Abstract
AIM
To assess the visual outcomes and possible risk factors associated with axis alignment and rotational stability after implantation of Toric implantable collamer lens (TICL) for the correction of high myopic astigmatism.
METHODS
In this prospective, nonrandomized clinical study, 54 consecutive eyes of 29 patients with high myopic astigmatism received TICL implantation. To evaluate postoperative axis deviation from the intended axis, a digital anterior segment photograph was taken. The ultrasound biomicroscopy(UBM) was used to observe footplate-position.
RESULTS
After mean follow-up of 8.6 months, mean manifest refractive cylinder (MRC) decreased 79.3% from (-1.88±1.49)D preoperatively to (0.39±0.61)D postoperatively. MRC within 1.00 D occurred in 68.5% (37/54) of eyes, whereas 48.1% (26/54) had MRC within 0.50 D. Mean manifest refraction spherical equivalent (MRSE) changed from (-12.08±4.22)D preoperatively to (-0.41±0.61)D postoperatively. Uncorrected binocular vision of 20/20 or better occurred in 72.2% (39/54) of patients compared with binocular best-corrected visual acuity (BCVA) of 20/20 or better in 44.4% (24/54) preoperatively. The mean difference between intended and achieved TICL axes was (6.96±8.37)°. Footplates of TICLs were in the ciliary sulcus in 22 eyes (46.3%), below the ciliary sulcus in 32 eyes (53.7%). The angle of TICL rotation had significant correlation with the footplates-position (t=2.127; P=0.045) and the postoperative TICL vaulting (r=-0.516; P=0.000).
CONCLUSION
The results of our study further support the safety, efficacy and predictability of TICL for the correct high myopic astigmatism. The footplate-position of TICL and vault value should be taken into consideration as two possible risks factors for TICL rotation.
Keywords: astigmatism, myopia, Toric
INTRODUCTION
Myopia is often combined with astigmatism. There are several ways to correct this refractive error. Spectacles are safe but not suitable for some patients with high myopic astigmatism due to limited visual field and distortion. The contact lenses have better visual quality than spectacles, but it has some disadvantages such as corneal infection and intolerance of contact lenses. Corneal relaxing incision is an option, but it is associated with low predictability and regression. Corneal reshaping surgeries, such as LASIK and photorefractive keratectomy are the best option for low to moderate levels of myopia astigmatism, but it may not be the best option for high myopia astigmatism due to various factors. Firstly, in the correction of high myopia by LASIK, relatively large amounts of cornea must be ablated, small effective optical zones are created, and the predictability and stability of the procedure begin to decrease[1],[2]. Secondly, the ocular high orders aberration (HOA), particularly positive spherical aberration significantly increases postoperatively, causing the quality of vision deteriorated[3]-[6]. Furthermore, the increasing number of reported corneal ectasia cases after LASIK, refractive surgeons are getting to better understanding of the biomechanical effect of LASIK on cornea.
The technique of clear lens extraction with IOL implantation is an option for correcting of high myopia. Co-existing astigmatism can be neutralised at the time of the surgery by varying the incision through which the lens is implanted or by the use of toric IOLs. However, the clear lens extraction causes loss of accommodation and increases the risk of retinal detachment and cystoid macular edema, especially if neodymium doped: yttrium–aluminium–garnet (Nd:YAG) laser posterior capsulotomy is required for posterior capsule opacification[7],[8].
Toric phakic intraocular lens (TICL) is an alternative to LASIK for the correction of high myopia combined with astigmatism. The advantage of TICL implantation is lack of disruption of cornea and potential removability and exchangeability compared with LASIK. Schallhorn et al[9] reported better outcomes using TICL compared with conventional PRK for moderate to high myopic astigmatism. Similarly, Kamiya et al[10] reported that TICL was safer, and more efficacious and predictable than wavefront-guided LASIK for high myopic astigmatism. Although several TICL studies[10]-[14] reported the efficacy, predictability and axis misalignment. It is seldom to study the rotational and footplate stability of TICL implantation with reliable, objective modalities, such as digital anterior segment photography, anterior optical coherence tomography (OCT) and ultrasound biomicroscopy(UBM). Because it is very important to maintain the intended TICL axis for achieving the desired astigmatic correction, this study was undertaken to evaluate the visual and refractive outcomes, especially possible risk factors for postoperative rotation of implantation with the Visian TICL version 4 in Chinese eyes.
SUBJECTS AND METHODS
Subjects
We conducted a prospective study of 29 consecutive patients (54 eyes) who underwent TICL implantation (model V4, Staar Surgical) between February 2010 and August 2011 at the Department of Ophthalmology in the People's Hospital of Ningxia Hui Autonomous Region. The risks and benefits of surgery including nonsurgical alternatives were discussed with all patients before obtaining informed consent. The study was approved by the hospital ethics committee and adhered to the tenets of the Declaration of Helsinki. This study was approved by the Institutional Review Board of Ningxia People Hospital, Yinchuan, Ningxia Hui Autonomous Region, China. Written informed consent was obtained from all patients.
The basic inclusion criteria were myopia ≥6.00 diopters (D); astigmatism ≥-1.00D; age 18 to 43 years; no preexisting ocular pathology, previous ocular surgery, or systemic disease; intraocular pressure (IOP) between 10 mmHg and 21mmHg; endothelial cell density >2000/mm2; and a clinically clear crystalline lens. Eyes with shallow anterior chamber depth (ACD) (<2.8mm), large scotopic pupil size (>7.5mm), or white-to-white distance (WTW) of less than 10.8mm were excluded from this study.
