Abstract
Aims
To report on the suturing techniques and aspects of postoperative management in penetrating keratoplasty in the United Kingdom.
Methods
A postal questionnaire was sent to 137 ophthalmic consultants identified from a Royal College of Ophthalmology database as having a special interest in anterior segment surgery. The questionnaire surveyed surgeon preferences for surgical and suturing technique for penetrating keratoplasty surgery, and the postoperative care of corneal grafts.
Results
In all, 68% of questionnaires were completed and returned: 73% of respondents used a Flieringa ring or equivalent, 94% routinely used cardinal sutures, with 50.5% removing them at the end of the procedure. The most common suturing technique for routine penetrating keratoplasty was a single continuous suture (35%). In these cases, a 10/0 nylon suture was used by 89%. Sixty-six percent changed their technique in high-risk cases, 52% used a 3-1-1 knot, and 75% made a distinction between a reef and granny knot, with 76% using a reef. Thirty percent buried the knots within the donor material, and 29% within the host tissue. Twenty-five percent had no routine time for graft suture removal, but 41% removed them between 1 and 2 years post-surgery. After suture removal, 98% used steroids and 88% used topical antibiotics. Thirty-four percent stopped topical steroids before suture removal, with 38% stopping topical steroids more than 3 months prior to suture removal.
Conclusion
This survey demonstrates that there is considerable variation in suturing techniques and postoperative care for penetrating keratoplasty. These significant variations in practice need to be considered when interpreting outcomes and research.
Keywords: corneal graft, penetrating keratoplasty, anterior segment surgery, cornea, corneal surgery, corneal transplantation
Introduction
The history of penetrating keratoplasty (PK) is almost 100 years old, starting with Elschnig in Prague and later Tudor-Thomas in the United Kingdom.1 There have been significant advances in instruments, suture materials, operating microscopes, medication, and surgical techniques used in PK surgery. A total of 2568 PK operations were undertaken in the United Kingdom in 2008–2009.2 There are a wide variety of suture techniques employed in corneal transplantation.3,4 They include single continuous (radial placement vs no torque), double continuous (same direction vs opposing pattern), interrupted, and a combination of interrupted and continuous sutures. Each technique has its own advantages and disadvantages, and suturing technique is perhaps the area of greatest variation in PK surgery. However, it is important that the surgeon is clear on the reason for their adopting a particular technique with a patient. Postoperative suture management is another area where great variation exists between surgeons. We designed this study to survey the suturing techniques and routine postoperative care regimes adopted by anterior segment specialists in the United Kingdom.
Materials and methods
In 2003, we identified all the consultants in the UK with an interest in corneal surgery from a Royal College of Ophthalmologists database. A postal questionnaire was sent out to 137 surgeons. It covered surgeons’ preferences for globe fixation and support for PK surgery (ie, the use of superior and inferior recti sutures, and circumstances in which a Flieringa ring is used), and included questions on the use of cardinal sutures, routine suture technique, whether technique was altered in high-risk cases, and routine postoperative management. The questionnaire was sent only once, and no reminder was posted.
Results
A total of 93 (68%) completed questionnaires were returned.
Globe fixation and support
For globe fixation, 40% used both inferior and superior rectus traction sutures, 4% used only superior, and 56% did not use them. Of those who used recti sutures, 95% used 4/0 (57%) and 6/0 (38%) silk.
For globe support, 73% of respondents used a Flieringa ring or the equivalent to provide scleral support. Of these respondents, 29.5% used a ring in all cases, 89% used a ring in aphakic patients, 33% in pseudophakic patients, and 4% in phakic patients. Other situations where a Fleiringa ring was used were pediatric cases, keratoconus, triple procedure, and vitrectomized eyes. The suture used to secure the ring included 6/0 silk (42%) or 6/0 polyglactin (Vicryl) (42%).
