Abstract
Objectives
Shoulder pain, for which acupuncture has been used, is a common complication after a stroke that interferes with the function of the upper extremities. The aim of this systematic review is to summarize and evaluate the effects of acupuncture for shoulder pain after stroke.
Methods
Randomized controlled trials (RCTs) involving the effects of acupuncture for shoulder pain, published between January 1990 and August 2009, were obtained from the National Libraries of Medicine, MEDLINE®, CINAHL, AMED, Embase, Cochrane Controlled Trials Register 2009, Korean Medical Database (Korea Institute of Science Technology Information, DBPIA, KoreaMed, and Research Information Service System), and the Chinese Database (China Academic Journal).
Results
Among the 453 studies that were obtained (300 written in English, 137 in Chinese, and 16 in Korean), 7 studies met the inclusion criteria for this review. All of them were RCTs published in China and reported positive effects of the treatment. The quality of the studies was assessed by the Modified Jadad Scores (MJS) and the Cochrane Back Review Group Criteria List for Methodologic Quality Assessment of RCTs (CBRG); the studies scored between 2 and 3 points on MJS, and between 4 and 7 points on CBRG.
Conclusions
It is concluded from this systematic review that acupuncture combined with exercise is effective for shoulder pain after stroke. It is recommended that future trials be carefully conducted on this topic.
Introduction
Shoulder pain is a common complication after stroke, interfering with the function of the upper extremities, regular daily activities, and active rehabilitation.1,2 The prevalence of shoulder pain relative to the degree of paralysis ranges from 16% to 84%.3 Over 70% of stroke patients experience significant shoulder pain.4
Shoulder pain after stroke has been connected with contracture of the shoulder, glenohumeral subluxation, injury of the axillary nerve, rupture of the rotator cuff, and spasticity of shoulder muscles, and it is associated with poor motor recovery.2 Therefore, it is very important for stroke patients to treat shoulder pain properly. For good motor recovery, various treatments have been suggested, including electrical stimulation, ultrasound, acupuncture, herbal medicine, exercise, taping, and physical therapy.
Acupuncture has been practiced for thousands of years, and it has been widely used in various conditions that include pain, musculoskeletal disorders, and several neurologic disorders.5,6 Recent articles reviewing the efficacy and safety of acupuncture in stroke have appeared, but no clear effects of acupuncture were shown.7,9 In the literature, there has been no systematic review assessing the effects of acupuncture for shoulder pain following stroke. Therefore, the aim of this study was to summarize and evaluate the results of relevant trials involving this area.
Methods
Search methods for identification of relevant studies
Randomized controlled trials (RCTs) reporting effects of acupuncture for shoulder pain, published between January 1990 and August 2009, were obtained from the National Libraries of Medicine, MEDLINE®, CINAHL, AMED, Embase, the Cochrane Controlled Trials Register 2009, Korean Medical database (Korea Institute of Science Technology Information, DBPIA, KoreaMed, and Research Information Service System), and the Chinese database (China Academic Journal). Articles written in the English, Korean, and Chinese languages were included in the search. The search string used was (stroke OR cva OR cerebrovascular accident OR intracranial hemorrhage OR ich OR cerebral infarction) AND (shoulder pain OR adhesive capsulitis OR subluxation OR RSD OR CRPS) AND (acupuncture OR electroacupuncture OR electrical stimulation).
Criteria for considering studies for this review
All prospective randomized controlled clinical studies of acupuncture for shoulder pain after stroke were considered. Trials that included patients of any age or sex, with any type of stroke, and with or without computed tomography scan were eligible. Trials were included if they were randomized studies of acupuncture or electroacupuncture as the sole treatment or as combined with other treatments. Trials that compared two different types of acupuncture were excluded.
