Abstract
The aim of this study is to report the first case of simultaneous appearance of cerebral venous thrombosis (CVT) and bilateral subdural hematomas (SDHs) following epidural analgesia for labor and delivery and to point out the difficulty of establishing such a diagnosis in the presence of postpartum headache. A 26-year old primigravida with a history of epilepsy received epidural analgesia for delivery. Three days after the uneventful spontaneous vaginal delivery she complained about the headache. Patient responded very well to the pain medication and oral hydration, and the headache was relieved. Ten days after the delivery, the headache reoccurred, and an epidural blood patch was performed that successfully relieved her symptom. Stronger progressive headache with nausea reappeared two days later and the parturient was readmitted to hospital. Urgent neuroimaging examinations detected CVT of right the transverse sinus, ipsilateral cortical veins, and partially occluded superior sagittal sinus, as well as bilateral subacute/chronic SDHs. The treatment of the patient with low molecular weight heparin and antiaggregation therapy was effective. In this case, the diagnosis was delayed because of atypical clinical presentation and potentially confounding events (epidural analgesia and assumption that it was a case of PDPH). It is important to carefully observe patients in such conditions and promptly conduct suitable diagnostic tests. Otherwise, unrecognized intracranial complications and delay of appropriate therapy could be life-threatening.
The use of epidural analgesia for pain relief during labor and delivery has become increasingly popular. Although it is considered effective and safe, epidural analgesia could be associated with a wide spectrum of neurological complications. The most common neurological complications include accidental dural puncture and post-dural puncture headache (PDPH), central nervous system infections such as meningitis, occurrence of cerebral venous thrombosis (CVT), or epidural spinal hematoma or intracranial subdural hematomas (SDHs) that can have similar or even identical symptoms such as headache (1-4). Fortunately, neurological complications following epidural analgesia are rare, but if they occur the consequences could be serious (5,6).
CVT and other intracranial events related to the peripartum period pathophysiology may present with a wide spectrum of different neurological symptoms including headache (7,8). The diagnosis of such complications can be delayed and challenging, especially in cases with atypical clinical presentation and concomitant use of regional anesthesia that can lead to misdiagnosis of headache assuming it to be the case of PDPH. We described a 26-year-old parturient who received epidural analgesia for labor and delivery and who simultaneously developed multiple CVT and bilateral SDHs.
Case report
A 26-year-old primigravida received epidural analgesia for successful vaginal delivery. She had a history of epilepsy since childhood, currently symptom-free. Two days following noncomplicated delivery, she and her healthy child were discharged from the hospital. On the third postpartum day, the patient started to complain about headache that was considered as PDPH, although no evident sign of dural puncture during epidural procedures was observed. She responded very well to recommended bed rest, pain medication (diclofenac, Voltaren, Pliva, Zagreb, Croatia) in a dose of 50 mg twice daily), and additional oral hydration at home, and headache was resolved. One week later, the headache reoccurred and the patient was readmitted to the hospital. The neurological examination was unremarkable and the inspection of epidural puncture site did not show any signs of infections. Blood tests and other biochemical laboratory data (red and white blood counts, metabolic profile, serum electrolytes, blood glucose, blood urea nitrogen, creatinine, arterial blood gas analyses, C-reactive protein) were within the reference range. Persistent PDPH was considered once again although the epidural block was uneventful. Epidural blood patch was performed at the level L3-L4 by using 20 mL of autologous blood. Within an hour, the headache was almost resolved, and the patient was discharged from the hospital on the same day. Two days later, she complained about strong fronto-occipital headache that was worsened in the standing position. The headache was followed by nausea and the patient was immediately readmitted to the emergency department. She was hemodynamic and respiratory stable, arterial blood pressure was normal, biochemical (red and white blood counts with differential tests, erythrocyte sedimentation rate, blood levels of sodium, potassium, chloride, magnesium, calcium, bicarbonate, urea, creatinine, glucose, pH and bicarbonate, arterial carbon dioxide and oxygen concentrations, as well as levels of the serum creatine kinase, C-reactive protein, lactate dehydrogenase, hepatic enzymes, and analysis of the protein electrophoresis) and coagulations (platelets count, prothrombin time, activated partial thromboplastin time and ratio, fibrinogen and antithrombin III levels) tests were within the reference range. She still had no other neurological symptoms and signs except headache. An urgent computerized tomography (CT, Sensation 16, Siemens, Forchheim, Germany) of the brain was performed and revealed bilateral parietal-occipital subacute/chronic SDHs (Figure 1A). The magnetic resonance imaging (MRI, Avanto 1,5 T, Siemens) confirmed the mentioned diagnosis (Figure 1B), and magnetic resonance venography (MRV, Avanto 1,5 T, Siemens) revealed right transverse sinus and right parietal cortical venous thrombosis, as well as partial thrombosis of the superior sagittal sinus (Figure 2).
