Abstract
Social marginalisation and other challenges facing HIV-positive pregnant women in Ukraine may put them at increased risk of relinquishing their infants to the state. We described rates of infant abandonment (exclusive non-parental care to most recent follow up, censored at two years of age) and investigated associated factors using logistic regression models, in 4759 mother-infant pairs enrolled across six Ukrainian sites in the European Collaborative Study from 2000 to May 2009. Median maternal age was 26.0 years, 81.8% were married or cohabiting and 60.6% were nulliparous at enrolment. An injecting drug use (IDU) history was reported by 18.4%, 80.2% took antiretroviral therapy (ART) antenatally and most deliveries were vaginal. A small but significant proportion of infants had been cared for exclusively in institutions by their second birthday (2.1% overall), decreasing from 3.8% (15/393) in 2000-02 to 1.6% (49/3136) in 2006-09 (p<0.01), concurrent with prevention of mother-to-child transmission (PMTCT) scale-up. A further 1% of infants spent some time in non-parental care. Antenatal ART was associated with an 88% reduced abandonment risk (AOR 0.12), versus receipt of single dose nevirapine only, and this was reflected in HIV infection prevalence in the two groups (17.1% of abandoned infants versus 6.6% in parental care). Mothers without a cohabiting partner or husband were more likely to abandon (AOR 4.08), as were active IDUs (AOR 3.27) and those with ≥1 previous children (AOR 1.89 for second-born, AOR 2.56 for subsequent births). Women delivering by elective caesarean section were less likely to abandon (AOR 0.37 versus vaginal), as were those leaving full time education later (AOR 0.61 for 17-18 years versus ≤16 years, AOR 0.23 for ≥19 years versus ≤16 years). Interventions to extend family planning and IDU harm reduction services along with non-stigmatising antenatal care to marginalised women are needed, and may reduce abandonment.
Keywords: HIV, infant abandonment, antenatal antiretroviral therapy, injecting drug use, Ukraine
Background
At the end of 2007, prevalence of HIV among the adult population of Ukraine was estimated at 1.63%, the highest adult (15-49 years) HIV prevalence in Europe. The initial driver of the epidemic in Ukraine was injecting drug use (IDU), but heterosexual transmission is becoming more important, with increasing exposure of people outside most at risk populations and increasing prevalence among women (Thorne C. et al, 2009; WHO et al., 2008). Forty-five percent of those living with HIV in Ukraine are women, mostly of child-bearing age, and prevalence among pregnant women is rising from 0.45% in 2005 to 0.52% in 2007 (Kruglov Y V et al, 2008).
Prior to the combination antiretroviral therapy (cART) era, cohorts in Western Europe reported that 19% of children born to HIV-infected women were in non-parental care by 12 months of age and around 40% at 60 months (European Collaborative Study & Thorne C. et al, 1998; Blanche S. et al, 1996). Since the advent of combination ART (cART), these children are less likely to need alternative care due to parental illness or death, but may be disproportionately vulnerable to adverse social conditions and more likely to be relinquished to the state (Khaldeeva N et al, 2003).
The socioeconomic upheaval and worsening public health in the Commonwealth of Independent States following the collapse of the Soviet Union (Little R.E., 1998) has impacted on child welfare; Russia and Ukraine have among the highest numbers of children aged under 3 years in institutional care in Europe (Browne K. et al, 2006). Infant abandonment is described as a social consequence of the HIV epidemic in these countries (Ministry of Health and Social Development of the Russian Federation, 2005), but the epidemic’s impact is set against high overall levels of abandonment; in Ukraine around 1% of children were placed in state care in 2005, with various estimates of 65-103,000 children living in state-run residential institutions in recent years (Thorne C. and Newell M.L., 2005; UNICEF, 2009b). Reliance on state institutional child care and the problems posed to normal child development (UNICEF, 2009a; Transatlantic Partners Against Aids, 2004; Maclean K., 2003; UNICEF, 2005) are not unique to countries in transition in the WHO European region (Browne K. et al, 2006), and information is lacking on the rates of and circumstances surrounding infant abandonment specific to HIV-infected women in Ukraine.
Implementation of the national prevention of mother-to-child transmission of HIV (PMTCT) programme (Thorne C. et al, 2009; Malyuta R. et al, 2006; Thorne C. and Newell M.L., 2005) and the scaling-up of HIV treatment and care services may be postulated to reduce risk of infant abandonment, for example through provision of opportunities to reduce MTCT risk and HIV disease progression, and through reducing stigma and discrimination. However, the potential impact of these programmes on infant abandonment has not been investigated to date, and the design and implementation of interventions requires a more thorough understanding of the problem. Our objectives were to quantify institutional care of infants born to HIV-1-infected women in Ukraine and describe associated factors, using data from an ongoing birth cohort study.
