Abstract
Objectives
This study aimed to examine the prevalence, trends, and correlates of practitioner-based complementary and alternative medicine (CAM) services use according to race in a socioeconomically disadvantaged population.
Design
Included in this cross-sectional analysis were 50,176 African Americans (AAs) and 19,038 whites enrolled into the Southern Community Cohort Study from March 2002 through September 2009. Logistic regression models were used to calculate odds ratios (ORs) and 95% confidence intervals (CIs) of CAM services use associated with participant characteristics.
Outcome measures
Outcomes include the prevalence of and trends in use of CAM services during 2002–2009 and correlates of use by race.
Results
CAM services use during 2002–2009 was greater among whites (11.7%) than among AAs (8.5%), but no significant temporal trends within the 8-year period were observed. The significant associations were observed for CAM services use with higher educational attainment (OR 1.78, 95% CI: 1.61–1.96 for college versus less than high school), household income (OR 1.61, 95% CI: 1.44–1.81 for ≥$50,000 versus <$15,000), and having a history of a chronic disease (OR 1.34, 95% CI: 1.21–1.47) among both AAs and whites. Significant differences in findings between AAs and whites were seen for age (with a sharp decline in use with older age among AAs but not whites), sex (with the excess of female users more striking among whites), employment (with the unemployed among AAs but not whites more likely to be users), alcohol consumption (with white but not AA drinkers more likely to report CAM services use), and cigarette smoking status (with negative association of use with current smokers more striking among whites).
Conclusions
CAM services use is associated with sociodemographic and health-related factors, and racial differences in such use exist. The descriptive findings of this study help supplement the limited information on CAM use among low-income and minority populations in the United States.
Introduction
Complementary and alternative medicine (CAM) constitutes a group of diverse medical and health care systems, practices, and products that are not currently an integral part of conventional medicine.1 Since the 1990s, interest in and use of CAM by the American public has substantially increased, and the popularity of CAM has impacted many aspects of the health care system.2–6 As a result, more information on CAM use has been required for clinical practice, research, education, and regulation.7–9 CAM use is believed to be closely associated with socioeconomic and cultural backgrounds that vary between different racial/ethnic groups.10,11 Although a number of national surveys have examined prevalence of CAM use in the general population and identified a number of associated factors/predictors,2–5,12–18 economically disadvantaged populations and racial/ethnic minority groups were underrepresented in the majority of previous studies; thus, there is a paucity of data on the relative or differential influence of the related factors on CAM use in these subpopulations. In addition, since CAM use may change over time,4–6 it should be evaluated periodically. The vast majority of large population-based studies on CAM use were conducted in the 1990s and early 2000s, and little is known about trends in use during recent years, particularly in economically disadvantaged populations.
The Southern Community Cohort Study (SCCS) is a landmark epidemiologic study designed to investigate causes and related health issues associated with cancer and other chronic diseases in the southeastern United States.19 The majority of SCCS participants are African Americans (AAs) and persons of low socio-economic status. The study's baseline interview included questions regarding practitioner-based CAM services use, providing a unique data source for evaluating utilization of CAM in a large, socioeconomically disadvantaged population. The aim of the present analyses is to examine prevalence of and trends in use of practitioner-based CAM services during the period of 2002 and 2009, identify sociodemographic and health-related factors associated with use, and further evaluate whether these associations differ between AA and white SCCS participants. Such information will enhance our understanding of the epidemiology and racial differences in CAM use.
Materials and Methods
The SCCS is an ongoing prospective cohort study of racial health disparities in the United States. Details of the SCCS have been described elsewhere.20 Briefly, the SCCS was initiated in 2001 and subject recruitment began in 2002. The recruitment strategies of the study included clinic-based recruitment from 71 community health centers (CHCs) across the southeastern United States. The CHCs provide medical and preventive care mainly to medically underserved and lower-income persons in urban and rural areas.21 At the CHCs, potential study subjects (patients and persons accompanying patients) were randomly approached and screened for eligibility and interest in study participation. Eligible participants were 40–79 years of age and had not received treatment for cancer within the past year. The study protocol was approved by the Institutional Review Boards at Vanderbilt University and Meharry Medical College.
