Abstract
Aim
To determine the extent of Turkish junior male physicians’ exposure to mobbing behavior and its correlation with physicians' characteristics.
Methods
The study included physicians recruited for compulsory military service in April 2009. No sampling method was used, questionnaires were delivered to all physicians, and 278 of 292 (95%) questionnaires were returned. We used Leymann Inventory of Psychological Terror including 45 items for data collection and structural equation model for data analysis.
Results
A total of 87.7% of physicians experienced mobbing behavior. Physicians who worked more than 40 hours a week, single physicians, physicians working in university hospitals and private hospitals, and physicians who did not have occupational commitment were more exposed to mobbing (P < 0.05). Mobbing was not associated with specialty status, service period, age, and personality variables (P > 0.05). All goodness-of- fit indices of the model were acceptable (χ2 = 1.449, normed fit index = 0.955, Tucker Lewis index = 0.980, comparative fit index = 0.985, and root mean square error of approximation = 0.040).
Conclusions
Workplace mobbing is a critical problem for junior male physicians in Turkey. We suggest an introduction of a reporting system and education activities for physicians in high-risk groups.
Mobbing has been shown to negatively affect the welfare and development of workers and organizations by increasing the rates of leave and absenteeism, lowering the morale, and causing anger, burnout, underperformance, and deterioration of corporate image and relationships among workers (1-5).
To minimize the number of cases, the issue of mobbing must first be thoroughly investigated (6). Although no definition has been generally accepted, mobbing usually refers to actions when someone is subjected to social isolation or exclusion, when their work and efforts are devaluated, and when they are threatened, worn down, or frustrated (7-10). The International Labour Organization (ILO) has defined the term as acting in unison against a coworker and exposing that individual to psychological harassment (11). The term mobbing has been used synonymously with suppression, attack, violence, bullying, psychological harassment, social isolation, threatening, and discrimination in the business life, and workplace trauma (12-14).
Mobbing has become a major problem in the health and other sectors (15-19). In the health sector, it can be increased by 24-hour service provision and intense work pace and correlates negatively with job satisfaction and performance, posing a threat to patients' safety (20-22).
In the ILO’s report from 2002, the health sector workers’ rate of exposure to mobbing in the USA has been sixteen times higher than in other sectors. More than half of the health personnel in different countries has in the previous year experienced at least one incident of physical or psychological violence (23,24). Although, there is no national study investigating the prevalence of mobbing in the health sector in Turkey, there have been some local studies focusing on the limited number of female nurses, indicating that mobbing is an important issue (25-28).
Although there are several studies on physicians’ exposure to mobbing, none of these investigated male physicians because it is generally thought that women are more often subjected to mobbing (29-33). However, negative and discomforting acts and interactions may not only be of a sexual nature or be solely directed toward women (9). This study aimed to determine the extent of junior male physicians’ exposure to mobbing behavior and to investigate its association with physicians’ characteristics.
Participants and methods
Sample
The research included 292 male physicians who started compulsory military service in the Ministry of Defense Samsun Military Medical Command in April 2009. All physicians gave informed consent and the participation was voluntary. A total of 278 (95%) questionnaires were returned.
Data collection
To assess mobbing behavior, we used the Leymann Inventory of Psychological Terror (LIPT) scale, including 45 mobbing behavior types (7). The scale has 45 items classified into five dimensions: the items 1-11 refer to “behavior threatening communication,” the items 12-16 refer to “behavior threatening social contacts,” the items 17-31 refer to “behavior threatening personal reputation,” the items 32-40 refer to “behavior threatening occupational situation,” and the items 41-45 refer to “behavior threatening physical health.”
Frequency of exposure to mobbing is assessed with the following scores: 1 – every day, 2 – a few times a week, 3 – a few times a month, 4 – a few times a year, and 5 – never. Exposure to even one of the 45 types of behavior is enough to classify the participant as a victim of mobbing (7). The exposure to mobbing is assessed subjectively based on participants’ views and perceptions, but since the LIPT scale had been used in several previous studies (7,27,34,35) and its validity and reliability had been assessed, it was deemed suitable for the purposes of this study.
The participants who selected the answers between “every day” and “a few times a year” were united and classified as “people who were exposed to mobbing,” whereas the participants who selected “never” were classified as “people who were not exposed to mobbing” (1).
The reliability score for behavior threatening communication was 0.87, for behavior threatening social contacts 0.71, for behavior threatening personal reputation 0.90, for behavior threatening occupational situation 0.89, for behavior threatening physical health 0.74, and the general reliability value was 0.95.
Data analysis
To analyze the questionnaire data, SPSS, version 14.0 (SPSS Inc., Chicago, IL, USA) and AMOS, version 6.0 (Amos Development Corporation, Spring House, PA, USA), software programs were used. While descriptive statistics was used to present the percentage of participants’ exposure to mobbing behavior, structural equation model (SEM) was used as a multivariate statistical method to determine the factors (physicians characteristics) affecting the level of exposure to mobbing behavior (36-38).
Structural equation model
SEM encompasses two major components: measurement and structural model. The measurement model establishes the relationships between latent (unobserved) variables and multiple observable items. This is the confirmatory factor analysis portion of a model. The structural model tests a set of hypothesized associations between two or more variables. It includes a set of paths (regression coefficients) or correlations between the various measured and unmeasured variables in the overall model (36-41).