Methods
The European Collaborative Study (ECS) is an ongoing birth cohort study, in which HIV-1 infected pregnant women are enrolled and their infants prospectively followed according to a standard protocol. The ECS was established in 1985 in Western Europe to estimate the rate of and risk factors for MTCT (European Collaborative Study, 1988). Centres from Ukraine joined in 2000: sites in Odessa, Mykolaiv and Simferopol started enrolling at the start of 2000 and those in Kiev, Donetsk and Mariupol in September 2006 (European Collaborative Study, 2006). In this study we used all data available from start of enrolment in Ukraine in 2000 to May 2009. Data are collected anonymously on standard questionnaires, using study serial numbers (linked anonymous data). Information collected includes maternal sociodemographic and clinical information, delivery and infant characteristics. Information on infant’s social care setting (i.e. with mother, father or other relative, fostered, adopted, or cared for in hospital or an institution) directly following birth is collected and updated at regular follow-up thereafter.
Definitions
In order to identify infants receiving institutional care as a permanent substitute for parental care, we used follow-up data censored at 24 months to categorise infants as ever or never in parental care. This was a conservative measure, distinguishing infants with even minimal parental involvement and mixed care settings (for example home and an orphanage) from those with no parental involvement. The small number (n=15) of infants in stable alternative family settings (i.e. fostered, adopted or cared for by another relative) were included in the ‘ever with parents’ group. The ‘never in parental care’ group, referred to as ‘abandoned’ throughout, includes infants voluntarily abandoned by their parents and those subject to child protection intervention.
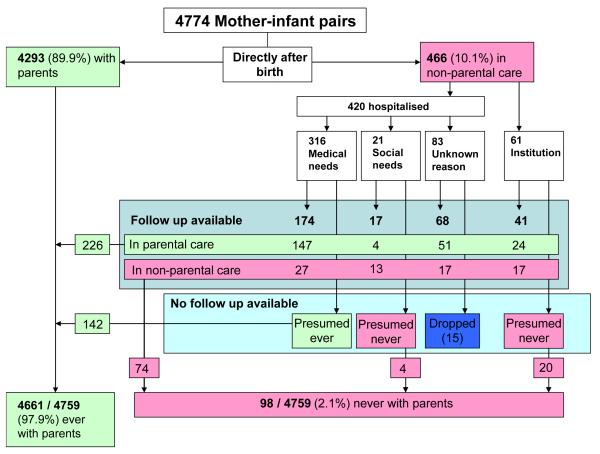
Assumptions were made on the longer term care setting of infants not in parental care at baseline and lacking follow-up information at the time of the analysis, due to recent enrolment in the cohort (n=181) (Figure 1). Infants staying in hospital beyond the 3-5 days after birth normally seen in Ukraine but with no documented reason were presumed to need medical care if birthweight <2500g, and/or gestational age <34 weeks, and/or reported perinatal problems (including neonatal abstinence syndrome (NAS)), and/or infant death (n=21). There was no significant difference in prevalence of maternal IDU history between this and other hospitalised groups. Infants with no documented reason for hospitalisation and no indication of medical needs were excluded from the analyses (n=15), as their longer-term care setting was unclear.
Figure 1.
Definition of outcome variable ‘abandoned’ (ever or never in parental care during first two years of life), using follow up data censored at 24 months
Gestational age was categorised as term (37 completed weeks or more), preterm (34-36 weeks) and severely preterm (<34 weeks). Birthweight was categorised as normal (≥2500g) and low birthweight (<2500g). Time of maternal HIV diagnosis was categorised as before pregnancy, during the first or second trimester, or later (third trimester or at delivery).
Statistical analysis
Univariable comparisons were assessed with the χ2 test for categorical variables. Logistic regression was used to obtain unadjusted odd ratios (OR) and adjusted odds ratios (AOR) and 95% confidence intervals (CI) in analyses identifying factors associated with infants never being in parental care. The model was built using a forward stepwise approach, with each factor tested for significant contribution to the fit using likelihood ratio test, at a significance level of p≤0.05.
The logistic regression analyses were limited to 4759 mother-infant pairs with complete data available on the following characteristics: maternal characteristics: age, marital status, IDU, time of HIV diagnosis, antenatal antiretroviral prophylaxis, mode of delivery, previous live births, previous terminations, sexual partner of IDU, receipt of single dose nevirapine (sdNVP); infant characteristics: gender, gestational age, year of birth, birthweight, NAS, receipt of sdNVP, congenital abnormalities, social care setting at birth.
Those missing data on age at leaving full time education (n=2301) were categorised within the variable ‘educational status’, to allow analyses adjusted for educational status to be conducted. Year of infant birth was adjusted for a priori in the multivariate analysis, due to potential confounding (infants born in later years less likely to have been ‘ever in parental care’, as they have had shorter follow-up).
The standard of care for antiretroviral prophylaxis for PMTCT underwent an important change in 2005, when antenatal prophylaxis in addition to or instead of sdNVP became the standard of care. From 2005, sdNVP was usually used alone only in women missing opportunities for antenatal antiretroviral prophylaxis (Thorne C. et al, 2009), and so reflected a different level of access to and receipt of antenatal care compared to pre-2005. In order to investigate the effect of prophylaxis on infant abandonment, a sub-analysis was carried out using only mother-infant pairs enrolled in 2005-09 (n=3646).
Statistical analyses were performed with STATA/IC v 10.0 for Windows (StataCorp, College Station, Texas.
