Abstract
AIM
To take fundus examination in the preterm neonates to observe the common diseases and report the outcomes in a neonatal intensive care unit (NICU) in Guangzhou between May 2008 and May 2011.
METHODS
Fundus examinations were performed with Retcam II in 957 prematures.
RESULTS
There were 957 prematures in this study, including 666 males and 291 females, 2 triple births, 152 twins and 803 singletons. During the three years, 86 infants with any stage retinopathy of prematurity (ROP) (9.0%), 123 infants with retinal hemorrhage(12.9%), 10 infants with neonatal fundual jaundice(1.0%) and 3 babies with congenital choroidal coloboma (0.3%) were found.
CONCLUSION
Early detection and prompt treatment of ocular disorders in neonates is important to avoid lifelong visual impairment. Examination of the eyes should be performed in the newborn period and at all well-child visits.
Keywords: fundus examination, premature, retinopathy of prematurity, retinal hemorrhage, choroidal coloboma, early detection
INTRODUCTION
The first embryonic 4-6 months is a crucial stage during the development of the eye, and the infant stage is also the critical stage in the process of visual development. Problems related to visual anomalies are common among young children, particularly in preterm neonates. Screening to enable early diagnosis and correction of visual deficiency is important as abnormal visual input can lead to abnormalities in visual development, which can become permanent visual impairment if left untreated. In 2003, the American Academy of Pediatrics, the American Association of Pediatric Ophthalmology and Strabismus, and the American Academy of Ophthalmology endorsed that vision should be assessed at the beginning of birth and at all well-child visits[1]. In China, neonatal ophthalmology screening has been paid attention in order to prevent neonatal disability since the Second International Conference on Woman and Child Health in 2006 .
This study aimed to report the outcomes of fundus examination with RetCam II in preterm neonates to observe the common diseases in the neonatal intensive care unit (NICU) of Zhujiang Hospital in Guangzhou between May 2008 and May 2011.
SUBJECTS AND METHODS
Subjects
There were 957 infants with a birth weight (BW) <2000g or an estimated gestational age (GA) ≤34 weeks or suffering from certain serious disease but exceeding the above criteria screened at the NICU of Zhujiang Hospital of Southern Medical University, Guangzhou, China, between May 2008 and May 2011.
Methods
The screening sessions and the follow-up were performed according to Chinese guidelines to detect and treat retinopathy of prematurity(ROP), which recommended initial ophthalmological examination should be performed between the fourth and sixth weeks of life or from 32 weeks of postmenstrual age and should be repeated weekly or more frequently according to the findings until full vascularization of the peripheral retina is observed or until 45 weeks of postmenstrual age. On each examination, pupils' dilation was done using 0.5% tropicamide at least 30 minutes prior to examination. Topical proparacaine was applied and an eye speculum was inserted. Digital images were taken with the Retinal Camera II (Massie Research Laboratories Inc.) using the 130° ROP lens. Indirect ophthalmoscopy was performed using a 28D lens and secleral depression in necessary. Findings were recorded.
Statistical Analysis
Data were entered into a spreadsheet and analyzed using SPSS for Windows statistical software Version 13.0 (SPSS Inc., Chicago, Illinois, USA). Clinical characteristics were described by mean±standard deviations. Statistical analysis was performed using the two sample Wilcoxon rank-sum test for continuous variables and Fisher's exact test and Chi-square for categorical variables. P<0.05 was considered statistically significant.
RESULTS
There were 957 infants in this study, including 666 males and 291 females, 2 triple births, 152 twins and 803 singletons. During the three years, 86 infants with any stage ROP(9.0%), 123 infants with retinal hemorrhage(12.9%), 10 infants with neonatal fundual jaundice(1.0%) and 3 babies with congenital choroidal coloboma(0.3%) were found. The incidence of these ocular diseases was significantly different between males and females except retinal hemorrhage(P=0.026). Table 1 showed clearly these neonatal fundal diseases through May 2008 to May 2011.
