Abstract
Objective To evaluate the risk of postoperative bleeding and reintervention with the use of systemic steroids in patients undergoing tonsillectomy.
Design Systematic review and meta-analysis of randomised controlled trials.
Data sources Medline, Embase, Cochrane Library, Scopus, Web of Science, Intute, Biosis, OpenSIGLE, National Technical Information Service, and Google Scholar were searched. References from reviews identified in the search and from included studies were scanned.
Review methods Randomised controlled trials comparing the administration of systemic steroids during tonsillectomy with any other comparator were eligible. Primary outcome was postoperative bleeding. Secondary outcomes were the rate of admission for a bleeding episode, reintervention for a bleeding episode, blood transfusion, and mortality.
Results Of 1387 citations identified, 29 randomised controlled trials (n=2674) met all eligibility criteria. Seven studies presented a low risk of bias, but none was specifically designed to systematically identify postoperative bleeding. Administration of systemic steroids did not significantly increase the incidence of post-tonsillectomy bleeding (29 studies, n=2674 patients, odds ratio 0.96 (95% confidence interval 0.66 to 1.40), I²=0%). We observed a significant increase in the incidence of operative reinterventions for bleeding episodes in patients who received systemic steroids (12, n=1178, 2.27 (1.03 to 4.99), I²=0%). No deaths were reported. Sensitivity analyses were consistent with the findings.
Conclusions Although systemic steroids do not appear to increase bleeding events after tonsillectomy, their use is associated with a raised incidence of operative reinterventions for bleeding episodes, which may be related to increased severity of bleeding events. Systemic steroids should be used with caution, and the risks and benefits weighed, for the prevention of postoperative nausea and vomiting after tonsillectomy before further research is performed to clarify their condition of use.
Introduction
Tonsillectomy with or without adenoidectomy is one of the most commonly performed ear, nose, and throat surgeries worldwide.1 2 After this intervention, many patients have nausea, vomiting, and pain.3 4 Without prophylaxis, the reported incidence of postoperative vomiting in children undergoing tonsillectomy ranges from 40% to 73%.5 6 7 8 Systemic steroids have been shown to be as efficient as 5-HT3 antagonists and droperidol in reducing postoperative nausea and vomiting.8 Their use is increasing and currently recommended in recent guidelines of the American Academy of Otolaryngology-Head and Neck Surgery Foundation for tonsillectomy in children.9 10 Furthermore, some studies suggest that steroids could be associated with an earlier return to a regular diet after tonsillectomy.2 11
A recent randomised controlled trial comparing different doses of dexamethasone for preventing postoperative nausea and vomiting after tonsillectomy showed an increased incidence of postoperative bleeding and reoperation due to bleeding in the steroid group.12 Previous observational studies have also reported this association.13 14 A recent meta-analysis on dexamethasone and tonsillectomy bleeding found no increased risk of postoperative bleeding with the use of steroids.15 However, this review was not exhaustive and did not evaluate clinically significant outcomes such as operative reinterventions.
Considering the frequent use and potential harm of systemic steroids to prevent postoperative nausea and vomiting after tonsillectomy, and the existence of effective alternatives such as 5-HT3 antagonists,10 we conducted a systematic review of randomised controlled trials to evaluate the risk of postoperative bleeding and of operative reinterventions after systemic steroids use in patients undergoing tonsillectomy.
Methods
Design and search strategy
We conducted a systematic review and meta-analysis of randomised controlled trials. A search strategy was developed for Medline (OVID, 1950-March 2011), Embase (OVID, 1947-March 2011), and the Cochrane Central Register of Controlled Trials (up to March 2011) (web appendix). We identified randomised controlled trials by incorporating validated filters for Medline16 and Embase.17 We also did a similar search of Scopus, the Web of Science, and Intute databases, as well as OpenSIGLE, Google Scholar, and the National Technical Information Service databases for the grey literature. Relevant abstracts and conference proceedings were identified using the Biosis database. References of pertinent reviews identified in the search were scanned to identify potentially relevant trials. Two reviewers (JP, LV) independently screened all studies for eligibility by titles and abstracts, and by full text publications if needed. A third reviewer (AFT) was consulted in instances when consensus could not be reached between the two reviewers. At the end of this selection process, Google Scholar was used to identify authors that cited any of the included studies. Additional studies identified by this method were then considered for eligibility.
Study eligibility
All randomised controlled trials of tonsillectomy (any indications) that compared the administration of any systemic steroids to any comparator (other intervention, placebo, or no intervention) were included, provided that bleeding or the absence of bleeding episodes (of any severity) were also reported or could be obtained from authors. We excluded studies including patients with bleeding disorders, patients on chronic steroid therapy, or patients in whom steroids were locally injected or sprayed on the tonsillar bed. Eligibility was not restricted by language, type of publication (for example, abstracts or full publications), or patients’ age.
The primary outcome was the incidence of postoperative bleeding from the tonsillar fossa (any type of bleeding and of any severity). The secondary outcomes were the incidence of admission for bleeding episodes, operative reinterventions for bleeding episodes, red blood cells transfusion, and mortality. We defined an operative reintervention for a bleeding episode as any surgical procedure performed in the operating room or in the emergency department to stop bleeding from the surgical site. Patients requiring a reintervention in the operating room were considered being admitted to hospital after the procedure, and were included in the meta-analysis of admissions for bleeding episodes.
Data abstraction
We developed a data abstraction form to standardise the data collection process, which was pilot tested on a landmark publication.12 For comparison purposes, all steroid doses were converted in dexamethasone equivalents. We converted fixed doses to mg/kg using the mean weight, when the data were provided. If weight was not provided, we used a standard weight of 60 kg for women and 70 kg for men in adults, and weight charts for children to estimate whether the mean dose was lower or greater than 0.5 mg/kg. Bleeding events that occurred on postoperative day zero, or within the first 24 hours, were considered as primary bleeding episodes. Episodes beyond that period of time were defined as secondary bleeding episodes. We contacted the corresponding authors of included studies if data were missing for bleeding episodes, admission, reintervention, red blood cells transfusion, or mortality, or if the methods required clarification. Two reviewers (JP, LV) performed the data collection process independently, and a third reviewer (AFT) resolved any discrepancies. A translator was consulted for studies published in languages other than English or French.
Risk of bias assessment
The risk of bias was assessed independently by two reviewers (JP, LV) using the Cochrane Collaboration’s risk of bias tool.16 Since the objective of the current review was to identify bleeding complications occurring in the acute and subacute perioperative period, studies with considerable numbers of patients lost to follow-up, as well as those with a short follow-up period (<24 h) were considered to have an increased risk of bias because of their potential for missed bleeding events.16 For this reason, we assigned an “unclear” overall risk of bias to studies with a proportion of lost to follow-up greater than 10% (incomplete outcome data).
Data synthesis
Data were analysed using Cochrane Review Manager version 5.0 (Cochrane Collaboration) and summarised using Peto fixed effects models, appropriate for meta-analysis of rare events.18 We applied a continuity correction of 0.5 to studies reporting no event in both groups. All data were dichotomous, and associations were presented using odds ratio with 95% confidence intervals. An odds ratio greater than 1 implies greater risk in the steroid group, and an odds ratio less than 1 implies greater risk in the control group. We assessed the presence of heterogeneity using the I² statistic, which estimates the percentage of variation between study results that is due to heterogeneity rather than sampling error.19 We did sensitivity analyses, based on clinical (adults v children, cold or combined v hot dissection, high [>0.5 mg/kg] v low [≤0.5 mg/kg] dose steroids, non-steroidal anti-inflammatory drug administration, type of comparator, and timing of bleeding) and methodological (risk of bias, blinding, sample size, and short [≤24 h] v long [>24 h] follow-up) characteristics, to understand potential sources of heterogeneity and to evaluate the robustness of the results. Potential publication bias was assessed using funnel plot analyses.20
Quality of evidence
We graded the quality of evidence for the three main outcomes using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach 21 with GRADEpro software (version 3.2 for Windows. Jan Brozek, Andrew Oxman, Holger Schünemann, 2008).