Results
Of the 4759 infants enrolled by May 2009, 98 (2.1%) had never been in parental care, with a further 47 (1%) spending some time in non-parental care, mostly in an institution. The majority never in parental care after follow-up (54/98) were in an institution or in hospital with a social admission at baseline (Figure 1). Baseline demographic and medical characteristics are given in Table 1. Most mothers were young, married or cohabiting and primiparous; a fifth had an IDU history and a third were sexual partners of IDUs. Antenatal ART coverage was around 80%, and most infants were vaginally delivered.
Table 1.
Baseline characteristics of mothers and infants by infant care setting at baseline (shortly after birth) (n= 5003 where data available)
| Infant care setting at baseline | Total | |||
|---|---|---|---|---|
| With parents/ adopted |
In hospital | In orphanage/ institution |
||
| Marital status | ||||
| Married or cohabiting | 3731 (83.6%) | 305 (67.3%) | 29 (46.0%) | 4065 (81.7%) |
| Single, separated, divorced or widowed |
731 (16.4%) | 148 (32.7%) | 34 (54.0%) | 911 (18.3%) |
|
Age at leaving full-time education |
||||
| ≤16 years | 482 (21.0%) | 60 (26.9%) | 19 (59.4%) | 561 (22.0%) |
| 17 -18 years | 676 (29.5%) | 74 (33.2%) | 7 (21.9%) | 757 (29.7%) |
| ≥19 years | 1135 (49.5%) | 89 (39.9%) | 6 (18.8%) | 1230 (48.3%) |
| Maternal age | ||||
| Median (IQR) | 25.9 (22.6,29.6) | 27.3 (23.2,31.5) | 28.2 (23.9,31.0) | 26.0 (22.7,29.8) |
| Parity | ||||
| 0 | 2759 (61.8%) | 224 (50%) | 23 (36.5%) | 3006 (60.5%) |
| 1 | 1295 (29.0%) | 150 (33.5%) | 28 (44.4%) | 1471 (29.6%) |
| ≥2 | 410 (9.2%) | 74 (16.5%) | 12 (19.0%) | 358 (10.0%) |
|
History of pregnancy termination |
||||
| No | 2711 (60.8%) | 260 (58.2%) | 35 (55.6%) | 3005 (60.5%) |
| Yes | 1751 (39.2%) | 187 (41.8%) | 28 (44.4%) | 1965 (39.5%) |
| History of IDU | ||||
| No | 3701 (83.5%) | 280 (63.1%) | 32 (50.8%) | 4012 (81.2%) |
| Yes | 733 (16.5%) | 164 (36.9%) | 31 (49.2%) | 927 (18.8%) |
| Sexual partner of IDU | ||||
| No | 2998 (68.0%) | 272 (62.2%) | 33 (52.4%) | 3303 (67.2%) |
| Yes | 1414 (32.0%) | 165 (37.8%) | 30 (47.6%) | 1609 (32.8%) |
| Timing of HIV diagnosis | ||||
| Before pregnancy | 1286 (29.1%) | 185 (41.5%) | 26 (41.9%) | 1496 (30.4%) |
| 1st/ 2nd trimester | 2216 (50.2%) | 107 (24.0%) | 7 (11.3%) | 2330 (47.3%) |
| 3rd trimester / at delivery | 915 (20.7%) | 154 (34.5%) | 29 (46.8%) | 1097 (22.3%) |
| Antenatal ART | ||||
| No | 751 (16.7%) | 255 (56.0%) | 47 (74.6%) | 1052 (21.0%) |
| Yes | 3732 (83.3%) | 200 (44.0%) | 16 (25.4%) | 3947 (79.0%) |
| Mode of delivery | ||||
| Vaginal | 2703 (60.3%) | 370 (81.3%) | 58 (92.1%) | 3129 (62.6%) |
| Elective CS | 1590 (35.5%) | 61 (13.4%) | 4 (6.4%) | 1655 (33.1%) |
| Emergency CS | 192 (4.3%) | 24 (5.3%) | 1 (1.6%) | 217 (4.3%) |
| Birthweight | ||||
| ≥2500g | 4084 (91.2%) | 252 (55.5%) | 41 (66.1%) | 4375 (87.6%) |
| <2500g | 398 (8.8%) | 202 (44.5%) | 21 (33.9%) | 621 (12.4%) |
| Gestational age | ||||
| ≥37 weeks | 4209 (94.0%) | 302 (66.4%) | 44 (71.0%) | 4554 (91.2%) |
| 34-36 weeks | 221 (4.9%) | 79 (17.4%) | 10 (16.1%) | 310 (6.2%) |
| <34 weeks | 48 (1.1%) | 74 (16.3%) | 8 (12.9%) | 130 (2.6%) |
| NAS | ||||
| No | 4393 (98.3%) | 407 (90.0%) | 51 (81.0%) | 4849 (97.3%) |
| Yes | 77 (1.7%) | 45 (10.0%) | 12 (19.1%) | 134 (2.7%) |
The proportion of infants abandoned in their first two years decreased from 3.8% (15/393) in 2000-02 to 2.8% (34/1230) in 2003-05 and 1.6% (49/3136) in 2006-09 (χtrend2=12.9, p<0.01). Over the same time periods, there was a decrease in the proportion of mothers reporting an IDU history from 29.8% (117/393) to 24.2% (298/1230) and 14.6% (459/3136) (χ2trend=89.6, p<0.01), with a concomitant decrease in proportion of infants with NAS, from 7.1% (n=28/393) to 3.9% (48/1230) and 1.4% (43/3136) (χ2 trend=60.5, p<0.01).
