Abstract
Objective
This study examined whether changes in self-efficacy explain the effects of a mailed print intervention on long-term dietary practices of breast and prostate cancer survivors. The relationship between change in self-efficacy and long-term physical activity (PA) also was examined.
Methods
Breast and prostate cancer survivors (N=543) from 39 U.S. states and two Canadian provinces participated in the FRESH START intervention trial. Participants were randomly assigned to receive a 10-month program of mailed print materials on diet and PA available in the public domain or a 10-month program of tailored materials designed to increase fruit and vegetable (F&V) intake, decrease fat intake, and/or increase PA. Changes in self-efficacy for F&V intake and fat restriction were analyzed as potential mediators of the intervention’s effects on diet at 2-year follow-up. Because we previously found that change in self-efficacy for PA did not vary by group assignment, the relationship between change in self-efficacy and PA at 2-year follow-up was examined across study conditions.
Results
Results suggest that change in self-efficacy for fat restriction partially explained the intervention’s effect on fat intake (mean indirect effect=-.28), and change in self-efficacy for F&V consumption partially explained the intervention’s effect on daily F&V intake (mean indirect effect=.11). Change in self-efficacy for fat restriction partially accounted for the intervention’s impact on overall diet quality among men only (mean indirect effect=.60). Finally, change in self-efficacy for PA predicted PA at 2-year follow-up.
Conclusions
Findings suggest that self-efficacy may influence long-term maintenance of healthy lifestyle practices among cancer survivors.
Keywords: cancer, oncology, survivors, diet, physical activity, randomized controlled trial
Progress in the early detection and treatment of cancer has resulted in rapid increases in the number of cancer survivors [1-2]. Currently, there are over 12 million cancer survivors in the United States, representing about 4% of the population [3]. The increase in cancer survivors is expected to continue due to the aging population and continued improvement in cancer screening and care [1].
Although the growth in cancer survivors is a positive trend, the negative health consequences of cancer and its treatment are a public health concern. Compared to people without a cancer history, cancer survivors have an increased risk for developing secondary malignancies and other medical conditions, such as heart disease, diabetes, osteoporosis, and functional limitations [4-8]. Factors contributing to survivors’ elevated risk for medical conditions may include genetic predisposition, effects of cancer treatment, and lifestyle factors [9].
Unhealthy lifestyle practices, including inadequate physical activity (PA) and fruit and vegetable (F&V) consumption and high fat intake, have been associated with increased risk of cardiovascular disease and other chronic health conditions [9-11]. Conversely, recent data suggest that a healthy diet may reduce cancer-related biomarkers and risk of cancer recurrence, although results have been mixed [12-17]. Unfortunately, many cancer survivors do not meet national guidelines regarding diet and PA [18-20]. Indeed, results of national surveys have revealed few differences in health behaviors between individuals diagnosed with cancer and healthy or noncancer control participants [18-20].
In an effort to improve cancer survivors’ health behaviors, over 60 diet and PA intervention trials have been conducted with this patient population [21-22]. Results of these trials suggest that PA interventions improve cardiorespiratory fitness, physical function, and quality of life, and dietary interventions result in lower body weight and increased nutrition-related biomarkers [22-27]. FRESH START was the first diet and PA trial for cancer survivors to deliver the intervention exclusively via mailed print materials [28]. The trial enrolled breast and prostate cancer survivors throughout North America. At 1-year follow-up [28], both the attention control group who received publicly available materials on diet and PA and the intervention group who received materials that were tailored to their demographic and psychological characteristics and progress toward achieving lifestyle goals showed improvement in specific health behaviors (i.e., increased PA and F&V consumption and reduced fat intake) as well as enhanced diet quality (a construct that reflects the overall dietary pattern and compares it with food patterns related to reduced risk of morbidity and mortality that involve high consumption of F&V, whole grains, low fat dairy products, and lean meats) [29-31]. The intervention group, however, showed significantly greater improvement than the control group in PA and dietary behaviors. At 2-year follow-up, the intervention group continued to report better overall diet quality and lower fat intake compared to the control group, but did not differ from controls with regard to F&V intake or PA [32].
The FRESH START intervention was informed by Social Cognitive Theory in which key determinants of health behaviors include self-efficacy (i.e., confidence that one can perform health behaviors in a variety of circumstances), knowledge of the benefits and risks of the behavior, outcome expectations, health goals, and plans for achieving these goals [33-34]. According to this theory, self-efficacy plays a critical role in health behavior initiation and maintenance by directly influencing health behavior and by affecting several other determinants [34]. People with high levels of self-efficacy are hypothesized to set realistic goals for themselves, maintain favorable outcome expectations, and persevere in the face of challenges [33-34]. The FRESH START intervention was designed to impact self-efficacy and related variables by detailing the benefits of practicing the goal behavior and incremental tasks toward the goal with an emphasis on overcoming perceived barriers and providing encouragement or praise for goal attainment [28]. At intervention completion (1 year post-baseline), change in self-efficacy was found to partially explain the effects of the FRESH START intervention on dietary outcomes [35].
Although long-term maintenance of PA and a healthy diet is critical for reducing cancer survivors’ risk of disease [9-11], psychosocial factors that influence health behavior maintenance (i.e., continuation of health behaviors at least 6-12 months post-intervention) are largely unknown, despite calls for their exploration in health promotion intervention trials [36-38]. Rothman and other theorists have noted that factors involved in initiation of health behaviors such as self-efficacy may not necessarily predict maintenance of these behaviors long-term [38-39]. Few research efforts have been made, however, to determine effects of diet and PA interventions on health behaviors over substantial time periods and psychosocial mediators of these effects. To address this gap in the literature, the present study prospectively examined the potential role of self-efficacy in long-term maintenance of dietary practices and PA. Specifically, change in self-efficacy from baseline to year 1 was examined as a potential mediator of the effects of the FRESH START intervention on breast and prostate cancer survivors’ dietary outcomes at year 2. Based on Social Cognitive Theory [33] and prior research [35, 40-42], we hypothesized that change in self-efficacy for F&V intake would partially mediate the intervention’s effect on daily servings of F&V and that change in self-efficacy for fat restriction would partially mediate the intervention’s effect on the percentage of kcal from fat. We also hypothesized that change in self-efficacy for F&V intake and fat restriction would partially mediate the intervention’s effect on diet quality. Gender and age also were examined as potential moderators of the relations between self-efficacy and dietary outcomes, as self-efficacy for eating a healthy diet has been correlated with these demographic factors [35, 43]. Change in self-efficacy for PA was not a hypothesized mediator of the intervention’s effect on total minutes of PA per week because group assignment did not predict change in self-efficacy for PA at 1-year follow-up [35]. Instead, we hypothesized that change in self-efficacy for PA from baseline to year 1 would predict PA at year 2 across study conditions.
Finally, we explored whether change in barriers to F&V intake and fat restriction from baseline to year 1 predicted dietary outcomes at year 2. We also explored whether change in barriers to PA from baseline to year 1 predicted PA at year 2. Our prior analysis indicated that group assignment was not associated with changes in barriers to F&V intake, fat restriction, and PA at 1-year follow-up [35], and, thus, changes in barriers were not analyzed as potential mediators of the intervention’s effects on study outcomes.