In this research, in order to obtain the model that best explains whether there was a significant relation between the level of physicians’ exposure to mobbing behavior and their characteristics, two models were developed and tested. The first used 19 variables, 8 of which were independent variables reflecting the physicians’ sociodemographic characteristics (work place [1 = Ministry of Health hospital, 2 = university hospital, 3 = private hospital], marital status [1 = married, 2 = single], specialty status [1 = practitioner, 2 = specialist physician], number of working hours per week [1 = 40 hours, 2 = 41-56 hours, 3 = 57 hours and more], age [years], duration of work [years], occupational commitment [1 = yes, 2 = no], and personality [1 = ambitious, 2 = emotional, 3 = passive]). Five variables (behavior threatening communication, behavior threatening social contacts, behavior threatening personal reputation, behavior threatening occupational situation, and behavior threatening physical health) were observed indicator variables and another five were unexplained indicators. Finally, the last variable was mobbing, which was the latent dependent variable. The second, revised, model used only four of socio-demographic characteristics that were found significant.
There are various indices to evaluate the goodness of fit of SEM. Most commonly used are χ2 value, comparative fit index (CFI), normed fit index (NFI), Tucker-Lewis index (TLI), and root-mean-square error approximation (RMSEA) (40).
A high χ2 value indicates that the model fit is poor; as it is dependent on sample size and both observed and expected covariance matrix, it has only a limited use. As the sample size increases with the residual covariance matrix, the χ2 value and the probability for rejecting the model will increase (42). Frequently used CFI, NFI, and TLI fitness measures have values between 0 and 1, with values closer to 1 indicating better fitness (36). For RMSEA, it has been argued that values less than or equal to 0.05 indicate excellent fit, between 0.08 and 0.10 indicate acceptable fit, and higher values indicate unacceptable fit (41).
Results
The mean age and service period of male physicians were 32.4 ± 2.5 years and 5.3 years ±2.9, respectively (Table 1). More than a half of the physicians (72.4%) were serving in hospitals affiliated to the Ministry of Health and the remaining were working in university and private hospitals. All of them were civilian physicians doing military service, rather than military personnel. A total of 18.3% had an administrative position such as head physician and vice head physician, 68.1% were married, 71.9% were specialist physicians, 71.7% worked more than 40 hours a week, 67% defined themselves as ambitious and hardworking, and 10.8% did not like medical profession (Table 1).
Table 1.
Personal characteristics of Turkish male physicians doing military service
| Personal characteristics | No. (%) of physicians |
|---|---|
|
Age in years (mean±standard deviation) |
32.4 ± 2.5 |
|
Service period in years (mean±standard deviation) |
5.3 ± 2.9 |
|
Administrative position: |
|
| yes |
51 (18.3) |
| no |
228 (81.7) |
|
Place of work: |
|
| Ministry of Health hospitals |
202 (72.4) |
| university hospitals |
42 (15.1) |
| private hospitals |
35 (12.5) |
|
Marital status: |
|
| married |
190 (68.1) |
| single |
89 (31.9) |
|
Specialty: |
|
| practitioner |
78 (28.1) |
| specialist |
200 (71.9) |
|
Weekly working hours: |
|
| 40 h |
79 (28.3) |
| 41-56 h |
126 (45.2) |
| 57 h and more |
74 (26.5) |
|
Personality: |
|
| ambitious and hardworking |
188 (67.4) |
| emotional |
68 (24.4) |
| passive |
23 (8.2) |
|
Occupational commitment: |
|
| yes |
248 (89.2) |
| no | 30 (10.8) |
A total of 87.7% of 278 participants were exposed to at least one of the 45 types of mobbing behavior defined in the questionnaire: 79.5%, reported “behavior threatening communication,” 64.7% reported “behavior threatening personal reputation,” 57.2% reported “behavior threatening occupational situation,” 48.9% reported “behavior threatening social contacts,” and 31.3% reported “behavior threatening physical health” (Table 2) (Figure 1).
Table 2.
Mobbing behavior experienced by male physicians
| Mobbing behaviors | Mean | Standard deviation | Non-victims |
victims |
||||
|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | |||||
|
Behavior threatening communication |
4.4 |
0.6 |
57 |
20.5 |
221 |
79.5 |
||
| 1. The aggressor or mobber gives the victim no possibility to communicate |
4.1 |
1.1 |
136 |
48.9 |
142 |
51.1 |
||
| 2. The victim is silenced or continuously interrupted |
4.1 |
1.1 |
132 |
47.5 |
146 |
