightly modified procedure was employed for correction of the right sided unilateral coronal synostosis, using a bifrontal craniotomy combined with unilateral orbital osteotomy (creating a unilateral supraorbital bar/bandeau), followed by radial osteotomies/kerfing, reshaping and advancement of the bifrontal calvarial segment. This was followed by the “tongue in groove” advancement of the right orbital segment (unilaterally). We preferred to spare osteotomising the contralateral (that is, the left) orbital region as it was not involved by compensatory growth deformity, and the frontal bossing/bulging was restricted to the upper forehead region alone. A gratifying aesthetic outcome and perfect symmetry was achieved using this technique. There were also no complications like wound infection or dehiscence, CSF leak, bone loss from resorption, damage to orbital contents or brain, recurrence of the dysmorphology or residual deformities or asymmetrics of the orbital region or forehead. Gratifying cosmetic results were seen using this modified technique and it was found that bilateral frontal reshaping and unilateral orbital advancement together with kerfing the frontal segment followed by fixation using resorbable implants is an effective strategy to not only permit remodelling of the skull and face thus correcting the cosmetic deformity, but also to increase the intracranial volume within the anterior cranial vault, without the need for any graft placement.
Keywords: Plagiocephaly, Craniosynostosis, Fronto-orbital advancement, Biodegradeable implants
Introduction
Anterior plagiocephaly is a generally non-syndromic premature fusion of one of the coronal sutures presenting as mild to severe calvarial asymmetry resulting in an asymmetric forehead and brow.
The standardised “Bilateral fronto-orbital advancement and reshaping” is the most widely advocated surgical management of Anterior Plagiocephaly, based on the “tongue in groove” technique developed by Tessier [1, 5, 8–10]. Our patient was a one year old female child with unilateral right coronal synostosis. As the deformity mainly involved the forehead region bilaterally (flattening on the right and bulging/“bossing” on the left) and the orbital region unilaterally (retrusion and recession on the right with an elevated supraorbital ridge and rim), we modified the standard procedure by avoiding osteotomising the contralateral unaffected left orbital segment, with the aim to reduce the extent and duration of surgery. Bilateral frontal osteostomy and reshaping of the calvarial segment was carried out together with a “unilateral” advancement of the affected orbital component. The latter involved a unilateral osteotomy of the right orbital bar comprising of the orbital roof, supraorbital ridge and rim and the upper half of the lateral orbital rim, followed by its horizontal advancement and repositioning to increase the anteroposterior projection and depth of the recessed upper orbit. This procedure was performed in conjunction with “kerf cutting” and radial osteotomies on the endocranial side of the osteotomised frontal calvarial segment.
Biodegradeable plates and screws were used to stabilize the anteriorly repositioned orbital bar and the reshaped frontal calvarium. The resorbable plates provide rigid fixation for 2−3 months, rigid support for 3−6 months and then biodegrade at 9-12 months, eliminating the possibility of intracranial implant migration.
Case Report
A one year old female child was brought to our hospital by her parents who had noticed an abnormality in the shape of her head. On examination, she displayed an asymmetry in the upper third of her face caused by a flattening of the forehead and supraorbital ridge on the right. The right forehead and orbit appeared “swept back”. There was a “bulging”/“bossing” of the left forehead which also had abrasions sustained in a recent fall (Fig. 1). The right supraorbital ridge was retruded and recessed with the overlying eyebrow appearing higher than its left counterpart, and also lay posterior to the cornea of the slightly proptotic right eye. The right palpebral fissure was wider than the left. The child exhibited no overt signs or symptom of raised intracranial pressure.The right orbit exhibited the typical “Harlequin“deformity on the anteroposterior skull radiograph, caused by the elevated sphenoid wing, flattened and raised supraorbital rim and the shortened anterior cranial base on that side, which was suggestive of Anterior Plagiocephaly due to a right sided unilateral coronal synostosis. Computed Tomographic scan confirmed fusion of the right coronal suture, as compared with the unaffected left one, and demonstrated recessed ipsilateral frontal bone with compensatory bossing on the left side, ipsilateral elevated supraorbital rim, shallow orbit with exorbitism/proptosis of the right globe (Fig. 2).
Fig. 1.
One year old child with anterior plagiocephaly, prior to and 2 months after surgery
Fig. 2.