Quality assessments for this review
Two (2) independent reviewers screened titles and abstracts of the database and searched for relevant articles according to predefined criteria. These reviewers also assessed the quality using the Modified Jadad Score (MJS)10,11 and the Cochrane Back Review Group Criteria List for Methodologic Quality Assessment of RCTs (CBRG).12
The MJS included the following criteria: method of randomization, double blinding, and reporting of withdrawal and dropouts. The CBRG was also examined, including the randomization method, concealment of treatment allocation, similar baseline, assessor blinding, selection of co-intervention, treatment compliance, dropouts, outcome measurement method, and intention-to-treat analysis. Quality assessment was performed by 2 independent reviewers, and disagreements were resolved by discussions between them.
Results
Study description
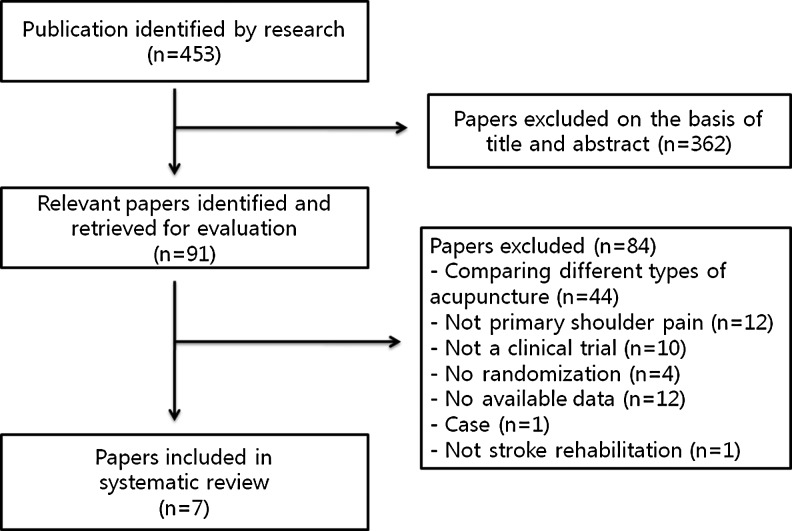
Among the 453 studies obtained from the authors' search (300 written in English, 137 in Chinese, and 16 in Korean), 362 studies were excluded on the basis of title and abstract outright (Fig. 1). Then an additional 84 studies were excluded as comparing different types of acupuncture, not relevant to primary shoulder pain, not a clinical trial, not a randomized trial, data not available, no more than a case report, or not relevant to stroke rehabilitation. Seven (7) studies finally met the inclusion criteria. All of them were RCTs published in China, and the results they describe all showed positive acupuncture effects.
FIG. 1.
Flowchart of the trial selection of studies included in the review.
Among the seven included studies, four compared a combined acupuncture/exercise treatment with exercise alone, one compared a combined acupuncture/exercise with drug treatment, one compared a combined acupuncture/exercise with combined drug treatment/exercise, and one compared electroacupuncture with transcutaneous electrical nerve stimulation (TENS) treatment (Table 1).
Table 1.
Characteristics of the Trials Included in This Review
| |
|
|
Interventions |
Outcomes |
Quality assessment |
||
|---|---|---|---|---|---|---|---|
| Country | Participants | Treatment group | Control group | Outcome measure | Results reported | MJS CBRG | |
| ➀ Clinical study on acupuncture combined with rehabilitation therapy for treatment of poststroke shoulder–hand syndrome Shang YJ et al.13 (2008) | China | (a) Acupuncture combined with rehabilitative exercises (n=40) - Average age: 53.42 years - Stage and severity of disease: 5.23 months (b) Acupuncture group (n=40) - Average age: 52.38 years - Stage and severity of disease: 5.37 months (c) Rehabilitation group (n=40) - Average age: 51.79 years - Stage and severity of disease: 5.02 months Stroke nature: not explained |
(a) Acupuncture combined with rehabilitative exercises - Simple acupuncture: 8 acupoints (LI15, jianquan, TE14, HT1, LI14, LI11, PC(HP)6, LI4): 2 sessions/day, 40 min, 30 days, total 60 sessions - Rehabilitative exercises: Bobath, OT: 2 sessions/day, approximately 30–40 min, 30 days, total 60 sessions |
(b) Acupuncture group - Simple acupuncture: 8 acupoints (LI15, jianquan, TE14, HT1, LI14, LI11, HP6, LI4) : 2 sessions/day, 40 min, 30 days, total 60 session (c) Rehabilitation group - Rehabilitative exercises: Bobath, OT: 2 sessions/day, approximately 30–40 min, 30 days, total 60 sessions |
FMA VAS ROM |