52.5 |
||
| 3. Colleagues prevent the victim to communicate |
4.2 |
0.9 |
138 |
49.6 |
140 |
50.4 |
||
| 4. Colleagues scream and shout at the victim |
4.6 |
0.8 |
201 |
72.3 |
77 |
27.7 |
||
| 5. The victim suffers verbal attacks regarding work assignments |
4.3 |
0.9 |
142 |
51.1 |
136 |
48.9 |
||
| 6. The victim suffers verbal attacks regarding her/his personal life |
4.7 |
0.7 |
216 |
77.7 |
62 |
22.3 |
||
| 7. The victim is terrorized by means of phone calls |
4.3 |
1.1 |
173 |
62.2 |
105 |
37.8 |
||
| 8. The victim suffers verbal threats |
4.6 |
0.7 |
204 |
73.4 |
74 |
26.6 |
||
| 9. The victim suffers written threats |
4.9 |
0.4 |
255 |
91.7 |
23 |
8.3 |
||
| 10. People at work refuse to make any contact with the victim |
4.5 |
0.8 |
173 |
62.2 |
105 |
37.8 |
||
| 11. The victim's presence is ignored |
4.5 |
0.8 |
172 |
61.9 |
106 |
38.1 |
||
|
Behavior threatening social contacts |
4.7 |
0.5 |
142 |
51.1 |
136 |
48.9 |
||
| 12. The aggressor does not talk to the victim |
4.8 |
0.5 |
223 |
80.2 |
55 |
19.8 |
||
| 13. The victim is forbidden to talk to the aggressor |
4.8 |
0.6 |
232 |
83.5 |
46 |
16.5 |
||
| 14. The victim is isolated in a room far away from others |
4.3 |
1.4 |
208 |
74.8 |
70 |
25.2 |
||
| 15. Colleagues are forbidden to talk to the victim |
4.9 |
0.5 |
261 |
93.9 |
17 |
6.1 |
||
| 16. The physical presence of the victim is denied |
4.7 |
0.7 |
220 |
79.1 |
58 |
20.9 |
||
|
Behavior threatening personal reputation |
||||||||
| 17. Slanders and lies about the victim are used at work |
4.4 |
0.8 |
158 |
56.8 |
120 |
43.2 |
||
| 18. The victim is gossiped |
4.4 |
0.8 |
159 |
57.2 |
119 |
42.8 |
||
| 19. The victim is ridiculed |
4.7 |
0.6 |
222 |
79.9 |
56 |
20.1 |
||
| 20. The victim is said to have a mental illness |
4.9 |
0.4 |
266 |
95.7 |
12 |
4.3 |
||
| 21. The aggressor tries to make the victim go through psychiatric exams |
4.9 |
0.3 |
266 |
95.7 |
12 |
4.3 |
||
| 22. The victim is supposed to be ill |
4.8 |
0.5 |
242 |
87.1 |
36 |
12.9 |
||
| 23. The victim's voice, gestures, and way of moving are imitated |
4.8 |
0.6 |
230 |
82.7 |
48 |
17.3 |
||
| 24. The victim suffers verbal attacks regarding her/his political and religious beliefs |
4.8 |
0.5 |
234 |
84.2 |
44 |
15.8 |
||
| 25. People at work make fun of the victim's personal life |
4.8 |
0.5 |
238 |
85.6 |
40 |
14.4 |
||
| 26. People at work make fun about the ethnic origin or nationality of the victim |
4.9 |
0.4 |
262 |
94.2 |
16 |
5.8 |
||
| 27. The victim is forced to do humiliating jobs |
4.8 |
0.6 |
234 |
84.2 |
44 |
15.8 |
||
| 28. The victim is controlled and his/her job performance is tracked for those with bad intentions |
4.7 |
0.6 |
208 |
74.8 |
70 |
25.2 |
||
| 29. Victim's decisions are questioned |
4.5 |
0.7 |
177 |
63.7 |
101 |
36.3 |
||
| 30. The victim is reviled using obscene or degrading terms |
4.9 |
0.5 |
260 |
93.5 |
18 |
6.5 |
||
| 31. The victim is sexually harassed |
4.9 |
0.4 |
260 |
93.5 |
18 |
6.5 |
||
|
Behavior threatening occupational situation |
4.7 |
0.5 |
119 |
42.8 |
159 |
57.2 |
||
| 32. The victim is not given any work assignments at all |
4.7 |
0.7 |
219 |
78.8 |
59 |
21.2 |
||
| 33. The victim is deprived of any activity when being at work |
4.8 |
0.5 |
236 |
84.9 |
42 |
15.1 |
||
| 34. The victim is given meaningless work assignments |
4.6 |
0.7 |
188 |
67.6 |
90 |
32.4 |
||
| 35. The victim is given work assignments far below her/his capacity |
4.4 |
0.9 |
172 |
61.9 |
106 |
38.1 |
||
| 36. The victim is continuously given new work assignments |
4.7 |
0.6 |
224 |
80.6 |
54 |
19.4 |
||
| 37. The victim is given humiliating work assignments |
4.6 |
0.8 |
210 |
75.5 |
68 |
24.5 |
||
| 38. The victim is given difficult work assignments far above her/his capacity |
4.7 |
0.7 |
228 |
82.0 |
50 |
18.0 |
||
| 39. The victim is deliberately forced to spend big sums of money |
4.7 |
0.7 |
209 |
75.2 |
69 |
24.8 |
||
| 40. Accidents are caused in the victim's workplace or home |
4.9 |
0.4 |
261 |
93.9 |
17 |
6.1 |
||
|
Behavior threatening physical health |
4.8 |
0.4 |
191 |
68.7 |
87 |
31.3 |
||
| 41. The victim is given dangerous work assignments |
4.6 |
0.9 |
207 |
74.5 |
71 |
25.5 |
||
| 42. The victim is physically threatened |
4.8 |
0.5 |
245 |
88.1 |
33 |
11.9 |
||
| 43. The victim is physically attacked as a threat |
4.9 |
0.5 |
251 |
90.3 |
27 |
9.7 |
||
| 44. The victim is physically attacked with serious consequences for his/her health |
4.9 |
0.3 |
264 |
95.0 |
14 |
5.0 |
||
| 45. The victim is sexually attacked |
5.0 |
0.3 |
272 |
97.8 |
6 |
2.2 |
||
| Overall mobbing | 34 | 12.3 | 244 | 87.7 | ||||
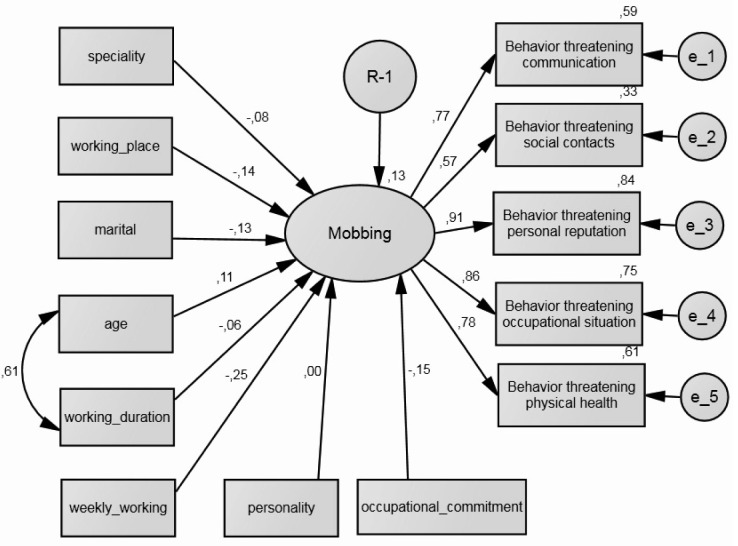
Figure 1.