Method
Participants
Participants in the randomized trial had been diagnosed with early stage (in situ, localized, or regional) breast cancer (n = 306) or prostate cancer (n = 237) within the prior 9 months. Individuals were excluded from the trial if they had conditions precluding unsupervised PA (uncontrolled angina or congestive heart failure, recent myocardial infarction, breathing difficulties requiring oxygen use or hospitalization, planned hip or knee replacement surgery, or use of a walker or wheelchair) or if they had conditions precluding a high F&V diet (renal failure or chronic warfarin use). Individuals with advanced cancer or an additional primary cancer and those who could not read and write in English also were excluded.
The present research examines data from survivors (n = 489) who participated in the 2-year follow-up assessment. Participants were primarily Caucasian (85%) or African American (12%) and 59% had a college degree. The average age of participants was 57.2 years (SD = 10.7) and the average time since diagnosis was 3.9 months (SD = 2.8) at the time of study enrollment. Most participants (85%) had undergone surgery and received adjuvant treatment, including chemotherapy (26%), radiation (45%), and hormonal therapy (40%).
Procedure
Recruitment
Following approval of study procedures by the Duke University Health System Institutional Review Board, participants were recruited via cancer registries of participating medical centers, large oncology practices, or self-referral in 39 states and 2 provinces in North America. Descriptions of the sample and intervention conditions and statistical analyses of the accrual procedures have been published [28, 44-46]. To summarize, significant differences were found between respondents and nonrespondents with respect to gender (54% vs. 46% female, respectively), race (19% vs. 38% minority, respectively), and age (58 vs. 62 years, respectively).
Potential participants (n = 678) underwent eligibility screening within 9 months of diagnosis. Survivors who were eligible and provided written informed consent began the intervention following receipt of primary cancer treatment. Survivors were not eligible for the intervention trial if they practiced two or more goal behaviors (exercising 150+ minutes per week, eating 5 or more daily servings of F&V, limiting total and saturated fat intakes to less than 30% and 10% of kcal, respectively).
Experimental and control conditions
Participants (n = 543) were randomized to receive one of two 10-month mailed print interventions focused on improving diet and PA. No differences were found between study arms (FRESH START intervention vs. attention control) with respect to gender, race, age, education, type and clinical stage of cancer, and cancer-related treatment. The interventions involved an initial workbook followed by a series of seven newsletters at 6-week intervals (the final newsletter was issued about two months after the 1-year assessment). Between mailings, participants in both study arms received brief surveys and a $5 incentive for each returned survey. The surveys for the control arm assessed the perceived helpfulness of the brochures, whereas the surveys for the experimental arm assessed current diet and PA and readiness to change these behaviors. This information was used to individually tailor each newsletter and provide continually updated feedback to experimental participants. Specifically, newsletters were tailored to the experimental participants’ demographic characteristics (age, race, and sex) [28], cancer coping style [47], stage of readiness, barriers to health behavior change, and progress toward goal behaviors (150+ minutes of PA, adherence to a low fat or high F&V diet) [44]. To enhance observational learning of lifestyle practices, newsletters included a survivor’s testimonial tailored on race (i.e., African American vs. other), age (i.e., <60 vs. ≥60 years old), and cancer coping style (e.g., “fighting spirit,” “fatalist,” “cognitive avoider,” “helpless-hopeless,” or “anxious preoccupier”) based on the modified version of the Mini-Mental Adjustment to Cancer subscale administered at baseline [47]. Newsletters also provided strategies for lifestyle change tailored to the participant’s reported barriers to healthy eating or PA (e.g., costs, time constraints). Each newsletter also included a graph indicating the participant’s progress toward the goal behavior and tailored messages of encouragement or praise regarding goal achievement. Finally, newsletters were tailored to the participant’s stage of readiness [i.e., precontemplation (not thinking about change), contemplation (thinking about change), and preparation/action (beginning to take or taking active steps toward change)] as a means of increasing engagement [48]. Non-tailored sections of the newsletter focused on the health benefits of lifestyle change. Experimental participants received two 5-month mailings on PA, F&V consumption, or dietary fat restriction and only received materials on goal behaviors that they did not meet. Participants who did not adhere to any goal behaviors at baseline were randomly assigned to two of the three 5-month mailings.
Control participants received an initial workbook that included the “Facing Forward” booklet from the National Cancer Institute and subsequent publicly available materials on PA, F&V intake, and dietary fat restriction. These materials were mailed on a similar schedule to the FRESH START intervention arm [44]. For example, control participants received the “Action Guide for Healthy Eating” brochure (National Institutes of Health) and the “Just Move” brochure (American Heart Association); a complete listing of the brochures is found in a published methods paper [44]. Current smokers in both study arms were mailed the American Lung Association “Quitting for Life” brochure (2003PS96328).
Participant retention
Computer-assisted telephone interviews of 45 to 55 minutes each were conducted at baseline and 1- and 2-year follow-ups. An excellent retention rate (90%) at 2-year follow-up was observed, with 519 survivors completing the 1-year follow-up and 489 survivors completing the 2-year follow-up. Reasons for attrition across both years of the study included participant withdrawal (n = 17), death (n = 8), familial illness (n = 7), and inability to reach the participant (n = 22). Attrition did not differ by sex or level of education; however, ethnic minority participants had a significantly higher attrition rate than Caucasian participants (16% vs. 9%, respectively, p = .02). In addition, the experimental arm had a higher attrition rate than the control arm (13% vs. 7%, respectively, p = .02).
Measures
Dietary outcomes
The Diet History Questionnaire (DHQ) [49-50] assesses fat intake, as well as consumption of many other foods and nutrients, during the past 12 months and was modified to include regionally consumed foods (e.g., hominy, okra). The DHQ has adequate reliability and validity [49-50]. Outcome variables for the present research included the number of servings of F&V per day, the percentage of kcal from fat, and the 100-point Diet Quality Index-Revised score [31], with higher numbers indicating better diet quality.
Physical activity
Participants completed the 7-day Physical Activity Recall (PAR) [51-53], a valid measure of PA that has been used in several large-scale studies [51-52]. Total minutes per week of moderate to vigorous PA was the outcome variable for the present research.
Self-efficacy
Participants rated their self-efficacy in response to the question, “How sure are you that you could (exercise at least 30 minutes a day at least 5 days a week; eat at least 5 servings of F&V per day; or eat a low-fat diet)?” Descriptions of exercise, F&V servings, and a low-fat diet were provided before each question (e.g., exercise: “Examples of exercise are brisk walking, cycling, swimming, weight lifting, or other activities that get your heart pounding or have you break out in a sweat and are NOT part of your normal activity on the job”). Response options ranged from 1 (very unsure) to 5 (very sure). The items were developed jointly by the 5-a-Day community research team and the NCI and validated against larger sets of self-efficacy items [54-55]. The items also have been tested with ethnically diverse samples, including African Americans in the Black Churches United for Better Health project [56-57].