This cross-sectional analysis utilized the baseline data collected from participants who enrolled in the SCCS at a CHC from March 2002 through September 2009. A comprehensive baseline interview for the study was conducted in person by trained interviewers, using a computer-assisted interview protocol, to elicit information on sociodemographics, lifestyle-related factors, health insurance coverage, medical history, anthropometry, and other characteristics. Race was self-reported. During the interview, a participant was asked “Which of the following describes your race or ethnic background?” The participant could choose white, black/African-American, Hispanic/Latino, Asian or Pacific Islander, American Indian or Alaska Native, and Other racial or ethnic group. Participants who chose white or black/African-American were included in this analysis. The question about recent use of practitioner-based CAM services was “Did you visit an ‘alternative medicine’ or ‘complementary medicine’ practitioner during the past year, such as a chiropractor, massage therapist, herbalist, acupuncturist, traditional healer, etc?” Participants were also asked about their history of visits for conventional physician services. Participants had the option of refusing to answer these questions or responding “don't know.”
Descriptive statistics (means and proportions) were used to describe the distribution of each variable. The χ2 test was applied to examine the difference in the proportion of CAM services use between AAs and whites in the study population. The Mantel-Haenszel linear trend test was used to examine trends in CAM services use during the study period. Multiple logistic regression models were used to estimate odds ratios (ORs) and 95% confidence intervals (CIs) of CAM use associated with demographic and other participant characteristics. The variables included in the models were age, race, sex, marital status, educational attainment, annual household income, employment status, type of community ever lived in (ever lived in a rural/farming community versus not), country of birth (inside versus outside the United States), levels of spiritual/religious beliefs, cigarette smoking status, alcohol consumption, body–mass index (BMI, kg/m2), history of a chronic disease (i.e., hypertension, coronary artery disease, diabetes, high cholesterol, stroke, transient ischemic attack, hepatitis, emphysema, chronic bronchitis, asthma, tuberculosis, sickle cell disease, heartburn, acid reflux, ulcer, Crohn's disease, ulcerative colitis, glaucoma, HIV/AIDS, Parkinson's disease, lupus, multiple sclerosis, depression, arthritis, noncancerous cyst in the breast, fibroids in the uterus, or cancers), health insurance coverage (including Medicaid and Medicare), physician services use, and CHCs. Tests for trends across levels of independent variables were performed by entering the categorical variables as continuous parameters in the models where appropriate. Interaction terms were included in the models to test for a differential effect of each variable of interest on CAM services use between AAs and whites. All analyses were conducted by using Statistical Analysis Software (version 9.1, SAS Institute Inc., Cary, NC). All statistical tests were based on a two-sided probability. For analysis of differences in the prevalence of CAM services use, p-values<0.05 were considered statistically significant. Because the multiple associations for AAs and whites were examined, Bonferroni correction was used to adjust p-value for trend (including categorical differences) and p-value for interaction. After adjustment, p-values<0.0014 for trend tests and p-values<0.0042 for interaction tests were considered statistically significant for the results of the multiple regression analyses.
Results
From March 2002 through September 2009, a total of 69,662 eligible AAs and whites were enrolled into the study and completed the baseline interview. Of them, 448 (0.6%) were excluded from the analysis due to missing data on their visits for CAM services. Thus, the present analysis included 69,214 SCCS participants.