The measurement model identifying physicians’ exposure to mobbing behavior. χ2/df = 12.865/5 = 2.573; normed fit index = 0.984; Tucker Lewis index = 0.980; comparative fit index = 0.990; and root mean square error of approximation = 0.075. Rectangles represent independent and indicator variables and ellipses represent latent variables. The arrows from latent variables to indicators show regression and indicator weights. The error for each variable is represented by the arrow pointing to the variable and “e” in the circle. These errors correspond to the errors in the indicator variables.
The measurement model shows the validity of the LIPT scale used to determine the level of male physicians’ exposure to mobbing behavior (Figure 1). To show whether the suggested model was compatible with the research data, a confirmatory factor analysis was conducted. As the standardized regression parameter values of five dimensions were higher than 0.50 (between 0.573-0.915), and all dimensions significantly related to the latent variable for mobbing (P < 0.001), it was accepted that the suggested measurement model was compatible with the research data and it had convergent validity. Furthermore, confirmatory factor analysis (Table 3) showed that mobbing behavior threatening occupational status and social contacts had more weight to explain the latent variable of mobbing. In other words, these dimensions best explained the variance in latent variable. On the other hand, the goodness-of-fit criteria of the measurement model were acceptable, except for the χ2 value, which was sensitive to the size of the sample (χ2 = 2.573, NFI = 0.984, TLI = 0.980, CFI = 0.990, and RMSEA = 0.075) (Figure 2).
Table 3.
Regression coefficients of the measurement model identifying male physicians’ exposure to mobbing behavior
| Standardized regression coefficients | Standard error | t test | P | |
|---|---|---|---|---|
| Behavior threatening communication |
0.763 |
0.051 |
14.609 |
<0.001 |
| Behavior threatening social contacts |
0.573 |
0.062 |
9.474 |
<0.001 |
| Behavior threatening personal reputation |
0.915 |
0.048 |
16.260 |
<0.001 |
| Behavior threatening occupational situation |
0.864 |
0.063 |
15.032 |
<0.001 |
| Behavior threatening physical health | 0.777 | 0.049 | 13.368 | <0.001 |
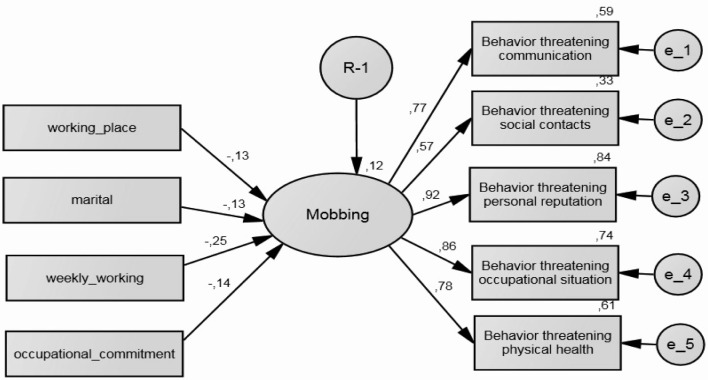
Figure 2.
The initial structural equation model identifying determinants of the physicians’ exposure to mobbing behavior. χ2/df = 282.611/64 = 4.416; normed fit index = 0.771; Tucker Lewis index = 0.728; comparative fit index = 0.809; root mean square error of approximation = 0.111. Rectangles represent independent and indicator variables and ellipses represent latent variables. The arrows from latent variables to indicators show regression and indicator weights. The error for each variable is represented by the arrow pointing to the variable and “e” in the circle. These errors correspond to the errors in the indicator variables.
The next step was to determine which independent variables influenced the extent of exposure to mobbing (Figure 2). In the initial structural equation model, eight personal characteristics were used as the explanatory variable: specialty status, working place, marital status, age, service period, weekly working hours, personality and occupational commitment. Working place (t = -2.226; P = 0.023), marital status (t = -2.103; P = 0.035), weekly working hours (t = -4.007; P = <0.001), and occupational commitment (t = -2.504; P = 0.012) significantly affected the extent of exposure to mobbing (Table 4), while specialty status, service period, age, and personality variables did not (P > 0.05). Moreover, the goodness-of-fit criteria of the suggested initial structural equation model pointed out that the model was not within acceptable limits (χ2 = 4.416, NFI = 0.771, TLI = 0.728, CFI = 0.809, and RMSEA = 0.111).
Table 4.