Barriers
An author-constructed barriers questionnaire [44] assessed 16 common barriers to PA, 12 common barriers to F&V consumption, and nine common barriers to adhering to a low-fat diet. For each item, participants were asked to indicate “yes, it was a reason for them not practicing goal behavior” or “no, it wasn’t a reason for them not practicing goal behavior.”
Data Analysis
We conducted multiple regression analyses to test for mediation using SPSS statistical software (version 19.0; SPSS, Chicago, IL, USA). Assumptions of multiple regression were evaluated using procedures outlined by Tabachnick and Fidell [58]. Skew and kurtosis indices suggested that the PA data deviated from normality. Logarithmic transformation of the PA data to reduce skewness and kurtosis did not alter the study findings; thus, results are reported without transformation of the data. As recommended by Shrout and Bolger [59], a bootstrap procedure was used to examine the significance of the indirect effects of intervention condition on dietary outcomes via self-efficacy [60]. Bootstrapping is a nonparametric resampling approach that offers an empirical approximation of the sampling distributions of the indirect effect from the available data. Contrary to other widely used mediation methods [61-62], the bootstrap procedure does not involve assumptions about the shape of the distributions of the variables or the sampling distribution of the statistic. We used a macro developed by Preacher and Hayes to create 5,000 bootstrap resamples [60]. Shrout and Bolger [59] suggested that researchers report the 95% confidence interval (CI) for the significance of mean indirect effects from bootstrap results. If the CI does not include zero, then the indirect effect is considered statistically significant at the 0.05 level. Bias-corrected and accelerated CIs are reported, as they have shown better performance under a variety of assumptions than percentile CIs [63-64]. Moderated mediation analyses also were conducted using a macro developed by Preacher and Hayes [65]. Specifically, gender and age were examined as potential moderators of the relations between self-efficacy and dietary outcomes.
The analysis of diet quality included data from all experimental participants who completed the study (n = 236) because each participant received at least one dietary intervention component (i.e., mailings to encourage F&V consumption, decreased fat intake, or both). When examining the effects of group assignment on specific health behaviors, only data from experimental participants who had received mailings targeting F&V intake (n = 111), kcal from fat (n = 190), and PA (n = 171) were included in each analysis. Data from control participants who completed the study were included in all analyses because the control arm received materials that targeted all three lifestyle practices (increased F&V intake, fat restriction, and PA). Intent-to-treat analyses were not conducted given the exploratory nature of this secondary analysis.
Baseline values of the mediator and dependent variables were included as covariates in all analyses; thus, the effects observed represent change during the study period. Changes in self-efficacy from baseline to year 1 were analyzed as potential mediators of the intervention’s effects on dietary outcomes at year 2. Demographic and medical variables were not included as covariates because they did not vary by intervention condition at baseline. Finally, multiple regression analyses were conducted across study conditions to examine whether change in self-efficacy from baseline to year 1 predicted PA at year 2 as well as potential relationships between barriers to goal behaviors and study outcomes.
Results
Table 1 presents descriptive statistics and comparisons of mean scores at 2-year follow-up for dietary outcomes and PA. Analyses are presented by outcome variable below, and unstandardized regression coefficients are reported. For each outcome, we first present the main effect of group assignment at year 2 (see Table 1). Then we report relations between group assignment and change in social cognitive factors (i.e., self-efficacy and barriers) from baseline to year 1 (see Table 2). Next, we report the extent to which change in social cognitive factors from baseline to year 1 predicted the outcome at year 2. Tests of mediation are presented if group assignment and the potential mediator (e.g., change in self-efficacy) were correlated with the outcome (see Figures 1a-b and 2). Finally, gender and age are examined as potential moderators of the mediated effects.
Table 1. Dietary outcomes and physical activity at baseline and 2-year follow-up as a function of group: assignment.
| FRESH START Intervention (n = 236) |
Attention Control (n = 253) |
||||
|---|---|---|---|---|---|
|
| |||||
| Baseline | 2-Year Follow-up |
Baseline | 2-Year Follow-up |
p | |
| Diet Quality Index- Revised score |
<.001 | ||||
| Mean | 66.6 | 71.5 | 67.0 | 68.9 | |
| Standard deviation | 11.1 | 10.5 | 9.4 | 10.6 | |
| Total percent of calories from fat |
.001 | ||||
| Mean | 38.0 | 36.5 | 37.8 | 38.0 | |
| Standard deviation | 5.7 | 6.6 | 5.6 | 5.4 | |
| No. of daily servings of F&V |
.152 | ||||
| Mean | 5.1 | 6.0 | 5.0 | 5.7 | |
| Standard deviation | 2.7 | 2.7 | 2.3 | 2.8 | |
| Physical activity, min/wk |
.740 | ||||
| Mean | 55.1 | 113.1 | 42.9 | 103.6 | |
| Standard deviation | 115.9 | 145.1 | 90.0 | 143.1 | |
Note. The Diet Quality Index-Revised scores range from 0 to 100 with higher scores indicating better diet quality. P values are presented for group comparisons at follow-up, controlling for baseline values of the dependent variables. F&V = fruits and vegetables.
Table 2. Self-efficacy and barriers at baseline and 1-year follow-up as a function of group assignment.
| FRESH START Intervention (n = 236) |
Attention Control (n = 253) |
||||
|---|---|---|---|---|---|
|
| |||||
| Baseline | 1-Year Follow-up |
Baseline | 1-Year Follow-up |
p | |
| Self-efficacy for fat restriction |
3.9 (.95) | 4.1 (.94) | 3.9 (.98) | 3.9 (1.0) | .025 |
| Self-efficacy for eating more F&V |
3.9 (.92) | 4.2 (.94) | 3.9 (1.1) | 4.0 (1.0) | .027 |
| Self-efficacy for physical activity |
3.9 (1.1) | 3.9 (1.1) | 3.8 (1.2) | 3.7 (1.2) | .244 |
| Barriers to fat restriction |
3.0 (2.2) | 2.6 (2.0) | 3.2 (2.1) | 2.6 (2.0) | .38 |
| Barriers to eating more F&V |
2.0 (2.2) | 2.0 (2.1) | 1.9 (1.9) | 1.8 (2.0) | .32 |
| Barriers to physical activity |
3.5 (2.5) | 3.3 (2.3) | 3.5 (2.4) | 3.0 (2.2) | .10 |
Note. Standard deviations are in parentheses. Self-efficacy scores range from 1 to 5 with higher scores indicating greater self-efficacy. Barriers scores range from 0 to 9 for barriers to fat restriction, 0 to 12 for barriers to eating more F&V, and 0 to 16 for barriers to physical activity with higher scores indicating more barriers. P values are presented for group comparisons at follow-up, controlling for baseline values of the dependent variable. F&V = fruits and vegetables.