All patients underwent a baseline ophthalmic examination that included the measurement of uncorrected visual acuity (UCVA), best-corrected visual acuity (BCVA), manifest and cycloplegic refractions (SE and refractive cylinder), mean keratometry (K), IOP, endothelial cell counts, slit-lamp microscopy of cornea and anterior segment, and a dilated fundus examination performed in all eyes preoperatively and at last follow-up.
Other ocular parameters which are needed to decide on the appropriate TICL (K readings, WTW distance and ACD as measured from the corneal endothelium) were measured using the Orbscan IIz (Bausch and Lomb, Salt Lake City, UT).
The minimum follow-up time was 3 months and the mean follow-up time was (8.6±4.6) months (ranged from 3 months to 20 months).
Methods
TICL length selection
All patients had implantation of a Vision TICL (STAAR Surgical Co., Monrovia, Calif, US). This TICL is made from a hydrophilic porcine collagen that filters ultraviolet light and is biocompatibile[15]. It is approved by the U.S. Food and Drug Administration (FDA) to treat -3.00D to -23.00D of myopia with less than -6.00D of astigmatism. TICL power calculation was performed by the manufacturer using the astigmatism decomposition method[16] TICLs were manufactured to minimize rotation to within ±22.5 degrees from the horizontal meridian. The size of TICL was also chosen by the manufacturer based on the WTW distance and anterior chamber depth with scanning-slit topography (Orbscan IIz, Bausch & Lomb). In all eyes, the preoperative manifest refraction was selected as the target myopic correction.
Surgical technique
At least 1 week before surgery, all patients received two peripheral iridectomies at the 10 and 2 o'clock positions by using a neodymium: YAG laser. On the day of surgery, the horizontal axis was marked at the 3 and 9 o'clock limbus immediately before surgery with the aid of a slit-lamp microscope while the patient was sitting upright. Surgeries were performed under topical anesthesia with fully pupil dilatation. Two paracenteses at the 6 and 12 o'clock meridians and a 3.2-mm temporal clear corneal incision were made with a diamond knife and the anterior chamber was filled with sodium hyaluronate. The TICL was inserted through the temporal incision with in a lens insertion cartridge. Footplates were tucked behind the iris and in the ciliary sulcus using a modified intraocular spatula. Correct positioning of the TICL was verified intraoperatively under microscope with Mendez-type axis ring marker. Viscoelastic was irrigated out of anterior chamber with balanced salt solution and acetylcholine injected to induce mitosis. Patients were monitored for half an hour with IOPs measurements performed 1-4 hours after surgery. Levofloxacin (0.5%) and Flurorometholone (0.1%) were administered 4 times daily for 2 weeks with a tapering dose postoperatively.
Postoperative measurement
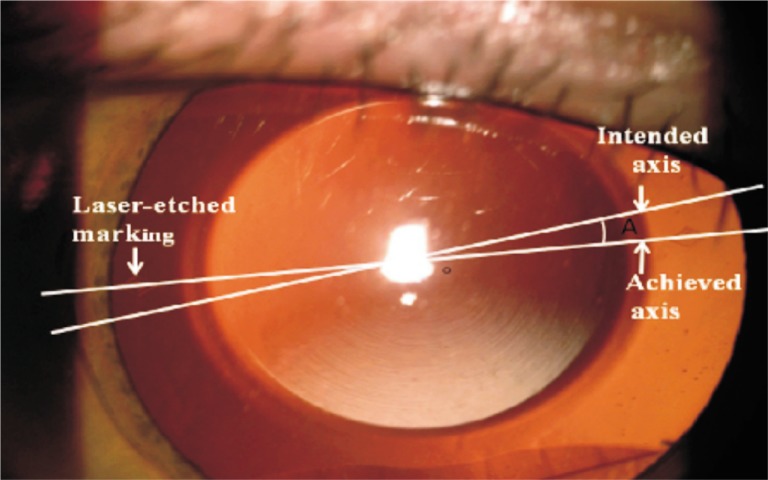
The minimum follow-up was 3 months. Vault was measured on the optical axis at each postoperative visit using anterior optical coherence tomography (OCT) (Carl Zeiss Meditec, Jena, Germany). The vault was measured three times, with the average value used for the analysis. Four footplate positions were observed with UBM(SW-3200L, SUOER), which provides high resolution images of anterior segment. A digital anterior segment photograph was taken after full mydriasis for evaluating postoperative axis deviation from the intended axis in sitting position using a digital camera (Nikon D2H; Nikon Corp, Tokyo, Japan) connected to slit-lamp microscope (Topcon SL-D7; Topcon Corp, Tokyo, Japan). Postoperative deviation from the intended TICL axis was measured from the photographs by the manner described by Park[17] (Figure 1).
Figure 1. Anterior segment photograph after implantation with the TICL, which was taken after full mydriasis for the laser-ecthed markings to be visible.
Statistical Analysis
Statistical analysis was performed on SPSS software (Ver. 17.0; SPSS Inc., Chicago, IL). Data were presented as mean±standard deviation. Differences between the groups were evaluated by t-test. A P value less than 0.05 was considered statistically significant. Possible risk factors for TICL misalignment, such as spherical and cylindrical power of TICL, preoperative spherical equivalent refraction (SE), postoperative TICL vaulting, and footplate position were analyzed through correlation analysis. P values and correlation coefficient were evaluated by Pearson correlation analysis; Standard Linear regression coefficient beta were evaluated by linear regression analysis.
