Abstract
Objective
To describe the epidemiology of emergency department (ED) visits for attempted suicide and self-inflicted injury over a 16-year period.
Method
Data were obtained from the National Hospital Ambulatory Medical Care Survey including all visits for attempted suicide and self-inflicted injury (E950–E959) during 1993–2008.
Results
Over the 16-year period, there was an average of 420,000 annual ED visits for attempted suicide and self-inflicted injury (1.50 [95% confidence interval (CI) 1.33–1.67] visits per 1,000 US population) and the average annual number for these ED visits more than doubled from 244,000 in 1993–1996 to 538,000 in 2005–2008. During the same timeframe, ED visits for these injuries per 1,000 US population almost doubled for males (0.84 to 1.62), females (1.04 to 1.96), whites (0.94 to 1.82), and blacks (1.14 to 2.10). Visits were most common among ages 15–19 and the number of visits coded as urgent/emergent decreased.
Conclusions
ED visit volume for attempted suicide and self-inflicted injury has increased over the past two decades in all major demographic groups. Awareness of these longitudinal trends may assist efforts to increase research on suicide prevention. In addition, this information may be used to inform current suicide and self-injury related ED interventions and treatment programs.
Keywords: Suicide, Emergency Departments, Public Health
Introduction
Current global estimates indicate that around one million people die by suicide each year, accounting for more than half of all violent deaths in the world.1 Suicide attempts are approximately 20 times more frequent than completed suicides.1 Attempts are concerning for many reasons, particularly due to their strong link to future attempts and suicide completion.2 In a review of 90 studies on deliberate self-harm, one year following the act an overall average of 16% repeated the self-harm behavior and approximately 2% died by suicide.3 Gairin et al.4 found that within one year before their deaths, 39% (n=85) of 219 suicide victims visited the emergency department (ED) at least once. In addition, one year before their deaths, 39% of these 85 suicide victims had an ED visit that was classified as nonfatal self-harm. However, the frequency of ED visits should be interpreted cautiously because these visits may simply reflect the overall annual frequency of ED visits in the general population, which from 1993–2008 was 38%.5 Since many suicide attempt and self-harm patients are treated in EDs, temporal trends in this population could help inform research and clinical policy on suicide prevention.
Using data from the National Hospital Ambulatory Medical Care Survey (NHAMCS), researchers have examined trends in ED visits for suicide attempts and self injury in the USA.6,7 Using NHAMCS data from 1997–2001, we found that ED visits for attempted suicide and intentional self-injury were more common for females, blacks, and those under the age of 20.6 A subsequent analysis of NHAMCS data from 1992–2001 found that ED visit rates for this population doubled over the 10-year timeframe.7 In the present study, we included 16-years of nationally representative data from 1993 to 2008 to examine subsequent trends in ED visits for attempted suicide and self-inflicted injury. We were not able to differentiate between suicidal and non-suicidal self-inflicted injury, so our rates include both types of self-inflicted injury. We compared groupings of 4-year timeframes (e.g., 1993–1996 vs. 2005–2008) to test our hypothesis that the frequency of ED visits for attempted suicide and self-inflicted injury has increased in all major demographic groups.
Methods
Setting, study design, and participant selection
Data from the NHAMCS ED database (1993–2008) were used to determine national estimates of ED visits for attempted suicide and self-injury. NHAMCS is a 4-stage probability sample of visits to the emergency and outpatient departments of non-institutional general and short stay hospitals, not including federal, military, or Veterans Affairs hospitals, in the United States.5 The survey is conducted annually. For each year of the study, patient visits were systematically selected over a randomly assigned 4-week period. The number of participating EDs differed each year (e.g., 395 in 1993 and 357 in 2008). The survey was conducted using a multistage sampling design that begins with geographically defined areas (primary sampling units (PSUs)) that are then stratified by socioeconomic and demographic variables. Individual visits were selected using a series of step-wise probability samples obtained by selecting a given PSU, a hospital within the PSU, an ED within the hospital, and then an individual patient encounter within that ED.8 Completed data collection forms were sent to the National Center for Health Statistics where they were coded using the International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM). National estimates were obtained through use of assigned patient visit weights and were rounded to the nearest thousand. Multiple imputation was used by NHAMCS to account for the high percentage of missing data for race and immediacy with which patient should be seen. Compared to other imputation methods, the process of multiple imputation accounts for a wider range of possible outcomes when imputing the missing data and it allows users to analyze the data using any standard statistical package. Although there are still limitations, multiple imputation is recognized as a preferred method for dealing with missing values in large datasets.9 Our analysis was exempted from human subjects review by the Partners Healthcare Human Research Committee.
Measurements or key outcome measures
Primary outcome measure
ED visits for attempted suicide and self-inflicted injury were defined by including visits with an ICD-9-CM code of E950 to E959 in the primary diagnosis field. These visits include suicide and self-inflicted injury due to poisoning, hanging, drowning, firearms, cutting/piercing, jumping, and other unspecified means.
Demographics
In addition to the estimated absolute number of ED visits, we calculated ED visit rates using mid-year age, sex, and race-specific civilian population estimates for 1993 to 2008 from the US Census Bureau10; all rates were reported per 1,000 individuals per year for the US population. The attempted suicide and self-inflicted injury ED visit rates were calculated for each individual year as well as for four 4-year periods (1993–1996, 1997–2000, 2001–2004, and 2005–2008). We then analyzed ED visit rates by age, sex, race (white, black, other), region (Northeast, Midwest, South and West), and metropolitan statistical area (MSA) status of the hospital. Ethnicity (Hispanic/non-Hispanic) was not analyzed by year, as it was not well reported in the NHAMCS database.5
ED visit characteristics
Visits were analyzed by season (January-March, April-June, July-September, October-December). We also examined visit urgency as determined at triage, with visits coded as “urgent/emergent” if patient should be seen in “<15 minutes” or “15–60 minutes,” and as “non-urgent” if recorded as should be seen in “>1–2 hours.” Two aspects of ED management were examined: performance of a mental status exam and screening for alcohol by blood alcohol concentration testing. Finally, we examined ED disposition: admitted, transferred, discharged home with referral, or other (e.g., left before being seen, discharged with no follow-up planned).