(a) Group significantly superior for all outcomes than (b)(c) group | MJS: 2 CBRG: 5 |
| ➁ Shoulder subluxation after stroke treated with acupuncture combined with rehabilitative exercises Zhu XJ et al.14 (2007) | China | (a) Acupuncture combined with rehabilitative exercises (n=30) - Average age: 54.79 years - Stage and severity of disease: 2.85 months (b) Rehabilitative group (n=30) - Average age: 55.29 years - Stage and severity of disease: 2.04 months Stroke nature: cerebral infarction |
(a) Acupuncture combined with rehabilitative exercises -Scalp acupuncture: 2 acupoints zone (Ding zone, Dingqian zone): 1 session/day, 6 hours, 6 sessions/week total 1 month (24 sessions) -Body acupuncture: 4 acupoints (LI15 with SI9, LE14 with SJ13): 1 sessions/day, 30 min, 6 sessions/week total 1 month (24 sessions) - Rehabilitative exercises: 1 session/day, 30 min daily for 1 month |
(b) Rehabilitative group - Rehabilitative exercises: 1 session/day, 30 min daily for 1 month |
VAS ROM Clinical score of neural lesion |
(a) Group significantly superior for all outcomes than (b) group | MJS: 2 CBRG: 4 |
| ➂ Shoulder-hand syndrome after stroke treated with acupuncture of 30 cases, Zhao XF et al.15 (2004) | China | (a) Acupuncture combined with rehabilitative exercises (n=30) -Average age: 55.43 years -Stage and severity of disease: 9–245 days (b) Rehabilitation exercises (n=24) - Average age: 57.26 years - Stage and severity of disease: 7–260 days Stroke nature: cerebral infarction |
(a) Acupuncture combined with rehabilitative exercises - Acupuncture: 7 acupoints (Jingbi, SI11, LI15, LI11, SJ7, SJ4, EX-UE9(Baxie)): 1 session/day, 20 min daily for 10 day, 10 sessions constituted a courses, with 3-day interval between courses, total 2 time courses (total 20 sessions) - Rehabilitation exercise: 1 session/day, 40 min daily for 10 days, 10 sessions constituted a course, with 3-day interval between courses, total 2 time courses (total 20 sessions) |
(b) Rehabilitative group - Rehabilitation exercise - 1 session/day, 40 min daily for 10 days, 10 sessions constituted a courses, with 3-day interval between courses, total 2 time courses (total 20 sessions) 23-day |
FMA | (a) Group significantly superior for all outcome than (b) group | MJS: 2 CBRG: 6 |
| ➃ Wrist–ankle needle combined with rehabilitative exercises treated hemiplegia patients with shoulder pain in 36 cases, Xiong et al.17 (2001) | China | (a) Acupuncture combined with rehabilitative exercises (n=36) -Average age : 58.9 years -Stage and severity of disease: unclear (b) Drug treatment (n=32) -Average age: 60.3 years -Stage and severity of disease: unclear Stroke nature: cerebral infarction |
(a) Acupuncture combined with rehabilitative exercises -Acupuncture: 3 acupoints (acupoints upper Four, Five and Six): 1 session/day 30 min daily for 10 days - Rehabilitative exercises: 1 session/day 30 min daily for 10 days |
(b) Drug treatment - Fenbid 0.6 g, 3 times/day+vitamin B1, 2 times/day daily for 10 days |
ROM | (a) Group significantly superior for outcome than (b) group | MJS: 2 CBRG: 5 |
| ➄ Observation of curative effect of acupuncture combined with rehabilitation training on hemiplegia patients with shoulder pain, Zhou GH16 (2002) | China | (a) Acupuncture combined with rehabilitation training (n=50) - Average age: 53.8 years - Stage and severity of disease: 1.61 months (b) Rehabilitation training (n=50) - Average age: 54.2 years - Stage and severity of disease: 1.66 months stroke nature: not explained |
