Abstract
Tumors in the cervical portion of the esophagus have traditionally been more difficult to manage. The implantation in the cervical esophagus is a technically demanding procedure. The implantation of modified self-expandable metal stents (SEMSs) was very effective perorally under endoscopic and fluoroscopic guidance. Experience with SEMS has revealed an increased risk of migration when either covered stents are used or a stent is implanted across the gastroesophageal junction. The modified, covered, esophageal stents appear to prevent stent migration and improve dysphagia in patients with malignant tumor stenosis at the esophagogastric junction. Besides heartburn, regurgitation is sometimes very distressing to patients and may lead to fatal aspiration due to reflux after stenting in esophagogastric junction. These symptoms can be reduced by the use of valved stent. The long S-shape valve is very effective in preventing acid reflux and valve inversion.
Keywords: Antimigration stent, Antireflux stent, Cervical esophageal stent
INTRODUCTION
Endoscopic endoprosthesis has been well established as a fast and durable procedure for palliation of malignant dysphagia. An ideal esophageal endoprosthesis should have the following characteristics: an optimal internal diameter, flexible and non-traumatic but sufficient radial force, a compact and easy-to-use delivery system, ability to reposition or remove if necessary, and long-term patency without ingrowth or migration.1 Currently, stent selection should be individualized on the basis of operator preference and experience, proximal or distal tumor location, presence of fistulas, degree of tumor shelf, and whether obstruction is intrinsic or extrinsic.
ESOPHAGEAL STENTING FOR CERVICAL ESOPHAGUS
Tumors in the cervical portion of the esophagus (7% to 10% of all esophageal cancer) have traditionally been more difficult to manage. Palliative resection, radiotherapy, and laser therapy are frequently associated with local treatment failure. The use of esophageal stents in this area was considered to be relatively contraindicated because of concerns about an increased risk of perforation, pulmonary aspiration, migration of the prosthesis into hypopharynx, and perhaps most importantly, an intolerable foreign body sensation.
Today, there is no doubt that the self-expandable metal stent (SEMS) is a well-established palliative treatment for stenotic malignant disease of esophagus. However, their implantation in the cervical esophagus is a technically demanding procedure and only a few successful cases are reported in the literature. Macdonald et al.2 reported 22 patients treated for malignant stricture of cervical esophagus using SEMS. They reported 93% of technical success but 28% of patient reported foreign body sensation.
We modified the SEMS for cervical esophageal cancer stenting. In order to decrease the foreign body sensation and to prevent migration of the stent, we reduced the length of its proximal funnel to 7 mm with fully expanded diameter of 18 mm (Fig. 1). We had experience in six patients with inoperable cervical esophageal stricture by implantation of modified SEMS inserted perorally under endoscopic and fluoroscopic guidance (Fig. 2). The placement of the stent was successful in all patients. Five of six patients had no serious complications such as perforation, pulmonary aspiration, stent migration, and foreign body sensation (Table 1).3
Fig. 1.
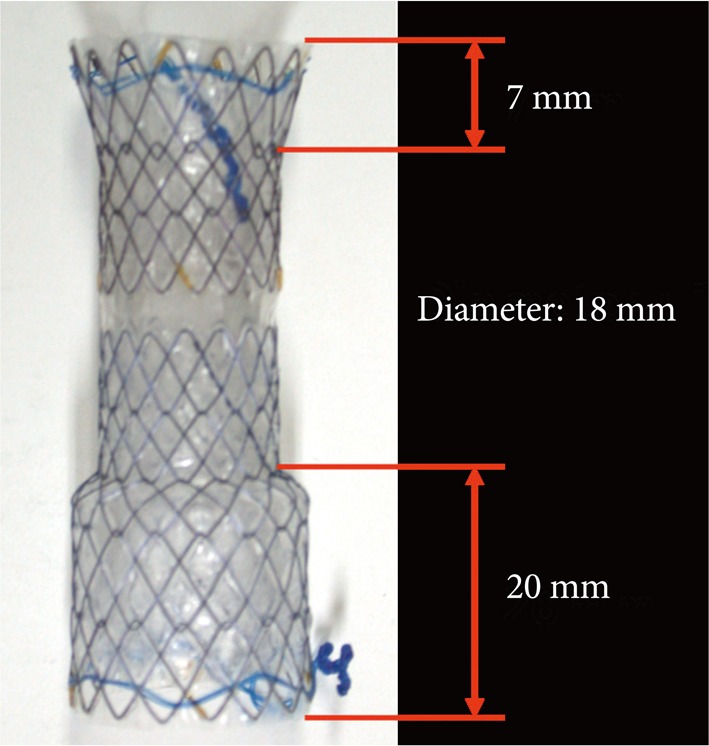
Self-expandable metal stents for the cervical esophagus. In order to decrease the foreign body sensation, we reduced the length of its proximal funnel to 7 mm, the fully expanded diameter being 18 mm.