Results
Search results
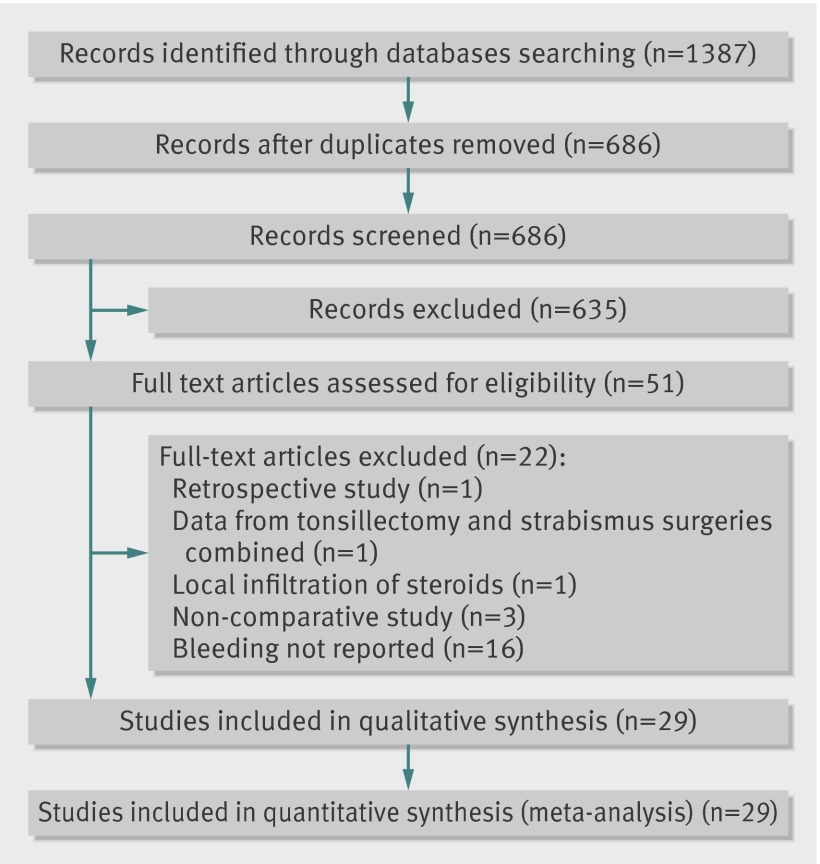
We retrieved a total of 1387 citations (fig 1). Fifty one studies were considered potentially eligible. Of these studies, 16 were excluded because they did not report bleeding episodes nor admission or reintervention, and this information could not be obtained despite attempts to contact the authors. The remaining excluded publications did not meet all inclusion criteria.22 23 24 25 26 27 We included 29 studies in this systematic review,12 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 representing 2674 patients (table 1).
Fig 1 Flow diagram of studies
Table 1.
Characteristics of included studies in meta-analysis
| Study (reference) | No of participants | Age inclusion criteria (years) | Procedure | Dissection technique | Drug regimen | NSAID use | Duration of follow-up | Bleeding outcome definition | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Steroids | Control | Steroids | Control | |||||||
| Catlin et al. (1991)32 | 10 | 15 | 4 to 12 | T, or T and A | Combined | Dexamethasone IV, 8 mg/m², before induction | Placebo | No | 3 weeks | NR |
| Volk et al. (1993)55 | 25 | 25 | 4 to 12 | T, or T and A | Combined | Dexamethasone IV, 10 mg, at induction | Placebo | No | 7 to 10 days | NR |
| Ohlms et al. (1995)47 | 34 | 35 | 3 to 18 | T, or T and A | Cold, combined | Dexamethasone IV, 0.5 mg/kg (max 12 mg), immediately before surgery | Placebo | No | 3 to 4 weeks | NR |
| April et al. (1996)30 | 41 | 39 | 3 to 15 | T and A | Hot | Dexamethasone IV, 1 mg/kg (max 16 mg), after induction | Placebo | NR | 24 h | NR |
| Tom et al. (1996)53 | 26 | 32 | 1 to 18 | T and A | Hot | Dexamethasone IV, 1 mg/kg (max 10 mg), after induction | Placebo | No | 10 days | NR |
| Kim et al. (1998)39 | 40 | 20 | 3 to 15 | T, or T and A | Combined | Dexamethasone IV, 1 mg/kg (max 15 mg), after induction or in the postanaesthetic care unit | No treatment or placebo | Yes | 3 days | NR |
| Carr et al. (1999)31 | 15 | 14 | Adults | T | Hot | Dexamethasone IV, 20 mg, during surgery | Placebo | No | 10 days | NR |
| Holt et al. (2000)36 | 68 | 60 | 2 to 14 | T, or T and A | Cold | Tropisetron and dexamethasone IV, 0.5 mg/kg (max 8 mg), after induction | Tropisetron alone, 0.1 mg/kg (max 2 mg) |
NR | 6 days | NR |
| Nawasreh et al. (2000)46 | 62 | 58 | 4 to 14 | T, or T and A | Hot | Dexamethasone IV, 1 mg/kg (max 16 mg), 1 h before surgery | Placebo | NR | 24 h | NR |
| Palme et al. (2000)48 | 25 | 25 | ≥5 | T, or T and A | Hot, combined | Prednisolone given orally, 10 mg daily (age 5-11 years) or 0.5 mg/kg daily (age ≥12 years), postoperative day 1 to 7 | Placebo | No | 2 weeks | NR |
| Giannoni et al. (2002)33 | 25 | 25 | 3 to 15 | T | Hot | Dexamethasone IV, 1 mg/kg (max 16 mg), after induction | Placebo | Yes | 10 days | NR |
| Güne et al. (2002)34 | 15 | 45 | 3 to 12 | T | NR | Dexamethasone IV, 0.15 mg/kg, after induction | 3 groups: placebo, ondansetron, 0.15 mg/kg, or droperidol, 0.075 mg/kg | NR | 6 h | NR |
| Stewart et al. (2002)52 | 132 | 68 | ≥16 | T | Hot | Dexamethasone alone or dexamethasone and piroxicam (same dose as controls); dexamethasone IV, 8 mg at induction, 2 mg on the night of surgery, 2 mg twice daily for 4 days, 2 mg daily for 4 days | Piroxicam alone, given orally: 10 mg given 2 h before surgery, 10 mg given on the night of surgery; 10 mg given twice daily for 4 days; 10 mg given daily for 4 days |
Yes | 2 weeks | NR |
| Hanasono et al. (2004)35 | 106 | 113 | ≤12 | T, or T and A | Hot, combined | Dexamethasone IV, 1 mg/kg (max 50 mg), at the start of surgery | Placebo | NR | 3 days | NR |
| Samarkandi et al. (2004)51 | 29 | 31 | 2 to 12 | T | Hot | Dexamethasone IV, 0.5 mg/kg, after induction | Placebo | NR | 24 h | NR |
| Malde et al. (2005)41 | 45 | 45 | >3 | T | Cold | Dexamethasone IV, 0.15 mg/kg, after induction | Placebo | NR | 7 days | NR |
| Trujillo et al. (2005)54 | 35 | 34 | 3 to 15 | T, or T and A | NR | Dexamethasone IV; 1 mg/kg (max 8 mg); immediately before surgery, 8 h after operation, 16 h after operation | Placebo | NR | 6 days | NR |
| Kaan et al. (2006)37 | 32 | 30 | 4 to 12 | T, or T and A | Cold | Dexamethasone IV, 0.5 mg/kg (max 16 mg), after induction | Placebo | NR | 8 h | NR |
| Kaufmann et al. (2006)38 | 101 | 103 | 2 to 16 | T and A | NR | Dexamethasone IV, 0.5 mg/kg (max 10 mg), during surgery | No treatment or placebo | NR | 10 days | NR |
| McKean et al. (2006)43 | 37 | 35 | 16 to 70 | T | Combined | Dexamethasone IV, 10 mg, at induction | Placebo | Yes | 7 days | NR |
| Mohammad et al. (2006)45 | 25 | 25 | 3 to 18 | T, or T and A | Cold, combined | Dexamethasone IV, 1 mg/kg (max 12 mg), during surgery | Unclear (placebo or no drug) |
Yes (steroid group 20%, controls 52%) | 24 h | NR |
| Alajmi et al. (2008)28 | 42 | 38 | 5 to 18 | T, or T and A | Cold, combined | Dexamethasone IV, 1 mg/kg (max 16 mg), after induction | Placebo | Yes (steroid group 14.3%, controls 47.4%) | 16 days | NR |
| Czarnetzki et al. (2008)12 | 161 | 54 | 2 to 17 | T, or T and A | Cold, hot, combined | 3 groups: dexamethasone IV, 0.05 mg/kg, 0.15 mg/kg, 0.5 mg/kg (max 20 mg); after induction | Placebo | Yes (steroid subgroups 38%, 43%, and 38%; controls 65%) | 10 days | History of bleeding leading to readmission, with or without evidence of bleeding at examination or need for emergency reoperation |
| Lachance et al. (2008)40 | 41 | 61 | 18 to 45 | T | Combined, 2 cold dissections in control group | Dexamethasone IV (8 mg during surgery), dexamethasone given orally (8 mg at home on day of surgery; 6, 4, and 2 mg twice daily on postoperative days 1, 2, and 3, respectively) | Placebo | No | 7 days | NR |
| Rujirojindakul et al. (2008)50 | 25 | 25 | 15 to 60 | T | Hot | Dexamethasone IV, 20 mg, after induction | Placebo | No | 7 days | NR |