Regression coefficients of the initial structural equation model estimating determinants of the physicians’ exposure to mobbing behavior
| Standardized regression coefficients | Standard error | t test | P | |
|---|---|---|---|---|
| Working place |
-0.137 |
0.060 |
-2.266 |
0.023 |
| Marital status |
-0.134 |
0.061 |
-2.103 |
0.035 |
| Specialty status |
-0.084 |
0.077 |
-1.096 |
0.273 |
| Service period |
-0.061 |
0.013 |
-.753 |
0.451 |
| Age |
0.109 |
0.015 |
1.272 |
0.203 |
| Weekly working hours |
-0.246 |
0.037 |
-4.007 |
<0.001 |
| Personality |
-0.001 |
0.042 |
-.013 |
0.989 |
| Occupational commitment | -0.152 | 0.088 | -2.504 | 0.012 |
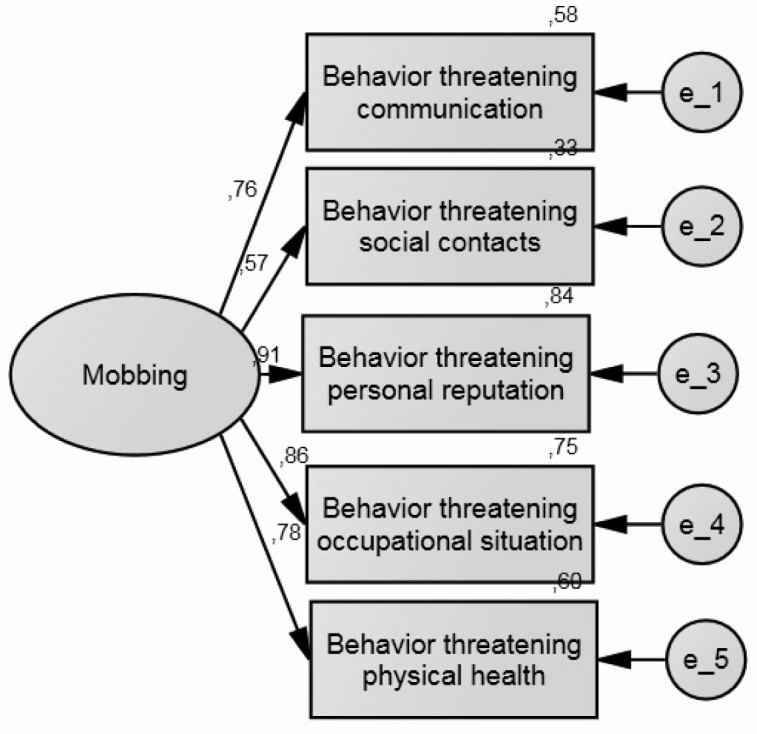
The four independent variables that were proven to be non-significant in the initial structural equation model were excluded and a revised new structural equation model was constituted (Figure 3) to achieve higher goodness-of-fit values and higher compatibility of the model to the data (Table 5).
Figure 3.
The revised structural equation model identifying determinants of the physicians’ exposure to mobbing behavior. χ2/df = 39.135/27 = 1.449; normed fit index = 0.955; Tucker Lewis index = 0.980; comparative fit index = 0.985; root mean square error of approximation = 0.040.
Table 5.
Regression coefficients of the revised structural equation model estimating determinants of the physicians’ exposure to mobbing behavior
| Standardized regression coefficients | Standard error | t test | P | |
|---|---|---|---|---|
| Weekly working hours |
-0.252 |
0.037 |
-4.135 |
<0.001 |
| Working place |
-0.132 |
0.059 |
-2.207 |
0.027 |
| Marital status |
-0.132 |
0.057 |
-2.216 |
0.027 |
| Occupational commitment | -0.141 | 0.086 | -2.362 | 0.018 |
The revised and improved model showed that the four independent variables (weekly working hours, marital status, working place, and occupational commitment) had a significant influence on mobbing (Table 5). Physicians who worked more than 40 hours a week, single physicians, and physicians working in university hospitals and private hospitals were more likely to be exposed to mobbing. A negative relationship was found between occupational commitment and exposure to mobbing – physicians who did not have occupational commitment were more exposed to mobbing.
The goodness-of-fit indices of the revised structural equation model increased significantly in comparison with the initial structural equation model, and all indices were within acceptable limits (χ2 = 1.449, NFI = 0.955, TLI = 0.980, CFI = 0.985, and RMSEA = 0.040). Therefore, as goodness-of-fit values improved, the model was adopted as the final model. Total explanatory coefficient of the model was 12%. In other words, four independent variables that were found to be significant in the revised structural equation model were able to clarify only 12% of the variance of physicians’ level of exposure to mobbing (Table 5).
Discussion
Our study showed that almost nine of ten physicians had a mobbing experience in the previous year and the frequency of mobbing exposure was higher than in other studies (2,11,19,22,24,43-45). These differences may be a result of the use of different mobbing definitions, scales, recall periods (46,47), settings (48-50), and participants (physicians or nurses) (28,43,51-55).
In this study, the most common mobbing behavior was “behavior threatening communication” and the least common was “behavior threatening physical health.” “Behavior threatening communication” was the most common mobbing behavior in other studies on health workers (16,19,27,43,53,56).
Another interesting finding was that the extent of exposure to mobbing was higher in the university hospitals and private hospitals than in the Ministry of Health hospitals, similar as in the study by Sahin and Dundar (27). This could be attributed to the greater complexity of university hospitals and a more stressful working environment (45,47).