Table 1. Fundal diseases found in the ocular screening between May 2008 and May 2011.
| Diseases | Incidence | Patients | Eyes | Males | Females | P |
| ROP | 9.0 | 86 | 172 | 53(8.0) | 33(11.3) | 0.092 |
| Retinal hemorrhage | 12.9 | 123 | 224 | 75(11.3) | 48(16.5) | 0.026 |
| Fundal jaundice | 1.0 | 10 | 20 | 8(1.2) | 2(0.7) | 0.735 |
| Choroidal coloboma | 0.3 | 3 | 4 | 1(0.2) | 2(0.7) | 0.221 |
n(%)
Among the 86 infants with any stage ROP, the mean birth weight was (1541.20±343.52)g, the average postnatal weight gain in the first six weeks was (729.18±214.72)g and the average gestational age was (31.21±2.46) weeks. Table 2 describes the incidence of ROP in any stage in the three years.
Table 2. Incidence of ROP in any stage between May 2008 and May 2011.
| Time | ROP | Mild ROP | Severe ROP | AP-ROP | Total patients |
| 2008.5-2009.5 | 44 (16.0) | 31 (11.7) | 13 (4.9) | 1 (0.4) | 265 |
| 2009.6-2010.5 | 18 (5.5) | 10 (3.1) | 8 (2.4) | 2 (0.6) | 328 |
| 2010.6-2011.5 | 24 (6.6) | 19 (5.2) | 5 (1.4) | 2 (0.6) | 364 |
| 2008.5-2011.5 | 86 (9.0) | 60 (6.3) | 26 (2.7) | 5 (0.5) | 957 |
AP-ROP: aggressive posterior retinopathy of prematurity.
n(%)
DISCUSSION
ROP is a multifactorial disease that occurs most frequently in very small and sick infants, which can cause blindness in babies born prematurely. With the increasing survival of premature babies, a “third epidemic” is in the making[2]. Since the incidence of ROP is different in accordance with the different criteria and time-periods in different countries, the incidence of ROP of 9.0% in our study was still comparable to the other countries. The reported incidence of acute ROP varies from 7.35% to 50.9% and the threshold ROP which needs treatment varies from 3.6% to 34.8% during the last 5 years[3]-[6]. In this study, the incidence of ROP (9.0%) was also fairly in agreement with the reported values in domestic cities, such as Guangzhou(5.4%)[7], Hangzhou (9.8%)[8] and Shenzhen (10.7%)[9] during the last 5 years. The study also found the incidence of ROP was much higher in 2008-2009 than the other two years, which we thought it related to the introduction of use of surfactant and prenatal steroids or to the improving neonatal care and better monitoring of oxygen saturation. We also found that 34 babies with low gestational age at birth had larger area of avascular retina in the initial screening, which progressed to any stage of ROP in the following days. Therefore, it is worth well observing the area of avascular retina which always predisposes the baby to developing ROP.
According to the treatment guidelines of the Early Treatment of Retinopathy of Prematurity (ET-ROP) study[10], the type I high-risk prethreshold and threshold ROP had been treated with cryotherapy and diode laser photocoagulation with 48 hours. Patients with stage 4 or 5 ROP needed for surgery and following-up. In the study, 17 patients (33 eyes) underwent treatment, besides 6 babies transferred to other hospital for intervention. We observed that 16 eyes of 8 infants' neovascularization regressed completely after laser treatment or cryotherapy, 2 babies (3 eyes) with different degree of the cicatricial changes, 1 baby (2 eyes) with AP-ROP underwent laser treatment in 24 hours but progressed rapidly to stage 4 and transferred to other hospital and 6 patients (12 eyes) with early intervention failed to follow-up. Obviously, early intervention is effective, while long term visual development should be observed in a long run.