Factors associated with infant abandonment
In unadjusted logistic regression analyses, gender and presence of congenital abnormalities in the infant were not significantly associated with risk of abandonment (p=0.292 and p=0.085 respectively). Maternal history of pregnancy termination and age were similarly non-significant factors, (p=0.123 and p=0.066 respectively). Factors significantly associated with infant abandonment in univariable analyses are presented in Table 2 and included marital status, maternal education, mode of delivery and birth order. Receipt of antenatal antiretroviral prophylaxis showed a strong univariable association with reduced risk of abandonment, and infants whose mothers had been diagnosed with HIV earlier (in the first and second trimesters) were also less likely to be abandoned.
Table 2.
Factors associated with infant abandonment (n=4759)
| Independent variables | Base | Crude OR (95% C.I.) |
Crude p value |
Adjusted OR (95% C.I.) |
Adjusted p value |
|---|---|---|---|---|---|
| Mother’s marital status | |||||
| Married or cohabiting | 3894 | 1 | 1 | ||
| Single, divorced, separated or widowed | 865 | 6.35 (4.23,9.54) | p≤0.001 | 4.08 (2.60,6.40) | p≤0.001 |
|
Mother’s age at leaving full- atime education |
|||||
| ≤16 years | 539 | 1 | 1 | ||
| 17-18 years | 727 | 0.50 (0.29,0.89) | p=0.019 | 0.61 (0.32,1.18) | p=0.142 |
| ≥19 years | 1192 | 0.13 (0.06,0.27) | p≤0.001 | 0.23 (0.10,0.52) | p≤0.001 |
| Missing | 2301 | 0.28 (0.17,0.46) | p≤0.001 | 0.37 (0.21,0.65) | p≤0.001 |
| Maternal IDU history | |||||
| No | 3895 | 1 | -- | -- | |
| Yes | 884 | 4.46 (2.98,6.67) | p≤0.001 | ||
| Mother a partner of IDU | |||||
| No | 3214 | 1 | -- | -- | |
| Yes | 1565 | 1.56 (1.04,2.34) | p=0.031 | ||
| Timing of maternal HIV diagnosis | |||||
| Before pregnancy | 1455 | 1 | |||
| 1st/2nd trimester | 2271 | 0.12 (0.06,0.25) | p≤0.001 | -- | -- |
| 3rd trimester /delivery | 1033 | 1.33 (0.87,2.03) | p=0.187 | ||
| ARV prophylaxis | |||||
| sdNVP only | 549 | 1 | 1 | ||
| None | 395 | 1.64 (1.04,2.58) | p=0.032 | 1.34 (0.82,2.18) | p=0.244 |
| Antenatal prophylaxis +/− sdNVP | 3815 | 0.05 (0.03,0.09) | p≤0.001 | 0.12 (0.06,0.23) | p≤0.001 |
| Mode of delivery | |||||
| Vaginal | 2962 | 1 | 1 | ||
| Elective CS | 1590 | 0.08 (0.03,0.21) | p≤0.001 | 0.37 (0.13,1.08) | p=0.069 |
| Emergency CS | 207 | 0.15 (0.02,1.08) | p=0.060 | 0.20 (0.03,1.54) | p=0.122 |
| Birth order of infant | |||||
| Firstborn | 2882 | 1 | 1 | ||
| Second born | 1409 | 2.90 (1.82,4.61) | p≤0.001 | 1.89 (1.14,3.13) | p=0.014 |
| ≥ Third born | 468 | 4.97 (2.89,8.55) | p≤0.001 | 2.56 (1.41,4.65) | p=0.002 |
| Gestational age of infant | |||||
| ≥37 weeks | 4342 | 1 | 1 | ||
| 34-36 weeks | 291 | 3.60 (2.06,6.29) | p≤0.001 | 1.79 (0.97,3.30) | p=0.064 |
| <34 weeks | 126 | 7.12 (3.83,13.26) | p≤0.001 | 3.40 (1.67,6.92) | p=0.001 |
| Birthweight of infant | |||||
| ≥2500g | 4165 | 1 | -- | -- | |
| <2500g | 594 | 3.71 (2.42,5.69) | p≤0.001 | ||
| NAS in infant | p≤0.001 | ||||
| No | 4640 | 1 | 1 | ||
| Yes | 119 | 10.97 (6.40,18.80) | p≤0.001 | 3.27 (1.76,6.09) | p≤0.001 |
Infants of active IDUs (indicated by presence of NAS) were at an almost 11-fold increased risk of abandonment. Separate univariable analyses showed smaller but significantly increased abandonment risk among mothers reporting an IDU history (OR 4.46, 95%CI 2.98-6.67, p≤0.001 versus no history) and among those with an IDU sexual partner (OR1.56 95%CI 1.04-2.34, p=0.031 versus no IDU sexual partner). Preterm birth and low birthweight were both associated with increased risk of abandonment, and with non-receipt of antenatal ART (χ2=162.51, p=<0.01 and χ2=154.94, p=<0.01 respectively) and presence of NAS (χ2=25.94, p=<0.01 and χ2=15.79, p=<0.01 respectively). Among women reporting an IDU history, 15.2% of births were preterm (≤36 weeks gestation) compared with 7.3% of births among women without an IDU history. Over a fifth (n=29) of women who continued to inject drugs in the third trimester abandoned their infants, compared to 2% (n=9) of those who reported last using drugs pre-conception.