Fig. 2.
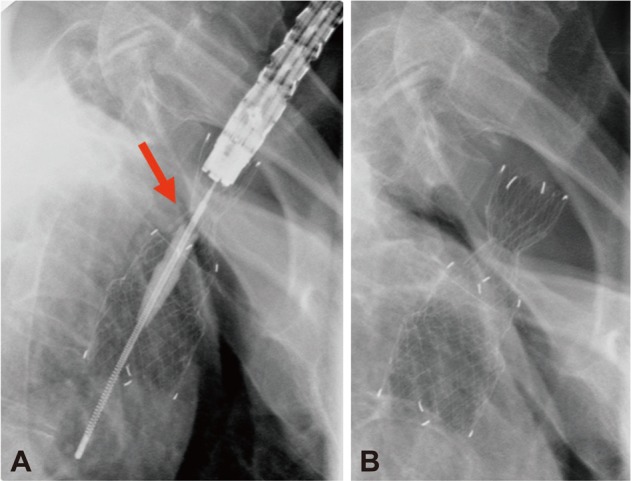
(A) The lesion was located 16 cm from the incisors, 1 cm below the upper esophageal sphincter. (B) Post-stenting radiograph, showing well positioned cervical stent.
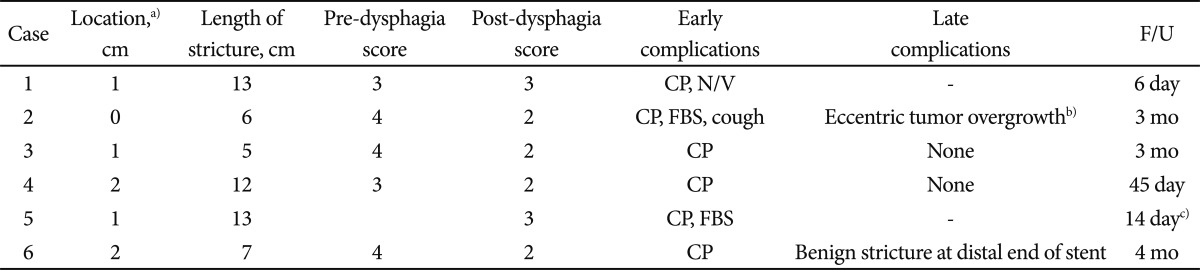
Table 1.
Results of Newly Designed Self-Expandable Metal Stents for Cervical Esophageal Stricture
Modified from Shim et al. Endoscopy 2004;36:554-557.3
F/U, follow-up; CP, chest pain; N/V, nausea/vomiting; FBS, foreign body sensation-mild and disappear severe days later.
a)Distance from upper esophageal sphincter; b)But didn't aggravate the dysphagia; c)Stent removed d/t severe chest pain.
ESOPHAGEAL STENTING FOR ESOPHAGOGASTRIC (GE) JUNCTION
Anti-migration stent
Experience with SEMS has revealed an increased risk of migration when either covered stents are used or a stent is implanted across the gastroesophageal junction. Data from several studies evaluating various types of SEMS indicated that the overall migration rate ranges from 2% to 8%, but the migration rate with membrane covered metal stents was higher, presumably due to reduced friction between the membrane and the esophageal wall. The migration rate with these stents ranges from 10% to 35% in reported series.4 Recently, various types of new stents and several methods to prevent stent migration have been tried.
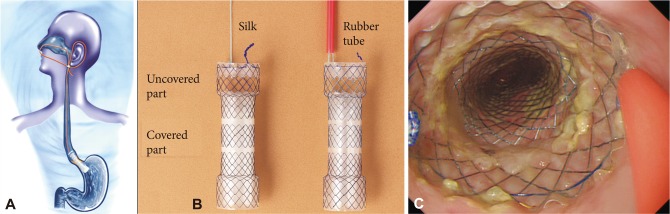
To prevent the migration of the stent, we made a modified, covered, self-expandable esophageal metal stent that could be fixated by using a silk thread attached on the edge of proximal end of the stent to the patient's ear via the nares (Fig. 3).
Fig. 3.
Shim's technique for antimigration. (A) A 14-Fr rubber tube covering the silk is connected to patient's earlobe until the proximal part of the stent becomes completely fixed to the esophageal mucosa. (B) The uncovered proximal flange will be firmly fixed to the esophageal mucosa, and prevents the stent migration. (C) Endoscopic image just after implantation of antimigration stent.