(a) Acupuncture combined with rehabilitation training - acupuncture: 7 acupoints (LI15, LE14, SI9, LI11, LI10, SJ5, LI4): 1 sessions/day, 20 min, 4 weeks - Rehabilitation training: Bobath, Rood, Brunnstrom: 1 session/day, 30 min, 4 weeks |
(b) Rehabilitation training - Bobath, Rood, Brunnstrom: 1 session/day, 30 min, 4 weeks 4 weeks |
VAS Brunnstrom's classification of upper limbs |
(a) Group significantly superior for all outcomes than (b) group | MJS: 2 CBRG: 6 |
| ➅ The rehabilitation effects of wrist–ankle needle on omalgia for poststroke patients, Zhang GP18 (2001) | China | (a) Acupuncture combined with exercise (n=20) - Average age: 65.82 years - Stage and severity of disease: 1 day −1 year (b) Drug treatment combined with exercise (n=20) - Average age: 68.7 years - Stage and severity of disease: 1 day–1 year Stroke nature: cerebral infarction |
(a) Acupuncture combined with exercise - Acupuncture: acupoints Upper One, Five, and A-shi point (3 points and less): 1 session/day, 2 hours/session daily for 15 days, 15 sessions constituted a course - Exercise treatment: shoulder joint range of motion exercise: 1 session/day, 45 min/session daily for 15 days, 15 sessions constituted a course |
(b) Drug treatment combined with exercise - Drug treatment: diclofenac diethylamine emulgel for external application: 2–4 g, 3 times/day, every day right after the first drugs to treat exercise - Exercise treatment: shoulder joint range of motion exercise: 1 session/day, 45 min/session daily for 15 days, 15 sessions constituted a course, 15 days |
VAS FMA MAS MMT ADL Brunnstrom's classification of upper limbs |
(a) Group significantly superior for VAS, FMA than (b) group | MJS: 3 CBRG: 7 |
| ➆ Comparative study of curative effect of low-cycle treatment and electro-acupuncture for a shoulder joint half-dislocation caused by apoplexy, hemiplegy, Zhang HY19 (2008) | China | (a) Electro acupuncture treatment group (n=30) - Average age: 59.87 years - Stage and severity of disease: ≤6 months (b) TENS treatment group (n=30) - Average years: 60.27 years - Stage and severity of disease: ≤6 months Stroke nature: cerebral infarction |
(a) Electroacupuncture treatment group -Electroacupuncture: 4 acupoints (LI15 with SI9, SI11 with LE14): 1 session/day, 30 min daily for 10 days, 10 sessions constituted a course, with 1-day interval between courses, total 3 courses |
(b) TENS treatment group -TENS: 4 acupoints(LI15 with SI9, SI11 with LE14): 100, 500, and 100 Hz, about 20–70 mA, 50 μ: 1 session/day, 20 min daily for 10 days, 10 sessions constituted a course, with 1-day interval between courses, total 3 courses, 32 days |
VAS Degree of shoulder joint half dislocation |
(a) Group significantly superior for VAS only (b) group | MJS: 2 CBRG: 5 |
MJS, Modified Jadad Score; CBRG, Cochrane Back Review Group Criteria List; FMA, Fugl-Meyer Assessment; VAS, Visual Analogue Scale; ROM, range of motion; OT, occupational therapy; MAS, Modified Ashworth Scale; MMT, manual muscle testing; ADL, activities of daily living.
Study quality
The average assessment of quality based on the MJS of each study was moderate (mean of 2.1, range of 2–3) (Table 1). Among the seven studies, six studies were scored with 2 points (1 point for the methods of randomization, and 1 for withdrawals/dropouts). One (1) study was scored with 3 points (1 point for the methods of randomization, 1 for blinding, and 1 for withdrawals/dropouts).