Additional self-harm and mental health indicators
We also examined method of injury and comorbid conditions, such as mental disorders (ICD-9-CM codes 290 to 319), alcohol abuse (ICD-9-CM codes 291, 303 or 305), and depressive disorders (ICD-9-CM code 311).
Data Analysis
We performed all analyses using STATA 11.2 (StataCorp, College Station, TX). The primary analysis was a descriptive summary of ED visits for attempted suicide and self-inflicted injury. Particular attention was paid to the percentage of patients who visited the ED for suicide attempt or self-inflicted injury, as well as characteristics of the visit (e.g., method of injury, day of the week). Confidence intervals for ED visits were calculated using the relative standard error of the estimate. All proportions were reported with 95% confidence intervals (95%CIs).
All estimates presented are based on at least 30 raw cases with a relative standard error of the estimate less than 30%. Trend analyses were conducted using STATA’s nptrend (a nonparametric test for trends that is an extension of the Wilcoxon rank-sum test) and regression analyses. A two-tailed P<.05 was considered statistically significant.
Results
The estimated number of ED visits attributable to attempted suicide and self-inflicted injury from 1993–2008 was 6,720,000, or an average of 420,000 visits per year. These visits accounted for 0.4% of the total 1.7 billion ED visits from 1993–2008. Overall, the estimated annual rate of ED visits attributable to attempted suicide and self-inflicted injury was 1.50 (95%CI 1.33 – 1.67) visits per 1,000 US population. Item nonresponse rates are generally 5% or less for NHAMCS data items. In the NHAMCS-ED file, five items were imputed: birth year (1.0%), sex (0.7%), ethnicity (23.8%), race (15.3%), and immediacy with which patient should be seen (3.0%).
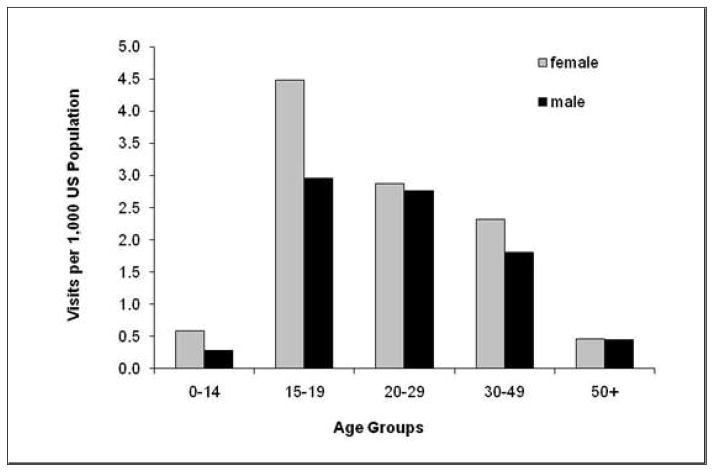
An examination of demographic characteristics revealed that ED visits for attempted suicide and self-inflicted injury varied by age, sex, and race (Table 1). The mean patient age was 31, with the highest visit rate per 1,000 US population among patients aged 15–19 (3.70; 95%CI, 3.11–4.30). We further examined the 15–19 year old age group by looking at sex differences by age for visits related to suicide and self-inflicted injury. We found females (4.49; 95%CI, 3.60–5.37) had a significantly higher visit rate (per 1,000 US population) than their male counterparts (2.96; 95%CI, 2.37– 3.54) (Figure 1). Overall, blacks had a slightly higher visit rate per 1,000 US population (1.94; 95%CI, 1.61–2.27) when compared to whites (1.49; 95%CI, 1.31–1.67) (See Table 1).
Table 1.
Distribution of Suicide Attempt and Self-Inflicted Injury Emergency Department Visits in The U.S. by Patient and Hospital Characterisitcs; 1993–2008.