In our study, no stent migration occurred during the mean follow-up period of 7.5 months (range, 1 to 17) among 61 patients.5 This result is very remarkable and an important point in our study. We think that this modified stent effectively prevented the distal migration.5 In conclusion, modified, covered, esophageal stents appear to prevent stent migration and improve dysphagia in patients with malignant tumor stenosis at the GE junction, a short segment of tumor stricture less than 5 cm in length, a soft tumor stenosis, and a tracheoesophageal fistula.
There was another esophageal stent designed for the prevention of migration by Taewoong Medical, Seoul, Korea. The Niti-S stent consists of an inner polyurethane layer to prevent tumor ingrowth and an outer uncovered nitinol wire tube to allow the mesh of the stent to embed itself in the esophageal wall (Fig. 4).
Fig. 4.
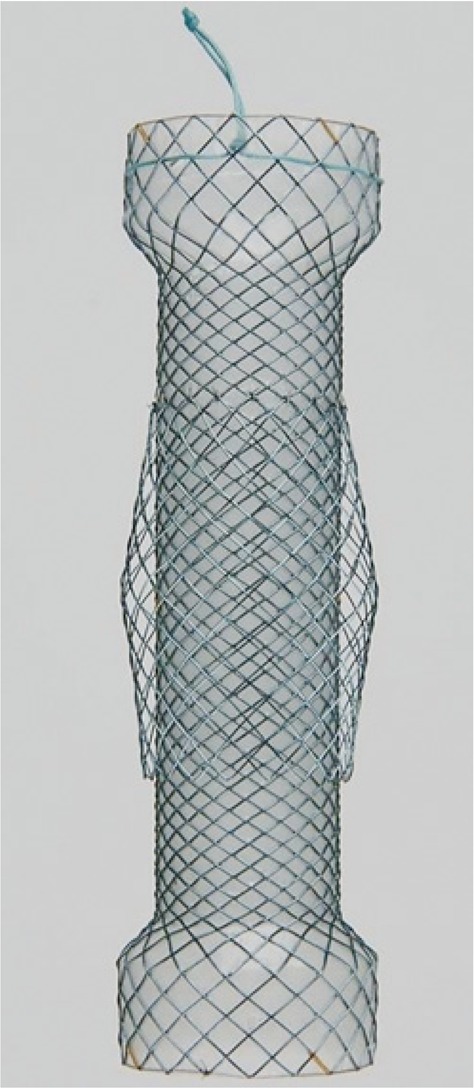
Niti-S stent with a double-layer configuration, consisting of an inner polyurethane layer and an outer uncovered Nitinol wire.
Its double-layered design is probably important in preventing migration. However the prevention of stent migration was note complete. The stent migration was 7% (3 of 42 patients).6
Anti-reflux stent
Are the antireflux stents necessary for stenting in gastroesophageal junction? The main criticism was that reflux was rare and could be readily treated by proton pump inhibitors. Also there was no effort to detect symptomatic reflux and underreport of reflux after stenting in GE junction. Besides heartburn, regurgitation is sometimes very distressing to patients and may lead to fatal aspiration. These symptoms can be reduced by the use of valved stent. There were a few attempts to develop antireflux stent.
Dua et al.7 designed the modified self expanding metal esophageal Z-stents to prevent reflux. It was modified by extending the polyurethane coating beyond the lower metal cage so as to form a "windsock"-type valve.
Dua stent was effective in preventing reflux without interfering with ante-grade flow. However it has some limitations such as difficult placement of stent and inversion of antireflux valve under high pressure gradients (e.g., belching, vomiting, and coughing). The FerX-Ella antireflux stent failed to prevent GE reflux due to obstruction by inverted membrane and migration at 7 of 30 cases.8
We evaluated the usefulness of previous antireflux esophageal stent (Dostent; M.I. Tech., Seoul, Korea). It is a fully covered esophageal stent with a tricuspid antireflux valve in a larger distal band. Most patients were relieved of the reflux symptoms, but some of them had an evidence of acid reflux on 24 hours pH monitoring and a reversed or broken valve upon endoscopic examination. So we designed the new model. The modified antireflux stent (Shim's Hanarostent; M.I. Tech.) is a fully covered esophageal stent that has a S-type antireflux valve with long leaflet inside the stent's body, and we fixed the antireflux valve at stent wall in order to minimize acid reflux and to prevent inversion of the valve (Fig. 5). We compared it with conventional SEMSs and Dostent in terms of reflux symptom, dysphagia score and ambulatory 24 hours pH monitoring. The dysphagia score improved significantly with all stents. After ambulatory 24 hours pH monitoring, the newly designed S-type antireflux valve, among the three stents, was found to the best for preventing acid reflux. These modifications do not appear to interfere with the primary function of the stent, that is, relieving dysphagia. From our little experience with the new antireflux valve stents, we believe the long S-shape valve is most effective in preventing acid reflux and valve inversion (Table 2).9
Fig. 5.