Figure 1.
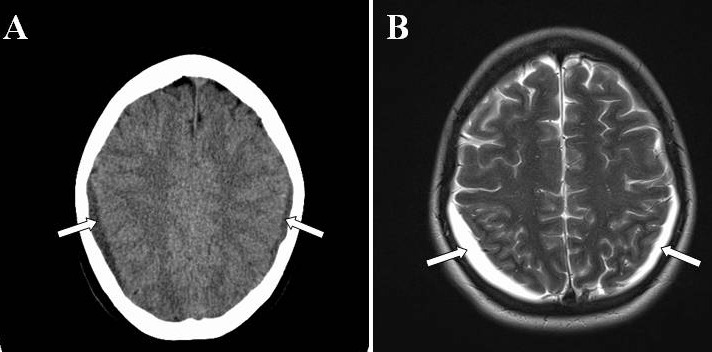
A non-contrast enhanced CT scan (A) and axial T2 weighted spin echo magnetic resonance imaging scan (B) showing bilateral subdural hematomas (marked by white arrows).
Figure 2.

Brain magnetic resonance venography (MRV) showing no flow in the right transverse sinus and ipsilateral cortical veins (white arrow) and partially occluded flow in the superior sagittal sinus (gray arrow).
The patient was transferred to the neurological intensive care unit where she was treated with low molecular heparin (LMWH), enoxaparin (Clexan, Sanofi Aventis, Paris, France), 1 mg/kg subcutaneously every 12 hours during 10 days. After LMWH therapy, the treatment was continued with acetylsalicylic acid (Aspirin, Bayer, Leverkusen, Germany) in a dose of 100 mg daily, and with 75 mg of the dipiridamol (Persantine, Boehringer, Ingelheim, Germany) once a day, during next six months. The dosage of sodium valporate was elevated to 500 mg daily during the hospital stay. Workup for vasculitis, lupus, antiphospholipid syndrome, and specific coagulation disorders was negative. Namely, antinuclear antibody, anti-neutrophil cytoplasmic antibody, anti-dsDNA, and extractable nuclear antigen tests were negative, lupus anticoagulant and other thrombophilic factors were also negative, and the levels of the complements C3 and C4 as well as proteins C and S were within the reference range. During further clinical course, patient remained asymptomatic and after four weeks she completely recovered and was discharged from hospital. A control MRI and MRV that were performed 14 days after hospital readmission showed partial regression of the SDHs with persistent CVT. A control neuroimaging that was made one month after hospital discharge revealed a completely spontaneous resolution of bilateral SDHs, and partial recanalization of the parietal cortical veins, superior sagittal sinus, and right transverse sinus. Three months after hospital discharge MRV examination showed full vein recanalization.
Discussion
Postpartum period could be a high-risk period for the development of different types of headaches. The overall incidence of postpartum headaches cannot be exactly determined due to limited and inconsistent studies (8-12). However, several studies reported that up to 75% of postpartum headaches are primary (migraines or tension-type headaches) in nature (10,12). Secondary headaches may occur due to intracranial pathologies including CVT, reversible cerebral vasoconstriction syndrome, stroke, intracranial hematomas, meningitis, or cerebral tumors (8). PDPH is the most common complication of obstetric regional anesthesia and the most probable cause of headache in pregnant women if epidural and/or spinal anesthesia or analgesia was applied during delivery.
This case report presents difficulties in diagnosing the cause of postpartum headache in a patient who underwent regional analgesia. The first suspected diagnosis was PDPH although the placement of lumbar epidural catheter and analgesia for labor was uneventful with no obvious sign of dural puncture. Therefore, we started with conventional treatment of PDPH by pain medication, hydration, and a subsequent blood patch insertion. The decision to perform the blood patch was based on the clinical finding that the patient had only headache and no additional neurological symptoms and signs, and that headache still had a postural component. A further increase in the headache severity with progressive nausea after epidural blood patch indicated that this was a case of more serious intracranial pathology, and the patient received diagnostic CT, MRI, and MRV.