| Ammar et al. (2009)29 | 30 | 30 | Adults and children | T, or T and A | Cold | Dexamethasone IV, 5 mg to children, 10 mg to adults, for 4 days after surgery | Placebo | Yes | 5 days | NR |
| Mohamed et al. (2009)44 | 100 | 50 | 2 to 12 | T, or T and A | Hot | 2 groups: dexamethasone alone or dexamethasone and glossopharyngeal nerve block (same dose as controls); dexamethasone IV, 0.15mg/kg (max 8 mg), before surgery | Bilateral glossopharyngeal nerve block alone with 3 mL of 0.5% bupivacaine | No | Until discharge time (up to 24 h) | NR |
| Rabbani et al. (2010)49 | 30 | 30 | Adults and children | T, or T and A | NR | Dexamethasone IV, 0.1 mg/kg for age <12 years or 8 mg for >12 years, at induction | Ondansetron, 0.1 mg/kg for age <12 years, 4 mg for age >12 years | NR | 24 h | NR |
| Mathiesen et al. (2011)42 | 48 | 99 | 18 to 50 | T | Combined | Dexamethasone IV, 8 mg, with paracetamol and pregabalin (same dose as controls) before induction | 2 groups: paracetamol alone, 1000 mg, or paracetamol and pregabalin, 300 mg | No | 2 weeks | Bleeding episodes requiring reoperation |
A=adenoidectomy; cold=dissection with cold steel instruments, haemostasis with gauze compression, or ligatures; combined=cold dissection with use of electrocautery for haemostasis; hot=dissection and haemostasis with electric device; IV=intravenous; max=maximum; NR=not reported; NSAID=non-steroidal anti-inflammatory drug; T=tonsillectomy.
Study characteristics
Of the included studies, 24 were published in English, and one each in Turkish,34 Korean,39 Spanish,54 Chinese,29 and Hebrew.38 Ten studies were conducted in North America,30 31 32 33 35 40 47 53 54 55 12 in Asia,28 29 34 37 38 39 41 45 46 49 50 51 four in Europe,12 42 43 52 two in Australia,36 48 and one in Africa.44 All studies were presented as full publications. In two studies, dexamethasone was provided by pharmaceutical companies,12 32 and one of these studies specified that the funding organisation had no role in the design or conduct of the study.12
Nineteen studies were performed in children, six in adults only, and four included both children and adults. Twenty four studies compared the effects of systemic steroids with placebo12 28 29 30 31 32 33 34 35 37 40 41 43 46 47 48 50 51 53 54 55 or no intervention (neither a placebo nor any intervention in the control group).38 39 45 Six studies compared systemic steroids with other treatments (tropisetron, ondansetron, droperidol, piroxicam, bilateral glossopharyngeal nerve block with bupivacaine, or paracetamol).
Dexamethasone was used in 28 studies, while prednisolone was administered in the remaining study.48 In 18 studies, the dexamethasone dose was calculated according to the patient’s weight (mg/kg) and varied from 0.05 mg/kg 12 to 1.0 mg/kg. In the remaining studies, the steroid dose was fixed29 31 40 42 43 50 52 55; based on the patient’s body surface (mg/m²)32; or either fixed or based on weight (mg/kg), according to patient’s age.48 49 Systemic steroids were administrated as a single dose, or repeated doses over a specific period of time: 16 h,54 three days,40 four days,29 seven days,48 or eight days.52 In these studies, the total dose was taken into account.
In most studies, the main outcomes were the effect of steroids on pain,12 28 29 30 31 32 33 35 37 38 39 40 41 42 43 44 45 47 48 50 51 52 53 54 55 nausea and vomiting,12 28 30 33 34 35 36 37 38 39 41 43 45 46 47 48 49 50 51 52 53 and oral intake 12 28 30 32 35 37 38 39 41 43 45 46 47 48 50 51 53 55 after tonsillectomy. Other main outcome measures of included studies were the effect of steroids on oedema, fever, trismus, halitosis, and level of activity.
Twenty six studies reported data for post-tonsillectomy bleeding. Through private communications with authors, we obtained details pertaining to the severity of and to interventions related to the bleeding episodes for three of these studies,40 42 53 and obtained unpublished data on bleeding episodes for three additional studies.43 44 49 Eight studies reported no postoperative bleeding episodes or mentioned uneventful surgeries.29 37 43 44 48 49 51 54 Among studies reporting bleeding episodes, 18 specified the timing of occurrence,12 28 30 31 32 33 34 35 36 39 41 42 45 46 47 50 52 53 nine reported the need for admission due to bleeding,12 28 30 31 35 46 47 50 53 and 12 reported data for reintervention.12 30 32 34 39 40 42 46 47 50 52 55 No study reported transfusion of red blood cells or mortality.
A clear definition of post-tonsillectomy bleeding was presented in two of 29 studies.12 42 Eight studies stated that bleeding episodes were going to be reported,12 28 31 32 33 35 37 41 while six clearly questioned their patients about postoperative bleeding or provided instructions in the event of unexpected bleeding.12 28 35 37 41 42 No study described a systematic method to evaluate postoperative bleeding.
Validity assessment
A low risk of bias was attributed to seven studies 33 35 36 40 41 42 50 (table 2). Fifteen studies had an adequate sequence generation,12 30 31 33 35 36 37 40 41 42 43 50 51 52 54 and 15 had an appropriate method of allocation concealment.12 30 33 35 36 40 41 42 43 47 48 50 52 53 55 Six studies were not blinded,28 38 39 45 46 49 and blinding was unclear in another study.34 One study was terminated early because of an increased incidence of post-tonsillectomy bleeding in the intervention group.12 Fourteen studies 12 31 32 33 36 38 40 41 42 43 47 52 53 55 reported losses to follow-up that varied from 2.7%12 to 36.1%,43 and losses to follow-up were unclear in four studies.29 39 45 48 Eight studies had a follow-up period of 24 h or less.30 34 37 44 45 46 49 51 Two studies reported performing an intention to treat analysis.12 40 Five studies did not report all outcomes stated in their methods.32 45 46 51 54
Table 2.