RESULTS
Patient Demographics
25/29 had toric ICL's in both eyes, whereas four patients received spherical ICL in the other eye. Mean age of patients was (30.77±7.20) years (ranged from 18 to 43 years). Of the 29 consecutive patients, 17 (58.6%) were female. All patients included in this study had completed 3 months follow-up with an average follow-up time of (8.6±4.6) months (range 3-20 months). 37 (68.5%) of 54 eyes were followed for ≥6 months, and 15 (27.8%) eyes were followed for ≥12 months. The mean preoperative MRSE was (-12.08±4.22)D (range from -6.00 D to -24.75D). All 54 eyes had preoperative myopia ≥6.00D; 21 were between 6.00D and 10.00D, 30 were >10.00D to <20.00 and 3 were ≥20.00D. Other baseline clinical characteristics are presented in Table 1.
Table 1. Clinical characteristics of 29 patients who underwent implantation of TICL.
| Characteristics | Results |
| Number of eyes | 54 |
| Mean age (range) (a) | 30.77 ±7.20(18 to 43) |
| Gender (n) | |
| Male | 12 |
| Female | 17 |
| Mean spherical equivalent refraction (range) (D) | -12.08±4.22(-6.00 to -24.75) |
| Mean refractive cylinder (range) (D) | -1.88±1.49 (-1.00 to -5.50) |
| Mean intraocular pressure (range) (mmHg) | 14.45±2.37 (10.00 to 19.70) |
| Anterior chamber depth (range) (mm) | 3.12±0.21 (2.81 to 3.91) |
| White-to-white distance (WTW) (range) (mm) | 11.27±0.32(10.8 to 12.4) |
| Mean follow-up (range) (month) | 8.6±4.6 (3 to 20) |
Postoperative mean endothelial cell counts was (2598.19±366.10) at the last postoperative visit, which showed no significant decrease compared with preoperative mean endothelial cell counts (2693.08±360.17)(P >0.05).
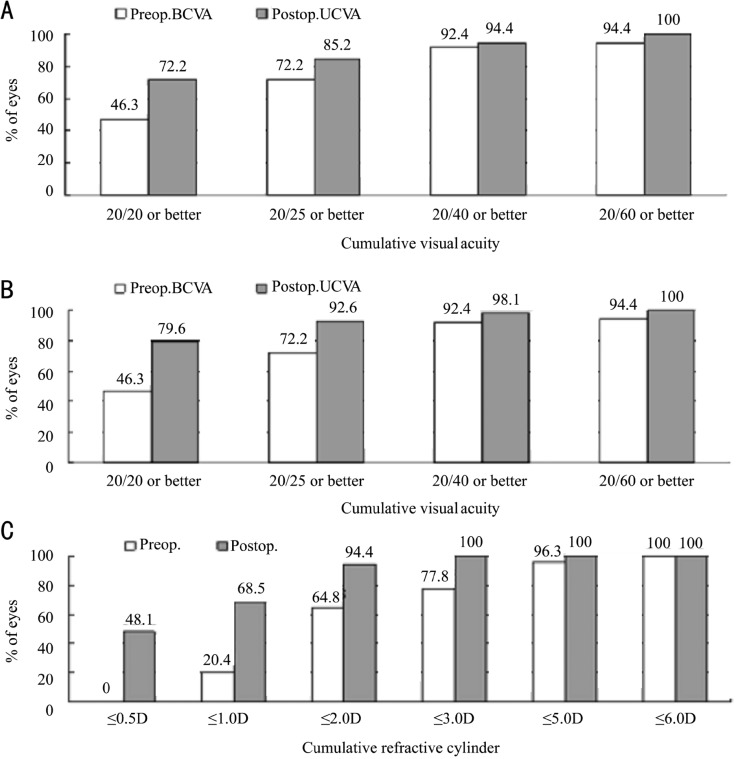
Visual Acuity
All eyes had a preoperative UCVA wore than 20/100 with 18.5% (10/54) having unaided acuity limited to counting fingers. After mean follow-up of (8.6±4.6) months, 72.2% (39/54) of eyes had UCVA of 20/20 or better, 85.2% (46/54) had 20/25 or better and 94.4% of eyes (51/54) had 20/40. Comparison results of preoperative BCVA values with postoperative UCVA values indicating good efficacy of TICL implantation were shown in Figure 2A. Comparison results of pre- and postoperative BCVA values were shown in Figure 2B; no patient had loss of BCVA at last postoperative visit indicating good safety of TICL implantation.
Figure 2. Visual acuity and refractive outcomes at mean follow-up of (8.6±4.6) months after implantation with the STAAR TICL.
A: Preoperative BCVA vs postoperative UCVA; B: Preoperative vs postoperative BCVA; C: Preoperative vs postoperative refractive cylinder.
Refractive Outcomes
The mean manifest refraction spherical equivalent (MRSE) improved significantly from (-12.08 ±4.22)D preoperatively to (-0.41±0.61)D at mean (8.6±4.6) months postoperatively (P<0.001). Preoperatively, all 54 eyes had myopia >6.00D; however, 100%, 88.9 % and 81.5% of eyes were within 2.00, 1.00 and 0.50D, respectively, of emmetropia after surgery, indicating good predictability of TICL implantation for high myopia correction.