| n | # Visits (thousands) | 95% Confidence Interval | Rate per 1,000 US Population | 95% Confidence Interval | Rate per 1,000 ED Visits | 95% Confidence Interval | ||||
|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||||
| Overall | 2,080 | 6,720 | 5,967 | 7,473 | 1.5 | 1.3 | 1.7 | 4.0 | 3.7 | 4.3 |
| Age Group (years) | ||||||||||
| <15 | 114 | 407 | 305 | 510 | 0.4 | 0.3 | 0.5 | 1.1 | 0.9 | 1.4 |
| 15–19 | 381 | 1,183 | 993 | 1,374 | 3.7 | 3.1 | 4.3 | 9.6 | 8.3 | 10.9 |
| 20–29 | 560 | 1,720 | 1,445 | 1,996 | 2.8 | 2.3 | 3.2 | 6.0 | 5.2 | 6.8 |
| 30–49 | 822 | 2,760 | 2,409 | 3,110 | 2.0 | 1.8 | 2.3 | 5.9 | 5.3 | 6.5 |
| >50 | 203 | 649 | 514 | 785 | 0.5 | 0.4 | 0.6 | 1.4 | 1.2 | 1.7 |
| Sex | ||||||||||
| Female | 1,162 | 3,760 | 3,292 | 4,228 | 1.6 | 1.4 | 1.9 | 4.2 | 3.8 | 4.5 |
| Male | 918 | 2,960 | 2,588 | 3,331 | 1.4 | 1.2 | 1.5 | 3.7 | 3.4 | 4.1 |
| Race | ||||||||||
| White | 1,617 | 5,447 | 4,792 | 6,102 | 1.5 | 1.3 | 1.7 | 4.3 | 3.9 | 4.6 |
| Black | 385 | 1,104 | 918 | 1,290 | 1.9 | 1.6 | 2.3 | 3.0 | 2.6 | 3.4 |
| Other | 78 | 169 | 107 | 230 | 0.6 | 0.4 | 0.9 | 3.3 | 2.2 | 4.5 |
| U.S. Region | ||||||||||
| Northeast | 513 | 1,147 | 891 | 1,402 | 1.4 | 1.1 | 1.7 | 3.5 | 3.0 | 4.0 |
| Midwest | 398 | 1,474 | 1,210 | 1,737 | 1.4 | 1.2 | 1.7 | 3.5 | 3.1 | 4.0 |
| South | 627 | 2,297 | 1,849 | 2,745 | 1.4 | 1.2 | 1.7 | 3.6 | 3.2 | 4.0 |
| West | 542 | 1,802 | 1,320 | 2,284 | 1.8 | 1.3 | 2.3 | 5.9 | 4.9 | 6.8 |
| MSA | ||||||||||
| Metro | 1,843 | 5,569 | 4,842 | 6,295 | 1.5 | 1.3 | 1.7 | 4.1 | 3.8 | 4.4 |
| Non-metro | 237 | 1,152 | 775 | 1,528 | 1.4 | 0.9 | 1.8 | 3.5 | 2.9 | 4.1 |
Figure 1.
Emergency department visits for attempted suicide and self–inflicted injury, by age and sex (1993–2008)
Visit rates did not differ significantly by month (P=0.20) or by day of week (P=0.87). An analysis of ED arrival time for all ED visits, regardless of complaint, indicated that most patients arrived in the ED between 10 AM and 10 PM. However, visits for attempted suicide and self-inflicted injury were more frequent from 4 PM to 12 AM.
Most suicide attempt and self-inflicted injury visits were coded as urgent/emergent (71%; 95%CI, 68–75); with 65% (95%CI, 63–66) of these visits classified as “should be seen in 15–60 minutes”. This 65% differs from the typical ED visit where 42% of visits were classified as should be seen in 15–60 minutes (95%CI, 41–44).
Poisoning was the most common method of attempted suicide and self-inflicted injury seen in the ED (67%), followed by self-inflicted injury by cutting or piercing instruments (21%). To test whether self-poisoning was predominately reported by women11 in an ED population, we examined sex differences among suicide attempts and self-inflicted injury visits due to poisoning. Compared to men, women constituted a larger percentage of the poisoning cases (73% vs. 59%, P<0.001). A sub-analysis of poisoning cases revealed that poisoning by unspecified drugs or medicinal substances accounted for the highest number of cases (27%; 95%CI, 23–31), followed by tranquilizers and other psychotropic agents (25%; 95%CI, 21–28), and then analgesics, antipyretics, and antirheumatics (21%; 95%CI, 18–24). Hanging and firearm-related visits were rare (Table 2).
Table 2.
Method of Injury, Comorbid Conditions, and Emergency Department Course for Suicide Attempt and Self-inflicted Injury Emergency Department Visits (1993–2008)
| Percentage (%) | 95% CI | ||
|---|---|---|---|
|
|
|||
| Method of Injury | |||
| Poisoning (overall) | 67 | 64 | 70 |
| Males | 59 | 54 | 63 |
| Females | 73 | 69 | 77 |
| Cutting/Piercing instruments | 21 | 18 | 23 |
| Hanging | 2 | 1.1 | 2.4 |
| Firearms* | <1 | nc | nc |
| Comorbid Conditions | |||
| Mental disorders | 54 | 51 | 58 |
| Depressive disorders | 34 | 30 | 38 |
| Alcohol abuse | 22 | 19 | 25 |
| ED Evaluation | |||
| Mental status exam** | 44 | 40 | 48 |
| Blood alcohol concentration*** | 27 | 24 | 29 |
| Disposition | |||
| Hospital admission | 34 | 31 | 37 |
| Transfer to another facility | 27 | 24 | 29 |
| Referred to other physician/clinic | 11 | 9 | 13 |
| Other (e.g., left before being seen, dead on arrival) | 27 | 24 | 30 |
nc - not calculable due to sample <30 or relative standard error >30%
Data available from 1995–2004
Data available from 1995–2008
Of all attempted suicide and self-inflicted injury visits, more than half (54%) were coded for mental disorders (ICD-9 290–319) with a depressive disorder constituting 34% of all attempted suicide and self-inflicted injury visits with mental disorders. A significant percentage of the visits were coded for alcohol abuse: 12% of all attempted suicide and self-inflicted injury visits, and 22% of all attempted suicide and self-inflicted injury visits with mental disorders. Of the total ED visits for attempted suicide and self-inflicted injury, 44% had documentation of a mental status exam, and 27% received testing for blood alcohol concentration (Table 2).
In the current study, data were available on mental status exams from 1995–2004. Over the 10-year timeframe, 44% of visits for attempted suicide and self-injury had a documented mental status exam. However, an examination of individual years showed that rates of mental status exams for attempted suicide and self-inflicted injury visits decreased from 57% in 1995 to 38% in 2004. In addition, only 27% of the visits for attempted suicide and self-inflicted injury had documentation of blood alcohol concentration testing. Of those who presented with alcohol abuse, only 35% had a blood alcohol concentration test documented.