In the multivariable logistic regression model, marital status, maternal education, receipt of antiretroviral prophylaxis, parity, gestational age of infant and NAS remained significantly associated with risk of infant abandonment (Table 2). Maternal IDU history was no longer significantly associated in adjusted analyses, the association with abandonment accounted for by active or recent drug use. Maternal receipt of antenatal prophylaxis was associated with an 88% reduction in abandonment and remained the strongest predictor. A four-fold higher infant abandonment rate was seen among single women versus those married or cohabiting and among women with minimal education versus those educated beyond 18 years. Severely preterm infants were over three times more likely to be abandoned than term infants, and a similarly increased risk was seen among infants with NAS. Infants born into larger families (third-born or subsequently) were 2.5 times more likely to be abandoned than firstborns, with second-borns at intermediate abandonment risk.
In a sub-analysis including 3646 mother-child pairs enrolled since 2005, univariable analysis showed a substantially lower abandonment risk among women receiving antenatal antiretroviral prophylaxis compared to sdNVP only (OR 0.04, 95%CI 0.02-0.08 p<0.01). This association remained after adjusting for marital status, maternal education, receipt of antenatal prophylaxis, mode of delivery, parity, gestational age, NAS and year of birth (AOR 0.10, 95%CI 0.05-0.20, p<0.01 for abandonment by women receiving antenatal antiretroviral prophylaxis versus those receiving sdNVP only). No significant difference in abandonment was found between women receiving sdNVP only and no antiretroviral prophylaxis, in both univariable and multivariable models (p=0.199 and p=0.521 respectively). Similar overall associations between independent variables and risk of infant abandonment were seen in 2005-09 as in the whole dataset 2000-09.
Characteristics of abandoned infants
HIV status was reported for 3166 (66.5%) children, the remainder having indeterminate status at most recent follow-up. Of the abandoned infants with HIV status reported, 12/70 (17.1%) were HIV-infected versus 205/3096 (6.6%) of infants in parental care. In univariable analysis, abandonment was almost three-fold higher in infants with confirmed HIV diagnosis (OR 2.92, 95%CI 1.54-5.52 p<0.01), than in uninfected infants. Of the 98 abandoned infants, 9/98 (9.2%) died compared with 89/4656 (1.9%) of the infants in parental care (median ages at death 127 and 62 days respectively). Post-mortem reports of the nine abandoned infants who died attributed deaths to infection in all but one case, where information was not available.
None of the infants lived to 18 months to receive antibody test confirmation of infection status. One infant was provisionally uninfected on the basis of two negative PCR tests, five had indeterminate infection status, two infants had presumptive infection on the basis of one positive PCR test and infective cause of death, and one infant had confirmed HIV infection, high viral load and multiple infections.
Discussion
Infant abandonment affected a small but significant proportion of infants in the first two years of life born to HIV-infected women in Ukraine in this cohort, decreasing over the 10 year study period. Overall, 2.1% of infants lacked parental care entirely and a further 1% experienced a mixture of parental and other care settings by their second birthday. The factor most strongly associated with reduced risk of infant abandonment was mother’s receipt of antenatal antiretroviral prophylaxis. In our sub-analysis of infants born since 2005, abandonment risk was equally elevated in women who had received sdNVP only and those receiving no antiretroviral prophylaxis, both scenarios indicating lack of antenatal care. Mothers who were married or cohabiting and who had higher levels of educational attainment were also substantially less likely to abandon. Preterm infants, those with NAS and infants with older siblings were at increased risk of abandonment.