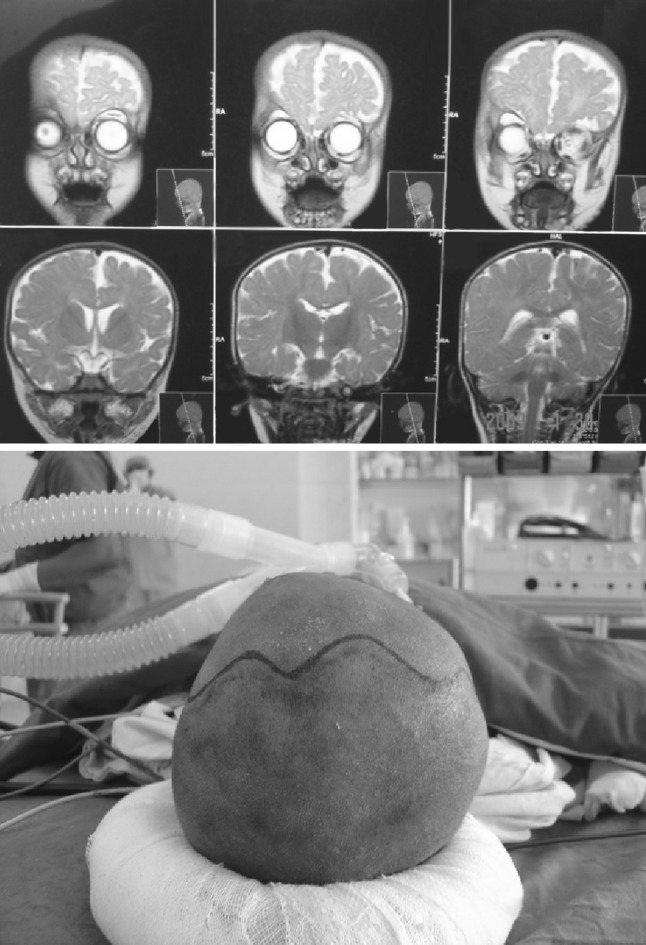
Rt. Fronto-orbital recession with proptotic Rt. globe
The child was otherwise in good health. After thorough systemic evaluation, blood typing and cross matching were done.
The child was positioned supine on the OT table and the anaesthesia team moved 110° away from the head end to allow maximum access for the operating team to the cranium and face. The hair on the head was shaved and the scalp, ears and entire face was prepared with Cutasept.
The bilateral coronal incision was marked (Fig. 2), following a zigzag, sinusoidal pattern in order to create a “stealth incision” which would be cosmetically acceptable as it would heal with less scarring due to a repeated change in the direction of force vectors. Such an incision is also less noticeable later in life as the hair will not part along a zig zag line as easily as it will along a straight incision line, particularly in patients with straight hair and especially when the hair is wet. The incision line was terminated a point 2 cm above the ear on each side. 0.25% Lidocaine with 1:200,000 adrenaline was infiltrated for hemostasis. Incision was made through the skin, subcutaneous tissue and galea. The subgaleal space was then dissected anteriorly in a blunt fashion detaching the cutaneous flap of the galea from the underlying periosteum/pericranium which was left intact. This separate dissection of the galea and periosteum renders the cutaneous flap more flexible. Electrocautery was used to ensure meticulous haemostasis right from the beginning of the surgery. The temporalis muscle was identified bilaterally and the periosteum along the border of the muscle was transected and the muscle dissected off the temporal fossa of the skull, as part of the scalp flap.
Approximately 2 cm above the supraorbital ridge, the pericranium was incised and dissected off the bone with the scalp flap which was then folded anteriorly and protected with wet abdominal pads. The nasofrontal suture was exposed. The supraorbital nerve lay in the supraorbital notch/goove and was reflected anteriorly, and the superior part of the eye capsule detached from the bony orbital funnel. The palpebgral ligament was detached from the frontozygomatic suture region.
The bilateral coronal craniotomy was outlined and cautery used to incise and dissect away the periosteum from the area of the proposed saw cuts. A Hudson brace hand drill was used to make bur holes through the calvaria and the bone dust so produced was stored in normal saline until the end of the procedure to later fill holes/defects in the calvaria. Rasps were used to undermine the dura and detach it from the bone along the lines of the proposed osteotomy. A gigli saw was then used to make the osteotomy between the adjacent bur holes, completing the frontal craniotomy. After completely detaching the remaining adherent dura, bicoronal bone flap/segment was carefully lifted off the underlying brain and removed to another table (Figs. 3, 4, 5).
Fig. 3.