Astigmatism preoperatively ranged from -1.00 to -5.50D with a mean preoperative refractive cylinder of (-1.88±1.49)D. All eyes had refractive cylinder of ≥1.00D preoperatively. At last postoperative visit, MRC was (-0.41±0.61)D, representing 78.2% decrease in astigmatism (P <0.001). Comparison results of pre- and postoperative refractive cylinder were shown in Figure 2C. A refractive cylinder of ≤0.5D was targeted in all eyes and achieved in 48.1% (26/54) of cases, whereas 68.5% cases (37/54) had cylinder ≤1.00D, indicating good predictability of TICL implantation for astigmatism correction.
Risk factors for rotation of TICL
The mean of the absolute value of difference between the intended and achieved cylinder axes was (6.96±8.37)° (range: 0° to 40°). At last postoperative follow-up, 46.2% of the TICLs were ≤5° from the intended axis, 80.8% were ≤10°, and 98.2% (1/54) were≤15°.
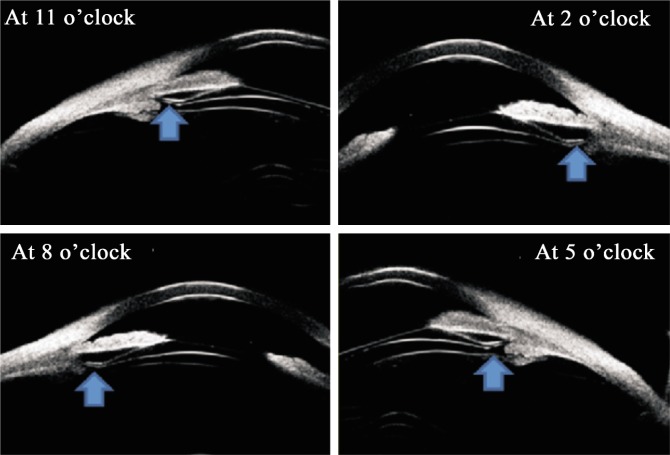
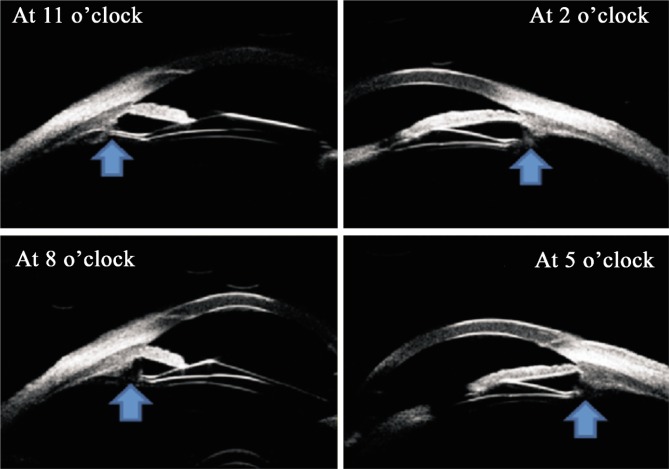
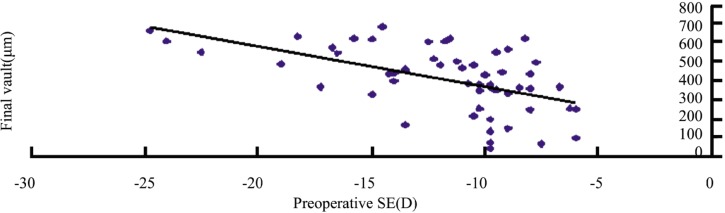
UBM revealed footplates of TICLs were in the ciliary sulcus (Figure 3) in 22 eyes(46.3%), below the ciliary sulcus (Figure 4) in 32 eye(53.7%)(Table 2). Rotation of TICL was observed in 20 of 22 eyes (90.9%) with footplates fixed in the ciliary sulcus and in 14 of 32 eyes (43.8%) with footplate fixed below the ciliary sulcus. The angle of TICL rotation had significant correlation with the fixed footplate position of TICL (Table 2). Mean vault at last postoperative visit was (0.44±0.17)mm. The patients with footplates of TICLs in the ciliary sulcus showed lower vault value than the patients with the footplates below the ciliary sulcus (t=3.395, P =0.01) (Table 3). The angle of TICL rotation had significant correlation with the postoperative TICL vaulting (Pearson's correlation coefficient (r=-0.516, P=0.000) (Figure 5) and had no significant correlation with the preoperative SE of the patient's eye, spherical power of the TICL and the cylindrical power of the TICL. A statistically significant correlation was observed between the vault value and the preoperative SE of the patient's eye (Pearson's correlation coefficient; r= -0.535, P=0.000) (Figure 6).
Figure 3. Postoperative UBM was performed on the four footplates (arrowheads) of each TICL at the patient's last follow-up. The four footplates were located in the ciliary sulcus (arrowhead).
Figure 4. Postoperative UBM was performed on the four footplates (arrowheads) of each TICL at the patient's last follow-up. The footplates were located below the ciliary sulcus (arrowhead).
Table 2. Angle of TICL rotation and footplates position.
| Footplates position | n(%) | Angle of TICL rotation (°) |
| In ciliary sulcus | 22(46.3) | 10.64±5.27 (0-40) |
| Below the ciliary sulcus | 32(53.7) | 3.85±4.85 (0-10) |
Using Independent-Sample T Test: t=2.127, P=0.045.