The decline in infant abandonment over time was concurrent with PMTCT scale up in Ukraine; these years saw substantially increased coverage with antiretroviral prophylaxis and concomitant declines in MTCT rates (from 15.2% in 2001 to 7% in 2006) (Thorne C. et al, 2009). The reduced risk of infant abandonment among women receiving antenatal antiretroviral prophylaxis compared to sdNVP only (because of late presentation and diagnosis in labour), supports previous findings associating maternal receipt of prophylaxis with reduced risk of infant non-parental care (Mayaux M.J. et al, 2003; Khaldeeva N et al, 2003). Greater understanding of the effectiveness of PMTCT interventions and of cART in HIV treatment may improve women’s aspirations for their own and their infant’s health, thus reducing abandonment (Thorne C. and Newell M.L., 2005) (Zabina H. et al, 2009). Previous studies have shown that a diagnosis of HIV earlier rather than later in pregnancy, affording an adjustment period and opportunity to receive PMTCT counselling and interventions, is associated with decreased risk of infant abandonment (Hillis S. et al, 2007), but there was no association in our adjusted analyses. Late diagnosis may not be an independent risk factor for abandonment per se, but indicate other problems underlying non-receipt of antenatal care. Training of healthcare professionals during PMTCT scale-up is likely to have reduced stigmatising and discriminatory attitudes towards HIV-infected pregnant women, recognised as a factor potentially contributing to abandonment earlier in the epidemic (Zabina H. et al, 2009; UNAIDS, 2008). ‘Baby-Friendly’ initiatives in maternity wards, introduced in Ukraine in 2000, have been associated with decreases in infant abandonment in the general population (Sherstyuk E. and Grover D. (UNICEF), 2006), also seen in Russia (Lvoff N. et al, 2000), and may have contributed to the declining rate of abandonment seen in our study.
The significant associations found between abandonment and parity, maternal education and marital status indicate the importance of financial and social resources in caring for a newborn. Women without a partner were at a four-fold increased risk of abandonment, affirming previous findings of the importance of support from the baby’s father (Shapoval A., 2008), and possibly extended family. Poverty and insecure or inadequate housing increase susceptibility to infant abandonment regardless of HIV infection status, and are likely more common among marginalised HIV-infected individuals; 82% of children in Ukraine staying with HIV-infected parent(s) remain in poverty (Zabina H. et al, 2009; Shapoval A., 2008). A social support payment has been introduced in Ukraine for women with newborns and may help to alleviate abandonment due to poverty, contributing to the decline in abandonment seen here since the subsidy was introduced, but could also encourage completion of unwanted pregnancies which would otherwise have been terminated (Thorne C. and Newell M.L., 2005).
Russian studies have found infant abandonment to be substantially more common among HIV-infected women whose pregnancies were unintended (Zabina H. et al, 2009; Hillis S. et al, 2007; Akatova N. et al, 2009). We did not have data available on whether the pregnancies in our study were planned, but two-fifths of the women had a history of pregnancy termination while a quarter of women in a nested post-natal cohort within the ECS reported not planning their most recent pregnancy (Jenny Saxton et al, 2009).
Abandonment was three times more likely in infants with NAS here, supporting previous findings from Ukraine, Russia, France, Western Europe and USA linking maternal IDU with increased infant abandonment, with rates of up to 30% in this group (Malyuta R. et al, 2006; Blanche S. et al, 1996; European Collaborative Study & Thorne C. et al, 1998; National Abandoned Infants Assistance Resource Center, 2005; Mok J.Y.Q. et al., 1996; Khaldeeva N et al, 2003). Our conservative measure of abandonment may have underestimated the true association between abandonment and maternal IDU, as infants born to IDUs are more likely to have medical problems after birth, and infants hospitalised for medical care but without follow-up were assumed not to be abandoned (Figure 1). Putative links between IDU and voluntary infant abandonment include poorer access to or use of family planning services with more unintended pregnancies (Malyuta R. et al, 2006), lifestyles non-conducive to parenting (Zabina H. et al, 2009) and acute withdrawal symptoms in the mother during and immediately after delivery, precipitating abandonment in search of drugs. Opioid substitution therapy (OST) improves neonatal outcomes when used in pregnancy, and could help prevent abandonment postnatally by controlling withdrawal symptoms and reducing drug-seeking behaviours such as commercial sex work (Minozzi S. et al, 2008). However, accessibility to OST in Ukraine is poor; buprenorphine and methadone OST became available in 2007 and 2008, only 1956 of an estimated 400,000 IDUs were enrolled in a programme by the end of 2008 (Aizberg O & Eurasian Harm Reduction Network, 2008). Childbearing women encounter specific barriers to engagement with drug treatment including an unwillingness to be seen as an unfit parent, lack of child care facilities for their existing children (EMCDDA, 2000) and objection of a partner (Open Society Institute, 2009). Effective harm reduction programmes would therefore need to be carefully tailored to the needs of pregnant HIV-infected IDUs.
Infants abandoned in this study were significantly more likely to be infected with HIV than their contemporaries in parental care, more of whom had benefited from PMTCT interventions, consistent with previous evidence (Transatlantic Partners Against Aids, 2004). HIV DNA PCR testing facilities for early diagnosis of HIV in vertically-exposed infants were introduced in Ukraine in 2006, but coverage remains patchy (Thorne C. et al, 2009), leaving some settings reliant on antibody testing at 18 months. In the vast majority of cases infant HIV diagnosis would have occurred after abandonment, suggesting that women more likely to transmit HIV (e.g. due to no or limited access to PMTCT interventions) were also more likely to abandon. The abandoned infants were also more frequently preterm and low birthweight, possibly due to higher prevalence of in utero exposure to drugs (Mok J.Y.Q. et al., 1996) and related maternal behaviours such as poor diet.