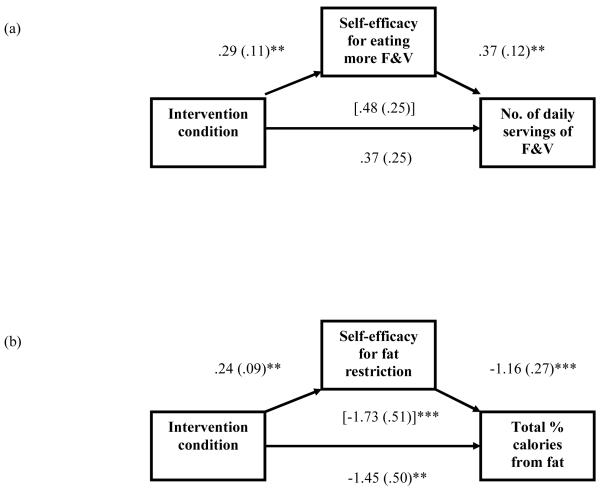
Figures 1a and 1b.
Models depicting the effects of intervention condition (coded 0 = attention control, 1 = FRESH START intervention) on dietary outcomes at year 2 and mediators at year 1, adjusting for baseline mediator and dependent variables. Unstandardized regression coefficients are reported. Standard errors are in parentheses. The coefficient in brackets is from the model that did not include the mediator. Self-efficacy scores range from 1 to 5 with higher scores indicating greater self-efficacy. F&V = fruits and vegetables. **p < .01. ***p < .001.
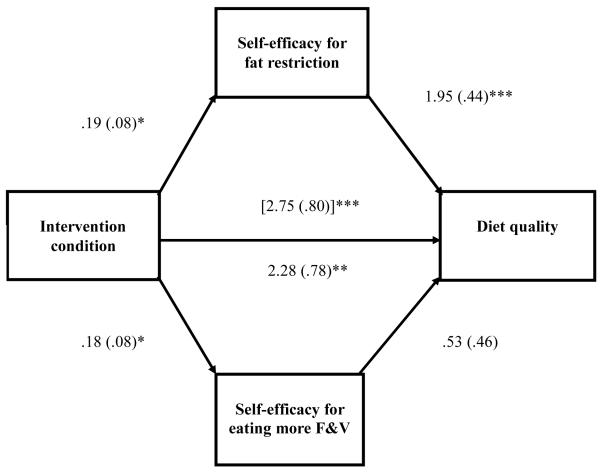
Figure 2.
Model depicting the effects of intervention condition (coded 0 = attention control, 1 = FRESH START intervention) on diet quality at year 2 and mediators at year 1, adjusting for baseline mediator and dependent variables. Unstandardized regression coefficients are reported. Standard errors are in parentheses. The coefficient in brackets is from the model that did not include the mediator. Self-efficacy scores range from 1 to 5 with higher scores indicating greater self-efficacy. Diet quality scores range from 0 to 100 with higher scores indicating better diet quality. F&V = fruits and vegetables. *p < .05. **p < .01. ***p < .001.
Fruit and Vegetable Consumption
As previously reported [32], F&V intake did not significantly differ as a function of group assignment at 2-year follow-up (see Table 1). Group assignment showed mixed associations with changes in social cognitive factors related to F&V intake from baseline to year 1. Specifically, experimental participants showed greater change in self-efficacy for F&V intake than control participants, but did not differ from controls with regard to change in barriers to F&V intake (see Table 2) [35]. In the current study, we examined whether change in self-efficacy for F&V intake and change in barriers to F&V intake from baseline to year 1 predicted daily servings of F&V at year 2 when controlling for baseline levels of the dependent variable. In the total sample, change in self-efficacy for F&V intake was positively associated with daily servings of F&V, B = .41, SE = .11, t(488) = 3.72, p < .001, and change in barriers to F&V intake was negatively associated with this outcome, B = −.25, SE = .06, t(488) = −.17, p < .001.
Next, we tested the hypothesis that change in self-efficacy for F&V intake would mediate the relation between intervention condition and daily servings of F&V (see Figure 1a). This model accounted for 38% of the variance in daily servings of F&V, F(4, 359) = 53.95, p < .001. The effect of the intervention was attenuated by the mediator, and partial mediation was suggested (mean indirect effect = .11, SE =.05, 95% CI = .03 to .23). Experimental participants endorsed greater change in self-efficacy for F&V intake than did control participants, which, in turn, was associated with more daily servings of F&V. Gender and age did not significantly interact with change in self-efficacy for F&V intake to predict daily servings of F&V.
Fat Restriction
As previously reported, the main effect of experimental condition was significant for percentage of kcal from fat at 2 years post-baseline (see Table 1) [32]. Experimental participants reported fewer calories from fat than control participants. Group assignment showed mixed associations with changes in social cognitive factors related to fat restriction from baseline to year 1. As found in Table 2, experimental participants showed greater change in self-efficacy for fat restriction than control participants, but did not differ from controls with regard to change in barriers to fat restriction [35]. In the present study, we examined whether change in self-efficacy for fat restriction and change in barriers to fat restriction from baseline to year 1 predicted the percentage of kcal from fat at year 2 when controlling for baseline levels of the dependent variable. In the total sample, change in self-efficacy for fat restriction was negatively associated with the percentage of kcal from fat, B = −1.28, SE = .26, t(488) = −4.94, p < .001, and change in barriers to fat restriction was positively associated with this outcome, B = .55, SE = .14, t(488) = 3.88, p < .001.
Next, we evaluated the hypothesis that change in self-efficacy for fat restriction would mediate the relation between intervention condition and the percentage of kcal from fat (see Figure 1b). This model accounted for 24.5% of the variance in the percentage of kcal from fat, F(4, 438) = 35.46, p < .001. The effect of the intervention was attenuated by the mediator, and partial mediation was suggested (mean indirect effect = −.28, SE =.12, 95% CI = −.55 to −.09). Experimental participants reported greater change in self-efficacy for fat restriction than did control participants, which, in turn, was associated with a lower percentage of kcal from fat. Gender and age did not significantly interact with change in self-efficacy for fat restriction to predict the percentage of kcal from fat.
Global Diet Quality
Prior research found that the main effect of experimental condition was significant for global diet quality at 2 years post-baseline (see Table 1) [32]. Experimental participants reported better diet quality than control participants. In this study, we examined whether change in self-efficacy for fat restriction and F&V intake and change in barriers to these dietary practices from baseline to year 1 predicted diet quality at year 2 when controlling for baseline diet quality. In the total sample, changes in self-efficacy for fat restriction and F&V intake were positively associated with diet quality (self-efficacy for fat restriction: B = 2.22, SE = .43, t(488) = 5.23, p < .001; self-efficacy for F&V intake: B = 1.36, SE = .46, t(488) = 2.99, p < .01), and changes in barriers to fat restriction and F&V intake were negatively associated with diet quality (barriers to fat restriction: B = −.94, SE = .23, t(488) = −4.01, p < .001; barriers to F&V intake: B = −.60, SE = .25, t(488) = −2.40, p < .05).