Risk of bias and methodological quality assessment of included studies
| Study (reference) | Sequence generation | Allocation concealment | Blinding | Incomplete outcome data | Selective reporting | Other bias | Follow-up period (>24 h) | Summary |
|---|---|---|---|---|---|---|---|---|
| Catlin et al. (1991)32 | Unclear | Unclear | Low | High | Unclear | Unclear | Low | Unclear |
| Volk et al. (1993)55 | Unclear | Low | Low | High | Low | High | Low | Unclear |
| Ohlms et al. (1995)47 | Unclear | Low | Low | High | Low | Low | Low | Unclear |
| April et al. (1996)30 | Low | Low | Low | Low | Low | Low | High | High |
| Tom et al. (1996)53 | Unclear | Low | Low | High | Low | Unclear | Low | Unclear |
| Kim et al. (1998)39 | Unclear | High | High | Unclear | Low | High | Low | High |
| Carr et al. (1999)31 | Low | Unclear | Low | High | Low | Low | Low | Unclear |
| Holt et al. (2000)36 | Low | Low | Low | Low | Low | Low | Low | Low |
| Nawasreh et al. (2000)46 | Unclear | High | High | Low | High | Unclear | High | High |
| Palme et al. (2000)48 | Unclear | Low | Low | Unclear | Low | Unclear | Low | Unclear |
| Giannoni et al. (2002)33 | Low | Low | Low | Low | Low | Low | Low | Low |
| Güne et al. (2002)34 | Unclear | High | Unclear | Low | Low | Unclear | High | High |
| Stewart et al. (2002)52 | Low | Low | Low | High | Low | Low | Low | Unclear |
| Hanasono et al. (2004)35 | Low | Low | Low | Low | Low | Low | Low | Low |
| Samarkandi et al. (2004)51 | Low | Unclear | Low | Low | Unclear | Low | High | High |
| Malde et al. (2005)41 | Low | Low | Low | Low | Low | Low | Low | Low |
| Trujillo et al. (2005)54 | Low | Unclear | Low | Low | Unclear | Low | Low | Unclear |
| Kaan et al. (2006)37 | Low | Unclear | Low | Low | Low | Low | High | High |
| Kaufmann et al. (2006)38 | Unclear | High | High | High | Low | High | Low | High |
| McKean et al. (2006)43 | Low | Low | Low | High | Low | Low | Low | Unclear |
| Mohammad et al. (2006)45 | Unclear | Unclear | High | Unclear | Unclear | High | Unclear | High |
| Alajmi et al. (2008)28 | High | High | High | Low | Low | High | Low | High |
| Czarnetzki et al. (2008)12 | Low | Low | Low | Low | Low | High | Low | Unclear |
| Lachance et al. (2008)40 | Low | Low | Low | Low | Low | Low | Low | Low |
| Rujirojindakul et al. (2008)50 | Low | Low | Low | Low | Low | Low | Low | Low |
| Ammar et al. (2009)29 | Unclear | Unclear | Low | Unclear | Low | Low | Low | Unclear |
| Mohamed et al. (2009)44 | Unclear | High | Low | Low | Low | Low | High | High |
| Rabbani et al. (2010)49 | High | High | High | Low | Unclear | High | High | High |
| Mathiesen et al. (2011)42 | Low | Low | Low | Low | Low | Low | Low | Low |
Post-tonsillectomy bleeding episodes
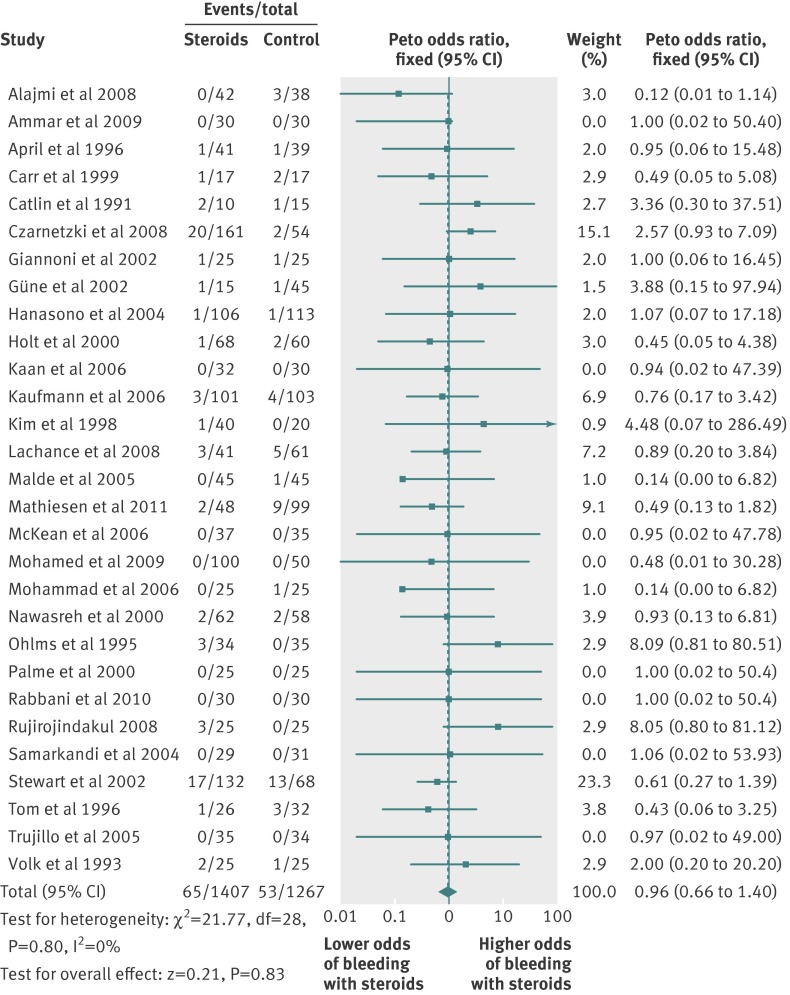
The administration of steroids did not increase the incidence of bleeding events after tonsillectomy, based on pooled data from the 29 studies (n=2674, odds ratio 0.96, 95% confidence intervals 0.66 to 1.40, I²=0%), of which eight did not observe any bleeding episodes29 37 43 44 48 49 51 54 (fig 2). Sensitivity analyses including trials with low risk of bias, observers blinded to the intervention, larger population, or longer follow-up periods yielded similar results (table 3). Results were also comparable regardless of the population age, surgical technique, steroid dose, or concomitant administration of non-steroidal anti-inflammatory drugs. When we analysed primary and secondary bleeding events separately, we observed no increase in bleeding incident with the administration of steroids.
Fig 2 Post-tonsillectomy bleeding. For Peto odds ratio, continuity correction k=0.5 was used when there was no event in both groups
Table 3.