HIV-exposed and abandoned infants in Russia and Ukraine are vulnerable to stigmatised care, in institutional rather than family settings (Thorne C. and Newell M.L., 2005; Transatlantic Partners Against Aids, 2004). Infant abandonment and state provision of institutional care predate Ukraine’s HIV epidemic, and institutions also formed a significant part of state care provision to infants abandoned by HIV-infected women in Western Europe in 1980-90s (Blanche S. et al, 1996; European Collaborative Study & Thorne C. et al, 1998). Institutional care of infants remains common throughout Europe (Browne K. et al, 2006) but its detrimental effect on all aspects of normal child development (Maclean K., 2003) provides the basis for child care and welfare system reform and impetus to move to family-based care settings.
Our study was limited by its observational nature, with potential for unmeasured confounding. A further limitation was our inability to distinguish between women voluntarily relinquishing infants and those subject to child protection interventions. Our cohort covers around 30% of HIV-infected pregnant women in Ukraine, making the data and conclusions broadly generalisable to such women countrywide. The assumptions leading to our definition of abandonment were conservative (Figure 1), and the prevalence reported here should be interpreted as a minimum.
Conclusions
To conclude, a decline in infant abandonment over the last ten years was seen in this cohort, concurrent with PMTCT scale-up, suggesting the importance of PMTCT programmes in reducing infant abandonment rates. However the challenge of ensuring coverage of hard-to-reach populations, such as IDUs and other marginalised groups, with PMTCT services remains, together with the need to provide adequate harm reduction, HIV treatment and care, family planning and pregnancy termination services, reflecting the complex factors behind infant abandonment. Further research on longitudinal patterns of social care in children without a stable home setting and in older children of HIV-infected mothers is needed.
Acknowledgments
The Ukraine European Collaborative Study Group consists of the following members who have contributed to this study: S Mahdavi, Prof ML Newell (UCL Institute of Child Health, UK), Y. Khomout (Perinatal Prevention of AIDS Initiative, Odessa, Ukraine), Dr S Posokhova (Regional Hospital, Odessa, Ukraine), Dr T Kaleeva, Dr. Y. Barishnikova, Dr. S. Servetsky (Odessa Regional Centre for HIV/AIDS, Ukraine), Dr A. Stelmah, Dr. G. Kiseleva, Dr E. Dotsenko, Dr O. A. Zalata (Crimean Republic Centre for HIV/AIDS, Ukraine), Dr. S. Solokha, Dr M. P. Grazhdanov (Donetsk Regional Centre for HIV/AIDS, Ukraine), Dr. N. Bashkatova (Marioupol AIDS Center, Ukraine), Dr. I.Raus, Dr O. V. Yurchenko (Kiev City Centre for HIV/AIDS, Ukraine), Dr. Z. Ruban, Dr.O. Gloushenko (Mikolaiv Regional Centre for HIV/AIDS, Ukraine). Dr. N. Primak (Kriviy Rig City Center for HIV/AIDS, Ukraine)
Funding
The ECS is a coordination action of the European Commission (PENTA/ECS 018865). Claire Thorne is supported by a Wellcome Trust Research Career Development Fellowship. Heather Bailey is supported by an MRC Doctoral Training Account PhD Studentship. Some of this work was undertaken at GOSH/UCL Institute of Child Health which received a proportion of funding from the UK Department of Health’s NIHR Biomedical Research Centres funding scheme. The Centre for Paediatric Epidemiology and Biostatistics also benefits from funding support from the Medical Research Council in its capacity as the MRC Centre of Epidemiology for Child Health.
Reference List
- Aizberg O, Eurasian Harm Reduction Network . Oral Substitution Therapy in Selected Countries of Eastern Europe and Central Asia - International AIDS Society. 2008. [Google Scholar]
- Akatova N, et al. Integration of family planning services into clinical services for HIV-infected women. Dec 1, 2009. Ref Type: Personal Communication
- Blanche S, et al. Separation between HIV-positive Women and Their Children: The French Prospective Study 1986 through 1993. American Journal of Public Health. 1996;86:376–381. doi: 10.2105/ajph.86.3.376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne K, et al. Overuse of institutional care for children in Europe. BMJ. 2006;332:485–487. doi: 10.1136/bmj.332.7539.485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- EMCDDA . Problems facing women drug users and their children - EMCDDA 2000 Annual report on the state of the drugs problem in the European Union. 2000. [Google Scholar]
- European Collaborative Study Mother-to-child transmission of HIV infection. Lancet. 1988;332:1039–1043. [PubMed] [Google Scholar]
- European Collaborative Study The mother-to-child HIV transmission epidemic in Europe: evolving in the East and established in the West. AIDS. 2006;20:1419–1427. doi: 10.1097/01.aids.0000233576.33973.b3. [DOI] [PubMed] [Google Scholar]