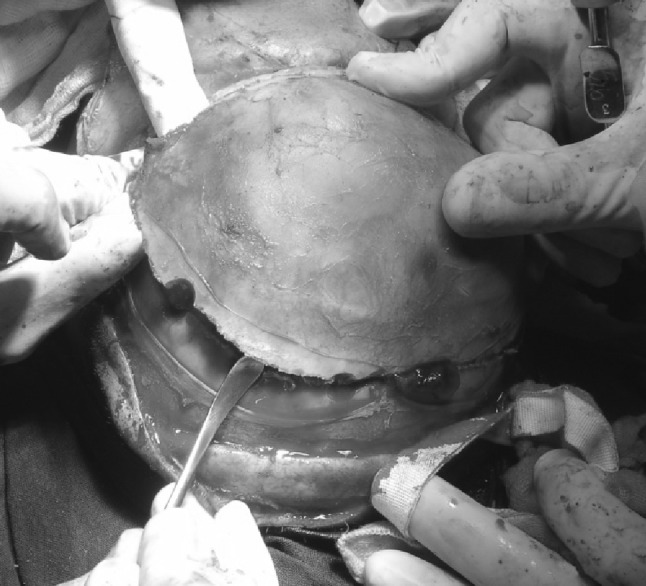
Bifrontal bone flap being raised
Fig. 4.

Bifrontal bone segment and Rt. supraorbital bar
Fig. 5.

Underlying brain and globe after removal of calvarial segment
Radial osteomies and “kerfing” were now performed on its endocranial side taking care to preserve the integrity of the pericranium (Fig. 6). “Kerfing” creates many microfractures within the bone so that appropriate remodelling can take place. The radial osteotomies would permit unrestricted expansion of the hitherto immobile right frontal bone (owing to the right coronal synostosis) allowing unrestricted calvarial growth commensurate with the growing brain underneath.
Fig. 6.

“Kerf cutting”/radial osteotomies of endocranial side of calvarial segment followed by fronto-orbital repositioning
Now in preparation for the osteotomy of the right orbital segment, the dura mater was dissected off the endocranial surface of the anterior orbital roof and squama of the temporal bone. The frontal lobe and anterior pole of the temporal lobe on the right were lifted epidurally from the bone. With the brain well protected by malleable retractors, the “tenon/tongue” portion, that is, the rectangular posterior extension of the supraorbital bar was cut using a reciprocating saw (0.6 mm blade thickness). The osteotomy was carried from posterior to anterior paralleling the zygomatic arch, then angled slightly inferiorly at the frontosphenoid suture and frontozygomatic suture regions. The anterior and lateral aspects of the frontal lobe were well protected. As the bone cut extended anteriorly across the roof of the orbit, the frontal lobe was retracted and the bulb or globe of the eye protected with a spatula to ensure that the eye capsule is not damaged by the tip of the saw. The lateral orbital wall osteotomy was completed with an oscillating saw (0.4 mm blade thickness). A thin 10 mm wide osteotome was then introduced intracranially, cutting across the frontosphenoid, frontozygomatic and sphenozygomatic sutures to complete the lateral orbital mobilization. The orbital roof cut now joined a vertical midline cut anterior to the foramen caecum and cribriform plate. The right supraorbital bar was now completely mobilized and removed (Fig. 5).
The unilateral right supraorbital bar was now replaced in an advanced position (Fig. 6), the extent of anterior osseous displacement being commensurate with and governed by the degree of deformity and orbital recession. We slightly over compensated the malformation and also slanted the orbital segment in a ventral direction to counter the raised and “swept back” supraorbital rim, thus creating a more aesthetic “take off angle” at the supraorbital ridge region. We relied on the classic “tongue in groove” pattern of the orbital bar. This pattern provides an interlocking between the posterior portion of the advanced fronto-spheno-parietal bone of the “tongue” portion of the supraorbital bar and the anterior portion of the remaining parietal bone forming the “groove”. This pattern breaks up what would be a long defect, into multiple smaller areas of cranial defects that are more likely to reossify spontaneously.
The supraorbital bar was fixed rigidly in place with resorbable plates and screws at the “tongue” region posteriorly and at the frontonasal region anteriorly. With the supraorbital bar fixed in the advanced position, the recontoured frontal bone segment was replaced, rotating and advancing it anteriorly to correct the forehead deformity. It was then secured rigidly to the advanced supraorbital bar below and to the cranial bones above using resorbable plates and screws (Fig. 7). The advancement resulted in a wide opening at the affected right coronal suture region without having to perform a craniectomy or the need for additional bone resection.
Fig. 7.