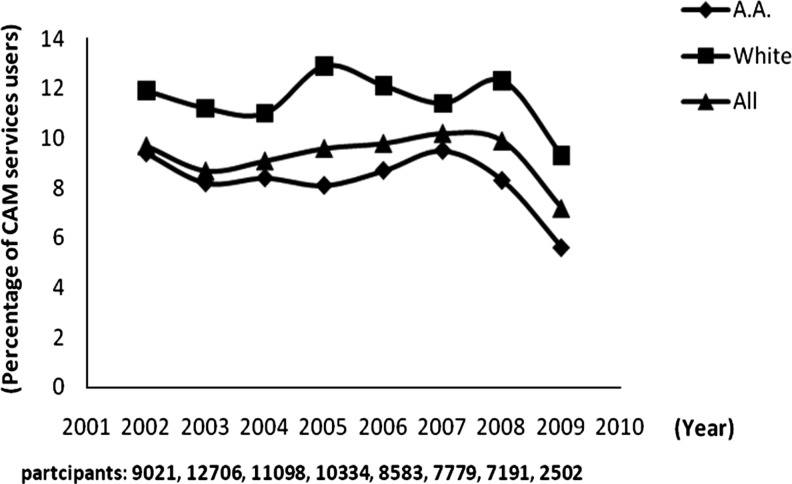
During the period 2002–2009, the annual prevalence of CAM services use in the SCCS cohort varied each year from 7.2% to 10.2% (Fig. 1). The prevalence of use was consistently higher in whites than in AAs throughout the study period (Fig. 1). No significant increased or decreased trends in use during the study period were detected (p for trends=0.084 for AAs, 0.756 for whites, and 0.257 for all participants). However, it was noted that there was a sharp reduction in CAM services use in 2009 (7.2%), which is markedly lower than the overall rate (9.4%) and the rate in 2008 (9.3%). A further analysis showed that a total of 2502 participants were enrolled from 17 CHCs in 2009, and over 75% of them were from six CHCs where there was a low rate of CAM services use in 2009 (6.3% on the average) and in general (overall rate of use in the six CHCs=8.6%) (data not shown). This may be attributed to the drop in rate of CAM services use seen in the 2009 SCCS sample.
FIG. 1.
Trends in prevalence of complementary and alternative medicine (CAM) service use in Southern Community Cohort Study (SCCS) population from 2002 to 2009. P-values for trends were 0.084 for African Americans (A.A.), 0.756 for whites, and 0.257 for all participants.
Table 1 shows use of CAM services and/or physician services in the past year in the study population by race. Of 69,214 participants, 9.4% reported having visited a CAM practitioner, 91% visited a physician, and 9.0% visited both. Compared to their white counterparts, AAs were less likely to visit a CAM practitioner (8.5% versus 11.7%; p<0.001) or a physician (90.6% versus 92.1%; p<0.001) or both (8.1% versus 11.2%; p<0.001). In addition, among 6,508 CAM services users, 95.3% also visited a physician, with similar rates in AAs and whites (95.2% versus 95.4; p=0.55); and among 63,003 physician services users, 9.8% also had visits for CAM, with 9.0% in AAs and 12.1% in whites (p<0.001) (data not shown).
Table 1.
Use of CAM Services and/or Physician Services in the Past Year, SCCS 2002–2009 Sample
| AAs and whites | AAs | Whites | p-Valuea | |
|---|---|---|---|---|
| Participants (n) | 69,214 | 50,176 | 19,038 | |
| CAM services users | 9.4% | 8.5% | 11.7% | <0.001 |
| Physician services users | 91.0% | 90.6% | 92.1% | <0.001 |
| Users of both | 9.0% | 8.1% | 11.2% | <0.001 |
Indicates significance levels for differences between African Americans (AAs) and whites.
CAM, complementary and alternative medicine.
Table 2 presents characteristics of the participants and adjusted ORs of CAM services use according to sociodemographic and health-related factors by race. The participants had a mean age of 52 years with a range of 40–79 years. The majority of participants were AAs (72%) and women (60%). In general, the participants represented a socioeconomically disadvantaged population; over 60% reported a total annual household income of less than $15,000; nearly one third had an educational attainment of less than 12 years of schooling; more than two thirds were divorced/separated, widowed, or never married; 63% were unemployed; and about 44% had no health insurance coverage (including Medicare and Medicaid). Approximately half of participants said that they were very spiritual or religious, 45% were current cigarette smokers, 29% consumed alcohol weekly or daily, 45% were obese (BMI≥30 kg/m2), and 87% had a history of a chronic disease.
Table 2.