Neonatal retinal hemorrhages related to birth trauma are common, benign, and self-limiting, other retinal hemorrhages in infancy may signify intracranial aneurysms, accidental or non-accidental injury, and a variety of ocular (e.g., Coats' disease, persistent hyperplasia of primary vitreous, ROP , retinal dysplasia, hypertension, myopia) or systemic disease (e.g. hematologic or cardiovascular disorders, infection, protein C deficiency)[11] . Twisted neonatal retinal vascular with uneven thickness of diameter, rapid continuous shunt, hypoplasia of branch vessel and most dense capillary network around the optic papilla, these are the reasons why the prematures are prone to retinal hemorrhage[12]. Retinal hemorrhage due to ROP tend to occur on the surface of the neovascular ridge, which represents an arteriovenous shunt formed by the anastomosis of primitive retinal vessels, meanwhile the vascular fragility also resulting in hemorrhage. Choi et al[13] found that most hemorrhages spontaneously resolved without any specific sequelae. Some domestic scholars[14]-[16] reported that neonatal retinal hemorrhage was related to the mode of delivery and the severity of suffocation and macula flava hemorrhage would influence the vision development in the long run. Intraretinal hemorrhages are common in the immediate postnatal period and resolve by 1 month of age. Retinal hemorrhage in infants older than 1 month should heighten suspicion that the hemorrhage is associated with factors other than birth[17].
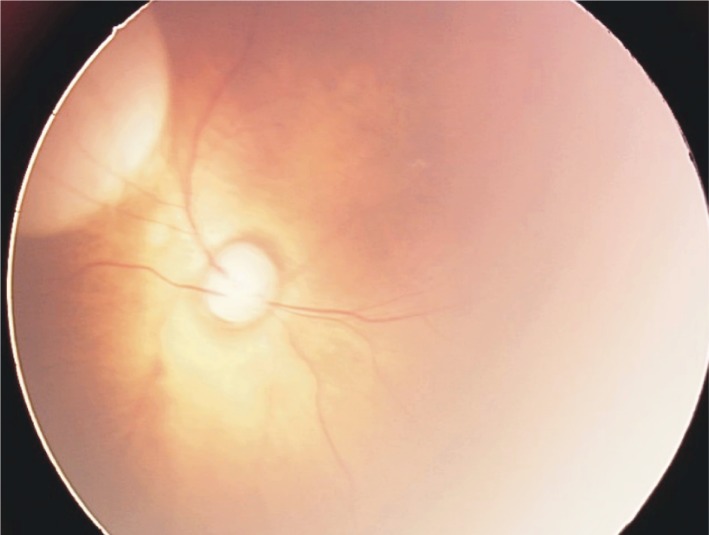
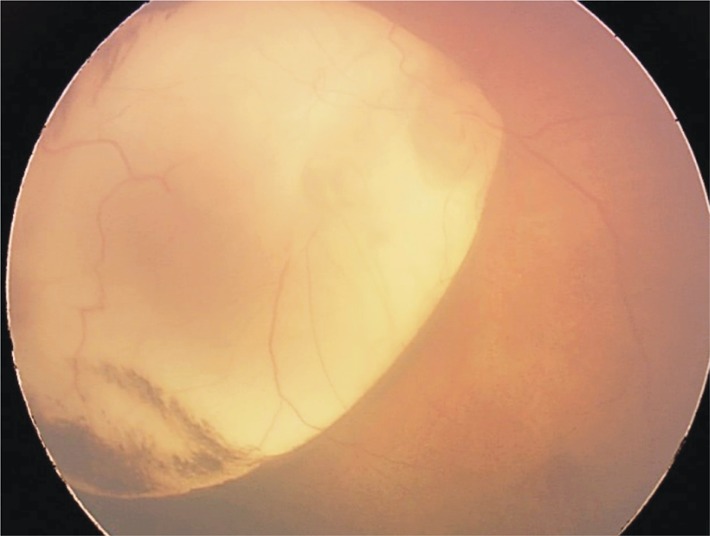
Choroidal coloboma is an inferiorly located congenital lesion characterized by absence of the normal retina, retinal pigment epithelium, and choroids. With the RetCam II, the defects of the choroid and retina are visible clearly. Choroidal colobomas are often associated with syndromes such as CHARGE association, Aicrdi's syndrome, and Goldenhar's syndrome. Posterior polar chorioretinal scarring is a pigmentary disturbance often caused by intrauterine toxoplasmosis[18]. Choroidal neovascularization (CNV) is a rare complication associated with coloboma of the choroid. CNV occurrence in choroidal colobomas is believed to be due to preexisting anomalies at the border of the coloboma where there is thickened and folded Retinal pigment epithelium (RPE), retina is atrophic and the barrier function of Bruch's membrane is disrupted. CNV though rare, assumes importance when the good eye of the patient is involved. Management of CNV in these eyes does not differ from that of CNV due to other causes. Laser photocoagulation, transpupillary thermotherapy (TTT), photodynamic therapy (PDT) and surgery have been reported[19]. Figure 1-3 showed the coloboma of the choroid in the three patients.