Next, we tested the hypothesis that changes in self-efficacy for fat restriction and self-efficacy for F&V intake would mediate the association between the intervention and diet quality (see Figure 2). The entire model accounted for 35.4% of the variance in diet quality, F(6, 482) = 44.03, p < .001, and the effect of the intervention was attenuated by the mediators. Results of the bootstrap procedure suggested that change in self-efficacy for fat restriction partially mediated the intervention’s effect on diet quality (mean indirect effect = .38, SE =.19, 95% CI = .08 to .84), whereas change in self-efficacy for F&V intake did not (mean indirect effect = .09, SE = .09, 95% CI = −.04 to .35).
Gender interacted with change in self-efficacy for fat restriction to predict diet quality (B = 1.76, SE = .79, t(487) = 2.23, p < .05), which supported a moderated mediation model. Specifically, results suggested that change in self-efficacy for fat restriction partially mediated the association between intervention condition and diet quality for men (mean indirect effect = .60, SE =.29, z = 2.10, p < .05), but not for women (mean indirect effect = .26, SE =.16, z = 1.60, p = .11). Age did not significantly interact with change in self-efficacy for fat restriction to predict diet quality.
Physical Activity
PA did not significantly differ as a function of group assignment at 2-year follow-up (see Table 1). In addition, as previously reported, experimental participants did not differ from control participants with regard to changes in self-efficacy for PA or barriers to PA from baseline to year 1 (see Table 2) [35]. In the current study, we examined whether change in self-efficacy for PA and change in barriers to PA from baseline to year 1 predicted total minutes of PA per week at year 2 when controlling for baseline levels of PA. In the total sample, change in self-efficacy for PA was positively correlated with total minutes of PA per week, B = 17.54, SE = 5.95, t(488) = 2.95, p < .01, and change in barriers to PA was negatively correlated with this outcome, B = −7.02, SE = 3.45, t(488) = −2.04, p < .05.
Discussion
This study evaluates whether change in self-efficacy accounts for the positive health behavior outcomes of FRESH START, a diet and PA intervention for cancer survivors, at 2 years post-baseline. As hypothesized, change in self-efficacy for F&V intake partially explained the intervention’s effect on daily servings of F&V, and change in self-efficacy for fat restriction partially explained the intervention’s effect on percentage of kcal from fat. Also consistent with our hypothesis, change in self-efficacy for fat restriction partially mediated the intervention’s effect on overall diet quality; however, this mediating effect was only found for men. In addition, across gender groups, change in self-efficacy for F&V intake did not mediate the intervention’s effect on diet quality. Our results replicate the mediating effects of self-efficacy on F&V intake and fat restriction found at 1-year follow-up [35] and extend these findings by suggesting that change in self-efficacy may play an important role in the durability of dietary gains. Our findings are also consistent with those of prior intervention trials that found support for the mediating effect of behavior-specific self-efficacy on F&V intake in community-dwelling adults [40-42].
The present results in combination with prior research largely support the prediction derived from Social Cognitive Theory that confidence in one’s ability to perform a behavior will play a critical role in health behavior change [33-34]. The FRESH START intervention was designed to increase self-efficacy by encouraging incremental goal setting with a focus on overcoming barriers to lifestyle change and reinforcing participants’ progress toward meeting their goals. Indeed, FRESH START participants reported positive changes in self-efficacy for dietary practices that predicted long-term change in F&V intake and fat restriction. These durable dietary changes support the notion of a “teachable moment” during which newly diagnosed cancer patients experience enhanced motivation to improve health behaviors [66-68]. Change in behavior-specific self-efficacy, especially self-efficacy for F&V intake, was less predictive of diet quality, which may reflect the varied food patterns that comprise this global construct.
Results also suggested that change in self-efficacy for PA during the first year of the trial and PA at 2-year follow-up did not vary by group assignment. The restricted range of self-efficacy and the reliance on 1-week assessments of PA across time points may have limited our ability to detect group differences in these variables. However, as hypothesized, a positive association was found between change in self-efficacy for PA from baseline to year 1 and total minutes of PA per week at year 2. To date, formal tests of self-efficacy as a mediator of PA interventions for healthy adolescents and adults have yielded mixed findings [69-73]. However, positive associations between self-efficacy and PA over a 1 year time period have been replicated across healthy adult samples [74-75]. The present results extend these findings by showing that self-efficacy for PA predicted cancer survivors’ PA at 2-year follow-up, though there was no evidence of mediation.
This study contributes to the limited literature on psychosocial mediators in diet and PA intervention trials involving cancer survivors as well as maintenance of these behaviors. A strength of the present analysis is the use of formal tests of mediation [60] with past beliefs and behavior as covariates. Findings provide a reliable estimate of the impact of the intervention on health beliefs and behavior due to the rigorous methods (e.g., randomization, attention control condition) and low attrition rate (10%). Our trial extends prior research by examining the role of self-efficacy in long-term dietary and PA outcomes of a mailed print intervention. Scarce research has examined the extent to which self-efficacy and other theory-driven factors predict health behavior maintenance in cancer survivors, a population at increased risk for chronic diseases [4-8]. Instead, most trials have examined the short-term effects of hospital-based or telephone-based programs on one health behavior. In addition, this study enrolled a large sample of breast and prostate cancer survivors throughout North America, whereas most studies have accrued smaller numbers of survivors of a single cancer type at one institution.
The present analysis is limited in that it does not comprehensively test Social Cognitive Theory by including other social cognitive factors that may influence health behaviors (e.g., facilitators, outcome expectations, self-regulatory strategies, social support). We did, however, find that changes in the number of barriers to goal behaviors from baseline to year 1 predicted study outcomes at year 2, although barriers did not vary by group assignment. Future randomized health promotion studies should examine the relative contribution of self-efficacy and other theory-driven variables to behavior change by prospectively assessing intervention components [76]. Another potential limitation is the reliance on 1-item measures of self-efficacy for fat restriction, F&V intake, and PA. These measures assessed how sure respondents felt that they could perform goal behaviors on 5-point scales, rather than their degree of confidence in overcoming specific barriers to goal behaviors on 11-point scales from 0% to 100%, as recommended by Bandura [77]. Although the method of assessing self-efficacy in this study has been widely used to reduce respondent burden, it may result in underestimations of effect sizes. Multi-item scales are more reliable and capture greater variability in the construct than single-item scales. We also may have obtained different findings regarding self-efficacy for PA if we had assessed the goal behavior (i.e., 150+ minutes of exercise per week) rather than self-efficacy for exercising “at least 30 minutes a day at least 5 days a week.” In addition, dietary and PA outcomes were self-reported. Although self-reported dietary outcomes were strongly supported by biomarker data (e.g., plasma alpha-carotene) from a 23% subsample at 1-year follow-up [28], further collection of biomarker data would have been desirable. Furthermore, there is no consensus with regard to clinically meaningful differences in self-efficacy and dietary and PA outcomes. Research is needed to address this gap in the scientific literature. In addition, only data from survivors who completed the study were included in the present analyses. However, there was minimal attrition and the sample size yielded adequate statistical power for examining the effect of the intervention on study outcomes [28]. It is possible, however, that the study was underpowered to detect moderated mediation effects. Simulation studies have found that bias-corrected and accelerated CIs, the approach used in this study, showed particularly high power; however, research on power for moderated mediation has been conducted under limited sets of conditions [65]. Finally, the lower proportions of ethnic minorities, older adults, and individuals with lower levels of education in this trial relative to the general population of cancer survivors should be noted. Further research is needed to examine psychosocial mechanisms underlying the effects of health promotion interventions with samples that are entirely representative of the population at large.