Routine graft suture technique
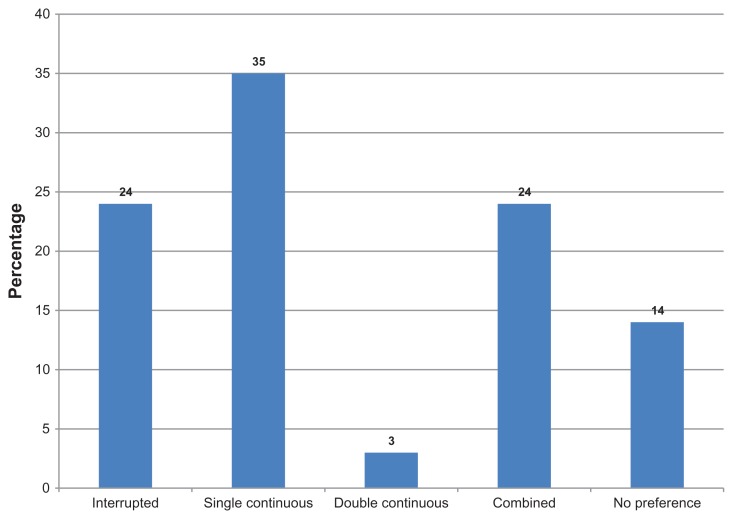
Ninety-four percent of respondents used nylon (10/0 or 6/0) for their cardinal sutures, and 4% used silk (6/0 or 8/0). In 50.5%, the cardinal sutures would be removed at the end of the procedure. Suture technique preference is summarized in Figure 1, respondents using nylon suture material in 89% and Mersilene in 3% of cases.
Figure 1.
Respondents’ preferences for corneal suturing technique employed.
Sixteen bites was the most popular choice for single continuous (39%) and interrupted (70%) suturing techniques. For combined interrupted and continuous sutures, 46% of respondents performed twelve continuous and twelve interrupted bites. In the majority of cases, the first suture is placed at 12 o’clock for cardinal sutures (86%), continuous (54%), and interrupted (76%) techniques.
Sixty-six percent of respondents reported changing from their usual suturing technique in high-risk cases (ie, vascularized corneas, multiple failed grafts, pediatric cases, therapeutic PK, and inflamed eyes). Of those that altered their techniques, 76 (82%) changed to an interrupted suture technique.
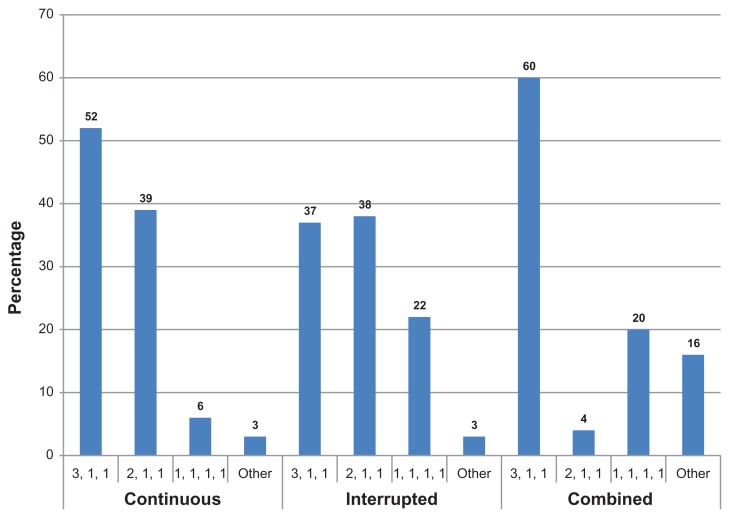
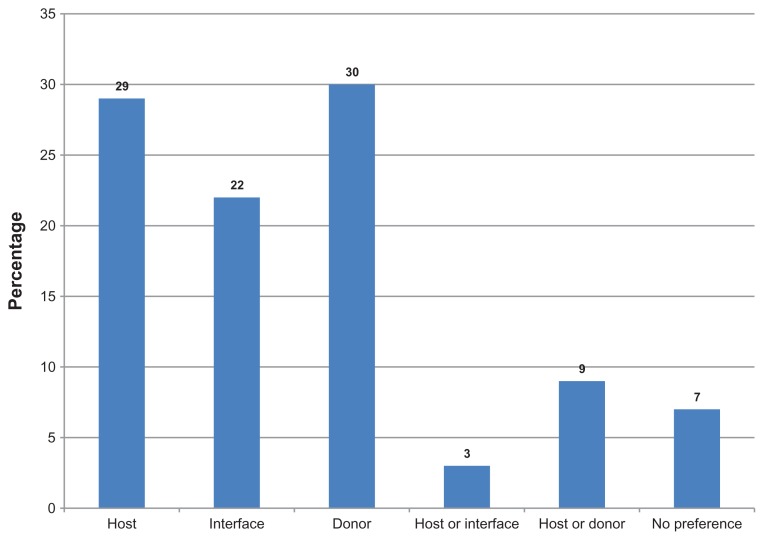
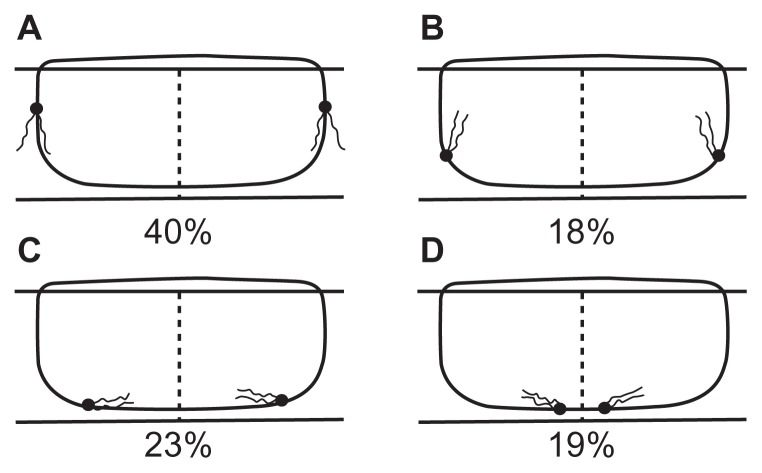
Knot technique is summarized in Figures 2 and 3. Seventy-five percent of respondents made a distinction between using a reef or a granny knot, and 76% of these respondents used a reef knot. The direction in which surgeons left knot tails facing is summarized in Figure 4.
Figure 2.
Respondents’ preferences for knots employed for different suturing techniques.
Figure 3.
Respondents’ preferences for position where knots were buried.
Figure 4.
Illustration of respondents’ preference for placing the direction of the tails of the knots: (A) facing away from the ocular surface; (B) facing towards the ocular surface; (C) facing towards the graft–host interface; (D) facing away from the graft–host interface.
Routine postoperative management
The majority (41%) removed all corneal sutures at 1–2 years, 24% removing sutures at 1 year, while 25% had no specific routine for the removal of graft sutures. When removing the knot, 47/89 (53%) responded that they pulled the knot through the host side, and 30/89 (34%) through the donor, with 12/89 (13%) replying “either.” Seven of 89 (8%) regularly pulled the knot through the interface.
Ninety-eight percent used topical steroids routinely following penetrating keratoplasty, 25% used topical steroids for 1 week, and 55% for between 1 week and 1 month, while 16% used topical steroids for more than 1 month. Eighty-eight percent of respondents used topical antibiotics following suture removal: 57% for 1 week, and 23% for 1 week to 1 month.
Thirty-four percent stopped topical steroids before suture removal, 38% of respondents stopping for more than 3 months before, 16% replying that their practice varied, and 22% did not specify for how long.