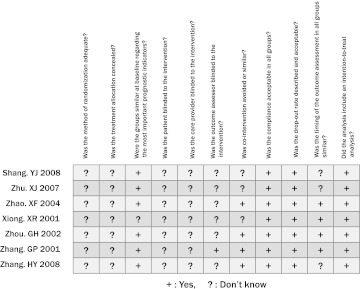
The average of quality using the CBRG score was moderate (mean of 5.4, range of 4–7) (Fig. 2). The CBRG was presented in Figure 1. According to this measure, the studies were insufficient in adequate randomization, concealed allocation, patient blinding, assessor blinding, and similar outcome assessment.
FIG. 2.
Assessment of the quality of the studies included in the review.
Outcomes
The study of Shang13 was divided into three groups: acupuncture combined with exercise, acupuncture alone, and exercise alone. There were significant differences between the combined acupuncture/exercise and the acupuncture-alone groups in outcome determined by the Fugl-Meyer Assessment (FMA), visual analogue scale (VAS), and range of motion (ROM). There was also a significant difference between the combined acupuncture/exercise and exercise-alone groups in outcome determined by the same tests.
Among the seven studies included in this review, three studies compared combined acupuncture/exercise to exercise alone for treating shoulder pain. Three (3) studies found that there was significant improvement in all outcomes determined by VAS14,16, ROM14, clinical score of neural lesion14, FMA15, and Brunnstrom's classification of upper limbs16 after intervention.
Xiong17 suggested that the outcome measure of ROM was significantly superior in the group treated with acupuncture combined with rehabilitative exercises rather than drug treatment.
Zhang18 found that there were significant differences in outcome measured by VAS and FMA in the combined acupuncture/exercise group compared to combined drug treatment/exercise. However, the outcome measure by Modified Ashworth Scale, Manual Muscle Test, Activity of Daily Living, and Brunnstrom's classification of upper limbs indicated no differences between the two groups.
Zhang19 showed that the outcome measure of pain by VAS was significantly lower in the electroacupuncture group than in the TENS group, whereas the outcome measure in degree of shoulder joint half dislocation indicated no difference between the two groups.
For the studies using the same measurements, three studies examining acupuncture effect on shoulder pain after stroke recorded changes in VAS after intervention. According to those studies, there was a significant effect in relieving the shoulder pain after acupuncture combined with exercise, which was more effective compared against the exercise alone. Shang,13 Zhu,14 and Zhou16 used a pain-intensity scale by VAS that ranged between 0 and 5, 0 and 75, and 0 and 100, respectively. Even though these studies had not used standardized pain scale as an outcome measure, three studies reported that acupuncture was effective in improving the shoulder pain.
Discussion
This systematic review provides suggestive evidence for the effectiveness of acupuncture in treating shoulder pain after stroke. However, the total numbers of RCTs were too small to draw concrete conclusions about the effectiveness of the therapeutic approach. Several other systematic reviews assessing the effects of acupuncture for stroke have been published.20,21 Most of them focused on the recovery of general status after stroke in rehabilitation, as measured by the Barthel Index, Nottingham Health Profile, or Scandinavian Stroke Scale. There were several limitations in the evidence showing an effect of acupuncture for stroke.
Zhang et al.8 reported that acupuncture appeared to be safe but without clear evidence of benefit in cases of acute stroke. Also, Wu et al.7 concluded that there is no clear evidence relating to the effects of acupuncture in subacute or chronic stroke.
The systematic review performed for this report study focused on uncovering evidence of the effects of acupuncture for shoulder pain after stroke, instead of a broader assessment of pain after stroke. Therefore, all relevant trials relating to the effects of acupuncture on shoulder pain after stroke were identified, including studies reported in both Western and Eastern databases. Among the 453 studies retrieved, only 7 of them met the inclusion criteria for this article. All seven studies were RCTs performed in China, and six showed favorable results for combined acupuncture/exercise compared with a control group, such as acupuncture or exercise alone, or a combined drug treatment/exercise or drug treatment regimen. One (1) study showed favorable results for electroacupuncture compared with TENS treatment. For measurement of outcome, VAS was used as the pain scale in the five studies. This scale is a common tool for evaluating pain intensity. Pain relief is an important treatment in stroke rehabilitation or common rehabilitation. In the quality assessment, by MJS the studies scored in the range of 2–3, and by CBRG in the range of 4–7. Even though the average assessments of quality were moderate, the systematic review provides appropriate significant evidence showing the effectiveness of acupuncture in treating shoulder pain after stroke.