The present findings suggest that self-efficacy plays an important role in long-term adherence to healthy dietary practices among cancer survivors and that dietary interventions for this population should be designed to enhance self-efficacy for healthy eating. Self-efficacy may increase as survivors are encouraged to set specific, attainable goals and are reinforced for steps toward goal attainment. Identifying key psychosocial determinants of long-term health behavior change is critical to the development of highly efficacious and cost-effective health promotion interventions for the growing population of cancer survivors.
Acknowledgments
FRESH START is supported by the National Institutes of Health through the following grants: CA81191, CA74000, CA63782, and M01-RR-30. The work of the first author is partly supported by KL2 RR025760 (A. Shekhar, PI). The authors wish to thank Drs. Colleen McBride and Bercedis Peterson, other co-investigators on this trial, as well as to acknowledge the memory of Dr. Elizabeth Clipp. We also wish to thank Drs. Marci Campbell, Harvey Cohen, Bethany Jackson, P. Kelly Marcom, Bess Marcus, and Thomas Polascik for their guidance in areas of design and implementation, and Drs. Walter Ettinger, Frank Harrell, and Thomas Scott for serving on our external data safety and monitoring board. We are grateful for the contributions and professionalism demonstrated by the staff of People Designs, Inc. (David Farrell, MPH, Jetze Beers, Marley Beers, MFA, and Kristin Trangsrud, MPH) who helped craft the FRESH START intervention materials, and Dr. Cecelia and Len Doak of Patient Learning Associates, Inc. who helped make them easily understandable. The authors also wish to thank the following individuals who have and are continuing to contribute expertise and support: Sreenivas Algoti, MS, Teresa Baker, Rita Freeman, Sonya Goode Green, MPH, Heather MacDonald, Barbara Parker, Shelley Rusincovitch, Rachel Schanberg, MS, and Russell Ward. We also are grateful to our participating institutions (Duke University Medical Center, Durham Regional Hospital, Durham VA Medical Center, Maria Parham Hospital, Raleigh Community Hospital, and Rex Healthcare), cancer registrars/patient care coordinators (Renee Gooch, Blanche Sellars, Dortch Smith, Donna Thompson, and Cheri Willard), and participating physicians (Drs. Victor E. Abraham, Anjana Acharya, David Albala, Alex Althausen, Everett Anderson, Roger F. Anderson, Mitchell Anscher, Guillermo Arana, Carlos Arcangelli, Sucha Asbell, Michael Aspera, James N. Atkins, Cheryl Aylesworth, Margaret Barnes, Brian Bauer, Louis Baumann, Michael Beall, Gregory Bebb, Michael Beecher, John Bell, Marc Benevides, Brian C. Bennett, Robert Bennett, Robert Bennion, James Benton, Stuart Bergman, William R. Berry, Kelly Blair, Kimberly Blackwell, Gayle Blouin, Peter Blumencranz, William Bobbitt, Daniel Borison, William Bouchelle, Elaine Bouttell, Don Boychuk, Barb Boyer, Albert Brady, Thomas Brammer, Scott Brantley, Joanna Brell, Charles Brendler, Thomas Brennan, Donald Brennan, Elizabeth Brew, Thomas Bright, Philip Brodak, Dieter Bruno, Dale Bryansmith, Niall Buckley, Walter W. Burns, W. Woodrow Burns, Thomas Buroker, Barbara Burtness, Amanullah Buzdar, David Caldwell, Elizabeth E. Campbell, Susan Campos, Sean Canale, Woodward Cannon, Dominick Carbone, Albert Casazza, George Case, Michael Cashdollar, Stanton Champion, Nitin Chandramouli, Marie Chenn, S. Chew, Stephen Chia, Warren Chin, Richard Chiulli, Elaine Chottiner, Walter Chow, Peter Clark, Kenneth Collins, Barry Conway, Suzanne Conzen, David Cook, John Corman, Shawn Cotton, D. Scott Covington, Edwin B. Cox, Frank Critz, Nancy J. Crowley, Sam Currin, Brian Czernieki, Brian Czito, Bruce Dalkin, John T. Daniel, John Danneberger, Leroy Darkes, Glenn Davis, Walter E. Davis, Jean de Kernion, Pat DeFusco, Fletcher Derrick, Margaret Deutsch, Gayle Dilalla, Robert Diloreto, Craig Donatucci, Michael Donovan, John Doster, Bradford Drury, Paul Dudrick, William Dunlap, Edward Eigner, Maha Elkordy, Matthew Ellis, Richard Evans, Jerry Fain, Anne Favret, Ira Fenton, Dirk Fisher, James Foster, Wyatt Fowler, Jeffrey Freeland, Daniel Frenning, Ralf Freter, Michael Frontiera, Michele Gadd, Anthony Galanos, Ronald Garcia, Antonio Gargurevich, Helen Garson, Morris Geffen, Gregory Georgiade, Ward Gillett, Paul Gilman,, Jeffrey Gingrich, Deborah Glassman, John Gockerman, Richard Goodjoin, J. Phillip Goodson, Joel Goodwin, Teong Gooi, Jeffrey Gordon, Narender Gorukanit, James Gottesman, Lav Goyal, William Graber, Margaret Gradison, Gordon Grado, Mark Graham, Michael Grant, Stephen Greco, Carl Greene, Peter Grimm, Nima Grissom, Irina Gurevich, Carol Hahn, Alex Haick, Craig Hall, Edward Halperin, Sabah Hamad, R. Erik Hartvigsen, Harold Harvey, Paul