Approximately one-third (34%) of ED visits for attempted suicide and self-inflicted injury resulted in direct hospitalization (Table 2). Approximately 11% were referred to another provider or setting following discharge home (e.g., social services), while 27% (95%CI, 24–29) were transferred to another facility.
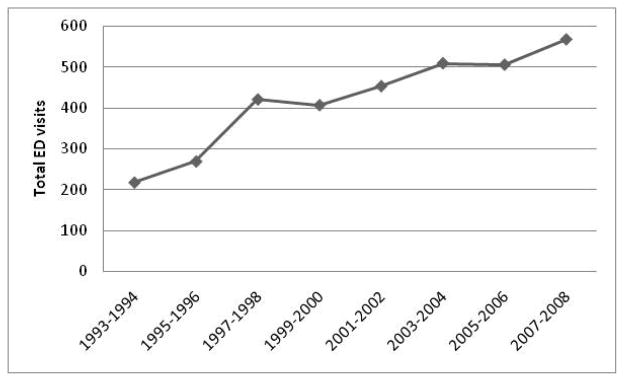
With regard to temporal trends, rates for attempted suicide and self-inflicted injury increased significantly over the 16-year period from 1993 to 2008 (P for trend <0.001). The average annual number of ED visits for suicide attempt and self-inflicted injury more than doubled from 244,000 between 1993–1996 to 538,000 between 2005–2008 (Figure 2), a ratio of 2.21 (95%CI; 2.02–2.40). By comparison, overall ED visits increased from 371 million between 1993–1996 to 475 million between 2005–2008, a ratio of 1.28 (95%CI; 1.17–1.40).
Figure 2.
Emergency department visits for attempted suicide and self-inflicted injury, by year
This increase in self-harm visit rates per 1,000 US population was seen in all major demographic groups. Comparing 1993–1996 to 2005–2008, rates nearly doubled for both males (0.84 to 1.62) and females (1.04 to 1.96). Similar increases were noted for patients aged 15–19 (2.57 to 4.53), 30–49 (1.29 to 2.49), and those over 50 (0.11 to 0.90). Likewise, increases were observed for whites (0.94 to 1.82) and blacks (1.14 to 2.10). By contrast, the rate of suicide attempt and self-injury visits coded as urgent/emergent decreased from 0.95 (95%CI, 0.91–0.99) in 1993–1996 to 0.70 (95%CI, 0.63–0.77) in 2005–2008 (P=0.045).
Over the 16-year period, there were no significant differences in the rates for methods of attempted suicide and self-inflicted injury seen in the ED. The only statistically significant change was an increase in suicide attempt and self-injury visits with documentation of alcohol abuse from 1.31 in 1993–1996 (95%CI, 1.19–1.43) to 2.09 in 2005–2008 (95%CI, 1.91–2.28) (P=0.005) (Table 3). ED disposition did not change significantly over the 16–year period, except for the “other” category, which decreased from a rate of 58 per 1,000 ED visits (95%CI, 56–60) in 1993–1996 to 44 per 1,000 ED visits (95%CI, 41–46) in 2005–2008 (P=0.004).
Table 3.
Method of Injury, Comorbid Conditions, and Emergency Department Course for Suicide Attempt and Self-inflicted Injury Emergency Department Visits (1993–2008)
| Year | n | Visits per 1,000 | 95%CI | Rate per 1,000 ED visits | 95%CI | |||
|---|---|---|---|---|---|---|---|---|
| Method of Injury | ||||||||
| Poisoning | 1993–1996 | 166 | 587 | 439 | 736 | 0.16 | 0.12 | 0.19 |
| 1997–2000 | 271 | 1121 | 877 | 1366 | 0.28 | 0.23 | 0.32 | |
| 2001–2004 | 455 | 1352 | 1111 | 1593 | 0.31 | 0.26 | 0.35 | |
| 2005–2008 | 425 | 1421 | 1101 | 1742 | 0.30 | 0.25 | 0.35 | |
| P=0.29 | P=0.29 | |||||||
| Cutting | 1993–1996 | 69 | 247 | 171 | 323 | 0.07 | 0.05 | 0.08 |
| 1997–2000 | 87 | 346 | 244 | 447 | 0.09 | 0.06 | 0.11 | |
| 2001–2004 | 140 | 362 | 270 | 454 | 0.08 | 0.06 | 0.10 | |
| 2005–2008 | 135 | 434 | 311 | 556 | 0.09 | 0.07 | 0.11 | |
| P=0.21 | P=0.20 | |||||||
| Hanging* | 1993–1996 | 9 | 25 | nc | nc | 0.007 | nc | nc |
| 1997–2000 | 4 | 15 | nc | nc | 0.004 | nc | nc | |
| 2001–2004 | 12 | 29 | nc | nc | 0.007 | nc | nc | |
| 2005–2008 | 22 | 50 | nc | nc | 0.011 | nc | nc | |
| P=0.59 | P=0.61 | |||||||
| Firearms* | 1993–1996 | 6 | 31 | nc | nc | 0.008 | nc | nc |
| 1997–2000 | 0 | 0 | nc | nc | 0 | nc | nc | |
| 2001–2004 | 3 | 8 | nc | nc | 0.002 | nc | nc | |
| 2005–2008 | 3 | 13 | nc | nc | 0.003 | nc | nc | |
| P=0.28 | P=0.20 | |||||||
| Comorbid conditions | ||||||||
| Mental disorders | 1993–1996 | 180 | 508 | 381 | 635 | 4.01 | 3.78 | 4.25 |