While most of the mobbing victims in this study were single, in the study by Kowalczuk et al (57) they were mostly married. Greater exposure of single physicians to mobbing can be explained by their younger age and lack of experience. Also, married physicians can be positively discriminated in terms of lower work load, especially working the night shifts. We also found that physicians working more than 40 hours were exposed to mobbing more than those working less than 40 hours. This could be attributed to the hectic work environment that paves the way for mobbing, or working more than others might be regarded as unfair and as mobbing behavior. Finally, we also found that physicians who did not show occupational commitment complained about mobbing behavior more than those showing occupational commitment. This can be explained by a greater exposure to mobbing of physicians without occupational commitment or loss of occupational commitment in physicians exposed to mobbing.
As this study is a descriptive study of physicians doing compulsory military service, the results cannot be generalized to all male physicians. Also, due to study design we were not able to determine the causal relationship between the variables. Also, a recall bias might have occurred because physicians had to report their experiences in the past year and some of the physicians may not have wanted to share their personal experience. Cowie et al (58) found that questionnaire formats were not sufficient in investigating mobbing. Another limitation was that four variables (working place, marital status, weekly working hours and occupational commitment) that had significant effects on the frequency of exposure to mobbing explained only 12% of variance. The advantage of this study is the use of SEM, which is a multivariate statistical analysis method.
In conclusion, we found that the physicians working in university or private hospitals, working more than 40 hours in a week, single physicians and those without professional commitment were more exposed to mobbing. In order to take proper preventive measures against mobbing, its exact causes must be determined and legal regulations should be introduced. Health care providers should also be informed about mobbing and their legal rights. Thus, hospital department heads must monitor the development of mobbing behavior, come up with solutions by making a risk analysis, and provide an environment in which employees are able to express their complaints.
Acknowledgments
Funding None.
Ethical approval Not required.
Declaration of authorship All authors contributed to design, data collection, analyses, and writing and revision of the manuscript.
Competing interests All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
References
- 1.Kivimaki M, Elovainio M, Vahtera J. Workplace bullying and sickness absence in hospital staff. Occup Environ Med. 2000;57:656–60. doi: 10.1136/oem.57.10.656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Quine L. Workplace bullying in NHS community trust: staff questionnaire survey. BMJ. 1999;318:228–32. doi: 10.1136/bmj.318.7178.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zapf D, Escartín J, Einarsen S, Hoel H, Vartia M. Empirical findings on the prevalence rate and risk groups of bullying in the workplace. In Einarsen S, Hoel HD, Zapf, CL. Cooper, editors. Bullying and harassment in the workplace: Developments in theory, research, and practice, 2nd ed. London: Taylor & Francis. 2010. p. 75-105. [Google Scholar]
- 4.Neuman JH, Baron RA. Aggression in the workplace: a social-psychological perspective. In: Fox S, Spector P, editors. Counterproductive work behavior: investigations of actors and targets. Washington, DC: American Psychological Association; 2005. p. 13-40. [Google Scholar]
- 5.Merecz D, Rymaszewska J, Moscicka A, Kiejna A. Jarosz- Norwak J. Violence at the workplace – a questionnaire survey of nurses. Eur Psychiatry. 2006;21:442–50. doi: 10.1016/j.eurpsy.2006.01.001. [DOI] [PubMed] [Google Scholar]
- 6.Einarsen S, Skogdstad A. Bullying at work: Epidemiological findings in public and private organizations. European Journal of Work and Organizational Psychology. 1996;5:185–201. doi: 10.1080/13594329608414854. [DOI] [Google Scholar]
- 7.Leymann H. The content and development of mobbing at work. European Journal of Work and Organizational Psychology. 1996;5:165–84. doi: 10.1080/13594329608414853. [DOI] [Google Scholar]
- 8.Einarsen S. The nature and causes of bullying at work. International Journal of Manpower. 1999;20:16–27. doi: 10.1108/01437729910268588. [DOI] [Google Scholar]
- 9.Einarsen S, Raknes BI. Harassment in the workplace and victimization of men. Violence Vict. 1997;12:247–63. [PubMed] [Google Scholar]
- 10.Ghasemi M, Rezaee M, Jafari NJ, Ashtiani AF, Izadi M, Ranjbar R. Physical violence against nurses in hospital. International Journal of Occupational Hygiene. 2009;1:43–7. [Google Scholar]
- 11.ILO/ICN/WHO/PSI. Framework guidelines for addressing workplace violence in the health sector. Geneva: International Labour Office 2002. Available from: http://www.who.int/violence_injury_prevention/violence/interpersonal/en/WVguidelinesEN.pdf Accessed: June 18, 2012.