Table 3. Footplates position and final Mean vault value.
| Footplates position | n | Vault at last postop visit |
| In ciliary sulcus | 22 | 322.23±169.43 (48-487) |
| Below the ciliary sulcus | 32 | 466.28±141.12 (140-680) |
Using Independent-Sample T Test: t=3.395, P=0.01.
(x±s, µm)
Figure 5. Correlation analysis between the absolute value of postoperative misalignment (the angle of rotation) of the TICL axis and the final vault showed significant negative correlation between these two variables (r=-0.516; P=0.000).
Figure 6. Correlation analysis between preoperative SE and final vault value showed significant negative correlation between these two variables. (r=-0.535; P=0.000<0.05).
Complications
No intraoperative complications or significant changes in IOP occurred. The mean IOP was (14.45±2.37)mmHg (range 10mmHg to 19.7mmHg) preoperatively and (15.66±2.62)mmHg (range 10mmHg to 20mmHg) postoperatively. In the immediate postoperative period and at the first day after surgery, five eyes had intraocular pressures increased (range 25mmHg to 28mmHg) and all resolved with systemic and topical treatment including oral Methazolamide 50mg (Pharmaceutical Division of Chinese Aoyibaoling Company, Hangzhou, Zhejiang Province, China) and Cartelolol 0.5% (Chinese Dazhong Company, Tianjin, China). In all cases, the angles were opened and there were no signs of pupillary block or excessive vaulting of the TICL. At the last postoperative visit, no cataract formation was observed under slit-lamp microscopy. No cases of chronic inflammation of the anterior chamber were noted at any postoperative visit.
Lens exchange was performed in two eyes because the TICLs were too short which resulted in low vault value of 48µm on the right eye and 80µm on the left eye. The TICLs showed 40° of postoperative deviation from the intended axis on the right eye and 10° on the left eye. UBM, performed at last follow-up, revealed all four footplates of two implanted TICLs were in the ciliary sulcus. In this case, preoperative SEs was -9.75D in both eyes and refractive cylinders were 1.25D on the right eye and 1.75D on the left eye. The TICLs were removed and the larger TICLS were inserted 10 months after the first implantation. The 10 months delay in replacing the low vaulting TICL for a larger TICL was the patient preference as he had 20/25 unaided vision on the right eye and 20/20 on the left eye. The larger TICLs resulted in 20/20 unaided vision on both eyes and healthy vault values, 0.50mm on the right eye and 0.49 mm on the left eye. The TICLs showed 2° of postoperative deviation from the intended axis on the right eye and no rotation on the left eye 3 months after the replacing surgery.
DISCUSSION
The predictability and safety of LASIK remains a challenge in patients with high myopic astigmatism[18]–[22]. This is limited by the ability to ablate the correction onto the corneal tissue, which is then subject to corneal healing, biomechanical effect and the positive spherical aberration increasing[3]-[6]. It is also contraindicated in patients with thin corneas. In current study, we found that the STAAR TICL implantation had effective and safe correction of high myopic astigmatism and the refractive outcome, predictability, and manifest cylinder and MRSE were excellent. After mean follow-up of (8.6±4.6) months, mean manifest refractive cylinder (MRC) decreased 79.3% from (-1.88±1.49)D preoperatively to (0.39D±0.61)D postoperatively. MRC within 1.00D occurred in 68.6% (51/54) of eyes, whereas 48.2% (26/54) had MRC within 0.50D and 68.6% within 1.00D. Mean manifest refraction spherical equivalent (MRSE) changed from (-12.08±4.22)D preoperatively to (-0.41±0.61)D postoperatively and 82.9% of eyes were within 0.50D of the intended MRSE, 97.1% within 1.00D. The improved both UCVA and BSCVA similar to a previous report[11],[17]. Preoperatively 90% eyes had BCVA of 20/40, whereas 95% eyes had UCVA of 20/40 or better at last postoperative visit. Uncorrected binocular vision of 20/20 or better occurred in 72.2% (39/54) of patients compared with binocular BCVA of 20/20 or better in 44.4% (24/54) preoperatively. 59.3% (32/54) gained up to one or more line BCVA and no patient had loss of BCVA.
For achieving the desired astigmatic correction with TICL implantation, it is imperative to maintain because rotation of a toric IOL was found to exponentially decrease the astigmatic correction and when the toric IOL became more off-axis, it showed a steady loss of astigmatism reduction in previous studies[14],[23],[24]. Therefore, the postoperative rotational stability is one crucial factor determining successful surgical outcome of TICL implantation. To make the TICL rotation measure more accurately, digital anterior segment photographs were used in our study instead of slit-lamp measurement. The mean of the absolute value of misalignment (6.96±8.37)° in our study was similar to the result of a previous study[17]. 98.2% of cases had ≤15° of misalignment from the intended axis and one patient in our study underwent TICL repositioning due to misalignment, whereas 4.6% of cases had >15° of misalignment and one patient had TICL repositioning in the previous study[11].In addition, all three eyes with 13° and 15° of TICL misalignment had UCVA of 20/20 in our study.