To the best of our knowledge, this is the first report of a simultaneous occurrence of CVT and bilateral SDHs in postpartum period following epidural analgesia. Our opinion is that the patient’s headache was a symptom of CVT and SDH due to peripartum pathophysiology, possibly coincidentally observed with regional analgesia, and that the patient unnecessarily received an epidural blood patch. This suggestion is in agreement with the case report by Takahashi et al (13), who described severe persistent headache as a single symptom of CVT followed by acute SDHs in a previously healthy male patient without spinal/epidural anesthesia or analgesia. In our patient, the systemic diseases, as well as specific coagulation disorders were excluded by using immunological, serological, and specific laboratory tests. Possible triggering factors for the appearance of CVT or SDHs in our case could be the significant changes in intracranial pressure, dehydratation, venous congestion, and endothelial damage during delivery in combination with increased hypercoagulability after labor (7). A typical presentation of symptoms related to CVT or SDHs include progressive positional headache often accompanied with other neurological signs and symptoms, such as expressive dysphasia, mental disturbance, poor coordination, weakness of the limbs, loss or disturbance of focal sensation, impairment or loss of speech, consciousness disturbance, clinical manifestations of cerebral herniation, and deep coma with cardiac arrest in the worst case (6,9).
In our patient, the diagnosis was delayed because of atypical presentation of symptoms and because it was assumed that it was a case of PDPH after epidural analgesia. It is evident that headache as a symptom of serious intracranial events in postpartum period can mimic PDPH. Therefore, the rare and potentially fatal cranial peripartum complications can easily be misdiagnosed, particularly in parturient with regional analgesia. As a rule these diagnoses were made after the placement of an epidural blood patch and subsequent persistent and deteriorated headache.
However, the occurrence of CVT and SDHs associated with regional analgesia cannot be excluded. Namely, there are several reports on postpartum CVT (4,14-21) or SDHs (3,6,12,22-30) due to dural puncture after obstetric regional analgesia (Table 1).
Table 1.
Cerebral venous thrombosis and subdural hematomas in postpartum period following epidural or spinal analgesia and anesthesia: clinical presentations, treatment, and outcome
| References | Procedures | Clinical presentations | Complications | Treatment | Outcome |
|---|---|---|---|---|---|
| Vaughan DJA et al, 2000 (3) |
Epidural analgesia |
Occipital headache, tonic-clonic seizures |
Subdural hematoma |
Conservative |
Recovered |
| Kapessidou Y et al, 2006 (4) |
Spinal anesthesia |
Frontal headache, dizziness, acute left hemiparesis, blurred vision, somnolence |
Thrombosis of the posterior sagittal venous sinus |
Conservative |
Recovered |
| Aziz F, 2010 (6) |
Epidural analgesia |
Headache, cardiac arrest |
Subdural hematoma |
Resuscitation, conservative |
Died |
| Mashour GA et al, 2006 (12) |
Epidural analgesia |
Headache, syncopal episode, blurry vision, seizure |
Subdural hematomas |
Surgery |
Recovered |
| Ravindran RS et al, 1989 (14) |
Epidural analgesia |
Frontal headache, nausea, vomiting, seizures |
Dural sinus thrombosis |
Conservative |
Recovered |
| Wittmann M et al, 2012 (21) |
Epidural analgesia |
Headache |
Sinous venous thrombosis |
Conservative |
Recovered |
| Stocks GM et al, 2000 (15) |
Epidural analgesia |
Headache, confusion, sedation |
Sinous venous thrombosis |
Conservative |
Recovered |
| Zeidan A et al, 2010 (30) |
Spinal anesthesia |
Headache, associated, right eye tearing, fifth cranial nerve palsy, left hemiparesis |
Subdural hematoma |
Conservative |
Recovered |
| Kardash K et al, 2002 (25) |
Epidural analgesia |
Headache, seizures |
Subdural hematoma |
Conservative |
Recovered |
| Moradi M et al, 2012 (28) |
Spinal anesthesia |
Headache, nausea, vomiting |
Subdural hematoma |
Surgical |
Recovered |
| Ezri T et al, 2002 (24) |
Epidural analgesia |
Headache |
Subdural hematoma |
Conservative |
Recovered |