- 12.Godin IM. Bullying, worker’s health, and labor instability. J Epidemiol Community Health. 2004;58:258–9. doi: 10.1136/jech.2003.009456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zapf D, Einarsen S. Bullying in the workplace: Recent trends in research and practice – an introduction. European Journal of Work and Organizational Psychology. 2001;10:369–73. doi: 10.1080/13594320143000807. [DOI] [Google Scholar]
- 14.Farrell GA, Bobrowski C, Bobrowski P. Scoping workplace aggression in nursing: Findings from an Australian study. J Adv Nurs. 2006;55:778–87. doi: 10.1111/j.1365-2648.2006.03956.x. [DOI] [PubMed] [Google Scholar]
- 15.Jones J, Lyneham J. Violence: part of the job for Australian nurses. Aust J Adv Nurs. 2000;18:27–32. [PubMed] [Google Scholar]
- 16.Lyneham J. Workplace violence in New South Wales Emergency Departments. Australian Emergency Nursing Journal. 2001;4:5–9. doi: 10.1016/S1328-2743(01)80013-4. [DOI] [PubMed] [Google Scholar]
- 17.Mayhew C, Chappell D. Violence in the work place. Med J Aust. 2005;183:346–7. doi: 10.5694/j.1326-5377.2005.tb07080.x. [DOI] [PubMed] [Google Scholar]
- 18.Beech B, Leather P. Workplace violence in the health care sector: a review of staff training and integration of training evaluation models. Aggress Violent Behav. 2005;11:27–43. doi: 10.1016/j.avb.2005.05.004. [DOI] [Google Scholar]
- 19.Ryan D, Maguire J. Aggression and violence. A problem in Irish and emergency departments? J Nurs Manag. 2006;14:106–15. doi: 10.1111/j.1365-2934.2006.00571.x. [DOI] [PubMed] [Google Scholar]
- 20.Kwok RPW, Law YK, Li KE, Ng YC, Cheung MH, Fung VKP, et al. Prevalence of workplace violence against nurses in Hong Kong. Hong Kong Med J. 2006;12:6–9. [PubMed] [Google Scholar]
- 21.Hesketh KL, Duncan SM, Estabrooks CA, Reimer MA, Giovannetti P, Hyndman K, et al. Workplace violence in Alberta and British Columbia Hospitals. Health Policy. 2003;63:311–21. doi: 10.1016/S0168-8510(02)00142-2. [DOI] [PubMed] [Google Scholar]
- 22.Josipovic-Jelic Z, Stoini E, Celic-Bunikic S. The effect of mobbing on medical staff performance. Acta Clin Croat. 2005;44:347–52. [Google Scholar]
- 23.Di Martino V. Workplace violence in the health sector- Country case studies Brazil, Bulgaria, Lebanon, Portugal, South Africa, Thailand, plus an additional Australian Study: Synthesis report. Geneva: ILO/ICN/WHO/PSI Joint programme on workplace violence in the health sector, 2002. Available from: http://www.who.int/violence_injury_prevention/violence/activities/workplace/WVsynthesisreport.pdf Accessed: July 3, 2012.
- 24.Hubert AB, Veldhoven M. Risk sectors for undesirable behavior and mobbing. European Journal of Work and Organizational Psychology. 2001;10:415–24. doi: 10.1080/13594320143000799. [DOI] [Google Scholar]
- 25.Ozturk H, Sokmen S, Yilmaz F, Cilingir D. Measuring mobbing experiences of academic nurses: Development of a mobbing scale. J Am Acad Nurse Pract. 2008;20:435–42. doi: 10.1111/j.1745-7599.2008.00347.x. [DOI] [PubMed] [Google Scholar]
- 26.Bilgel N, Aytac S, Bayram N. Bullying in Turkish white-collar workers. Occup Med (Lond) 2006;56:226–31. doi: 10.1093/occmed/kqj041. [DOI] [PubMed] [Google Scholar]
- 27.Sahin B, Dundar T. Investigation the factors affecting the level of health employees exposure to mobbing behavior: A study in Bolu. TISK Akademi. 2011;6:88–117. [in Turkish] [Google Scholar]
- 28.Erkol H, Gokdogan M, Erkol Z, Boz B. Aggression and violence towards health care providers- a problem in Turkey? J Forensic Leg Med. 2007;14:423–8. doi: 10.1016/j.jflm.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 29.Einarsen S, Matthiesen S, Skogstad A. Bullying at work: bullying, burnout and well-being among assistant nurses. Journal of Occupational Health Safety. 1998;14:563–8. [Google Scholar]
- 30.Levin PF, Hewitt JB, Misner ST. Insights of nurses about assault in hospital-based emergency departments. Image J Nurs Sch. 1998;30:249–54. doi: 10.1111/j.1547-5069.1998.tb01300.x. [DOI] [PubMed] [Google Scholar]
- 31.Frank E, McMurray JE, Linzer M, Elon L. Career satisfaction of US women physicians: results from the women physicians’ health study. Arch Intern Med. 1999;159:1417–26. doi: 10.1001/archinte.159.13.1417. [DOI] [PubMed] [Google Scholar]
- 32.Jackson D, Clare J, Mannix J. Who would want to be a nurse? Violence in the workplace – a factor in recruitment and retention. J Nurs Manag. 2002;10:13–20. doi: 10.1046/j.0966-0429.2001.00262.x. [DOI] [PubMed] [Google Scholar]
- 33.Hegney D, Plank A, Parker V. Workplace violence in nursing in Queensland, Australia: a self-reported study. Int J Nurs Pract. 2003;9:261–8. doi: 10.1046/j.1440-172X.2003.00431.x. [DOI] [PubMed] [Google Scholar]
- 34.Niedhammer I, David S, Degioanni S. Association between workplace bullying and depressive symptoms in the French working population. J Psychosom Res. 2006;61:251–9. doi: 10.1016/j.jpsychores.2006.03.051. [DOI] [PubMed] [Google Scholar]