“Acupuncture” means “puncture with a needle” (acus in Latin means “needle”). Acupuncture has been found to relieve pain, sometimes quite dramatically, in many chronic conditions.22 There is no clear evidence of the effects of acupuncture on stroke rehabilitation. Acupuncture has biologic effects that might improve recovery from stroke or facilitate rehabilitation.7 Properly performed acupuncture seems to be a safe procedure. Basic scientific research is beginning to provide evidence that offers plausible mechanisms for the presumed physiologic effects of acupuncture. Multiple research approaches have shown that acupuncture activates endogenous opioid mechanisms.23
Acupuncture is a nondrug therapy that is being used more and more often to treat shoulder pain. It is thought that acupuncture works by releasing chemical compounds in the body that relieve pain, by overriding pain signals in the nerves, or by allowing energy (qi) or blood to flow freely through the body.2 Although the exact mechanism of this treatment remains unclear, it is apparent that reproducible neurological and chemical changes occur in response to acupuncture, and that these changes almost certainly modify the response to perception of pain.24
Even though this review has provided many positive conclusions, there are also several limitations. Although great efforts were made to retrieve all trials on the subject, only 7 studies among 453 studies that were retrieved met the inclusion criteria. All of them were published in China, and all showed positive results related to the effects of acupuncture. Moreover, it was not possible to perform a funnel plot for checking publication bias in this systematic review because of the limited number of trials for each outcome.
In addition, there were insufficient quality assessments with respect to allocation concealment, blinding of outcome assessors, and long-term follow-up. Therefore, larger methodologically sound trials would be required in order to confirm or refute the available evidence.
Conclusions
It was found in this review of reported RCTs that acupuncture is an effective treatment for shoulder pain after stroke. Acupuncture can be considered as an adjuvant therapy in combination with exercise for rehabilitation of the stroke patients who are suffering from shoulder pain. Further trials concerning this topic should be conducted according to the highest methodological standards for certainty.
Acknowledgments
This research was supported by a grant (08-B-02) from Korea National Rehabilitation Research Institute.
Disclosure Statement
No competing financial interests exist.
References
- 1.Griffin JW. Hemiplegic shoulder pain. Phys Ther. 1986;66:1884–1893. doi: 10.1093/ptj/66.12.1884. [DOI] [PubMed] [Google Scholar]
- 2.Turner-Stokes L. Jackson D. Shoulder pain after stroke: A review of the evidence base to inform the development of an integrated care pathway. Clin Rehabil. 2002;16:276–298. doi: 10.1191/0269215502cr491oa. [DOI] [PubMed] [Google Scholar]
- 3.Snels IA. Dekker JH. van der Lee JH, et al. Treating patients with hemiplegic shoulder pain. Am J Phys Med Rehabil. 2002;81:150–160. doi: 10.1097/00002060-200202000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Bohannon RW. Larkin PA. Smith MB. Horton MG. Shoulder pain in hemiplegia: Statistical relationship with five variables. Arch Phys Med Rehabil. 1986;67:514–516. [PubMed] [Google Scholar]
- 5.Ernst E. Acupuncture: A critical analysis. J Intern Med. 2006;259:125–137. doi: 10.1111/j.1365-2796.2005.01584.x. [DOI] [PubMed] [Google Scholar]