Discussion
The aim of this questionnaire survey was to assess trends in PK suturing technique and postoperative care among consultant ophthalmologists registered with the Royal College of Ophthalmologists with a special interest in anterior segment surgery. Lamellar surgery has become increasingly more popular, due to the reduced risk of immune rejection and intraoperative or postoperative complications.5,6 However PK surgery is still necessary in situations where there is full-thickness corneal disease. Our survey, performed in 2003, is therefore still relevant and applicable to ophthalmologists today. We had a good response rate (68%), which is comparable to other surveys on PK technique.3,4 Whereas previous surveys have focused more on such aspects of PK surgery as management of additional surgery and type of graft material used, our survey highlights the differences in surgical techniques used and postoperative management.
Globe fixation
The majority of respondents used a Flieringa ring or equivalent for support, especially in aphakic patients, but also with pediatric cases, keratoconus, vitrectomized eyes or triple procedures. In the pediatric eye, the Flieringa ring acts as a useful support due to the increased scleral elasticity and reduced rigidity of the eyes.7
Suturing technique
The results show that the most popular suturing technique in PK was single continuous (35%), comparable to 39% in the 1992 survey, and the most popular suture material was 10/0 nylon. There is continuing debate regarding which suturing technique is superior.8,9 However, other factors that can impact on postoperative astigmatism include patient diagnosis,10 tissue distribution, and preexisting donor shape, rather than suture pattern. Other advantages of using continuous sutures are the ease of placement of sutures, the ability to adjust loop tension intraoperatively as well as in the immediate postoperative period for reduction of astigmatism, and the presence of fewer knots that may irritate and induce vascularization.
The disadvantage of the continuous suture technique is the potential for corneal graft wound dehiscence if the suture should break, especially if only a single continuous suture has been used. Experimental studies on animal models have suggested that interrupted sutures have faster wound healing and a greater stromal inflammatory response, although there was no difference in blowout pressure between either suturing technique when comparing wound strength.11 Another study has suggested from its experimental model of wound closure that a continuous suture offers better wound closure than interrupted sutures.12 However, in our survey, 82% used interrupted sutures in high-risk cases. This is a much higher response than the 1992 paper, where only 28% of consultants altered their suturing technique.3
In our survey, only three respondents (3%) used Mersilene. These surgeons used the 11/0 Mersilene interrupted sutures. Mersilene is a non-biodegradable material with minor long term changes in postoperative astigmatism, unlike nylon sutures, which have a tendency to break.13 Mersilene sutures are associated with a higher risk of complications and interventions to correct suture-related problems in the first year postoperatively, but fewer suture-related complications have been observed at 2 years.14
The vast majority of surgeons (75%) make a distinction between reef and granny knot. Hammond et al demonstrated with electron microscopy that a 2-1-1 nylon reef knot was a slim knot that allowed easier knot burial and atraumatic suture removal, thus reducing the risk of wound dehiscence.15 The way in which the knots are buried can determine how easily they can be removed later on. It is generally undesirable to drag the knot through the graft–host interface, and we would recommend that the knots should not be buried at the interface.
Postoperative care
Although 25% of surgeons had no set routine for suture removal, 68% tended to remove them within 2 years. In the 1992 survey,3 a greater proportion of respondents had no set routine for suture removal (44%), although removal of sutures was comparable with our survey at 1 year (24% vs 33%) and at 2 years (8% vs 7%). In our survey, 34% stopped topical steroids before suture removal, ranging from 1 week to more than 3 months. There is ongoing debate as to whether topical steroids impair wound healing. In some animal studies, reduced fibroblastic response and impaired wound healing have been found,16 whereas in others no difference was found when compared with a placebo.17 However, in keeping with other surveys of postoperative care, the majority of surgeons in our survey used topical steroids following PK, although the duration of treatment was variable.18
Graft rejection can occasionally occur following removal of sutures,19 and consequently 98% of respondents tended to cover such risk by giving topical steroid. Most (80%) were given for up to a 1-month period. The removal of corneal sutures can also increase the risk of wound dehiscence following trauma.20 However long-term sutures can become loose or break with time, and this is associated with microbial keratitis, which can result in a failed graft or reduced visual acuity.21 We found that the majority of surgeons tended to cover suture removal with antibiotic prophylaxis to try and prevent this.