| Verdu MT et al, 2007 (26) |
Spinal anesthesia |
Headache, dysphasia, numbness in upper right limb and face |
Subdural hematoma |
Conservative |
Recovered |
| Todorov L et al, 2005 (18) |
Epidural anesthesia |
Headache, seizures |
Sinus venous thrombosis |
Conservative |
Recovered |
| Davies JM et al, 2001 (23) |
Epidural analgesia |
Headache, disphasia, deterioration, right-handed dysdiadokinesis |
Subdural hematoma |
Surgical |
Recovered |
| Diemunsch P et al, 1998 (22) |
Epidural analgesia |
Headache, focal neurological signs |
Bilateral subdural hematomas |
Conservative |
Recovered |
| Ghatge S et al, 2008 (19) |
Epidural analgesia |
Headache, confusion, disphagia, hemiparesis, nystagmus |
Superior sagitalis sinus, galen vein and straight sinus thrombosis |
Conservative |
Recovered |
| Karci A et al, 2005 (17) |
Spinal-epidural anesthesia |
Headache, hemiparesis, Babinski sign positive |
Superior sagital sinus thrombosis |
Conservative |
Recovered |
| Kueper M et al, 2008 (20) |
Epidural analgesia |
Headache, hemiparesis, hemihypesthesia |
Sinus venous thrombosis |
Conservative |
Recovered |
| Kulandayan S, 2002 (16) |
Epidural analgesia |
Headache, hemiparesis, seizures, loss of consciousness 3-5 min |
Sinus venous thrombosis |
Conservative |
Recovered |
| Liang MY and Pagel PS, 2012 (29) |
Epidural
analgesia |
Headache, radiating pain in legs, paresthesias on the left side of body |
Bilateral interhemispheric subdural hematoma |
Conservative |
Recovered |
| Dawley B and Hendrix A, 2009 (27) | Spinal anesthesia | Headache, nausea, vomiting | Subdural hematoma | Surgery | Recovered |
In our case, since accidental dural puncture was not observed, its presence could not have been safely excluded. The incidence of PDPH after unrecognized dural puncture following epidural analgesia during labor and delivery is very rare and amounts to 0.6% or less (31). Therefore, in such patients at low risk for PDPH, in the case of postpartum headache, other causes of headaches have to be carefully considered, and suitable diagnostic tests have to be performed without delay.
CVT and SDHs are serious events that should be immediately detected and appropriately treated. Treatment with heparin is the first choice upon confirmation of CVT, even in the presence of small intracerebral hemorrhage or small SDHs (32,33). In the reported case, the low molecular weight heparin and antiaggregation treatment were shown as a good therapy choice leading to a successful outcome.
In conclusion, we described a parturient with progressive headache due to simultaneous appearance of CVT and SDHs, as complications related to peripartum pathophisiology, possibly coincidentally observed with epidural analgesia. Our case points out that special attention should be given to differential diagnosis of headaches following epidural analgesia in the purperium, and that neurological examination should be carried out before performing an epidural blood patch, especially when the presentation of symptoms is atypical. Our experience suggests that rapid diagnostic, neuroimaging tests (CT, MRI, and MRV) should be carried out in all parturients with progressive and strong headache after failure of an epidural blood patch, and in some patients even before its placement. Early diagnosis and appropriate treatment are essential for a successful recovery because severe morbidity as well as mortality can occur following unrecognized CVT and SDHs, especially if these intracranial complications appear simultaneously, as it was in our case.
Acknowledgments
Funding None.
Ethical approval Not required.
Declaration of authorship ŽŽ conceived the idea for the study, wrote all parts of the manuscript, contributed substantially to the literature search, and critically reviewed the final draft of the manuscript. VST participated in the analysis, literature search, and writing of the manuscript. MMM and AŠ provided significant intellectual input by participating in the interpretation of the case report and critical revision of the manuscript. IA and SD contributed to the final revision of the manuscript. IP and RA interpreted the neuroimaging findings and gave the final approval of the version to be published.