Associations of Sociodemographic and Health-Related Factors with CAM Services Use in SCCS 2002–2009 Sample
| |
All participants (N=69,214) |
AAs (N=50,176) |
Whites (N=19,038) |
|
||||
|---|---|---|---|---|---|---|---|---|
| Variables | % of sample | Adjusted ORsb | 95% CI | Adjusted ORsb | 95% CI | Adjusted ORsb | 95% CI | p for interactiona |
| Age at interview | ||||||||
| 40–49 | 48.1 | ref. (1.00) | ref. (1.00) | ref. (1.00) | 0.003 | |||
| 50–59 | 33.2 | 0.94 | 0.89, 1.00 | 0.94 | 0.87, 1.01 | 0.90 | 0.81, 1.00 | |
| 60–79 | 18.7 | 0.74 | 0.68, 0.80 | 0.65 | 0.58, 0.72 | 0.83 | 0.73, 0.95 | |
| p for trend | <0.001 | <0.001 | 0.011 | |||||
| Sex | ||||||||
| Male | 39.9 | ref. (1.00) | ref. (1.00) | ref. (1.00) | 0.004 | |||
| Female | 60.1 | 1.23 | 1.16, 1.31 | 1.16 | 1.07, 1.25 | 1.39 | 1.24, 1.55 | |
| p for categorical differences | <0.001 | <0.001 | <0.001 | |||||
| Marital status | ||||||||
| Married/living with a partner | 31.5 | ref. (1.00) | ref. (1.00) | ref. (1.00) | 0.175 | |||
| Separated/divorced | 34.7 | 1.07 | 1.00, 1.14 | 1.09 | 1.01, 1.19 | 1.05 | 0.93, 1.17 | |
| Widowed | 9.9 | 0.93 | 0.84, 1.03 | 0.93 | 0.82, 1.06 | 0.94 | 0.79, 1.12 | |
| Never been married | 23.8 | 0.95 | 0.87, 1.03 | 0.92 | 0.83, 1.01 | 1.07 | 0.91, 1.27 | |
| p for categorical differences | <0.001 | <0.001 | 0.588 | |||||
| Educational attainment | ||||||||
| <High school | 32.1 | ref. (1.00) | ref. (1.00) | ref. (1.00) | 0.096 | |||
| = High school | 35.4 | 1.15 | 1.07, 1.23 | 1.15 | 1.05, 1.25 | 1.12 | 0.98, 1.27 | |
| Some college | 23.7 | 1.34 | 1.24, 1.45 | 1.33 | 1.21, 1.46 | 1.35 | 1.17, 1.54 | |
| ≥College | 8.9 | 1.78 | 1.61, 1.96 | 1.63 | 1.44, 1.84 | 1.97 | 1.67, 2.32 | |
| p for trend | <0.001 | <0.001 | <0.001 | |||||
| Annual household income (US$) | ||||||||
| <15,000 | 60.5 | ref. (1.00) | ref. (1.00) | ref.(1.00) | 0.307 | |||
| 15,000–24,999 | 21.8 | 1.04 | 0.97, 1.12 | 1.03 | 0.94, 1.12 | 1.11 | 0.98, 1.26 | |
| 25,000–49,999 | 11.8 | 1.24 | 1.14, 1.35 | 1.16 | 1.04, 1.29 | 1.37 | 1.19, 1.58 | |
| ≥50,000 | 4.9 | 1.61 | 1.43, 1.81 | 1.48 | 1.26, 1.74 | 1.62 | 1.35,1.94 | |
| p for trend | <0.001 | <0.001 | <0.001 | |||||
| Employment status | ||||||||
| Employed | 36.2 | ref. (1.00) | ref. (1.00) | ref.(1.00) | <0.001 | |||
| Unemployed | 62.8 | 1.10 | 1.04, 1.17 | 1.24 | 1.15, 1.33 | 0.88 | 0.79, 0.97 | |
| p for categorical differences | <0.001 | <0.001 | 0.008 | |||||
| Spiritual/religious beliefsc | ||||||||
| Fairly/slightly/not at all | 37.0 | ref. (1.00) | ref. (1.00) | ref.(1.00) | 0.065 | |||
| Very | 50.7 | 1.15 | 1.08, 1.22 | 1.10 | 1.02, 1.18 | 1.23 | 1.12, 1.36 | |
| p for categorical differences | <0.001 | 0.013 | <0.001 | |||||
| Cigarette smoking status | ||||||||
| Never | 34.6 | ref. (1.00) | ref. (1.00) | ref.(1.00) | <0.001 | |||
| Former | 20.8 | 1.04 | 0.97, 1.12 | 1.08 | 0.99, 1.18 | 0.96 | 0.86, 1.08 | |
| Current | 44.5 | 0.80 | 0.75, 0.85 | 0.89 | 0.82, 0.97 | 0.66 | 0.58, 0.74 | |