- 35.Niedl K. Mobbing and wellbeing. European Journal of Work and Organizational Psychology. 1996;5:239–49. doi: 10.1080/13594329608414857. [DOI] [Google Scholar]
- 36.Garver MS, Mentzer JT. Logistic research methods: employing structural equation modeling to test for construct validity. Journal of Business Logistics. 1999;20:33–57. [Google Scholar]
- 37.Siddiqui O, Ali MW. Linear structural equation model in analyzing quality-of-life data from clinical trials. J Biopharm Stat. 1999;9:661–81. doi: 10.1081/BIP-100101202. [DOI] [PubMed] [Google Scholar]
- 38.Hofer S, Benzer W, Alber H, Ruttmann E, Kopp M, Schussler G, et al. Determinants of health-related quality of life in coronary artery disease patients: A prospective study generating a structural equation model. Psychosomatics. 2005;46:212–23. doi: 10.1176/appi.psy.46.3.212. [DOI] [PubMed] [Google Scholar]
- 39.Khan S, Murray RP, Barnes GE. A structural equation model of the effect of poverty and unemployment on alcohol abuse. Addict Behav. 2002;27:405–23. doi: 10.1016/S0306-4603(01)00181-2. [DOI] [PubMed] [Google Scholar]
- 40.MacCallum RC, Austin JT. Applications of structural equation modeling in psychological research. Annu Rev Psychol. 2000;51:201–26. doi: 10.1146/annurev.psych.51.1.201. [DOI] [PubMed] [Google Scholar]
- 41.Streiner DL. Building a better model: An introduction to structural equation modeling. Can J Psychiatry. 2006;51:317–24. doi: 10.1177/070674370605100507. [DOI] [PubMed] [Google Scholar]
- 42.Schreiber JB, Stage FK, King J, Nora A, Barlow EA. Reporting stuctural equation modeling and confirmatory factor analysis results: A review. J Educ Res. 2006;99:323–37. doi: 10.3200/JOER.99.6.323-338. [DOI] [Google Scholar]
- 43.Ferrinho P, Biscaia A, Fronteira I, Craveiro I, Antunes AR, Conceicao C, et al. Patterns of perceptions of workplace violence in the Portuguese health care sector. Hum Resour Health. 2003;1:11. doi: 10.1186/1478-4491-1-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pranjic N, Males-Bilic L, Beganlic A, Mustajbegovic J. Mobbing, stress, and work ability index among physicians in Bosnia and Herzegovina: Survey study. Croat Med J. 2006;47:750–8. [PMC free article] [PubMed] [Google Scholar]
- 45.Quine L. Workplace bullying in junior doctors: Questionnaire survey. BMJ. 2002;324:878–9. doi: 10.1136/bmj.324.7342.878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chen WC, Hwu HG, Kung SM, Chiu HJ, Wang JD. Prevalence and determinants of workplace violence of health care workers in a psychiatric hospital in Taiwan. J Occup Health. 2008;50:288–93. doi: 10.1539/joh.L7132. [DOI] [PubMed] [Google Scholar]
- 47.Daugherty SR, Baldwin DC, Rowley BD. Learning, satisfaction, and mistreatment during medical internship. JAMA. 1998;279:1194–9. doi: 10.1001/jama.279.15.1194. [DOI] [PubMed] [Google Scholar]
- 48.May DD, Grubbs LM. The extent, nature, and precipitating factors of nurse assault among three groups of registered nurses in a regional medical center. J Emerg Nurs. 2002;28:11–7. doi: 10.1067/men.2002.121835. [DOI] [PubMed] [Google Scholar]
- 49.Atawneh FA, Zahid MA, Al-Sahlawi KS, Shahid AA, Al-Farrah MH. Violence against nurses in hospitals: prevalence and effects. Br J Nurs. 2003;12:102–7. doi: 10.12968/bjon.2003.12.2.11049. [DOI] [PubMed] [Google Scholar]
- 50.Lin YH, Liu HE. The impact of workplace violence on nurses in South Taiwan. Int J Nurs Stud. 2005;42:773–8. doi: 10.1016/j.ijnurstu.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 51.Rutherford A, Rissel C. A survey of workplace bullying in a health sector organisation. Aust Health Rev. 2004;28:65–72. doi: 10.1071/AH040065. [DOI] [PubMed] [Google Scholar]
- 52.Uzun O, Bag B, Ozer N. Impacts on nurses of verbal abuse in the workplace. Journal of Nursing School of Ataturk University. 2001;4:41–7. [Google Scholar]
- 53.Cox HC. Verbal abuse in nursing: report of a study. Nurs Manage. 1987;18:47–50. doi: 10.1097/00006247-198711000-00015. [DOI] [PubMed] [Google Scholar]
- 54.Yildirim A, Yildirim D. Mobbing in the workplace by peers and managers: Mobbing experienced by nurses working in healthcare facilities in Turkey and its effect on nurses. J Clin Nurs. 2007;16:1444–53. doi: 10.1111/j.1365-2702.2006.01814.x. [DOI] [PubMed] [Google Scholar]
- 55.El Gilany A, El-Wehady A, Amr M. Violence against primary health care workers in Al-Hassa, Suudi Arabia. J Interpers Violence. 2010;25:716–34. doi: 10.1177/0886260509334395. [DOI] [PubMed] [Google Scholar]
- 56.Ng K, Yeung J, Cheung I, Chung A, White P. Workplace violence – a survey of diagnostic radiographers working in public hospitals in Hong Kong. J Occup Health. 2009;52:355–63. doi: 10.1539/joh.O8021. [DOI] [PubMed] [Google Scholar]
- 57.Jankowiak B, Kowalczuk JB, Krajewska-Kulak E, Sierakowska M, Lewko J, Klimaszewska K. Exposure the doctors to aggression in the workplace. Adv Med Sci. 2007;32:89–92. [PubMed] [Google Scholar]
- 58.Cowie H, Naylor P, Rivers I, Smith P-K, Pereira B. Measuring workplace bullying. Aggress Violent Behav. 2002;7:33–51. doi: 10.1016/S1359-1789(00)00034-3. [DOI] [Google Scholar]