Figure 1. Coloboma of the choroid in the macula zone in the right eye, about 1.5 PD.
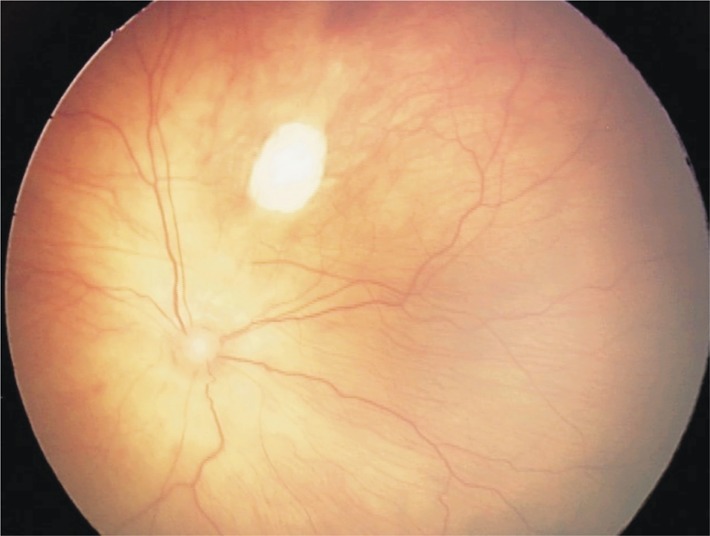
Figure 3. Choroidal coloboma in the macula zone with neovascularization, about 5 PD.
Figure 2. Posterior polar chorioretinal coloboma with choroidal neovascularization, about 10 PD.
In conclusion, early detection and prompt treatment of ocular disorders in infants is important to avoid lifelong visual impairment. Examination of the eyes should be performed beginning in the newborn period and at all well-child visits. And Ret Cam II is a crucial tool for the neonatal fundal examination, not only in the screening of ROP, but also used in screening of ocular disease.
Footnotes
Foundation item: Guangdong Provincial Science and Technology Projects, China(No. 2011B031800105)
REFERENCES
- 1.Eye examination in infants, children, and young adults by pediatricians: organizational principles to guide and define the child health care system and/or improve the health of all children. Ophthalmology. 2003;110(4):860–865. doi: 10.1016/S0161-6420(03)00414-7. [DOI] [PubMed] [Google Scholar]
- 2.Tasman W. Retinopathy of prematurity: do we still have a problem? the Charles L. Schepens lecture. Arch Ophthalmol. 2011;129(8):1083–1086. doi: 10.1001/archophthalmol.2011.192. [DOI] [PubMed] [Google Scholar]
- 3.Austeng D, Kallen KB, Ewald UW, Jakobsson PG, Holmström GE. Incidence of retinopathy of prematurity in infants born before 27 weeks' gestation in Sweden. Arch Ophthalmol. 2009;127(10):1315–1319. doi: 10.1001/archophthalmol.2009.244. [DOI] [PubMed] [Google Scholar]
- 4.Ebrahim M, Ahmad RS, Mohammad M. Incidence and risk factors of retinopathy of prematurity in Babol, North of Iran. Ophthalmic Epidemiol. 2010;17(3):166–170. doi: 10.3109/09286581003734860. [DOI] [PubMed] [Google Scholar]
- 5.Lad EM, Nguyen TC, Morton JM, Moshfeghi DM. Retinopathy of prematurity in the United States. Br J Ophthalmol. 2008;92(3):320–325. doi: 10.1136/bjo.2007.126201. [DOI] [PubMed] [Google Scholar]
- 6.Akman I, Demirel U, Yenice O, Ilerisoy H, Kazokoğlu H, Ozek E. Screening criteria for retinopathy of prematurity in developing countries. Eur J Ophthalmol. 2010;20(5):931–937. doi: 10.1177/112067211002000519. [DOI] [PubMed] [Google Scholar]
- 7.Huang XL, Zhang Y, Yang J, Luo XQ. Clinical analysis of the retinopathy of prematurity after criterion oxygen-treatment. Int J Ophthalmol (Guoji Yanke Zazhi) 2009;9(4):693–694. [Google Scholar]