| p for categorical differences | <0.001 | 0.001 | <0.001 | |||||
| Alcohol consumption | ||||||||
| Never or rarely | 58.9 | ref. (1.00) | ref. (1.00) | ref. (1.00) | 0.001 | |||
| Monthly | 11.9 | 1.13 | 1.04, 1.23 | 1.02 | 0.92, 1.12 | 1.30 | 1.14, 1.49 | |
| Weekly | 19.9 | 1.10 | 1.02, 1.18 | 1.01 | 0.92, 1.10 | 1.20 | 1.04, 1.38 | |
| Daily | 8.9 | 1.01 | 0.91, 1.13 | 0.89 | 0.78, 1.01 | 1.31 | 1.07, 1.62 | |
| p for trend | 0.042 | 0.275 | <0.001 | |||||
| BMI (kg/m2) | ||||||||
| <25 | 25.7 | ref. (1.00) | ref. (1.00) | ref. (1.00) | 0.013 | |||
| ≥25, <30 | 28.8 | 1.10 | 1.02, 1.18 | 1.16 | 1.06, 1.28 | 1.03 | 0.91, 1.17 | |
| ≥30 | 44.8 | 1.11 | 1.04, 1.20 | 1.22 | 1.12, 1.34 | 0.99 | 0.88, 1.12 | |
| p for trend | 0.006 | <0.001 | 0.565 | |||||
| History of a chronic disease | ||||||||
| No | 12.8 | ref. (1.00) | ref. (1.00) | ref. (1.00) | 0.354 | |||
| Yes | 87.2 | 1.34 | 1.21, 1.47 | 1.29 | 1.16, 1.44 | 1.46 | 1.19, 1.79 | |
| p for categorical differences | <0.001 | <0.001 | <0.001 | |||||
| Health insurance coverage | ||||||||
| No | 43.5 | ref. (1.00) | ref. (1.00) | ref. (1.00) | 0.853 | |||
| Yes | 56.4 | 1.19 | 1.12, 1.26 | 1.21 | 1.13, 1.29 | 1.14 | 1.03, 1.27 | |
| p for categorical differences | <0.001 | <0.001 | 0.006 | |||||
Indicates significance levels of interaction between race/ethnicity (African American (AA) and white) and each factor listed in the table.
Obtained from logistic regression models with mutual adjustment of the other factors listed in the table, as well as origin of birth, type of community, physician services use, and CHCs.
Approximately 12% participants did not disclose their perceived levels of spiritual/religious beliefs.
AAs, African Americans; ORs, odds ratios; CI, confidence interval; BMI, body–mass index.
From the logistic regression analyses used to examine the associations between CAM services use and sociodemographic and health-related factors by race (Table 2), among both AAs and whites the strongest correlates of use were higher educational attainment (OR 1.78, 95% CI: 1.61–1.96 for college versus less than high school) and household income (OR 1.61, 95% CI: 1.43–1.81 for ≥$50,000 versus <$15,000). Use was also moderately more common among those having a history of chronic disease (OR 1.34, 95% CI: 1.21–1.47). Significant differences in associations with CAM use between AAs and whites were seen for age (with a less sharp decline in use with older age among whites than AAs; p for interaction=0.003), sex (with the excess of female users more striking among whites; p for interaction=0.004), employment (with the unemployed among AAs but not whites more likely to be users; p for interaction<0.001), alcohol consumption (with white but not AA drinkers more likely to report CAM services use; p for interaction=0.001), and cigarette smoking status (with negative association of use with current smokers more striking among whites; p for interaction<0.001).