Sensitivity analysis of post-tonsillectomy bleeding outcome
| Subgroups | No of studies | No of participants | Odds ratio (95% CI) | I2 (%) |
|---|---|---|---|---|
| Methodological quality | ||||
| Low risk of bias | 7 | 786 | 0.82 (0.38 to 1.74) | 0 |
| High risk of bias | 11 | 986 | 0.71 (0.31 to 1.61) | 0 |
| Blinding | ||||
| Double blinded | 22 | 2040 | 1.04 (0.68 to 1. 56) | 0 |
| No blinding or unclear | 7 | 634 | 0.67 (0.27 to 1.70) | 0 |
| Sample size | ||||
| <100 patients | 20 | 1189 | 1.15 (0.60 to 2.42) | 0 |
| ≥100 patients | 9 | 1485 | 0.88 (0.55 to 1.40) | 0 |
| Duration of follow-up | ||||
| ≤24 h | 8 | 642 | 0.92 (0.30 to 2.82) | 0 |
| >24 h | 21 | 2032 | 0.96 (0.64 to 1.44) | 0 |
| Age group | ||||
| Children only | 19 | 1809 | 1.24 (0.74 to 2.08) | 0 |
| Adults only | 6 | 605 | 0.73 (0.41 to 1.30) | 0 |
| Surgical technique | ||||
| Cold or combine dissection | 13 | 861 | 0.82 (0.43 to 1.56) | 0 |
| Hot dissection | 9 | 592 | 0.76 (0.42 to 1.40) | 0 |
| Dose regimen of steroid | ||||
| ≤0.5 mg/kg | 19 | 1784 | 1.05 (0.68 to 1.61) | 0 |
| >0.5 mg/kg | 9 | 840 | 0.77 (0.34 to 1.74) | 0 |
| Coadministration of NSAID | ||||
| NSAID | 8 | 787 | 0.92 (0.52 to 1.62) | 26 |
| No NSAID | 20 | 1683 | 1.00 (0.60 to 1.65) | 0 |
| Type of comparator | ||||
| Placebo | 20 | 1615 | 1.32 (0.80 to 2.20) | 0 |
| Other drugs | 6 | 745 | 0.62 (0.33 to 1.16) | 0 |
| Moment of bleeding episode | ||||
| Primary bleedings | 9 | 952 | 0.93 (0.33 to 2.59) | 0 |
| Secondary bleedings | 14 | 1437 | 0.97 (0.61 to 1.56) | 18 |
Cold=dissection with cold steel instruments, haemostasis with gauze compression, or ligatures; combined=cold dissection with use of electrocautery for haemostasis; hot=dissection and haemostasis with electric device; NSAID=non-steroidal anti-inflammatory drug.
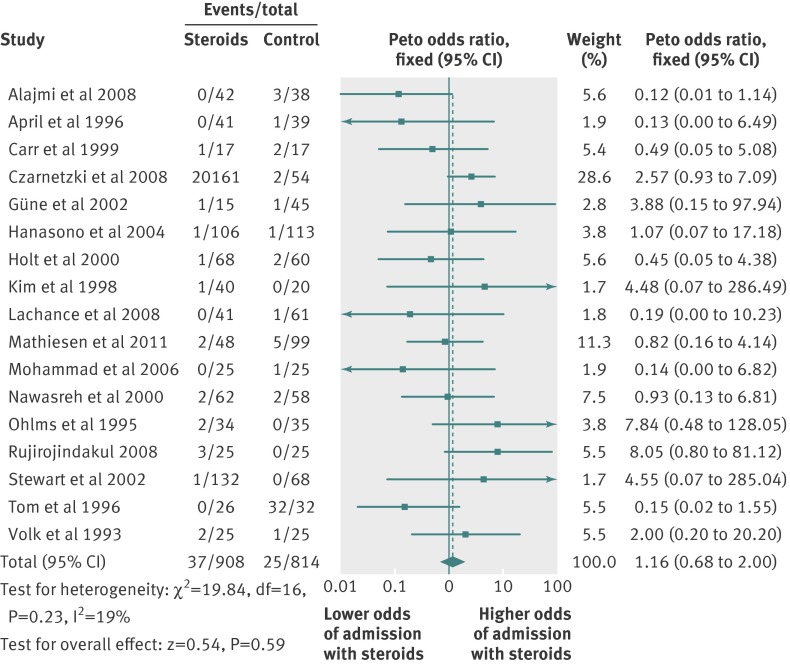
Hospital admission
Seventeen studies reported data for admission12 28 30 31 35 46 47 50 53 or reinterventions34 36 39 40 42 45 52 55 that required admission (fig 3). The incidence of admission due to a bleeding episode did not increase in the steroid group (17 studies, n=1722 patients, odds ratio 1.16, 95% confidence interval 0.68 to 2.00, I²=19%). All sensitivity analyses accorded with this finding (data not shown).
Fig 3 Admission for post-tonsillectomy bleeding
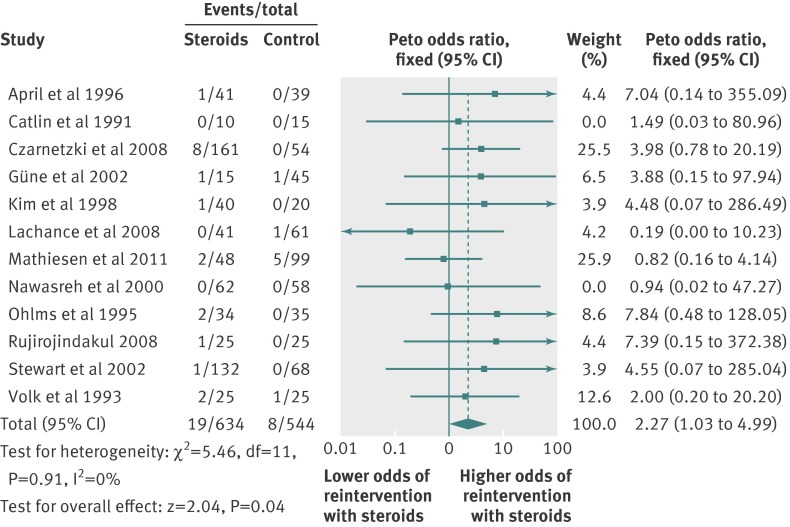
Reintervention for a bleeding episode
The incidence of operative reintervention for bleeding episodes was significantly increased in the steroid group (12 studies, n=1178; odds ratio 2.27, 95% confidence interval 1.03 to 4.99, I2=0%; fig 4). The average incidence of reintervention due to bleeding in patients receiving steroids was 3.0% versus 1.5% in controls. Sensitivity analyses were performed to evaluate the incidence of reintervention for bleeding episodes among different subgroups (table 4). We observed a significant increase of reinterventions in children (eight studies12 30 32 34 39 46 47 55; 3.43, 1.29 to 9.13, I²=0%) but not in adults (four40 42 50 52; 1.07, 0.29 to 4.03, I²=0%). A dose effect was not observed. We found an increased incidence of reinterventions among patients receiving non-steroidal anti-inflammatory drugs (three12 39 52; 4.10, 0.99 to 16.97, I²=0%). No significant association was seen among double blinded studies (nine12 30 32 40 42 47 50 52 55; 2.22, 0.95 to 5.18, I2=0%) and those with longer follow-up periods (nine12 32 39 40 42 47 50 52 55; 2.16, 0.92 to 5.06, I2=0%). In each case, the incidence of reinterventions for bleeding episodes was increased in the steroid group compared with the control group without reaching significance (P=0.07 for double blinding, P=0.08 for longer follow-up periods), although the results suggested a strong trend. Studies with low risk of bias showed no clear association between steroids use and the incidence of operative reintervention (three studies40 42 50; 0.91, 0.22 to 3.68, I²=0%).
Fig 4 Reintervention for post-tonsillectomy bleeding. For Peto odds ratio, continuity correction k=0.5 was used when there was no event in both groups
Table 4.