Competing interests All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: no support from any organization for the submitted work; no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
References
- 1.Loo CC, Dahlgren G, Irestedt L. Neurological complications in obstetric regional anaesthesia. Int J Obstet Anesth. 2000;9:99–124. doi: 10.1054/ijoa.1999.0347. [DOI] [PubMed] [Google Scholar]
- 2.Moen V, Irestedt L. Neurological complications following central neuraxial blockades in obstetrics. Curr Opin Anaesthesiol. 2008;21:275–80. doi: 10.1097/ACO.0b013e3282f8e22f. [DOI] [PubMed] [Google Scholar]
- 3.Vaughan DJA, Stirrup CA, Robinson PN. Cranial subdural hematoma associated with dural puncture in labour. Br J Anaesth. 2000;84:518–20. doi: 10.1093/oxfordjournals.bja.a013483. [DOI] [PubMed] [Google Scholar]
- 4.Kapessidou Y, Vokaer M, Laureys M, Bier JC, Boogaerts JG. Case report: cerebral vein thrombosis after subarachnoid analgesia for labour. Can J Anaesth. 2006;53:1015–9. doi: 10.1007/BF03022531. [DOI] [PubMed] [Google Scholar]
- 5.Palot M, Visseaux H, Botmans C, Pire JC. Epidemiology of complications of obstetrical epidural analgesia. Cah Anesthesiol. 1994;42:229–33. [PubMed] [Google Scholar]
- 6.Aziz F. A fatal case of subdural hematoma: A complication of epidural analgesia. J Emergency Medicine. 2010; 6(2). Available from: www.ispub.com/journal/the-internet-journal-of-emergency-medicine/volume-6- number-2/a-fatal- case-of-subdural-hematoma-a-complication-of-epidural-analgesia.html Accessed: July 12, 2012.
- 7.Lockhart EM, Curtis L, Baysinger L. Intracranial venous thrombosis in the parturient. Anesthesiology. 2007;107:652–8. doi: 10.1097/01.anes.0000282103.70955.c4. [DOI] [PubMed] [Google Scholar]
- 8.Klein AM, Loder E. Postpartum headache. Int J Obstet Anesth. 2010;19:422–30. doi: 10.1016/j.ijoa.2010.07.009. [DOI] [PubMed] [Google Scholar]
- 9.Saurel-Cubizolles MJ, Romito P, Lelong N, Ancel PY. Women’s health after childbirth: a longitudinal study in France and Italy. BJOG. 2000;107:1202–9. doi: 10.1111/j.1471-0528.2000.tb11608.x. [DOI] [PubMed] [Google Scholar]
- 10.Ashkenazi A, Silberstein SD. Hormone-related headache: pathophysiology and treatment. CNS Drugs. 2006;20:125–41. doi: 10.2165/00023210-200620020-00004. [DOI] [PubMed] [Google Scholar]
- 11.Goldszmidt E, Kern R, Chaput A, Macarthur A. The incidence and etiology of postpartum headaches: a prospective cohort study. Can J Anaesth. 2005;52:971–7. doi: 10.1007/BF03022061. [DOI] [PubMed] [Google Scholar]
- 12.Mashour GA, Schwamm LH, Leffert L. Intracranial subdural hematomas and cerebral herniation after labor epidural with no evidence of dural puncture. Anesthesiology. 2006;104:610–2. doi: 10.1097/00000542-200603000-00030. [DOI] [PubMed] [Google Scholar]
- 13.Takahashi S, Shinoda J, Hayashi T. Cerebral venous sinus thrombosis in an adult patient presenting as headache and acute subdural hematoma. J Stroke Cerebrovasc Dis. 2012;21:338–40. doi: 10.1016/j.jstrokecerebrovasdis.2009.12.011. [DOI] [PubMed] [Google Scholar]
- 14.Ravindran RS, Zandstra GC, Viegas OJ. Postpartum headache following regional analgesia: a symptom of cerebral venous thrombosis. Can J Anaesth. 1989;36:705–7. doi: 10.1007/BF03005426. [DOI] [PubMed] [Google Scholar]
- 15.Stocks GM, Wooller DJ, Young JM, Fernando R. Postpartum headache after epidural blood patch: investigation and diagnosis. Br J Anaesth. 2000;84:407–10. doi: 10.1093/oxfordjournals.bja.a013451. [DOI] [PubMed] [Google Scholar]
- 16.Kulandayan S. Cortical vein thrombosis as cause for postpartum headache. J Anesth. 2002;6(1). Available from: http://www.ispub.com/journal/the-internet-journal-of anesthesiology/volume-6 number1/cortical-vein-thrombosis-as-cause-for-postpartum-headache.html. Accessed: July 12, 2012.