Hatcher, James Hathorn, Robert Hathorn, Carolyn Hendricks, David Hesse, Martin Hightower, Peter Ho, Leroy Hoffman, Frankie Ann Holmes, Sidney Hopkins, Samuel Huang, Robert Huben, Cliff Hudis, Thelma Hurd, Sally Ingram, Philip Israel, Naresh Jain, Nora Jaskowiak, Jean Joseph, Jacqueline Joyce, Walton Joyner, Ray Joyner, Scott Kahn, Sachin Kamath, Carsten Kampe, Michael Kane, Richard Kane, Michael Kasper, Uday Kavde, Thomas Keeler, Douglas Kelly, Michael Kent, Kevin Kerlin, Kenneth Kern, Huathin Khaw, Jay Kim, Houston Kimbrough, Charmaine Kim-Sing, John Kishell, Petras Kisielius, George Kmetz, Lawrence Knott, Ronald Konchanin, Cyrus Kotwall, Kenneth Kotz, Charles Kraus, Bruce Kressel, Alan Kritz, John Lacey, Susan Laing, David Larson, Barry Lee, W. Robert Lee, Douglas Leet, Natasha Leighl, George Leight, Paul LeMarbre, Herbert Lepor, Seth Lerner, Margaret Levy, Lori Lilley, Steve Limentani, Robert Lineberger, Lenis Livesay, Fred J. Long, Richard Love, Mark Lucas, James Lugg, Charles Lusch, H. Kim Lyerly, Janet Macheledt, Thomas Maddox, Patrick Maguire, Mark Makhuli, Rajeev Malik, Mary Manascalco-Theberge, P. Kelly Marcom, Manfred Marcus, Neal Mariados, Lawrence Marks, Shona Martin, Eric Matayoshi, Gordon Mathes, Mark McClure, Scott McGinnis, David McLeod, Warren McMurry, William McNulty, Robert McWilliams, Cynthia Menard, Mani Menon, Richard Michaelson, Michael Mikolajczyk, David Miles, Dixie Mills, Jesse Mills, David Mintzer, David Molthorp, Allen Mondzac, Gustavo Montana, Angelica Montesano, Leslie Montgomery, Joseph O. Moore, William Morgan, Patricia Morrison, Michael A. Morse, Jacek Mostwin, Judd Moul, Brian Murphy, William Muuse, J. William Myers, Richard S. Myers, Richard Mynatt, Gene Naftulin, Vishwanath Nagale, Niam Nazha, Charles Neal, James Neidhart, Joseph D. Neighbors, Philip Newhall, Robert Nichols, William Niedrach, Peter Oh, John Oh, John A. Olson, Robert Ornitz, David Ornstein, Alexander Panutich, Maria Papaspyrou, Steven Papish, Dhaval Parikh, James Parsons, George Paschal, Robert Paterson, Dev Paul, David F. Paulson, Samuel Peretsman, Jorge Perez, Mark Perman, Thomas Polascik, Klaus Porzig, David C. Powell, Kenneth Prebil, Glenn Preminger, Adele Preto, Leonard Prosnitz, Robert Prosnitz, Scott K. Pruitt, Robert Reagan, Carl Reese, John Reilly, Robert Renner, Alan Rice, Melvin Richter, Adrien Rivard, Ralph Roan, Cary Robertson, Steve Robeson, Linda Robinson, Mark Romer, Eric Rosen, Amy Rosenthal, Alison Ross, William Russell, Lewis Russell, Charles Scarantino, Candace Schiffer, Mark Schoenberg, Mark Scholz, William Schuessler, Stuart Schwartzberg, Janell Seeger, Victoria Seewaldt, Hillard Seigler, Pearl Seo, Phillip Shadduck, Timothy Shafman, Rohit Shah, Arieh Shalhav, Peter Shapiro, Fred Shapiro, Heather Shaw, Robert Siegel, Daniel Silver, Mary Simmonds, Jane Skelton, Barbara Smith, Mitchell Sokoloff, Douglas Sorensen, Angela Soto-Hamlin, Alexander Sparkuhl, Thomas Spears, Merle Sprague, Mark St. Lezin, Steven J. Stafford, B. Dino Stea, Gary Steinberg, Patricia Steinecker, Mary Stewart, Jerry Stirman, Lewis Stocks, Christopher Stokoe, Warren Streisand, Mark Sturdivant, Paul Sugar, Steven Sukh, Perry Sutaria, Linda Sutton, Phillip Sutton, John Sylvester, Beth Szuck, Darrell Tackett, Ernesto Tan, Sharon Taylor, John Taylor, Dina Tebcherany, Chris Teigland, Marcos Tepper, Haluk Tezcan, William Thoms, Ellis Tinsley, Jr., Lisa Tolnitch, Angel Torano, Frank Tortora, William Truscott, Theodore Tsangaris, Peter Tucker, Walter Tucker, Ingolf Tuerk, Wade Turlington, Richard Tushman, Michael Tyner, Pascal Udekwu, Eric Uhlman, Linda Vahdat, Louis Vandermolen, George Vassar, Margaret Vereb, Johannes Vieweg, Daniel Vig, Tom Vo, Walter Vogel, David Wahl, B. Alan Wallstedt, Patrick Walsh, Philip Walther, Robert Waterhouse, Charles Wehbie, Seth Weinreb, Marissa Weiss, Raul Weiss, Geoffrey White, Edward Whitesides, Lee Wilke, Hamilton Williams, Matthew Wilner, Don Wilson, James S. Wilson, Bristol Winslow, Rachel Wissner, James Wolf, Lawrence Womack, Charles Woodhouse, Clifford Yaffe, Daniel Yao, Richard Yelverton, Lemuel Yerby, Mark Yoffe, Martin York, Gregory Zagaja, Kenneth Zeitler, Elizabeth Zubek, and Raul Zunzunegui). Most of all, we are indebted to the many cancer survivors who helped us pilot test, re-test, and then formally test the intervention.
Footnotes
Authors’ Disclosures of Potential Conflicts of Interest
The authors indicated no potential conflicts of interest.
References
- 1.Gapstur SM, Thun MJ. Progress in the war on cancer. JAMA. 2010;303:1084–5. doi: 10.1001/jama.2010.284. [DOI] [PubMed] [Google Scholar]
- 2.National Cancer Institute [Accessed on March 15, 2011];Cancer advances in focus. Available at: http://www.cancer.gov/cancertopics/factsheet/cancer-advances-in-focus/cancer. Updated November 29, 2010.