Rigid fixation using biodegradeable plates and screws
The dissected temporalis muscle was now reattached to the bone with absorbable sutures. The scalp flap was replaced and symmetry confirmed. A single 7 mm suction drain was placed underneath the flap (Fig. 8) and the wound closed in layers using interrupted 4-0 Vicryl sutures for the galea and staples for the skin closure. A light dressing and head bandage were then applied.
Fig. 8.

Closure following placement of suction drain
Following extubation, the child was transferred to the pediatric ICU for a 24 h observation period to allow close monitoring of the level of consciousness, and the respiratory, haemodynamic and neurological status. A short-term steroid (dexamethasone 2 mg/day) was administered to reduce the edema in the craniofacial, particularly the periorbital region, thus reducing the risk of excessive pressure on the globe with consequent discomfort. A 72 h antibiotic cover with cefotaxime was given. Post-operative 3-D CT scan was performed to evaluate the reconstruction, symmetry and advancement at the osteotomy sites.
Regular follow up was planned at 3 weeks (Fig. 1), 6 weeks, 3 months, 6 months and yearly thereafter.
Discussion
Treatment of Craniosynostosis consists of Craniofacial surgery for suture release, intracranial decomression and simultaneous cranial vault and upper orbital osteotomies with reshaping and advancement carried out at infancy.
The goals and objectives of surgery are
To release synostosis and to increase intracranial volume to allow the otherwise restricted brain to grow and expand unhindered in a normal manner. Normal brain volume triples in the first year of life, quadrules in the second year and reaches 80% of the adult volume by the 3rd year. Opening the stenosed cranial vault suture/s allows expansion of the cranial capsule to accommodate the enlarging brain.
To reshape the head and face to establish a normal or acceptable contour of the brow, forehead and skull. The forehead and orbits, in particular, are aesthetic units that cannot easily be disguised, so surgical correction of the disfigurement is essential to prevent cosmetic and sociopsychological problems.
The history of surgical approaches to craniosynostosis includes:-
“Strip Craniectomies” which were performed by Lannelongue in 1890 and Lane in 1892, the rationale being to simply release/resect the synostotic suture/s. Surgical release of the afflicted suture alone was supposed to allow the head to expand normally without the need for any cranial vault remodelling. However, results were unpredictable and the goal of spontaneous normalisation and self correction of the head and fronto orbital disfigurement was rarely achieved.
In 1967, Tessier [1] pioneered the concept of Craniotomy for suture release together with skull reshaping using an intracranial and extracranial approach, ingenious osteotomy sites, 360° periorbital dissection and autogenous bone grafting.
The same concept of suture release combined with skull reshaping carried out in infancy was pioneered by Hoffman and Mohr [3], Whitaker et al. [4] and Marchac and Renier [2].
Optimal timing for surgery has been debated over the years and depends upon the etiology, time of presentation and severity of the condition (Table 1).
Table 1.
Optimal timing for Craniofacial Surgery
| At 0−9 months | After 9 months | ||
|---|---|---|---|
| Indication Particularly advocated for severe syndromic multiple suture craniosynostosis in whom signs of increased Intracranial pressure are identified. | Indication Less severely affected and non-syndromic, single suture cranio synostosis, Late presentation cases. | ||
| Before 3 months (Very Early Surgery) | Between 3 and 9 months (Early Surgery) | Between 9 and 12 months (Moderately Delayed Surgery) | After 12 Months (Late Surgery) |
| Advantages: | Advantages: | Advantages: | Disadvantages: |
| 1. Less invasive | 1. Remodelling is easier as bone is very malleable | 1. Bones are better developed and easier to stabilise | 1. Deforming vectors of continually growing brain results in progression of deformity with increasing age |
| 2. Microscopic/Endoscopic procedures | 2. Advantage can be taken of rapid, propulsive brain growth to support the advanced/repositioned calvarial segments | 2. They still are soft and easy to work with | 2. Progressive deformity of cranial base leads to abnormal facial growth and asymmetry of maxilla and mandible |
| 3. Smaller incision | 3. High regenerative capacity and osteogenic potential of dura and periosteum | 3. There is less reliance on growth of operated bones and brain to maintain the initial surgical results | 3. Soft tissue envelope more constricted |