- 17.Karci A, Boyaci F, Yaka E, Cakmur R, Men S, Elaz Z. Cerebral venous thrombosis initially considered as a complications of spinal-epidural anaesthesia. J Int Med Res. 2005;33:711–4. doi: 10.1177/147323000503300615. [DOI] [PubMed] [Google Scholar]
- 18.Todorov L, Laurito CE, Schwartz DE. Postdural headache in the presence of cerebral venous sinus trombosis. Anesth Analg. 2005;101:1499–500. doi: 10.1213/01.ANE.0000181003.37968.CB. [DOI] [PubMed] [Google Scholar]
- 19.Ghatge S, Uppugonduri S, Kamarzaman Z. Cerebral venous sinus thrombosis following accidental dural puncture and epidural blood patch. Int J Obstet Anesth. 2008;17:267–70. doi: 10.1016/j.ijoa.2008.01.001. [DOI] [PubMed] [Google Scholar]
- 20.Kueper M, Goericke SL, Kastrup O. Cerebral venous thrombosis after epidural blood patch: coincidence or causal relation? A case report and review of the literature. Cephalalgia. 2008;28:769–73. doi: 10.1111/j.1468-2982.2008.01573.x. [DOI] [PubMed] [Google Scholar]
- 21.Wittmann M, Dewald D, Urbach H, Gast AS, Linnebank M, Baumgarten G, et al. Sinus venous thrombosis: A differential diagnosis of postpartum headache. Arch Gynecol Obstet. 2012;285:93–7. doi: 10.1007/s00404-011-1964-0. [DOI] [PubMed] [Google Scholar]
- 22.Diemunsch P, Balabaud VP, Petiau C, Marescaux C, Muller A, Valfrey J, et al. Bilateral subdural hematoma following epidural anesthesia[in French]. Can J Anaesth 199845328–31. 10.1007/BF03012023 [DOI] [PubMed] [Google Scholar]
- 23.Davies JM, Murphy A, Smith M, Sullivan GO. Subdural hematoma after dural puncture headache treated by epidural blood patch. Br J Anaesth. 2001;86:720–3. doi: 10.1093/bja/86.5.720. [DOI] [PubMed] [Google Scholar]
- 24.Ezri T, Abouleish E, Lee C, Evron S. Intracranial subdural hematoma following dural puncture in a parturient with HELLP syndrome. Can J Anaesth. 2002;49:820–3. doi: 10.1007/BF03017415. [DOI] [PubMed] [Google Scholar]
- 25.Kardash K, Morrow F, Belque F. Seizures after epidural blood patch with undiagnosed subdural hematoma. Reg Anesth Pain Med. 2002;27:433–6. doi: 10.1053/rapm.2002.33281. [DOI] [PubMed] [Google Scholar]
- 26.Verdu MT, Martinez Lage JF, Alonso B, Snaches-Ortega JL, Garsia-Candel A. Non-surgical management of intracranial subdural hematoma complicating spinal anesthesia. Neurocirugia. 2007;18:40–3. [PubMed] [Google Scholar]
- 27.Dawley B, Hendrix A. Intracranial subdural hematoma after spinal anesthesia in a parturient. Obstet Gynecol. 2009;113:570–3. doi: 10.1097/AOG.0b013e318195c15b. [DOI] [PubMed] [Google Scholar]
- 28.Moradi M, Shami S, Farhadifar F, Nesseri K. Cerebral subdural hematoma following spinal anesthesia: Report of two cases. Case Reports in Medicine. Available from: http://www.hindawi.com/journals/crim/2012/352028/. Accessed: July 12, 2012. [DOI] [PMC free article] [PubMed]
- 29.Liang MY, Pagel PS. Bilateral interhemispheric sudural hematoma after inadvertent lumbar puncture in a parturient. Can J Anaesth. 2012;59:389–93. doi: 10.1007/s12630-011-9664-6. [DOI] [PubMed] [Google Scholar]
- 30.Zeidan A, Farhat O, Maaliki H, Baraka A. Does postdural puncture headache left untreated lead to subdural hematoma? Case report and review of the literature. Middle East J Anesthesiol. 2010;20:483–92. [PubMed] [Google Scholar]
- 31.Okell RW, Sprigge JS. Unintentional dural puncture: A survey of recognition and management. Anesthesia. 1987;42:1140–3. doi: 10.1111/j.1365-2044.1987.tb05181.x. [DOI] [PubMed] [Google Scholar]
- 32.Masuhr F, Mehraein S, Einhäupl K. Cerebral venous and sinus thrombosis. J Neurol. 2004;251:11–23. doi: 10.1007/s00415-004-0321-7. [DOI] [PubMed] [Google Scholar]
- 33.Bousser MG. Cerebral venous thrombosis: Diagnosis and management. J Neurol. 2000;247:252–8. doi: 10.1007/s004150050579. [DOI] [PubMed] [Google Scholar]