| 1997–2000 | 232 | 883 | 697 | 1069 | 4.62 | 4.35 | 4.89 | |
| 2001–2004 | 407 | 1059 | 871 | 1245 | 5.24 | 5.00 | 5.48 | |
| 2005–2008 | 403 | 1194 | 893 | 1495 | 5.61 | 5.33 | 5.89 | |
| P=0.45 | P=0.45 | |||||||
| Depression | 1993–1996 | 47 | 125 | 79 | 172 | 0.45 | 0.40 | 0.51 |
| 1997–2000 | 80 | 306 | 208 | 405 | 0.57 | 0.50 | 0.65 | |
| 2001–2004 | 134 | 366 | 271 | 460 | 0.74 | 0.67 | 0.81 | |
| 2005–2008 | 140 | 442 | 292 | 593 | 0.74 | 0.66 | 0.81 | |
| P=0.12 | P=0.13 | |||||||
| Alcohol abuse | 1993–1996 | 32 | 89 | 42 | 137 | 1.31 | 1.19 | 1.43 |
| 1997–2000 | 41 | 127 | 67 | 188 | 1.48 | 1.34 | 1.62 | |
| 2001–2004 | 105 | 267 | 190 | 343 | 1.75 | 1.62 | 1.87 | |
| 2005–2008 | 122 | 314 | 209 | 420 | 2.09 | 1.91 | 2.28 | |
| P=0.008 | P=0.005 | |||||||
| ED evaluation | ||||||||
| Mental status exam** | 1995–1996 | 84 | 292 | 199 | 385 | 13.3 | 11.3 | 15.4 |
| 1997–2000 | 187 | 748 | 568 | 929 | 13.4 | 11.8 | 15.0 | |
| 2001–2004 | 326 | 787 | 638 | 936 | 9.8 | 8.2 | 11.5 | |
| 2005–2008 | - | - | - | - | - | - | - | |
| P=0.07 | P=0.07 | |||||||
| Blood alcohol concentration*** | 1995–1996 | 35 | 140 | 67 | 212 | 1.67 | 1.44 | 1.89 |
| 1997–2000 | 110 | 435 | 323 | 561 | 1.52 | 1.37 | 1.66 | |
| 2001–2004 | 156 | 489 | 367 | 609 | 1.45 | 1.30 | 1.59 | |
| 2005–2008 | 179 | 616 | 461 | 773 | 1.82 | 1.62 | 2.03 | |
| P=0.82 | P=0.82 | |||||||
| Disposition | ||||||||
| Hospital admission | 1993–1996 | 117 | 374 | 261 | 487 | 12.6 | 11.9 | 13.3 |
| 1997–2000 | 136 | 546 | 403 | 687 | 13.0 | 12.4 | 13.6 | |
| 2001–2004 | 237 | 695 | 539 | 852 | 13.4 | 12.7 | 14.1 | |
| 2005–2008 | 227 | 675 | 500 | 852 | 14.0 | 13.0 | 14.9 | |
| P=0.104 | P=0.11 | |||||||
| Transfer to another facility | 1993–1996 | 71 | 243 | 174 | 313 | 1.73 | 1.54 | 1.93 |
| 1997–2000 | 116 | 485 | 350 | 621 | 1.77 | 1.55 | 1.99 | |
| 2001–2004 | 179 | 494 | 375 | 612 | 1.84 | 1.68 | 2.00 | |
| 2005–2008 | 167 | 585 | 431 | 740 | 1.74 | 1.53 | 1.95 | |
| P=0.061 | P=0.07 | |||||||
| Referred to other physician/clinic | 1993–1996 | 44 | 152 | 94 | 210 | 27.4 | 25.6 | 29.1 |
| 1997–2000 | 75 | 294 | 188 | 401 | 33.5 | 31.6 | 35.3 | |
| 2001–2004 | 90 | 236 | 172 | 300 | 24.8 | 23.0 | 26.5 | |
| 2005–2008 | 138 | 465 | 325 | 605 | 40.1 | 37.8 | 42.4 | |
| P=0.150 | P=0.16 | |||||||
| Other (e.g., left before being seen, dead on arrival) | 1993–1996 | 63 | 208 | 137 | 279 | 58.3 | 56.3 | 60.2 |
| 1997–2000 | 78 | 325 | 224 | 425 | 51.7 | 49.9 | 53.6 | |
| 2001–2004 | 176 | 502 | 348 | 656 | 60.0 | 58.2 | 61.9 | |
| 2005–2008 | 280 | 390 | 274 | 506 | 44.2 | 41.9 | 46.4 | |
| P=0.006 | P=0.004 | |||||||
P values denote P for trend
nc - not calculable due to sample <30 or relative standard error >30%
Data available from 1995–2004
Data available from 1995–2008
Discussion
The current findings indicate that attempted suicide and self-inflicted injury account for an annual average of 420,000 ED visits and that ED visits for suicide attempt and self-injury varied by age, sex, and race. Comparison of visits by 4-year groupings showed that US population rates for suicide attempt and self-injury visits doubled from 1993–1996 to 2005–2008. Similar trends were observed for rates among males and females, as well as whites and blacks. We also noted a significant increase in suicide attempt and self-injury visits documenting alcohol abuse. Although there was no difference in the rates for methods of self-inflicted injury, there was a decrease from 1993–1996 to 2005–2008 in the number of suicide attempt and self-injury visits coded as urgent/emergent. Each of these findings is discussed in further detail in the following section.