Sensitivity analysis of operative reintervention to treat post-tonsillectomy bleeding
| Subgroups | No of studies | No of participants | Odds ratio (95% CI) | I2 (%) |
|---|---|---|---|---|
| Methodological quality | ||||
| Low risk of bias | 3 | 299 | 0.91 (0.22 to 3.68) | 0 |
| High risk of bias | 4 | 320 | 3.31 (0.51 to 21.61) | 0 |
| Blinding | ||||
| Double blinded | 9 | 938 | 2.22 (0.95 to 5.18) | 0 |
| No blinding or unclear | 3 | 240 | 2.64 (0.31 to 22.41) | 0 |
| Sample size | ||||
| <100 patients | 7 | 394 | 3.85 (1.13 to 13.17) | 0 |
| ≥100 patients | 5 | 784 | 1.57 (0.56 to 4.38) | 0 |
| Follow-up | ||||
| ≤24 h | 3 | 260 | 3.06 (0.37 to 25.07) | 0 |
| >24 h | 9 | 918 | 2.16 (0.92 to 5.06) | 0 |
| Age group | ||||
| Children only | 8 | 679 | 3.43 (1.29 to 9.13) | 0 |
| Adults only | 4 | 499 | 1.07 (0.29 to 4.03) | 0 |
| Surgical technique | ||||
| Cold or combined dissection | 6 | 453 | 1.45 (0.50 to 4.20) | 0 |
| Hot dissection | 4 | 450 | 3.84 (0.53 to 28.00) | 0 |
| Dosage regimen of steroid | ||||
| ≤0.5 mg/kg | 8 | 816 | 2.45 (1.04 to 5.76) | 0 |
| >0.5 mg/kg | 4 | 362 | 1.52 (0.21 to 11.20) | 0 |
| Coadministration of NSAID | ||||
| NSAID | 3 | 475 | 4.10 (0.99 to 16.97) | 0 |
| No NSAID | 9 | 703 | 1.75 (0.68 to 4.50) | 0 |
Cold=dissection with cold steel instruments, haemostasis with gauze compression, or ligatures; combined=cold dissection with use of electrocautery for haemostasis; hot=dissection and haemostasis with electric device; NSAID=non-steroidal anti-inflammatory drug.
Allogenic transfusion and mortality
None of the included studies reported transfusion of red blood cells or mortality.
Publication bias and quality of evidence
We evaluated the presence of potential publication bias using a funnel plot of intervention effect estimates versus the standard error for studies presenting data for bleeding episodes. Visual inspection of the funnel plot did not reveal evidence of publication bias (web figure). According to the GRADE methodology, the quality of the evidence for bleeding and admission outcomes after tonsillectomy was low; however, the association between post-tonsillectomy reintervention and systemic steroids was considered to be of high quality (table 5).
Table 5.
Summary of evidence for key outcomes
| Outcome | No of participants/studies | Quality of evidence (GRADE) | Summary | |
|---|---|---|---|---|
| Relative effect, odds ratio (95% CI) | Study events rates (steroid/control groups (%)) | |||
| Post-tonsillectomy bleeding episodes | 2674/29 | Very low | 0.96 (0.66 to 1.40) | 4.6/4.2 |
| Admission | 1722/17 | Very low | 1.16 (0.68 to 2.00) | 4.1/3.1 |
| Reintervention | 1178/12 | High | 2.27 (1.03 to 4.99) | 3.0/1.5 |
Discussion
In this systematic review, we did not observe an increased incidence of postoperative bleeding events after perioperative administration of systemic steroids in patients undergoing tonsillectomy. However, we did observe a significant increase in the incidence of operative reinterventions needed to manage clinically significant bleeding episodes in patients who received systemic steroids. The quality of the evidence according to the GRADE approach was high for this specific outcome. This raised incidence of reinterventions was significantly increased in children.
Strengths and limitations if the study
An important limitation of our study concerned the data available within included publications. None of the included studies was designed to evaluate adverse complications of steroids use after tonsillectomy, and no study systematically screened for bleeding events after tonsillectomy. Therefore, the incidence of this complication could have been systematically underestimated. Moreover, only two studies presented a clear definition of post-tonsillectomy bleeding. Bleeding episodes of varying severity may not have received equal consideration across all studies, which could lead to an underestimation of overall bleeding episodes. This could explain why we did not observe a significant association between steroids use and bleeding events, while we did observe an association with reintervention for bleeding events.
On the other hand, the inclusion in meta-analyses of studies reporting no bleeding event in either group using a continuity correction could have underestimated the association. The majority of included studies were of limited methodological quality, and many studies had substantial numbers of patients who were lost to follow-up. These factors provide further concern that bleeding episodes may have been missed. A significant proportion of studies had a very limited follow-up period precluding the evaluation of the incidence of secondary bleeding episodes. Since bleeding episodes are relatively rare events, unreported episodes could greatly affect the study results.
Despite of known limitations, our systematic review had important strengths. Firstly, the extensive search strategy using different databases, including the grey literature and conference proceedings, allowed us to retrieve a comprehensive list of the studies performed on the topic. Importantly, the decision to evaluate the incidence of reinterventions for bleeding episodes, as opposed to only bleeding episodes, allowed us to summarise the effect of clinically significant bleeding events with greater fidelity. We believe that operative reintervention for bleeding episodes represents a more reliable and clinically meaningful endpoint than bleeding episodes. Severe enough bleeding events to require operative reintervention are less likely to have been overlooked and may therefore represent the optimal clinical outcome to understand the impact of systemic steroids in tonsillectomy.
Comparison with other studies
Overall, the mean incidence of post-tonsillectomy bleeding events observed in our systematic review was 4.4%, which is consistent with the current literature.56 57 58 59 60 Our results on postoperative bleeding are in accordance with a recent systematic review.15 However, this previous meta-analysis identified half the number of studies as compared with our study, and did not evaluate other clinically significant outcomes such as operative reinterventions for bleeding and hospital admission. The increased incidence of reintervention observed in a recent landmark study by Czarnetzki and colleagues12 was also seen in our pooled analysis. But our systematic review did not confirm the higher incidence of bleeding episodes associated with perioperative steroids use in tonsillectomy procedures, as observed in this trial.
The increased incidence of reinterventions associated with steroids occurred in the absence of increased bleeding events, and thus probably represents an increased severity of bleeding when steroids are administered. Although no study specified indications to undergo a reintervention in the event of bleeding, this procedure usually suggests that the bleeding was significant enough to require an emergency procedure. Bleeding events requiring reintervention are more likely to be noticed and reported in a publication as opposed to minor events. Therefore, reinterventions to manage bleeding events may be a more objective and reliable outcome to assess clinically significant bleeding events after tonsillectomy.
Conclusions and policy implications
We did not observe an increased incidence of postoperative bleeding events following administration of systemic steroids during tonsillectomy. We did, however, observe a significant increase in the incidence of operative reintervention associated with the use of steroids, which may be related to an increased severity of a given bleeding episode. Considering the potential for harm and the availability of other drugs to prevent postoperative nausea and vomiting, we recommend that steroids should be used with caution; risks and benefits must be weighted; and steroids should not be used routinely for such purposes, especially in children. Further studies should be designed to answer concerns about the safety of the perioperative use of steroids in tonsillectomy procedures.
What is already known on this topic
Tonsillectomy is one of the most commonly performed ear, nose, and throat surgeries worldwide, but has a high underlying risk of postoperative nausea and vomiting
Systemic use of steroids to reduce postoperative nausea and vomiting is increasing, and recommended in addition to the use of 5-HT3 antagonists in recent guidelines
A recent study has linked such use of steroids with an increased incidence of postoperative bleeding after tonsillectomy
What this study adds
Overall, the risk of postoperative bleeding did not increase after perioperative administration of systemic steroids in patients undergoing tonsillectomy
However, the incidence of reinterventions for bleeding episodes did increase overall with steroids, and especially among children, which could represent a greater severity of bleeding associated with use of steroids
Systemic steroids should be used with caution; risks and benefits must be weighted, and steroids should not be used routinely to prevent postoperative nausea and vomiting after tonsillectomy, especially in children
We thank Lucie Côté from the Library of the Centre Hospitalier Affilié Universitaire de Québec, Enfant-Jésus Hospital, for her help with the retrieval of study publications.
Contributors: JP, AFT, RZ, FL, LM, and DAF contributed to the conception and design of the study. JP and LV determined eligibility of search results and extracted data from included studies. JP, AB, and AFT performed and reviewed the analyses, and drafted the manuscript. All authors participated in the interpretation of the data and the critical review of the manuscript, and approved the version to be published. AFT is the guarantor.