- European Collaborative Study. Thorne C, et al. Social care of children born to HIV-infected mothers in Europe. AIDS care. 1998;10:7–16. doi: 10.1080/713612346. [DOI] [PubMed] [Google Scholar]
- Hillis S, et al. Rapid HIV testing, pregnancy, antiretroviral prophylaxis and infant abandonment in St Petersburg. International Journal of STD & AIDS. 2007;18:120–122. doi: 10.1258/095646207779949781. [DOI] [PubMed] [Google Scholar]
- Jenny Saxton, et al. Use of condoms and family planning by HIV-positive women of childbearing age in Ukraine; Eastern Europe and Central Asia AIDS Conference 2009; 2009. Ref Type: Abstract
- Khaldeeva N, et al. HIV-1 seroprevalence rates in women and relinquishment of infants to the state in St Petersburg, Russia, 2002. The Lancet. 2003:362. doi: 10.1016/s0140-6736(03)15019-2. [DOI] [PubMed] [Google Scholar]
- Kruglov YV, et al. The most severe HIV epidemic in Europe: Ukraine’s national HIV prevalence estimates for 2007. Sexually Transmitted Infections. 2008;84:i37–i41. doi: 10.1136/sti.2008.031195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little RE. Public health in central and eastern Europe and the role of environmental pollution. Annu Rev Public Health. 1998:153–172. doi: 10.1146/annurev.publhealth.19.1.153. [DOI] [PubMed] [Google Scholar]
- Lvoff N, et al. Effect of Baby-Friendly Initiative on Infant Abandonment in a Russian Hospital. Archive of Paediatric and Adolescent Medicine. 2000;154:474–477. doi: 10.1001/archpedi.154.5.474. [DOI] [PubMed] [Google Scholar]
- Maclean K. The impact of institutionalisation on child development. Development and Psychopathology. 2003;15:853–884. doi: 10.1017/s0954579403000415. [DOI] [PubMed] [Google Scholar]
- Malyuta R, et al. Prevention of mother-to-child transmission of HIV infection: Ukraine experience to date. European Journal of Public Health. 2006;16(2):123–127. doi: 10.1093/eurpub/cki150. Ref Type: Journal (Full)
- Mayaux MJ, et al. Characteristics of HIV-Infected Women Who Do Not Receive Preventive Antiretroviral Therapy in the French Perinatal Cohort. J Acquir Immune Defic Syndr. 2003;34:338–343. doi: 10.1097/00126334-200311010-00013. [DOI] [PubMed] [Google Scholar]
- Ministry of Health and Social Development of the Russian Federation, A. S. C. o. t. M. o. H. o. R. a. U. Children, Women and HIV Infection in the Russian Federation Moscow. 2005. [Google Scholar]
- Minozzi S, et al. Maintenance agonist treatments for opiate dependent pregnant women. 2008. [DOI] [PubMed] [Google Scholar]
- Mok JYQ, Amanda Ross, Gillian Raab, et al. Maternal HIV and drug use: effect on health and social morbidity. Archives of Diseases in Childhood. 1996:210–214. doi: 10.1136/adc.74.3.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Abandoned Infants Assistance Resource Center, U. o. C. B. Boarder Babies, Abandoned Infants, and Discarded Infants. 2005. [Google Scholar]
- Open Society Institute . Women, Harm Reduction and HIV: Key findings from Azerbaijan, Georgia, Kyrgyzstan, Russia and Ukraine. 2009. [Google Scholar]
- Shapoval A. Socioeconomic profile of HIV+ mothers including those who abandon their infants in Ukraine; XVII International AIDS Conference; 2008.Jan 1, Ref Type: Abstract
- Sherstyuk E, Grover D, UNICEF . A warm and welcoming start to life - The expanded Baby Friendly Hospital Initiative in Ukraine. 2006. [Google Scholar]
- Thorne C, Newell ML. 2005. Prevention of HIV Infection in Infants: Documenting and learning from the Ukraine experience. [Google Scholar]
- Thorne C, et al. Progress in prevention of mother-to-child transmission of HIV infection in Ukraine: results from a birth cohort study. BMC Infectious Diseases. 2009:9. doi: 10.1186/1471-2334-9-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Transatlantic Partners Against Aids . Abandoned Children Born to HIV-positive Women: Analysis of the situation in Russia. 2004. [Google Scholar]
- UNAIDS, U. B. R. C. Living with HIV in Eastern Europe and the CIS: The Human Cost of Social Exclusion. 2008. [Google Scholar]
- UNICEF UNICEF: Children in residential institutions vulnerable to abuse. 2005 http://www.unicef.org.uk/press/news_detail_full_story.asp?news_id=451 [On-line]
- UNICEF UNICEF Central and Eastern Europe/Commonwealth of Independent States webpage: child protection. 2009a http://www.unicef.org/ceecis/protection_1174.html [On-line]
- UNICEF UNICEF: Children in Ukraine. 2009b UNICEF website [On-line]. Available: http://www.unicef.org/ukraine/children.html.
- WHO. UNICEF. UNAIDS UNAIDS/WHO Epidemiological Fact Sheets on HIV and AIDS - Ukraine. 2008 2008 Update.
- Zabina H, et al. Abandonment of infants by HIV-positive women in Russia and prevention measures. Reproductive Health Matters. 2009;17:162–170. doi: 10.1016/S0968-8080(09)33438-2. [DOI] [PubMed] [Google Scholar]