We would recommend using a Flieringa ring for support in certain circumstances such as aphakic eyes, pseudophakic eyes, or those eyes to be rendered aphakic or pseudophakic as part of the procedure, and pediatric eyes. While surgeons can choose freely between single continuous or interrupted sutures, we would recommend the latter for high-risk cases such as children and hot eyes (infection and inflammation), as there will be a high risk of early suture loosening. We consider 10-0 monofilament nylon superior to other suture material. Except where tension is important, such as the four cardinal sutures, we would recommend a 2-1-1 knot (preferably reef), as it has a small profile that allows for easier knot burial and atraumatic suture removal at a later date. Although there is debate as to which side of the interface the knot should be buried, it is certainly undesirable to pull the knot through the interface. Topical steroids should be stopped before suture removal, but then should be reinitiated with topical antibiotic cover after removal of sutures.
Limitations of this study include the fact that it was performed only in the United Kingdom and therefore may not be applicable to other parts of the world. We also did not assess for differences in surgical techniques and postoperative management in lamellar graft surgery, although this is being planned for our next study, which is about to commence.
Conclusion
The results of this survey provide a snapshot of surgical techniques preferred by corneal surgeons for PK in the United Kingdom, and demonstrate that a great degree of variation exists in PK techniques and postoperative management of corneal grafts. These significant variations in practice need to be considered when interpreting outcomes and research.
Footnotes
Disclosure
No financial support was received for this submission. None of the authors has any conflict of interest with this work.
References
- 1.Foster CS, Azar DT, Dohlman CH, editors. Smolin and Thoft’s the Cornea: Scientific Foundations and Clinical Practice. Philadelphia: Lippincott Williams & Wilkins; 2004. [Google Scholar]
- 2.UK transplant activity 2008–2009 report. [Accessed June 19, 2011]. Available at: http://www.organdonation.nhs.uk/ukt/statistics/transplant_activity_report/archive_activity_reports/pdf/ukt/transplant_activity_uk_2008-2009.pdf.
- 3.Burdon MA, McDonnell P. A survey of corneal graft practice in the United Kingdom. Eye (Lond) 1995;9(Pt 6 Suppl):6–12. [PubMed] [Google Scholar]
- 4.Steven P, Winter R, Geerling G. Current state of mechanical corneal surgery – results of a questionnaire to members of the cornea section of the German Society of Ophthalmologists. German Klin Monbl Augenheilkd. 2006;223(10):844–848. doi: 10.1055/s-2006-926813. [DOI] [PubMed] [Google Scholar]
- 5.Tan DT, Anshu A, Mehta JS. Paradigm shifts in corneal transplantation. Ann Acad Med Singapore. 2009;38(4):332–338. [PubMed] [Google Scholar]
- 6.Reinhart WJ, Musch DC, Jacobs DS, Lee WB, Kaufman SC, Shtein RM. Deep anterior lamellar keratoplasty as an alternative to penetrating keratoplasty: a report by the American Academy of Ophthalmology. Ophthalmology. 2011;118(1):209–218. doi: 10.1016/j.ophtha.2010.11.002. [DOI] [PubMed] [Google Scholar]