The postoperative TICL vaulting was taken into consideration as a possible risk factor for TICL rotation according to a previous report[25]. It is sure that oversized TICL length results in a high vault, whereas an undersized TICL length results in a low vault and easier rotation. Generally, the TICL size is determined based on the horizontal corneal diameter (white-to-white) and ACD. However, size mismatches can occur. Some studies pay attention to the correlation between the corneal diameter and sulcus-to-sulcus diameter and found it is weak[26],[27]. Especially, the higher levels of myopia were typically accompanied by a larger sulcus diameter, which may make the TICL length relatively shorter and result in a low vault and easy rotation. Our study showed that the angle of TICL rotation had significant correlation with the postoperative TICL vaulting, which was contrary with the Park' report[17]. One of the reasons for no significant correlation between the postoperative TICL vaulting and TICL rotation in Park' study may be the lack of cases with very low vaulting, which could possibly cause clinically significant postoperative TICL rotation. However, in this study, one patient had very low vaulting, 48µm on the right eye and 80µm on the left eye, which caused clinically significant postoperative TICL rotation, 40° of postoperative deviation from the intended axis on the right eye and 10° on the left eye. It was obvious that the TICLs were too short. Therefore, the TICLs were removed and the larger TICLS were inserted, which resulted in healthy vault values, 390µm on the right eye and 420µm on the left eye. The TICLs showed 2° of postoperative deviation from the intended axis on the right eye and no rotation on the left eye 3months after the larger TICL replacing.
In this study, a significant correlation between the absolute angles of rotation with the fixed footplate position of TICL was observed. The ideal fixed position of the TICL footplates is to rest on the ciliary sulcus. However, one study reported that 35.3% of implanted eyes with ICL were fixed in the ciliary body[28]. In present study, 22 eyes (46.3%) of implanted eyes with TICL were fixed in the ciliary sulcus and 32 eyes (53.7%) (Table 2) were fixed below the ciliary sulcus. Rotation of TICL was observed in 90.9% eyes with footplates fixed in the ciliary sulcus and in 43.8% eyes with footplate fixed below the ciliary sulcus. The results indicate the hypothesis that the TICL footplates to rest on the ciliary body may lead to more stability than to rest in the ciliary sulcu.
A previous study by Park et al[17] reported that the spherical power of the TICL alone was found to have significant correlation with the angle of TICL rotation. The thickness and overall height of STAAR TICLs vary with its spherical power. As the spherical power of the TICL becomes more highly negative, the thickness and overall height increase. In other words, the TICL gets bulkier and heavier with its increase in negative spherical power. Therefore, these changes in the dimension of the TICL according to its spherical power might be related to the stability and its postoperative rotation. In this study, the preoperative SE was also considered a possible ocular risk factor for TICL rotation, but no significant correlation between the TICL rotation with the preoperative SE of the patient's eye or spherical power of the TICL was found. According to a hypothesis for the significant relationship between spherical power of the TICL and the angle of postoperative TICL rotation, a higher levels of myopia, which required a TICL with more highly negative spherical power, were typically accompanied by a larger sulcus diameter, leading to less vaulting and easier rotation. However, a statistically significant negative correlation was observed between the vault value and the preoperative SE of the patient's eye (r= -0.535, P=0.000) in this study. It was quite interesting that a higher levels of myopia, which required a TICL with more highly negative spherical power lead to higher vaulting. Therefore, fixed position of the TICL should be considered as one of the major reasons for the negative correlation between the TICL vaulting and preoperative SE. In Park' study, the footplates of all TICLs were in situ in the ciliary sulcus except for one case in which one of the four footplates was located below the ciliary sulcus. In our study, 46.3% of implanted eyes with TICL were fixed in the ciliary sulcus and 53.7% were fixed below the ciliary sulcus. Theoretical analyses indicate that the vault value in the eyes with fixating location on the ciliary sulcus should be smaller than fixating location on the ciliary body. Our study found that the patients with footplates of TICLs in the ciliary sulcus showed significant lower vault value than the patients with the footplates below the ciliary sulcus (t=3.395, P=0.01) (Table 3). It is reasonable to assume that if the TICL footplates are to rest on the ciliary body, it may not lead to vary low vaulting and easier rotation, even if a case with higher level of myopia, accompanied by a larger sulcus diameter, requires a TICL with more highly negative spherical power.
Two major concerns with TICLs include anterior subcapsular cataract formation and glaucoma. Low and high vault are reported to be risks for cataract formation and angle closure, respectively. Low vault is thought to be related to direct contact or be interference with aqueous humour circulation over the crystalline lens[29]-[31]. High vault is thought to cause angle close and pupillary block. In our study, the angles of all cases were opened and no pupillary block or excessive vaulting of the TICL occurred. At the last postoperative visit, no case of premature cataract formation was observed under slit-lamp microscopy, although our follow-up was only 3-20 months. Two eyes required TICLs replacement due to the vault values of 48µm on the right eye and 80µm on the left eye. At the introductory stages of ICL surgery, if the vault value was less than 0.5mm, it was considered to increase the risk of anterior subcapsular cataract formation. Gonvers et al[32], reported on 75 eyes that underwent ICL surgery and found 20 cataracts had occurred when the central vaulting was equal to or less than 90µm the recommendation is to aim for a higher central vaulting of 150µm[21]. Thus the vault values of 48µm and 80µm would be not tolerated as safe although the two eyes had the 20/25 unaided vision on the right eye and 20/20 on the left eye.
The limitation of our study is lack of serial measurements of TICL axis and refractive astigmatism, so we do not know whether the TICL rotated postoperatively and/or was placed off-axis during surgery. No consideration for changes in cylindrical power and axis caused by surgical incision in preparing TICL implantation is another limitation of the present study, as clear corneal incision of 3.0mm to 3.5mm can surgically induce 0.20 to 0.68D of astigmatism.