Funding: This study was funded by personal funds. AFT and FL are recipients of a research career award from the Fonds de Recherche Québec-Santé. AFT and FL are supported by the Traumatology Research Consortium of the Fonds de Recherche Québec-Santé. LM and DAF are recipients of New Investigator Awards from the Canadian Institutes for Health Research. RZ is a recipient of a randomised controlled trials mentorship award from the Canadian Institutes for Health Research.
Competing interests: All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: no support from any organisation for the submitted work; no financial relationships with any organisations that might have an interest in the submitted work in the previous three years; no other relationships or activities that could appear to have influenced the submitted work.
Ethical approval: This study did not require ethical approval.
Data sharing: No additional data available.
Cite this as: BMJ 2012;345:e5389
Web Extra. Extra material supplied by the author
Web appendix: Medline search strategy
Web figure: Funnel plot of post-tonsillectomy bleeding
References
- 1.Bolton CM, Myles PS, Nolan T, Sterne JA. Prophylaxis of postoperative vomiting in children undergoing tonsillectomy: a systematic review and meta-analysis. Br J Anaesth 2006;97:593-604. [DOI] [PubMed] [Google Scholar]
- 2.Steward DL, Grisel J, Meinzen-Derr J. Steroids for improving recovery following tonsillectomy in children. Cochrane Database Syst Rev 2011:CD003997. [DOI] [PMC free article] [PubMed]
- 3.Randall DA, Hoffer ME. Complications of tonsillectomy and adenoidectomy. Otolaryngol Head Neck Surg 1998;118:61-8. [DOI] [PubMed] [Google Scholar]
- 4.Johnson LB, Elluru RG, Myer CM 3rd. Complications of adenotonsillectomy. Laryngoscope 2002;112:35-6. [DOI] [PubMed] [Google Scholar]
- 5.Litman RS, Wu CL, Catanzaro FA. Ondansetron decreases emesis after tonsillectomy in children. Anesth Analg 1994;78:478-81. [DOI] [PubMed] [Google Scholar]
- 6.Furst SR, Rodarte A. Prophylactic antiemetic treatment with ondansetron in children undergoing tonsillectomy. Anesthesiology 1994;81:799-803. [DOI] [PubMed] [Google Scholar]
- 7.Ferrari LR, Donlon JV. Metoclopramide reduces the incidence of vomiting after tonsillectomy in children. Anesth Analg 1992;75:351-4. [DOI] [PubMed] [Google Scholar]
- 8.Apfel CC, Korttila K, Abdalla M, Kerger H, Turan A, Vedder I, et al. A factorial trial of six interventions for the prevention of postoperative nausea and vomiting. N Engl J Med 2004;350:2441-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baugh RF, Archer SM, Mitchell RB, Rosenfeld RM, Amin R, Burns JJ, et al. Clinical Practice Guideline. Otolaryngol Head Neck Surg 2011;144:S1-30. [DOI] [PubMed] [Google Scholar]
- 10.Gan TJ, Meyer TA, Apfel CC, Chung F, Davis PJ, Habib AS, et al. Society for Ambulatory Anesthesia guidelines for the management of postoperative nausea and vomiting. Anesth Analg 2007;105:1615-28. [DOI] [PubMed] [Google Scholar]
- 11.Goldman AC, Govindaraj S, Rosenfeld RM. A meta-analysis of dexamethasone use with tonsillectomy. Otolaryngol Head Neck Surg 2000;123:682-6. [DOI] [PubMed] [Google Scholar]
- 12.Czarnetzki C, Elia N, Lysakowski C, Dumont L, Landis BN, Giger R, et al. Dexamethasone and risk of nausea and vomiting and postoperative bleeding after tonsillectomy in children: a randomized trial. JAMA 2008;300:2621-30. [DOI] [PubMed] [Google Scholar]
- 13.Collison PJ, Mettler B. Factors associated with post-tonsillectomy hemorrhage. Ear Nose Throat J 2000;79:640-2. [PubMed] [Google Scholar]
- 14.Macassey EA, Baguley C, Dawes P, Gray A. 15-year audit of post-tonsillectomy haemorrhage at Dunedin Hospital. ANZ J Surg 2007;77:579-82. [DOI] [PubMed] [Google Scholar]
- 15.Geva A, Brigger MT. Dexamethasone and Tonsillectomy Bleeding. Otolaryngol Head Neck Surg 2011;144:838-43. [DOI] [PubMed] [Google Scholar]
- 16.Higgins JPT, Green S, eds. Cochrane handbook for systematic reviews of interventions, version 5.1.0. Cochrane Collaboration, 2011. www.cochrane-handbook.org.
- 17.Wong SS, Wilczynski NL, Haynes RB. Developing optimal search strategies for detecting clinically sound treatment studies in EMBASE. J Med Libr Assoc 2006;94:41-7. [PMC free article] [PubMed] [Google Scholar]
- 18.Yusuf S PR, Lewis J, Collins R, Sleight P Beta blockade during and after myocardial infarction: an overview of the randomized trials. Prog Cardiovasc Dis 1985;27:335-71. [DOI] [PubMed] [Google Scholar]
- 19.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ioannidis JP, Trikalinos TA. The appropriateness of asymmetry tests for publication bias in meta-analyses: a large survey. CMAJ 2007;176:1091-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Atkins D, Best D, Briss PA, Eccles M, Falck-Ytter Y, Flottorp S, et al. Grading quality of evidence and strength of recommendations. BMJ 2004;328:1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fujii Y, Tanaka H, Toyooka H. Granisetron and dexamethasone provide more improved prevention of postoperative emesis than granisetron alone in children. Can J Anaesth 1996;43:1229-32. [DOI] [PubMed] [Google Scholar]
- 23.Gunter JB, McAuliffe JJ, Beckman EC, Wittkugel EP, Spaeth JP, Varughese AM. A factorial study of ondansetron, metoclopramide, and dexamethasone for emesis prophylaxis after adenotonsillectomy in children. Paediatr Anaesth 2006;16:1153-65. [DOI] [PubMed] [Google Scholar]
- 24.Liechti M, Feurer R, Gross D, Schmitz A, Stutz K, Gerber A, et al. Prevention of postoperative nausea and vomiting in children following adenotonsillectomy, using tropisetron with or without low-dose dexamethasone. J Anesth 2007;21:311-6. [DOI] [PubMed] [Google Scholar]
- 25.McAuliffe JJ, Gunter JB, Beckman EC. Dose-response relationship of dexamethasone and recovery after tonsillectomy in children [abstract 1228]. American Society of Anesthesiologists Annual Meeting; 2001 October. New Orleans, Anesthesiology, 2001.
- 26.McAuliffe JJ, Gunter JB, Beckman EC. A factorial study of ondansetron, metoclopramide, and dexamethasone for the prevention of emesis after tonsillectomy in children: model development [abstract 1225]. American Society of Anesthesiologists Annual Meeting; 2001 October. New Orleans, Anesthesiology, 2001.