Discussion
Although many studies have examined the overall prevalence and correlates of CAM use.2–5,12–18,22–27 the current study is the largest study of CAM services use among socioeconomically disadvantaged AAs and whites. It was possible not only to estimate point prevalence and evaluate a wide range of potential correlates of use, but also to examine the trends of the prevalence in use during the past 8 years and compare association patterns for consistency between the two racial groups.
There are several widely cited studies that previously examined prevalence of practitioner-based CAM use in the U.S. general population, with varied estimates. The Robert Wood Johnson Foundation National Access to Care Survey reported that nearly 10% of the U.S. population saw a CAM practitioner during 1994.12 The Medical Expenditure Panel Survey estimated that nearly 9% of the U.S. population visited a CAM practitioner during 1996.13 In Eisenberg surveys, the estimated prevalence of visits to a CAM practitioner was 12.1% in 1990 and increased to 19.2% in 1997.4 The 2002 National Health Interview Survey (NHIS) reported that 11.8% of adults sought care from a licensed or certified CAM provider in the past year.2 The 2007 NHIS, compared to 2002 NHIS, showed that there was a slight increase in use of certain practitioner-based CAM therapies among adults, including acupuncture (1.1% versus 1.4%), massage therapy (5.0% versus 8.3%), and naturopathy (0.2% versus 0.3%).21 Variation in the estimates of the prevalence of CAM services use from different studies may be attributable to differences in the sampling frame, timing of sampling, categorization of CAM providers, and the target populations. In the SCCS, overall 9.4% of participants reported CAM services use in the past year during the period of 2002 and 2009. CAM services use also varied by race, with whites showing higher rates in use than AAs every year, but no significant increasing or decreasing trends in use found for either racial group. This study's results reflect the most recent prevalence of and trends in CAM services use in a socioeconomically disadvantaged population in the southeastern United States.
Individuals who visit CAM practitioners may seek complementary medical therapies or alternative medical therapies. Complementary therapies are used together with conventional medicine, whereas alternative therapies are used in place of conventional treatment.1 It has been reported that one of the reasons that some patients seek CAM therapies is because they are disappointed in conventional medicine,3 implying that CAM therapies may be used as a substitute for conventional treatment in a subset of users. However, other studies reported that most CAM users also visit physicians, suggesting that CAM therapies as an “add on” to conventional medical treatments.4,14 In the Medical Expenditure Panel Survey, an estimated 6.5% of the U.S. population had visits for both CAM therapies and conventional medical care; 1.8% used only CAM services. This study's data show that the vast majority of users of practitioner-based CAM services were also users of physician services, as would be expected since the vast majority of participants were recruited into the SCCS at CHCs that are conventional physician-based. Although the prevalence of use of CAM services alone cannot be adequately estimated, the current data do provide strong support to the notion that use of CAM services may often serve as a complement to conventional medicine,14 even among low-income groups.
Although many studies have reported that sociodemographic and health-related factors influence CAM use,12–18,22–25 limited information is available about the influences of various correlates on practitioner-based CAM use, particularly about the relative or differential effects of those correlates on such use across racial/ethnic groups.17,18,24 A major finding of the present study is that the effects of several sociodemographic and health-related factors on CAM services use may differ between AAs and whites. Of note were the markedly stronger inverse association with age among AAs but not whites; the greater sex differential among whites than AAs, with the highest use group being white women (13.1%); and the association between unemployment and use seen in AAs but not whites. Also, the positive association of use with alcohol consumption was seen among whites but not AAs, while the negative association of use with current smokers was more striking among whites. The reasons for the differential influence of these factors on CAM services use are unknown and warrant further investigation.