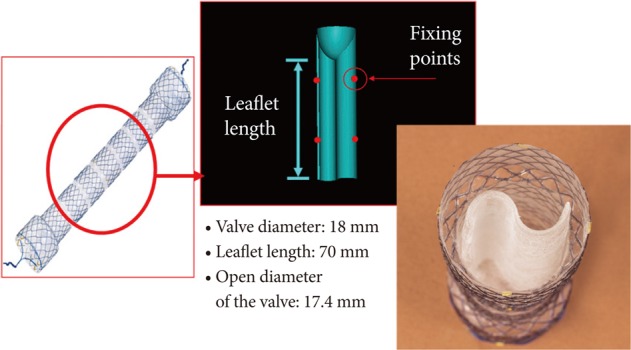
Esophageal stent with S-type antireflux valve. Modified antireflux stent is a fully covered esophageal stent which has a S-type antireflux valve with long leaflet inside the stent's body and we fixed antireflux valve at stent wall in order to minimize acid reflux and to prevent inversion of the valve.
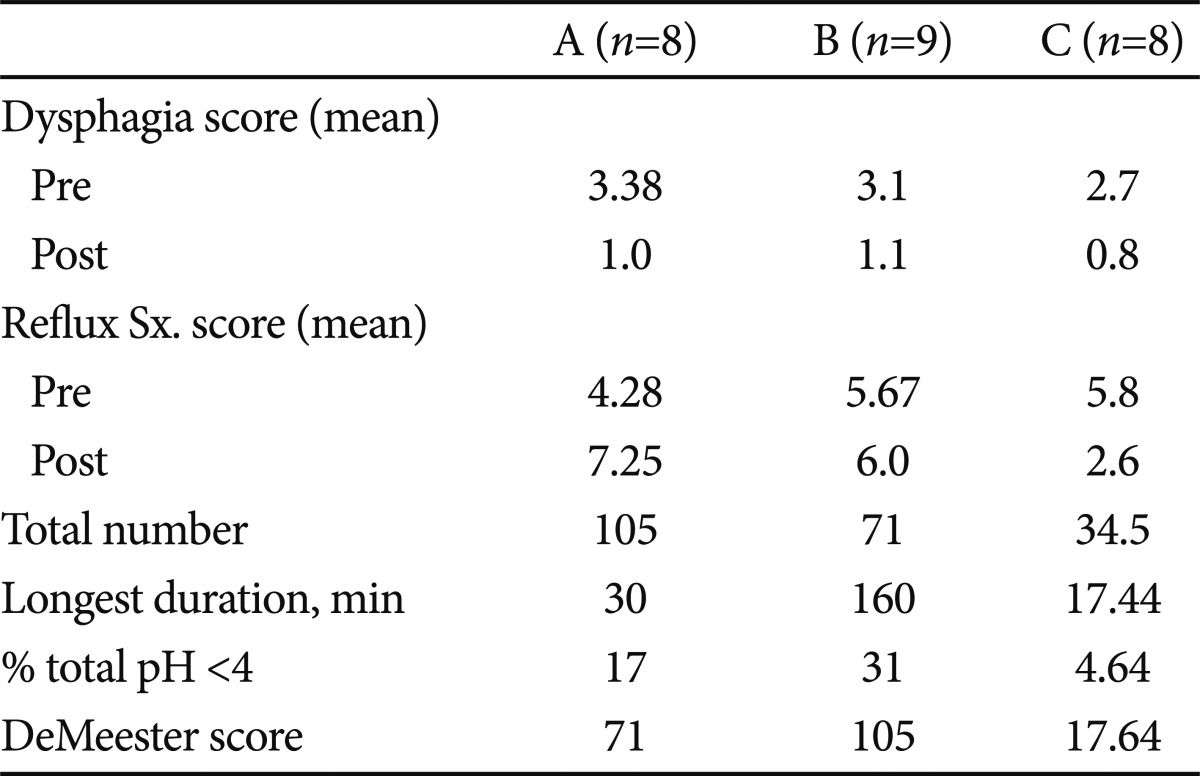
Table 2.