Similar to earlier analyses by our group and others6,7, the current national study found that suicide attempt and self-inflicted injury ED visits were highest among youth between the ages of 15 and 19, a finding consistent with evidence that suicide is the third leading cause of death among 15–24 year olds.12 Notably, this age group is at higher risk than other age groups for non-suicidal self injury. In a recent study, half of the adolescents presenting to emergency crisis services had self-harmed within the previous 24 hours, with most (91%) classified as non-suicidal self-injury only.13 Another consideration for the high rates of suicide attempts and self-inflicted injury visits for this age group is the Black-box warning that was enacted in 2004.14 Recent research indicates that there has been a significant decrease in prescribing antidepressants to children and adolescents following the release of the Black-box warning, resulting in rising rates of reported suicidal thoughts and behaviors for this age group.15 This may be contributing to the rising ED visit rates for suicide attempts and self-inflicted injury for 15–19 year olds in our study. Where the ED may be the first point of contact for these adolescents16, diagnosing and providing effective treatment plans before they commit suicide is imperative.6, 17
Our study also confirmed previous findings that ED visits for suicide attempt and self-inflicted injury were higher for females than for males.6 For example, ED visit rates for females in the 15–19 year age group were almost double those of their male counterparts. Research indicates that women attempt suicide 2 to 3 times more frequently than men18, while men are 4 times more likely to complete suicide. Women tend to use less lethal means such as poisoning, which may be one reason why they present to the ED more frequently following an attempt. However, the overall sex difference in population rates was only marginally significant (P=0.06). This may be because when it comes to medically serious suicide attempts, men and women do not differ significantly.19,20 Regardless, ED visits rates continue to rise for both sexes, suggesting that improved treatments and interventions are needed for both sexes.
Contrary to findings that whites attempt suicide and self-harm more frequently than blacks21, we found blacks had higher population rates of ED visits for suicide attempts and self-inflicted injury when compared to whites. Recent research supports this trend, suggesting that this difference may be due to a significant rise in young African American male suicide.22 This increase has been attributed to the large percentage of black individuals who do not see depression as a mental illness.23 Other research indicates that younger blacks have increased access to lethal methods24, have more psychiatric disorders, and may hold accepting attitudes toward suicide.25,26 Educational status also seems to play a role as blacks with less than a high school education are more likely to attempt suicide.27
Regardless of race, 90% of people who die by suicide have a diagnosable psychiatric disorder at the time of their death, most often unrecognized or untreated depression.28 The NHAMCS data, which undoubtedly underestimate true psychiatric comorbidity, found that 54% of ED visits for attempted suicide and self-inflicted injury also had mental disorders, especially depression. In our previous research, we recommended that patients who present to the ED with attempted suicide and self-inflicted injury as well as a mental illness should be evaluated by a psychiatrist or psychologist with a mental status exam.6 However, findings from the current research show that the rates of mental status exams continued to decrease from 1993–2004. Although Doshi et al.6 state that failure to document this fundamental aspect of the emergency evaluation requires corrective action, these data suggest no improvement in this possible quality measure. This may be because many aspects of mental health are not integrated into emergency medicine departments and procedures.29
Although underreporting of alcohol abuse is common30, we found that about 22% of the ED visits for attempted suicide and self-inflicted injury also were coded for alcohol abuse. From 1993–2008 there has been a significant increase in the ED visit rate for suicide attempt and self-injury visits with documented alcohol abuse. Previous studies have documented a positive association between alcohol use and self-injury. One study found that suicide attempt rates in the ED were significantly higher for individuals reporting alcohol use at least 6 hours before presentation for a suicide attempt.31 Alcohol misuse is an important risk factor for deliberate self-harm.32 Almost half of those presenting to services after an episode of deliberate self-harm have consumed alcohol in the period prior to the act.32 Once again, earlier research has indicated that alcohol screenings were unacceptably low for this ED population6, yet there has been little change in the rate of alcohol screenings from 1993 to 2008. The conflicting evidence on the effectiveness of alcohol screenings and interventions in EDs, as well as the unreliability of self-reported alcohol use may be possible explanations for low screening rates.33
Finally, ED dispositions were examined to determine how the patients were managed following stabilization in the ED. Approximately one-third of the visits were admitted to the hospital (34%) and almost another third (27%) were transferred to another facility. There were no significant changes in ED disposition over the 16-year timeframe. However, there was a noticeable decrease in the ED visit rate for visits categorized as urgent/emergent. Often serious suicide attempts are the only ones admitted. This means that non-hospitalized suicide attempt patients may go untreated, in turn, increasing their risk for future suicidal behavior. We were not able to examine what other factors (e.g., trends in ED consultation) may be affecting these changes. Future studies should investigate additional factors that may be associated with hospitalization for suicide attempt and self-inflicted injury visits to guide the design and implementation of improved suicide screening and related interventions in the ED.
Limitations
One potential limitation is data for this study were obtained via chart review. However, NHAMCS represents the most comprehensive national data set on ED visits, and comparable studies on this topic (e.g., the National Electronic Injury Surveillance System-All Injury Program (NEISS-AIP)) also use chart review as their primary methodology. 6,7,21 In addition, the data on race and ethnicity in the NHAMCS database has a high non-response rate (e.g., 15% missing race data in 2008; 24% missing ethnicity data in 2008). However, the method used to impute race and ethnicity was recently refined by NHAMCS5 so that the race and ethnicity assignments were based on diagnosis and patient’s zip code or state/county of residence. When a race or ethnicity value could not be assigned using patient locality, then the new approach attempted to impute within the same facility. If that was not possible, then imputation was based on diagnosis, hospital, clinic, and immediacy, or as a last resort, a randomly selected record. This method of multiple imputation helped reduce the likelihood that the imputed values are misclassified.