One should be cautious when interpreting the current results. First, a broad definition of CAM includes various CAM therapies that can be administered by CAM providers or by oneself. This study's reported prevalence should specifically reflect practitioner-based CAM services used in the study population; it does not represent an estimate of all CAM use. Second, racial differences in use of specific CAM modalities may also exist. Unfortunately, no information was available regarding such detail of CAM type. In addition, this study relied on self-report, and thus could have been subject to reporting bias. However, the standardized personal interview-based approach used in this study should have reduced reporting errors associated with health illiteracy, poor comprehension, or low patient educational level.
Conclusions
It was found that the prevalence of CAM services use in the generally low-income AAs and whites studied was fairly stable during the study period. It was also found that whites had higher rates of use than AAs, identified a wide range of sociodemographic and health-related factors associated with such use, and racial differences were described in terms of the effects of some factors on use. These findings help fill the need for increasing information on CAM use in the United States.
Acknowledgments
This work was supported by National Cancer Institute grants: R01 CA092447 and U01CA114641.
Disclosure Statement
No competing financial interests exist.
References
- 1.National Center for Complementary and Alternative Medicine. http://nccam.nih.gov. [Apr 17;2011 ]. http://nccam.nih.gov
- 2.Barnes PM. Powell-Griner E. McFann K. Nahin RL. Complementary and alternative medicine use among adults: United States, 2002. Adv Data. 2004;343:1–19. [PubMed] [Google Scholar]
- 3.Astin JA. Why patients use alternative medicine: Results of a national study. JAMA. 1998;279:1548–1553. doi: 10.1001/jama.279.19.1548. [DOI] [PubMed] [Google Scholar]
- 4.Eisenberg DM. Davis RB. Ettner SL, et al. Trends in alternative medicine use in the United States, 1990–1997: Results of a follow-up national survey. JAMA. 1998;280:1569–1575. doi: 10.1001/jama.280.18.1569. [DOI] [PubMed] [Google Scholar]
- 5.Tindle HA. Davis RB. Phillips RS. Eisenberg DM. Trends in use of complementary and alternative medicine by US adults: 1997–2002. Altern Ther Health Med. 2005;11:42–49. [PubMed] [Google Scholar]
- 6.Kessler RC. Davis RB. Foster DF, et al. Long-term trends in the use of complementary and alternative medical therapies in the United States. Ann Intern Med. 2001;135:262–268. doi: 10.7326/0003-4819-135-4-200108210-00011. [DOI] [PubMed] [Google Scholar]
- 7.Wetzel MS. Kaptchuk TJ. Haramati A. Eisenberg DM. Complementary and alternative medical therapies: Implications for medical education. Ann Intern Med. 2003;138:191–196. doi: 10.7326/0003-4819-138-3-200302040-00011. [DOI] [PubMed] [Google Scholar]
- 8.Pearson NJ. Chesney MA. The CAM Education Program of the National Center for Complementary and Alternative Medicine: An overview. Acad Med. 2007;82:921–926. doi: 10.1097/ACM.0b013e31814a5014. [DOI] [PubMed] [Google Scholar]
- 9.Bent S. Herbal medicine in the United States: Review of efficacy, safety, and regulation: Grand rounds at University of California, San Francisco Medical Center. J Gen Intern Med. 2008;23:854–859. doi: 10.1007/s11606-008-0632-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hsiao AF. Wong MD. Goldstein MS, et al. Variation in complementary and alternative medicine (CAM) use across racial/ethnic groups and the development of ethnic-specific measures of CAM use. J Altern Complement Med. 2006;12:281–290. doi: 10.1089/acm.2006.12.281. [DOI] [PubMed] [Google Scholar]