| 4. Less blood loss | 4. Bone defects heal rapidly | 4. Allowing the child to age enables other medical problems to be identified and managed effectively | 4. Bones more rigid, resulting in less than ideal correction |
| 5. Decreased operating time | 5. Less need for bone grafts | 5. Optimal age to allow for maximum correction and minimum morbidity | 5. Reduced osteogenic capability of dura and periosteum |
| 6. Shorter hospital stay | 6. Minimises compensatory deformational changes in skull and face shape | 6. More successful recontouring because of softer nature of bone and positive response to microfracturing craniofacial techniques as compared with the brittle bone of the older child | 6. Reduced reossification of osseous detect |
| 7. Early decompression relieves the raised Intracranial pressure and alleviates its symptoms | 7. More extensive bone grafting required | ||
| Disadvantage: Possibility of relapse due to malleable infant bones |
8. Cranial and orbital bones become brittle with increasing age | ||
Inadequate stabilization of skeletal segments can contribute to relapse, trauma to the brain from mobile bone segments and infection. Rigid internal fixation was employed using Biodegradable/Resorabable bone plates & screws made from polylactide polymers. Advantage of these over the traditional metal plate and screw fixation is that with the latter, intracranial implant migration can occur in the growing children as the result of cranial remodelling (endocranial bone resorption and exocranial bone deposition) [6, 7]. Also, the long term effect of implanted metals is not known. On the other hand, resorbable plates and screws provide rigid fixation for the initial period of 2−3 months rigid support for a further period of 6−9 months and then biodegrade at 9−12 months after having served their purpose [8, 9]. We achieved a gratifying aesthetic outcome and perfect symmetry using this technique.
There were no complications like wound infection or dehiscence, CSF leak, bone loss from resorption, damage to orbital contents or brain, recurrence of the dysmorphology or residual deformities or asymmetries of the orbital region or forehead.
A perfect cosmetic result was achieved by providing the necessary surgical correction of the deformity, in the one year old child with Anterior plagiocephaly using this “bilateral frontal-unilateral orbital advancement“technique. The aesthetic outcome was gratifying with restoration of perfect symmetry to the deformed upper third of the child’s face.
References
- 1.Tessier P. Osteotomies totales de la face: Syndrome de Crouzon, syndrome d’ Apert—oxcephalies, scaphocephalies, turricephalies. Ann Chir Plast. 1967;12:273. [PubMed] [Google Scholar]
- 2.Marchac D, Renier D. “Le Front flottant”: traitement precocedes facio—Craniostenoses. Ann Chir Plast. 1979;24:121. [PubMed] [Google Scholar]
- 3.Mohr G, Hoffman HJ. Lateral canthal advancement of the cranio-orbital margin: a new corrective technique in the treatment of coronal synstosis. J Neurosurg. 1976;45:376. doi: 10.3171/jns.1976.45.4.0376. [DOI] [PubMed] [Google Scholar]
- 4.Whitaker LA, Schut L, Kerr LP. Early surgery for isolated craniofacial dysostosis. Plast Reconstr Surg. 1977;60:575. doi: 10.1097/00006534-197711000-00079. [DOI] [PubMed] [Google Scholar]
- 5.Posnick JC. Unilateral coronal synostosis (anterior plagiocephaly): current clinical perspectives. Ann Plast Surg. 1996;36:430–447. doi: 10.1097/00000637-199604000-00021. [DOI] [PubMed] [Google Scholar]
- 6.Surpure SJ, Smith KS, Sullivan SM, et al. The use of resorbable plating system for treatment of craniosynostosis. J Oral Maxillofac Surg. 2001;59:1271. doi: 10.1053/joms.2001.27497. [DOI] [PubMed] [Google Scholar]
- 7.Acosta HL, Stelnicki EJ, Rodriguez L, et al. Use of absorbable poly (d, o) lactic acid plates in cranial vault remodelling: presentation of first case and lessons learned about its use. Cleft Palate Craniofac J. 2005;42:333. doi: 10.1597/03-071.1. [DOI] [PubMed] [Google Scholar]
- 8.Jethani J, Dagar A, Vijayalakshmi P, et al. Anterior plagiocephaly with contralateral superior oblique overaction. Indian J Ophthalmol. 2008;56(6):504–507. doi: 10.4103/0301-4738.43374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kabbani H, Raghuveer TS. Coronosynostosis. Am Fam Phys. 2004;690:2863–2870. [PubMed] [Google Scholar]
- 10.Anantheswar YN, Venkatramana NK. Pediatric craniofacial surgery for craniosynostosis: our experience and current concepts. J Paediatr Neurosci. 2009;4(2):86–99. doi: 10.4103/1817-1745.57327. [DOI] [PMC free article] [PubMed] [Google Scholar]