The results of our study further support that the safety and efficacy of implantation of the TICL for the correct high myopic astigmatism in Chinese eyes. The footplate-position and vault value should be taken into consideration as two possible risk factors for TICL rotation. The preoperative SE of the patient's eye was negatively correlated with the vault value but the reason for this correlation could not be clarified. This study analyzed 54 consecutive eyes during mean 8.6-month follow-up, therefore a larger sample size and longer follow-up study is conducting to further elucidate possible risk factors for postoperative TICL misalignment and the results of which will be reported in the future.
Footnotes
Foundation item: Ningxia Scientific and Technological Projects (2012) from Department of Science and Technology in Ningxia Hui Autonomous Region, China (No. 2012ZYS175) The first two authors contributed equally to this publication
REFERENCES
- 1.Applegate RA, Howland HC. Refractive surgery, optical aberrations, and visual performance. J Refract Surg. 1997;13(6):295–299. doi: 10.3928/1081-597X-19970501-16. [DOI] [PubMed] [Google Scholar]
- 2.Oliver KM, Hemenger RP, Corbett MC, O'Brart DP, Verma S, Marshall J, Tomlinson A. Corneal optical aberrations induced by photorefractive keratectomy. J Refract Surg. 1997;13:246–254. doi: 10.3928/1081-597X-19970501-10. [DOI] [PubMed] [Google Scholar]
- 3.Seiler T, Kahle G, Kriegerowski M. Excimer laser (193nm) myopic keratomileusis in sighted and blind human eyes. Refract Corneal Surg. 1990;6:165–173. [PubMed] [Google Scholar]
- 4.óBrart DP, Lohmann CP, Fitzke FW, Klonos G, Corbett MC, Kerr-Muir MG, Marshall J. Disturbances in night vision after excimer laser photorefractive keratectomy. Eye. 1994;8:46–51. doi: 10.1038/eye.1994.9. [DOI] [PubMed] [Google Scholar]
- 5.Gatinel D, Hoang-Xuan T, Azar DT. Determination of corneal asphericity after myopia surgery with the excimer laser: a mathematical model. Invest Ophthalmol Vis Sci. 2001;42:1736–1742. [PubMed] [Google Scholar]
- 6.Holladay JT, Dudeja DR, Chang J. Functional vision and corneal changes after laser in situ keratomileusis determined by contrast sensitivity, glare testing, and corneal topography. J Cataract Refract Surg. 1999;25:663–669. doi: 10.1016/s0886-3350(99)00011-5. [DOI] [PubMed] [Google Scholar]
- 7.Colin J, Robinet A. Clear lensectomy and implantation of a lower-power posterior chamber intraocular lens for correction of high myopia. Ophthalmology. 1997;104:73–78. doi: 10.1016/s0161-6420(97)30360-1. [DOI] [PubMed] [Google Scholar]
- 8.Goldberg MF. Clear lens extraction for axial myopia. Ophthalmology. 1987;94:571–582. doi: 10.1016/s0161-6420(87)33425-6. [DOI] [PubMed] [Google Scholar]
- 9.Schallhorn S, Tanzer D, Sanders DR, Sanders ML. Randomized prospective comparison of Visian Toric Implantable Collamer Lens and conventional photorefractive keratectomy for moderate to high myopic astigmatism. J Refract Surg. 2007;23:853867. doi: 10.3928/1081-597X-20071101-01. [DOI] [PubMed] [Google Scholar]
- 10.Kamiya K, Shimizu K, Igarashi A, Komatsu M. Comparison of Collamer toric contact lens implantation and wavefront guided laser in situ keratomileusis for high myopic astigmatism. J Cataract Refract Surg. 2008;34:1687–1693. doi: 10.1016/j.jcrs.2008.06.030. [DOI] [PubMed] [Google Scholar]
- 11.Sanders DR, Schneider D, Martin R, Brown D, Dulaney D, Vukich J, Slade S, Schallhorn S. Toric Implantable Collamer Lens for moderate to high myopic astigmatism. Ophthalmology. 2007;114:54–61. doi: 10.1016/j.ophtha.2006.08.049. [DOI] [PubMed] [Google Scholar]
- 12.Chang J, Lau Silvania. Toric Implantable Collamer Lens for High Myopic Astigmatic Asian Eyes. Ophthalmology. 2009;116:2340–2347. doi: 10.1016/j.ophtha.2009.04.053. [DOI] [PubMed] [Google Scholar]
- 13.MBChB RB, FRCOphth SR, FRANZCO TG. Toric implantable collamer lens for patients with moderate to severe myopic astigmatism: 12-month follow-up. Clin Experiment Ophthalmol. 2010;38:467–474. doi: 10.1111/j.1442-9071.2010.02273.x. [DOI] [PubMed] [Google Scholar]
- 14.Till JS, Yoder PR, Jr, Wilcox TK, Spielman JL. Toric intraocular lens implantation:100 consecutive cases. J Cataract Refract Surg. 2002;28:295–301. doi: 10.1016/s0886-3350(01)01035-5. [DOI] [PubMed] [Google Scholar]