Comparison of S-Type Valve Antireflux Esophageal Stent with Conventional SEMS and Dostent in Dysphagia Score, Reflux Symptom Score and Ambulatory 24 Hours pH Monitoring
Modified from Shim et al. Endoscopy 2005;37:335-339.9
A, conventional self expandable stent; B, Dostent, anti-reflux esophageal stent with tricuspid type valve; C, anti-reflux esophageal stent with S-type valve.
SEMS, self-expandable matallic stent; Sx., symptom.
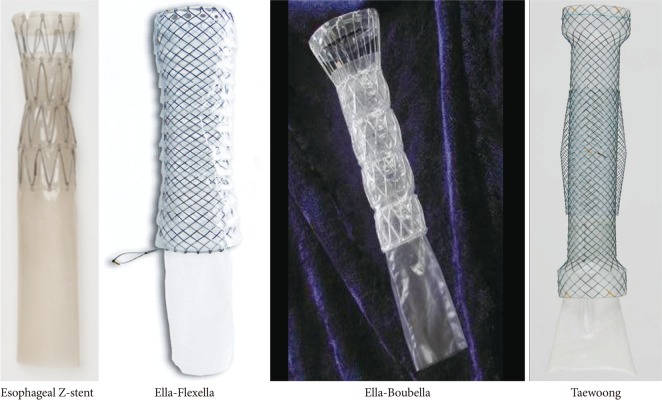
Recently a few skirt type antireflux stents have been introduced on the market (Fig. 6).
Fig. 6.
Various modified skirt type self-expanding metal esophageal antireflux stents.
CONCLUSIONS
Insertion of stents is virtually always successful, with relatively few complications and excellent palliation of patient's symptoms. It is a field of rapid technological advances, and self-expandable metallic stents have made a significant contribution to the management and palliation of symptoms in a group of patients that has traditionally been proved extremely difficult to treat.
Footnotes
The author has no financial conflicts of interest.
References
- 1.Shields SJ. Esophageal self-expandable metallic stents. Gastrointest Endosc. 1997;45:439–442. doi: 10.1016/s0016-5107(97)70163-9. [DOI] [PubMed] [Google Scholar]
- 2.Macdonald S, Edwards RD, Moss JG. Patient tolerance of cervical esophageal metallic stents. J Vasc Interv Radiol. 2000;11:891–898. doi: 10.1016/s1051-0443(07)61807-7. [DOI] [PubMed] [Google Scholar]
- 3.Shim CS, Jung IS, Bhandari S, et al. Management of malignant strictures of the cervical esophagus with a newly-designed self-expanding metal stent. Endoscopy. 2004;36:554–557. doi: 10.1055/s-2004-814555. [DOI] [PubMed] [Google Scholar]
- 4.Kozarek RA, Raltz S, Brugge WR, et al. Prospective multicenter trial of esophageal Z-stent placement for malignant dysphagia and tracheoesophageal fistula. Gastrointest Endosc. 1996;44:562–567. doi: 10.1016/s0016-5107(96)70009-3. [DOI] [PubMed] [Google Scholar]
- 5.Shim CS, Cho YD, Moon JH, et al. Fixation of a modified covered esophageal stent: its clinical usefulness for preventing stent migration. Endoscopy. 2001;33:843–848. doi: 10.1055/s-2001-17326. [DOI] [PubMed] [Google Scholar]
- 6.Verschuur EM, Homs MY, Steyerberg EW, et al. A new esophageal stent design (Niti-S stent) for the prevention of migration: a prospective study in 42 patients. Gastrointest Endosc. 2006;63:134–140. doi: 10.1016/j.gie.2005.07.051. [DOI] [PubMed] [Google Scholar]
- 7.Dua KS, Kozarek R, Kim J, et al. Self-expanding metal esophageal stent with anti-reflux mechanism. Gastrointest Endosc. 2001;53:603–613. doi: 10.1067/mge.2001.114054. [DOI] [PubMed] [Google Scholar]
- 8.Homs MY, Wahab PJ, Kuipers EJ, et al. Esophageal stents with antireflux valve for tumors of the distal esophagus and gastric cardia: a randomized trial. Gastrointest Endosc. 2004;60:695–702. doi: 10.1016/s0016-5107(04)02047-4. [DOI] [PubMed] [Google Scholar]
- 9.Shim CS, Jung IS, Cheon YK, et al. Management of malignant stricture of the esophagogastric junction with a newly designed self-expanding metal stent with an antireflux mechanism. Endoscopy. 2005;37:335–339. doi: 10.1055/s-2005-861113. [DOI] [PubMed] [Google Scholar]