- 7.Vanathi M, Panda A, Vengayil S, Chaudhuri Z, Dada T. Pediatric keratoplasty. Surv Ophthalmol. 2009;54(2):245–271. doi: 10.1016/j.survophthal.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 8.Solano JM, Hodge DO, Bourne WM. Keratometric astigmatism after suture removal in penetrating keratoplasty: double running versus single running suture techniques. Cornea. 2003;22(8):716–720. doi: 10.1097/00003226-200311000-00002. [DOI] [PubMed] [Google Scholar]
- 9.Kim SJ, Wee WR, Lee JH, Kim MK. The effect of different suturing techniques on astigmatism after penetrating keratoplasty. J Korean Med Sci. 2008;23(6):1015–1019. doi: 10.3346/jkms.2008.23.6.1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Claesson M, Armitage WJ, Fagerholm P, Stenevi U. Visual outcome in corneal grafts: a preliminary analysis of the Swedish Corneal Transplant Register. Br J Ophthalmol. 2002;86(2):174–180. doi: 10.1136/bjo.86.2.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eliason J, McCulley J. A comparison between interrupted and continuous suturing techniques in keratoplasty. Cornea. 1990;9(1):10–16. [PubMed] [Google Scholar]
- 12.Au YK, Mahjoub S, Hart J. A comparison of the wound integrity produced by various suture patterns in penetrating keratoplasty: a cadaver eye model. Ophthalmic Surg. 1990;21(2):123–125. [PubMed] [Google Scholar]
- 13.Bartels MC, van Rooij J, Geerards AJ, Mulder PG, Remeijer L. Comparison of complication rates and postoperative astigmatism between nylon and mersilene sutures for corneal transplants in patients with Fuchs endothelial dystrophy. Cornea. 2006;25(5):533–539. doi: 10.1097/01.ico.0000214218.60249.e5. [DOI] [PubMed] [Google Scholar]
- 14.Landau D, Siganos CS, Mechoulam H, Solomon A, Frucht-Pery J. Astigmatism after mersilene and nylon suture use for penetrating keratoplasty. Cornea. 2006;25(6):691–694. doi: 10.1097/01.ico.0000208821.32614.49. [DOI] [PubMed] [Google Scholar]
- 15.Hammond CJ, Chan WY, Liu CS. Scanning electron microscopic study of monofilament suture knots. Br J Ophthalmol. 1996;80:164–167. doi: 10.1136/bjo.80.2.164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Barba KR, Samy A, Lai C, Perlman JI, Bouchard CS. Effect of topical anti-inflammatory drugs on corneal and limbal wound healing. J Cataract Refract Surg. 2000;26(6):893–897. doi: 10.1016/s0886-3350(00)00364-3. [DOI] [PubMed] [Google Scholar]
- 17.McCarey BE, Napalkov JA, Pippen PA, Koester JM, al Reaves T. Corneal wound healing strength with topical antiinflammatory drugs. Cornea. 1995;14(3):290–294. doi: 10.1097/00003226-199505000-00010. [DOI] [PubMed] [Google Scholar]
- 18.Randleman JB, Stulting RD. Prevention and treatment of corneal graft rejection: current practice patterns (2004) Cornea. 2006;25(3):286–290. doi: 10.1097/01.ico.0000178731.42187.46. [DOI] [PubMed] [Google Scholar]
- 19.Abou-Jaoude E, Brooks M, Katz D, Van Meter W. Spontaneous wound dehiscence after removal of single continuous penetrating keratoplasty suture. Ophthalmology. 2002;109(7):1291–1296. doi: 10.1016/s0161-6420(02)01078-3. discussion 1297. [DOI] [PubMed] [Google Scholar]
- 20.Lam FC, Rahman MQ, Ramaesh K. Traumatic wound dehiscence after penetrating keratoplasty – a cause for concern. Eye. 2007;21(9):1146–1150. doi: 10.1038/sj.eye.6702407. [DOI] [PubMed] [Google Scholar]
- 21.Wright TM, Afshari NA. Microbial keratitis following corneal transplantation. Am J Ophthalmol. 2006;142(6):1061–1062. doi: 10.1016/j.ajo.2006.06.051. [DOI] [PubMed] [Google Scholar]