Another potential limitation is that we examined ED visits only, which may limit the generalizability of findings to other clinical settings. Yet, for the purposes of this study, we were interested in providing an epidemiological foundation for suicide attempt and self-inflicted injury visits to the ED. Therefore, the data were appropriate and do provide information directly relevant to the clinical population of interest. However, findings on screening prevalence (e.g., mental health, alcohol use) should be interpreted cautiously as we are unable to determine whether the low rates of screening are due to poor screening practices or improper documentation. We suspect that both are problematic.
Lastly, we were unable to distinguish between self-injury that was suicidal or non-suicidal in nature. Thus, we cannot say with certainty that ED visits for suicidal behavior are increasing. The highest rate of nonfatal self-harm behaviors occurs during adolescence, particularly among youth who present with mental health issues. Self-inflicted injuries that require an ED visit, whether suicidal or non-suicidal, are a cause for concern. As suicide attempts and self-injury remain predominant health risks among adolescents, future studies should focus on distinguishing features of self-harming adolescents from those who are at risk for suicidal behaviors.34
Conclusions
Attempted suicide is one of the strongest clinical predictors of subsequent suicide and occurs up to 20 times more frequently than completed suicide.1 As a result, suicide prevention has become a central focus of mental health policy. To improve current treatment and intervention strategies for those presenting with suicide attempt and self-injury in the ED, it is necessary to have a better understanding of the types of patients that present to the ED with these complaints. We found that ED visits for attempted suicide and self-inflicted injury were especially common among adolescents/young adults, females, and blacks. As previously discussed, although these groups may not have the highest rates of ED visits, they represent a higher proportion of visits related to suicide attempt and self-inflicted injury. In addition, attention should be directed at ensuring that proper screening is provided to patients presenting with mental disorders and alcohol use.
As ED staff are often the first points of primary care contact for these patients16, they need to be able to recognize factors that could increase the risk for attempted and completed suicide.6 According to the World Health Organization1, adequate prevention and treatment of depression and alcohol and substance abuse can reduce suicide rates, as well as follow-up contact with those who have attempted suicide. Only a few countries have included prevention of suicide among their priorities.1 Increasing awareness of epidemiological trends related to suicide attempts and self-inflicted injury is an early and important step toward developing effective strategies for preventing recurring or fatal suicide behaviors.
Acknowledgments
Funding: This project was supported by Award Number U01MH088278 from the National Institute of Mental Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health.
Footnotes
Disclosures and Acknowledgments: We thank Janice Espinola, MPH, for her contributions to the statistical analysis.
Conflict of interest: The authors have no conflicts of interest to report.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.World Health Organization (WHO) [Accessibility verified February 18, 2011.];Suicide prevention (SUPRE) Available at http://www.who.int/mental_health/prevention/suicide/suicideprevent/en/
- 2.Nock M, Kessler RC. Prevalence of risk factors for suicide attempts versus suicide gestures: analysis of the national comorbidity survey. J Abnorm Psychol. 2006;115(3):616–623. doi: 10.1037/0021-843X.115.3.616. [DOI] [PubMed] [Google Scholar]
- 3.Owens D, Horrocks J, House A. Fatal and non-fatal repetition of self-harm: systematic review. Brit J Psychiat. 2002;181:193–199. doi: 10.1192/bjp.181.3.193. [DOI] [PubMed] [Google Scholar]
- 4.Gairin I, House A, Owens D. Attendance at the accident and emergency department in the year before suicide: Retrospective study. Brit J Psychiat. 2003;183:28–33. doi: 10.1192/bjp.183.1.28. [DOI] [PubMed] [Google Scholar]
- 5.United States Department of Health and Human Services: National Center for Health Statistics. National Hospital Ambulatory Medical Care Survey. 2008. [Google Scholar]
- 6.Doshi A, Boudreaux ED, Wang N, Pelletier AJ, Camargo CA., Jr National study of US emergency department visits for attempted suicide and self-inflicted injury, 1997–2001. Ann Emerg Med. 2005 Oct;46(4):369–375. doi: 10.1016/j.annemergmed.2005.04.018. [DOI] [PubMed] [Google Scholar]
- 7.Larkin GL, Smith RP, Beautrais AL. Trends in US emergency department visits for suicide attempts, 1992–2001. Crisis. 2008;29(2):73–80. doi: 10.1027/0227-5910.29.2.73. [DOI] [PubMed] [Google Scholar]
- 8.Niska R, Bhuiya F, Xu J. National Hospital Ambulatory Medical Care Survey: 2007 Emergency Department Summary. National health statistics reports; no 26. Hyattsville, MD: National Center for Health Statistics; 2010. [PubMed] [Google Scholar]
- 9.Sinharay S, Stern H, Russell D. The use of multiple imputation for the analysis of missing data. Psychol Methods. 2001;6:317–329. [PubMed] [Google Scholar]
- 10.U.S. Census Bureau. [Accessibility verified February 18, 2011.];Population estimates. Available at http://www.census.gov/popest/datasets.html.
- 11.Jack R. Women and attempted suicide. Hove: Erlbaum; 1992. [Google Scholar]
- 12.Centers for Disease Control and Prevention. Youth suicide and attempted suicide. MMWR Morb Mortal Wkly Rep. 2004;53:471–98. [Google Scholar]
- 13.Cloutier P, Martin J, Kennedy A, Nixon MK, Muehlenkamp JJ. Characteristics and co-occurrence of adolescent non-suicidal self-injury and suicidal behaviours in pediatric emergency crisis services. J Youth Adolescence. 2010;39(3):259–269. doi: 10.1007/s10964-009-9465-1. [DOI] [PubMed] [Google Scholar]
- 14.US Department of Health and Human Services. [Accessed on March 15, 2012.];FDA Launches a Multi-Pronged Strategy to Strengthen Safeguards for Children Treated With Antidepressant Medications. http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/2004/ucm108363.htm.