- 8.Gu MH, Jin J, Yuan TM, Yu HM. Risk factors and outcomes for retinopathy of prematurity in neonatal infants with a birth weight of 1,501-2,000 g in a Chinese Neonatal Unit. Med Princ Pract. 2011;20(3):244–247. doi: 10.1159/000323764. [DOI] [PubMed] [Google Scholar]
- 9.Li WL, He L, Liu XH, Wang YM, Liu JQ. Analysis of risk factors for retinopathy of prematurity. Int J Ophthalmol. 2011;4(6):631–633. doi: 10.3980/j.issn.2222-3959.2011.06.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Good WV. Final results of the Early Treatment for Retinopathy of Prematurity (ETROP) randomized trial. Trans Am Ophthalmol Soc. 2004;102:233–48, 248-250. [PMC free article] [PubMed] [Google Scholar]
- 11.Kaur B, Taylor D. Fundus hemorrhages in infancy. Surv Ophthalmol. 1992;37(1):1–17. doi: 10.1016/0039-6257(92)90002-b. [DOI] [PubMed] [Google Scholar]
- 12.Hughes LA, May K, Talbot JF, Parsons MA. Incidence, distribution, and duration of birth-related retinal hemorrhages: a prospective study. J AAPOS. 2006;10(2):102–106. doi: 10.1016/j.jaapos.2005.12.005. [DOI] [PubMed] [Google Scholar]
- 13.Choi YJ, Jung MS, Kim SY. Retinal hemorrhage associated with perinatal distress in newborns. Korean J Ophthalmol. 2011;25(5):311–316. doi: 10.3341/kjo.2011.25.5.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Fan Zh, Liang CP, Yun SJ. Clinical analysis of retinal hemerrhage in the newborn. Chinese J Strabismus Pediatr Ophthalmol. 2003;11(03):106–108. [Google Scholar]
- 15.Huang XH, Yu J, Xiong K, Zong JH, Tan Q. Observation of neonatal retinal haemorrhage with distress in utero. Int J Ophthalmol(Guoji Yanke Zazhi) 2009;9(1):83–84. [Google Scholar]
- 16.Tan ZX, Li RQ, Chen ZF, Di XH. Analysis of relative factors for retinal hemorrhage in preterms. Guangdong Yixueyuan Xuebao. 2011;29(4):451–452. [Google Scholar]
- 17.Emerson MV, Pieramici DJ, Stoessel KM, Berreen JP, Gariano RF. Incidence and rate of disappearance of retinal hemorrhage in newborns. Ophthalmology. 2001;108(1):36–39. doi: 10.1016/s0161-6420(00)00474-7. [DOI] [PubMed] [Google Scholar]
- 18.PaulRiordan-Eva JohnP. Beijing: Peolples's Military Publisher; 2011. Vaughan&Asbury's General Ophthalmology; p. 422. [Google Scholar]
- 19.Bhende M, Suganeswari G, Gopal L, Bhende PS, Gopal L, Rao C. Choroidal neovascularization associated with coloboma of the choroid: a series of three cases. Indian J Ophthalmol. 2011;59(2):148–151. doi: 10.4103/0301-4738.77043. [DOI] [PMC free article] [PubMed] [Google Scholar]