- 15.Allarakhia L, Knoll RL, Lindstrom RL. Soft intraocular lens. J Cataract Refract Surg. 1987;13:607–620. doi: 10.1016/s0886-3350(87)80149-9. [DOI] [PubMed] [Google Scholar]
- 16.Sarver EJ, Sanders DR. Astigmatic power calculations for intraocular lenses in the phakic and aphakic eye. J Refract Surg. 2004;20:472–477. doi: 10.3928/1081-597X-20040901-10. [DOI] [PubMed] [Google Scholar]
- 17.Park SC, Kwun YK, Chung ES, Ahn K, Chung TY. Postoperative Astigmatism and Axis Stability After Implantation of the STAAR Toric Implantable Collamer Lens. J Refract Surg. 2009;25:403–409. doi: 10.3928/1081597X-20090422-01. [DOI] [PubMed] [Google Scholar]
- 18.Pérez-Santonia JJ, Bellot J, Claramonte P, Ismail MM, Alió JL. Laser in situ keratomileusis to correct high myopia. J Cataract Refract Surg. 1997;23:372–385. doi: 10.1016/s0886-3350(97)80182-4. [DOI] [PubMed] [Google Scholar]
- 19.Donnenfeld ED, Kornstein HS, Amin A, Speaker MD, Seedor JA, Sforza PD, Landrio LM, Perry HD. Laser in situ Keratomilersis for correction of myopia and astigmatism after penetrating keratoplasty. Ophthalmology. 1999;106:1966–1974. doi: 10.1016/S0161-6420(99)90410-4. [DOI] [PubMed] [Google Scholar]
- 20.Saver EJ, Sanders DR, Vukich JA. Image quality in myopia eyes corrected with laser in situ keratomileusis and phakic intraocular lens. J Refract Surg. 2003;19:397–404. doi: 10.3928/1081-597X-20030701-04. [DOI] [PubMed] [Google Scholar]
- 21.Niesen U, Businger U, Hartmann P, Senn P, Schipper I. Glare sensitivity and visual acuity after excimer laser photorefractive keratectomy for myopia. Br J Ophthalmol. 1997;81(2):136–140. doi: 10.1136/bjo.81.2.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Seiler T, Koufala K, Richter G. Iatrogenic Keratectasia after laser in situ keratomileusis. J Refract Surg. 1998;14:312–317. doi: 10.3928/1081-597X-19980501-15. [DOI] [PubMed] [Google Scholar]
- 23.Gerten G, Michels A, Olmes A. Toric intraocular lenses. Clinical results and rotational stability. Ophthalmology. 2001;98:715–720. doi: 10.1007/s003470170077. [DOI] [PubMed] [Google Scholar]
- 24.Sanders DR, Grabow HB, Shepherd J, Raanan MR. STAAR AA-4203T Toric Silicone IOL. In: Martin RG, Sanders DR, Gillis JP, editors. Foldable Intraocular Lenses. Thorofare, NJ: SLACK Inc; 1993. pp. 237–250. [Google Scholar]
- 25.Jiménez-Alfaro I, Benitez del Castillo JM, Garcia-Feijoó J, Gil de Bernabé JG, Serrano de La Iglesia JM. Safety of posterior chamber phakic intraocular lenses for the correction of high myopia: anterior segment changes after posterior chamber phakic intraocular lens implantation. Ophthalmology. 2001;108:90–99. doi: 10.1016/s0161-6420(00)00403-6. [DOI] [PubMed] [Google Scholar]
- 26.Kim KH, Shin HH, Kim HM, Song JS. Correlation between ciliary sulcus diameter measured by 35 MHz ultrasound biomicroscopy and other ocular measurements. J Cataract Refract Surg. 2008;34:632–637. doi: 10.1016/j.jcrs.2007.11.034. [DOI] [PubMed] [Google Scholar]
- 27.Pop M, Payette Y, Mansour M. Predicting sulcus size using ocular measurements. J Cataract Refract Surg. 2001;27:1033–1038. doi: 10.1016/s0886-3350(00)00830-0. [DOI] [PubMed] [Google Scholar]
- 28.Choi KH, Chung SE, Chung TY, Chung ES. Ultrasound biomicroscopy for determining visian implantable contact lens length in phakic IOL implantation. J Refract Surg. 2007;23:362–367. doi: 10.3928/1081-597X-20070401-08. [DOI] [PubMed] [Google Scholar]
- 29.Alio L, de la Hoz F, Perez-Santonja JJ, Ruiz-Moreno JM, Quesada JA. Phakic anterior chamber lenses for the correction of myopia; a 7-year cumulative analysis of complications in 263 cases. Ophthalmology. 1999;109:458–466. doi: 10.1016/S0161-6420(99)90103-3. [DOI] [PubMed] [Google Scholar]
- 30.Trindade F, Pereira F. Cataract formation after posterior chamber phakic intraocular lens implantation. J Cataract Refract Surg. 1998;24:1661–1663. doi: 10.1016/s0886-3350(98)80361-1. [DOI] [PubMed] [Google Scholar]
- 31.Brauweiler PH, Wehler T, Busin M. High incidence of cataract formation after implantation of a silicone posterior chamber lens in phakic, highly myopic eyes. Ophthalmology. 1999;106:1651–1655. doi: 10.1016/S0161-6420(99)90352-4. [DOI] [PubMed] [Google Scholar]
- 32.Gonvers M, Bornet C, Othenin-Girard P. Implantable Contact Lens for moderate to high myopia: relation-ship of vaulting to cataract formation. J cataract Refract Surg. 2003;29:918–924. doi: 10.1016/s0886-3350(03)00065-8. [DOI] [PubMed] [Google Scholar]