- 11.Katz P. Lee F. Racial/ethnic differences in the use of complementary and alternative medicine in patients with arthritis. J Clin Rheumatol. 2007;13:3–11. doi: 10.1097/01.rhu.0000255579.59597.d2. [DOI] [PubMed] [Google Scholar]
- 12.Paramore LC. Use of alternative therapies: Estimates from the 1994 Robert Wood Johnson Foundation National Access to Care Survey. J Pain Symptom Manage. 1997;13:83–89. doi: 10.1016/s0885-3924(96)00299-0. [DOI] [PubMed] [Google Scholar]
- 13.Bausell RB. Lee WL. Berman BM. Demographic and health-related correlates of visits to complementary and alternative medical providers. Med Care. 2001;39:190–196. doi: 10.1097/00005650-200102000-00009. [DOI] [PubMed] [Google Scholar]
- 14.Druss BG. Rosenheck RA. Association between use of unconventional therapies and conventional medical services. JAMA. 1999;282:651–656. doi: 10.1001/jama.282.7.651. [DOI] [PubMed] [Google Scholar]
- 15.Ni H. Simile C. Hardy AM. Utilization of complementary and alternative medicine by United States adults: Results from the 1999 national health interview survey. Med Care. 2002;40:353–358. doi: 10.1097/00005650-200204000-00011. [DOI] [PubMed] [Google Scholar]
- 16.Graham RE. Ahn AC. Davis RB, et al. Use of complementary and alternative medical therapies among racial and ethnic minority adults: Results from the 2002 National Health Interview Survey. J Natl Med Assoc. 2005;97:535–545. [PMC free article] [PubMed] [Google Scholar]
- 17.Keith VM. Kronenfeld JJ. Rivers PA. Liang SY. Assessing the effects of race and ethnicity on use of complementary and alternative therapies in the USA. Ethn Health. 2005;10:19–32. doi: 10.1080/1355785052000323010. [DOI] [PubMed] [Google Scholar]
- 18.Mackenzie ER. Taylor L. Bloom BS, et al. Ethnic minority use of complementary and alternative medicine (CAM): A national probability survey of CAM utilizers. Altern Ther Health Med. 2003;9:50–56. [PubMed] [Google Scholar]
- 19.Signorello LB. Hargreaves MK. Blot WJ. The Southern Community Cohort Study: Investigating health disparities. J Health Care Poor Underserved. 2010;21(1 suppl):26–37. doi: 10.1353/hpu.0.0245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Signorello LB. Hargreaves MK. Steinwandel MD, et al. The Southern Community Cohort Study: Establishing a cohort to investigate health disparities. J Natl Med Assoc. 2005;97:927–929. [PMC free article] [PubMed] [Google Scholar]
- 21.Hargreaves MK. Aronld CW. Blot WJ. Community health centers: Their role in the treatment of minorities and in health disparities research. In: Satcher D, editor; Pamies RJ, editor. Multiculture Medicine and Health Disparities. New York: McGraw-Hill; 2006. pp. 485–494. [Google Scholar]
- 22.Barnes PM. Bloom B. Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;10:1–23. [PubMed] [Google Scholar]
- 23.Lafferty WE. Tyree PT. Bellas AS, et al. Insurance coverage and subsequent utilization of complementary and alternative medicine providers. Am J Manag Care. 2006;12:397–404. [PMC free article] [PubMed] [Google Scholar]
- 24.Cherkin DC. Deyo RA. Sherman KJ, et al. Characteristics of visits to licensed acupuncturists, chiropractors, massage therapists, and naturopathic physicians. J Am Board Fam Pract. 2002;15:463–472. [PubMed] [Google Scholar]
- 25.Dessio W. Wade C. Chao M, et al. Religion, spirituality, and healthcare choices of African-American women: Results of a national survey. Ethn Dis. 2004;14:189–197. [PubMed] [Google Scholar]
- 26.Levin J. Chatters LM. Taylor RJ. Religion, health and medicine in African Americans: Implications for physicians. J Natl Med Assoc. 2005;97:237–249. [PMC free article] [PubMed] [Google Scholar]
- 27.Brown CM. Barner JC. Richards KM. Bohman TM. Patterns of complementary and alternative medicine use in African Americans. J Altern Complement Med. 2007;13:751–758. doi: 10.1089/acm.2006.6392. [DOI] [PubMed] [Google Scholar]