- 27.Inci N, Basut O, Kasapoglu F, Coskun H. Management of pain after tonsillectomy: a prospective, randomized clinical study. Kulak Burun Bogaz Ihtis Derg 2009;19:1-8. [PubMed] [Google Scholar]
- 28.Alajmi MA, Al Noumas HS, Al-Abdulhadi KA, Kavitha G. Steroids for reducing post-tonsillectomy morbidity. Kuwait Med J 2008;40:211-5. [Google Scholar]
- 29.Ammar G, Wang Z. Effect of dexamethasone on post tonsillectomy pain. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 2009;23:936-8. [PubMed] [Google Scholar]
- 30.April MM, Callan ND, Nowak DM, Hausdorff MA. The effect of intravenous dexamethasone in pediatric adenotonsillectomy. Arch Otolaryngol Head Neck Surg 1996;122:117-20. [DOI] [PubMed] [Google Scholar]
- 31.Carr MM, Williams JG, Carmichael L, Nasser JG. Effect of steroids on posttonsillectomy pain in adults. Arch Otolaryngol Head Neck Surg 1999;125:1361-4. [DOI] [PubMed] [Google Scholar]
- 32.Catlin FI, Grimes WJ. The effect of steroid therapy on recovery from tonsillectomy in children. Arch Otolaryngol Head Neck Surg 1991;117:649-52. [DOI] [PubMed] [Google Scholar]
- 33.Giannoni C, White S, Enneking FK. Does dexamethasone with preemptive analgesia improve pediatric tonsillectomy pain? Otolaryngol Head Neck Surg 2002;126:307-15. [DOI] [PubMed] [Google Scholar]
- 34.Güne Y, Ünlügenç H, Gündüz M, Tuncer Ü, Akman H. [Comparison of the effects of ondansetron, dexamethasone and droperidol on the nausea and vomiting after tonsillectomy in children]. Çukurova Üniv T p Fak Derg 2002;27:13-9. [Google Scholar]
- 35.Hanasono MM, Lalakea ML, Mikulec AA, Shepard KG, Wellis V, Messner AH. Perioperative steroids in tonsillectomy using electrocautery and sharp dissection techniques. Arch Otolaryngol Head Neck Surg 2004;130:917-21. [DOI] [PubMed] [Google Scholar]
- 36.Holt R, Rask P, Coulthard KP, Sinclair M, Roberts G, Van Der Walt J, et al. Tropisetron plus dexamethasone is more effective than tropisetron alone for the prevention of postoperative nausea and vomiting in children undergoing tonsillectomy. Paediatr Anaesth 2000;10:181-8. [DOI] [PubMed] [Google Scholar]
- 37.Kaan MN, Odabasi O, Gezer E, Daldal A. The effect of preoperative dexamethasone on early oral intake, vomiting and pain after tonsillectomy. Int J Pediatr Otorhinolaryngol 2006;70:73-9. [DOI] [PubMed] [Google Scholar]
- 38.Kaufmann M, Deutsch E, Hamouri H. The effect of steroid therapy on post adenotonsillectomy recovery. Harefuah 2006;145:577-80. [PubMed] [Google Scholar]
- 39.Kim M, Lee J, Lee S, Baik S, Chang B. The Effect of Dexamethasone in Tonsillectomy. Korean J Otolaryngol Head Neck Surg 1998;41:783-7. [Google Scholar]
- 40.Lachance M, Lacroix Y, Audet N, Savard P, Thuot F. The use of dexamethasone to reduce pain after tonsillectomy in adults: a double-blind prospective randomized trial. Laryngoscope 2008;118:232-6. [DOI] [PubMed] [Google Scholar]
- 41.Malde A, Sonawane V, Jagtap S. Effect of dexamethasone on post tonsillectomy morbidities. Indian J Anaesth 2005;49:202-7. [Google Scholar]
- 42.Mathiesen O, Jorgensen DG, Hilsted KL, Trolle W, Stjernholm P, Christiansen H, et al. Pregabalin and dexamethasone improves post-operative pain treatment after tonsillectomy. Acta Anaesthesiol Scand 2011;55:297-305. [DOI] [PubMed] [Google Scholar]
- 43.McKean S, Kochilas X, Kelleher R, Dockery M. Use of intravenous steroids at induction of anaesthesia for adult tonsillectomy to reduce post-operative nausea and vomiting and pain: a double-blind randomized controlled trial. Clin Otolaryngol 2006;31:36-40. [DOI] [PubMed] [Google Scholar]
- 44.Mohamed SK, Ibraheem AS, Abdelraheem MG. Preoperative intravenous dexamethasone combined with glossopharyngeal nerve block: role in pediatric postoperative analgesia following tonsillectomy. Eur Arch Otorhinolaryngol 2009;266:1815-9. [DOI] [PubMed] [Google Scholar]
- 45.Mohammad L, Ahmad R, Latoo M, Qazl S, Wanl A. Post-tonsilelectomy morbidity—do steroids help. Indian J Otolaryngol Head Neck Surg 2006;58:141-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Nawasreh O, Fraihat A, Maaita J. The effect of preoperative intravenous dexamethasone in pediatric adenotonsillectomy. J Bahrain Med Soc 2000;12:130-3. [Google Scholar]
- 47.Ohlms LA, Wilder RT, Weston B. Use of intraoperative corticosteroids in pediatric tonsillectomy. Arch Otolaryngol Head Neck Surg 1995;121:737-42. [DOI] [PubMed] [Google Scholar]
- 48.Palme CE, Tomasevic P, Pohl DV. Evaluating the effects of oral prednisolone on recovery after tonsillectomy: a prospective, double-blind, randomized trial. Laryngoscope 2000;110:2000-4. [DOI] [PubMed] [Google Scholar]
- 49.Rabbani MZ, Khan MNA, Qureshi R, Zubair M, Bin Pervez M. Does the added benefit of Ondansetron over Dexamethasone, to control post-operative nausea and vomiting, justify the added cost in patients undergoing tonsillectomy and adenotonsillectomy? J Pak Med Assoc 2010;60:559-61. [PubMed] [Google Scholar]
- 50.Rujirojindakul P, Atchariyasathian V, Uakrìtdathikran T, Boonyata N, Boonthida Saefung B. Effect of dexamethasone on postoperative pain after adult tonsillectomy. Thai J Anesthesiol 2008;34:1-8. [Google Scholar]
- 51.Samarkandi AH, Shaikh MA, Ahmad RA, Alammar AY. Use of dexamethasone to reduce postoperative vomiting and pain after pediatric tonsillectomy procedures. Saudi Med J 2004;25:1636-9. [PubMed] [Google Scholar]
- 52.Stewart R, Bill R, Ullah R, McConaghy P, Hall SJ. Dexamethasone reduces pain after tonsillectomy in adults. Clin Otolaryngol Allied Sci 2002;27:321-6. [DOI] [PubMed] [Google Scholar]
- 53.Tom LWC, Templeton JJ, Thompson ME, Marsh RR. Dexamethasone in adenotonsillectomy. Int J Pediatr Otorhinolaryngol 1996;37:115-20. [DOI] [PubMed] [Google Scholar]
- 54.Trujillo M, Ramírez J, Fuentes S. Efecto de la administración de dexametasona intravenosa en pacientes pediátricos post operados de amigdalectomía com o sin adenoidectomía. An ORL Méx 2005;50:61-4. [Google Scholar]
- 55.Volk MS, Martin P, Brodsky L, Stanievich JF, Ballou M. The effects of preoperative steroids on tonsillectomy patients. Otolaryngol Head Neck Surg 1993;109:726-30. [DOI] [PubMed] [Google Scholar]
- 56.O’Leary S, Vorrath J. Postoperative bleeding after diathermy and dissection tonsillectomy. Laryngoscope 2005;115:591-4. [DOI] [PubMed] [Google Scholar]
- 57.Lee M, Montague M, Hussain S. Post-tonsillectomy hemorrhage: cold versus hot dissection. Otolaryngol Head Neck Surg 2004;131:833-6. [DOI] [PubMed] [Google Scholar]
- 58.British Association of Otorhinolaryngologists—Head and Neck Surgeons Comparative Audit Group and the Clinical Effectiveness Unit of the Royal College of Surgeons of England. National prospective tonsillectomy audit. Royal College of Surgeons of England, 2005.
- 59.Raut V, Bhat N, Kinsella J, Toner J, Sinnathuray A, Stevenson M. Bipolar scissors versus cold dissection tonsillectomy: a prospective, randomized, multi-unit study. Laryngoscope 2001;111:2178-82. [DOI] [PubMed] [Google Scholar]
- 60.Windfuhr JP, Chen YS. Incidence of post-tonsillectomy hemorrhage in children and adults: a study of 4,848 patients. Ear Nose Throat J 2002;81:626-8. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix: Medline search strategy
Web figure: Funnel plot of post-tonsillectomy bleeding