- 6.Ernst E. Acupuncture. Lancet Oncol. 2010;11:20. doi: 10.1016/S1470-2045(09)70399-7. [DOI] [PubMed] [Google Scholar]
- 7.Wu HM. Tang JL. Lin XP, et al. Acupuncture for stroke rehabilitation. Cochrane Database Syst Rev. 2006;3:CD004131. doi: 10.1002/14651858.CD004131.pub2. [DOI] [PubMed] [Google Scholar]
- 8.Zhang SH. Liu M. Asplund K. Li L. Acupuncture for acute stroke. Cochrane Database Syst Rev. 2005;2:CD003317. doi: 10.1002/14651858.CD003317.pub2. [DOI] [PubMed] [Google Scholar]
- 9.Sze FK. Wong E. Or KK, et al. Does acupuncture improve motor recovery after stroke? A meta-analysis of randomized controlled trials. Stroke. 2002;33:2604–2619. doi: 10.1161/01.str.0000035908.74261.c9. [DOI] [PubMed] [Google Scholar]
- 10.White AR. Ernst E. A systematic review of randomized controlled trials of acupuncture for neck pain. Rheumatology (Oxford) 1999;38:143–147. doi: 10.1093/rheumatology/38.2.143. [DOI] [PubMed] [Google Scholar]
- 11.Jadad AR. Moore RA. Carroll D, et al. Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 12.van Tulder M. Furlan A. Bombardier C. Bouter L. Updated method guidelines for systematic reviews in the Cochrane Collaboration Back Review Group. Spine (Phila Pa 1976) 2003;28:1290–1299. doi: 10.1097/01.BRS.0000065484.95996.AF. [DOI] [PubMed] [Google Scholar]
- 13.Shang YJ. Ma CC. Cha YY, et al. Clinical study on acupuncture combined with rehabilitation therapy for treatment of poststroke shoulder-hand syndrome. Chin Acupuncture Moxibustion. 2008;28:331–333. [PubMed] [Google Scholar]
- 14.Zhu XJ. Gao WB. Yang XY. Shoulder subluxation after stroke treated with acupuncture combined with rehabilitative exercises. J Beijing Univ Chin Med. 2007;14:23–25. [Google Scholar]
- 15.Zhao XF. Song H. Shoulder-hand syndrome after stroke treated with acupuncture of 30 cases. Chin J Information Trad Chin Med. 2004;11:532–533. [Google Scholar]
- 16.Zhou GH. Observation of curative effect of acupuncture combined with rehabilitation training on hemiplegia patients with shoulder pain. Chin J Rehabil Theory Pract. 2002;8:244–245. [Google Scholar]
- 17.Xiong XR. Lin Q. Yao ZF. Yang CX. Wrist-ankle needle combined with rehabilitative exercises treated hemiplegia patients with shoulder pain of 36 cases. Fujian J TCM. 2001;32:33. [Google Scholar]
- 18.Zhang GP. The Rehabilitation Effects of Wrist-Ankle Needle on Omalgia for Post-stroke Patients. Fujian: Fujian University of Traditional Chinese Medicine; 2001. [Google Scholar]
- 19.Zhang HY. Study Comparatively the Curing Effect of Low Cycle Treatment and Electro-acupuncture Treatment in Curing the Shoulder Joint Half Dislocation Caused by Apoplexy Hemiplegy. Heilongjiang: Heilongjiang University of Chinese Medicine; 2008. [Google Scholar]
- 20.Park J. Hopwood V. White AR. Ernst E. Effectiveness of acupuncture for stroke: A systematic review. J Neurol. 2001;248:558–563. doi: 10.1007/s004150170132. [DOI] [PubMed] [Google Scholar]
- 21.Kong JC. Lee MS. Shin BC, et al. Acupuncture for functional recovery after stroke: A systematic review of sham-controlled randomized clinical trials. CMAJ. 2010;182:1723–1729. doi: 10.1503/cmaj.091113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Perlow BW. Acupuncture: Its theory and use in general practice. Proc R Soc Med. 1973;66:426–428. doi: 10.1177/003591577306600505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kaptchuk TJ. Acupuncture: theory, efficacy, and practice. Ann Intern Med. 2002;136:374–383. doi: 10.7326/0003-4819-136-5-200203050-00010. [DOI] [PubMed] [Google Scholar]
- 24.Lewith GT. How effective is acupuncture in the management of pain? J R Coll Gen Pract. 1984;34:275–278. [PMC free article] [PubMed] [Google Scholar]