- 15.Cheung A, Sacks D, Dewa CS, Pong J, Levitt A. Pediatric prescribing practices and the FDA Black-box warning on antidepressants. J Dev Behav Pediatr. 2008;29:213–215. doi: 10.1097/DBP.0b013e31817bd7c9. [DOI] [PubMed] [Google Scholar]
- 16.Buzan RD, Weissberg MP. Suicide: risk factors and therapeutic considerations in the emergency department. J Emerg Med. 1992;10:335–343. doi: 10.1016/0736-4679(92)90340-y. [DOI] [PubMed] [Google Scholar]
- 17.Boeninger DK, Masyn KE, Feldman BJ, Conger RD. Sex differences in developmental trends of suicide ideation, plans, and attempts among European American adolescents. Suicide Life Threat Behav. 2010;40(5):451–464. doi: 10.1521/suli.2010.40.5.451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Weissman MM, Bland RC, Canino GJ, et al. Prevalence of suicide ideation and suicide attempts in nine countries. Psychol Med. 1999;29(1):9–17. doi: 10.1017/s0033291798007867. [DOI] [PubMed] [Google Scholar]
- 19.Kumar CTS, Mohan R, Ranjith G, Chandrasekaran R. Gender differences in medically serious suicide attempts: A study from South India. Psychiat Res. 2006;144:78–86. doi: 10.1016/j.psychres.2005.11.012. [DOI] [PubMed] [Google Scholar]
- 20.Beautrias AL. Suicides and serious suicide attempts: Two populations or one? Psychol Med. 2001;31:837–845. doi: 10.1017/s0033291701003889. [DOI] [PubMed] [Google Scholar]
- 21.Ikeda R, Mahendra R, Saltzman L, et al. Nonfatal self-inflicted injuries treated in hospital emergency departments – United States, 2000. MMWR Morb Mortal Wkly Rep. 2002;51(20):436–438. [PubMed] [Google Scholar]
- 22.Wadsworth T, Kubrin C, Herting J. Trends in Suicide Among Urban White and African American Males: 1980–2002. Paper presented at the annual meeting of the ASC Annual Meeting; San Francisco, California. 2010. Nov, [Google Scholar]
- 23. [Accessibility verified February 18, 2011.];Healthy Place. Suicide among blacks. 2008 Dec; Available at http://www.healthyplace.com/depression/minorities/suicide-among-blacks/menu-id-68/
- 24.Shaffer D, Gould M, Hicks RC. Worsening suicide rate in black teenagers. Am J Psychiat. 1994;151:1810–1812. doi: 10.1176/ajp.151.12.1810. [DOI] [PubMed] [Google Scholar]
- 25.Gibbs JT. African-American suicide. Suicide Life Threat Behav. 1997;27:68–79. [PubMed] [Google Scholar]
- 26.Joe S. Implications of focusing on black youth self-destructive behaviors instead of suicide when designing preventative interventions. In: Romer D, editor. Reducing Adolescent Risk: Toward an Integrated Approach. Thousand Oaks, Calif: SAGE Publications; 2003. pp. 325–332. [Google Scholar]
- 27.Joe S, Baser RS, Neighbors HW, Caldwell CH, Jackson JS. 12-month and lifetime prevalence of suicide attempts among black adolescents in the National Survey of American Life. J Am Acad Child Psy. 2009;48(3):271–282. doi: 10.1097/CHI.0b013e318195bccf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.American Foundation for Suicide Prevention. [Accessibility verified February 18, 2011.];Facts and Figures. Available at http://www.afsp.org/index.cfm?fuseaction=home.viewpage&page_id=050fea9f-b064-4092-b1135c3a70de1fda.
- 29.Larkin GL, Beautrais A, Spirito A, Kirrane B, Lippmann MJ, Milzman DP. Mental health and emergency medicine: A research agenda. Acad Emerg Med. 2009;16:1110–1119. doi: 10.1111/j.1553-2712.2009.00545.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McDonald AJ, III, Wang N, Camargo CA., Jr US emergency department visits for alcohol-related diseases and injuries between 1992 and 2000. Arch Intern Med. 2004;164:531–537. doi: 10.1001/archinte.164.5.531. [DOI] [PubMed] [Google Scholar]
- 31.Borges G, Cherpitel CJ, MacDonald S, Giesbrecht N, Stockwell T, Wilcox HC. A case crossover study of acute alcohol use and suicide attempt. J Stud Alcohol. 2004;65(6):708–714. doi: 10.15288/jsa.2004.65.708. [DOI] [PubMed] [Google Scholar]
- 32.Crawford MJ, Csipke E, Brown A, Reid S, Nilsen K, Redhead J, Touquet R. The effect of referral for brief intervention for alcohol misuse on repetition of deliberate self-harm: an exploratory randomized control trial. Psychol Med. 2010;40:1821–1828. doi: 10.1017/S0033291709991899. [DOI] [PubMed] [Google Scholar]
- 33.Bernstein E, Bernstein J. Effectiveness of alcohol screening and brief motivational intervention in the emergency department setting. Inj Prev. 2008;51:751–754. doi: 10.1016/j.annemergmed.2008.01.325. [DOI] [PubMed] [Google Scholar]
- 34.Brausch AM, Gutierrez PM. Differences in non-suicidal self-injury and suicide attempts in adolescents. J Youth Adolescence. 2009;39(3):233–242. doi: 10.1007/s10964-009-9482-0. [DOI] [PubMed] [Google Scholar]