- 3.Altekruse SF, Kosary CL, Krapcho M, Neyman N, Aminou R, Waldron W, Ruhl J, Howlader N, Tatalovich Z, Cho H, Mariotto A, Eisner MP, Lewis DR, Cronin K, Chen HS, Feuer EJ, Stinchcomb DG, Edwards BK, editors. SEER Cancer Statistics Review, 1975-2007. National Cancer Institute; Bethesda, MD: 2010. http://seer.cancer.gov/csr/1975_2007/, based on November 2009 SEER data submission, posted to the SEER web site. [Google Scholar]
- 4.Aziz NM. Cancer survivorship research: Challenge and opportunity. J Nutr. 2002;132:3494S–503S. doi: 10.1093/jn/132.11.3494S. [DOI] [PubMed] [Google Scholar]
- 5.Rowland J, Mariotto A, Aziz N, et al. Cancer survivorship-United States, 1971-2001. MMWR Morbid Mortal Wkly Rep. 2004;53:526–9. [PubMed] [Google Scholar]
- 6.Yabroff KR, Lawrence WF, Clauser S, Davis WW, Brown ML. Burden of illness in cancer survivors: Findings from a population-based national sample. J Natl Cancer Inst. 2004;96:1322–30. doi: 10.1093/jnci/djh255. [DOI] [PubMed] [Google Scholar]
- 7.Aziz NM, Rowland JH. Trends and advances in cancer survivorship research: Challenge and opportunity. Semin Radiat Oncol. 2003;13:248–66. doi: 10.1016/S1053-4296(03)00024-9. [DOI] [PubMed] [Google Scholar]
- 8.Hewitt M, Rowland JH, Yancik R. Cancer survivors in the United States: Age, health, and disability. J Gerontol A Biol Sci Med Sci. 2003;58:82–91. doi: 10.1093/gerona/58.1.m82. [DOI] [PubMed] [Google Scholar]
- 9.Doyle C, Kushi LH, Byers T, et al. Nutrition and physical activity during and after cancer treatment: An American Cancer Society guide for informed choices. CA: A Cancer Journal for Clinicians. 2006;56:323–53. doi: 10.3322/canjclin.56.6.323. [DOI] [PubMed] [Google Scholar]
- 10.Pinto B, Trunzo J. Health behaviors during and after a cancer diagnosis. Cancer. 2005;104:2614–23. doi: 10.1002/cncr.21248. [DOI] [PubMed] [Google Scholar]
- 11.Pearson TA, Blair SN, Daniels SR, et al. AHA guidelines for primary prevention of cardiovascular disease and stroke: 2002 update. Circulation. 2002;106:388–91. doi: 10.1161/01.cir.0000020190.45892.75. [DOI] [PubMed] [Google Scholar]
- 12.Aronson WJ, Barnard RJ, Freedland SJ, et al. Growth inhibitory effect of low fat diet on prostate cancer cells: results of a prospective, randomized dietary intervention trial in men with prostate cancer. J Urol. 2010;183:345–50. doi: 10.1016/j.juro.2009.08.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chlebowski RT, Blackburn GL, Thomson CA, et al. Dietary fat reduction and breast cancer outcome: Interim efficacy results from the Women’s Intervention Nutrition Study. J Natl Cancer Inst. 2006;98:1767–76. doi: 10.1093/jnci/djj494. [DOI] [PubMed] [Google Scholar]
- 14.George SM, Neuhouser ML, Mayne ST, et al. Postdiagnosis diet quality is inversely related to a biomarker of inflammation among breast cancer survivors. Cancer Epidemiol Biomarkers Prev. 2010;19:2220–8. doi: 10.1158/1055-9965.EPI-10-0464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gold EB, Pierce JP, Natarajan L, et al. Dietary pattern influences breast cancer prognosis in women without hot flashes: The women’s healthy eating and living trial. J Clin Oncol. 2009;27:352–9. doi: 10.1200/JCO.2008.16.1067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rock CL, Flatt SW, Natarajan L, et al. Plasma carotenoids and recurrence-free survival in women with a history of breast cancer. J Clin Oncol. 2005;23:6631–8. doi: 10.1200/JCO.2005.19.505. [DOI] [PubMed] [Google Scholar]
- 17.Rock CL, Natarajan L, Pu M, et al. Longitudinal biological exposure to carotenoids is associated with breast cancer-free survival in the Women’s Healthy Eating and Living Study. Cancer Epidemiol Biomarkers Prev. 2009;18:486–94. doi: 10.1158/1055-9965.EPI-08-0809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mayer D, Terrin N, Menon U, Kreps G, et al. Health behaviors in cancer survivors. Oncol Nurs Forum. 2007;34:643–51. doi: 10.1188/07.ONF.643-651. [DOI] [PubMed] [Google Scholar]
- 19.Bellizzi KM, Rowland JH, Jeffery DD, McNeel T. Health behaviors of cancer survivors: Examining opportunities for cancer control intervention. J Clin Oncol. 2005;23:8884–93. doi: 10.1200/JCO.2005.02.2343. [DOI] [PubMed] [Google Scholar]
- 20.Coups EJ, Ostroff JS. A population-based estimate of the prevalence of behavioral risk factors among adult cancer survivors and noncancer controls. Prev Med. 2005;40:702–11. doi: 10.1016/j.ypmed.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 21.Stull VB, Snyder DC, Demark-Wahnefried W. Lifestyle interventions in cancer survivors: designing programs that meet the needs of this vulnerable and growing population. J Nutr. 2007;137:243S–8S. doi: 10.1093/jn/137.1.243S. [DOI] [PubMed] [Google Scholar]
- 22.Pekmezi DW, Demark-Wahnefried W. Updated evidence in support of diet and exercise interventions in cancer survivors. Acta Oncol. 2011;50:167–78. doi: 10.3109/0284186X.2010.529822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Demark-Wahnefried W, Case LD, Blackwell K, et al. Results of a diet/exercise feasibility trial to prevent adverse body composition change in breast cancer patients on adjuvant chemotherapy. Clin Breast Cancer. 2008;8:70–9. doi: 10.3816/CBC.2008.n.005. [DOI] [PubMed] [Google Scholar]
- 24.Demark-Wahnefried W, Pinto BM, Gritz ER. Promoting health and physical function among cancer survivors: Potential for prevention and questions that remain. J Clin Oncol. 2006;24:5125–31. doi: 10.1200/JCO.2006.06.6175. [DOI] [PubMed] [Google Scholar]
- 25.Morey MC, Snyder DC, Sloane R, et al. Effects of home-based diet and exercise on functional outcomes among older, overweight long-term cancer survivors: RENEW: a randomized controlled trial. JAMA. 2009;301:1883–91. doi: 10.1001/jama.2009.643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Parsons JK, Newman V, Mohler JL, Pierce JP, Paskett E, Marshall J. The Men’s Eating and Living (MEAL) study: A Cancer and Leukemia Group B pilot trial of dietary intervention for the treatment of prostate cancer. Urology. 2008;72:633–7. doi: 10.1016/j.urology.2007.11.050. [DOI] [PubMed] [Google Scholar]
- 27.Ferrer R, Huedo-Medina T, Johnson B, Ryan S, Pescatello L. Exercise interventions for cancer survivors: A meta-analysis of quality of life outcomes. Ann Behav Med. 2011;41:32–47. doi: 10.1007/s12160-010-9225-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Demark-Wahnefried W, Clipp EC, Lipkus IM, et al. Main outcomes of the FRESH START trial: a sequentially tailored, diet and exercise mailed print intervention among breast and prostate cancer survivors. J Clin Oncol. 2007;25:2709–18. doi: 10.1200/JCO.2007.10.7094. [DOI] [PubMed] [Google Scholar]
- 29.Mai V, Kant AK, Flood A, Lacey JV, Schairer C, Schatzkin A. Diet quality and subsequent cancer incidence and mortality in a prospective cohort of women. Int J Epidemiol. 2005;34:54–60. doi: 10.1093/ije/dyh388. [DOI] [PubMed] [Google Scholar]
- 30.Kant AK, Schatzkin A, Graubard BI, Schairer C. A prospective study of diet quality and mortality in women. JAMA. 2000;283:2109–15. doi: 10.1001/jama.283.16.2109. [DOI] [PubMed] [Google Scholar]
- 31.Haines PS, Siega-Riz AM, Popkin BM. The Diet Quality Index revised: A measurement instrument for populations. J Am Diet Assoc. 1999;99:697–704. doi: 10.1016/S0002-8223(99)00168-6. [DOI] [PubMed] [Google Scholar]
- 32.Christy SM, Mosher CE, Sloane R, Snyder DC, Lobach D, Demark-Wahnefried W. Long-term dietary outcomes of the FRESH START intervention for breast and prostate cancer survivors. J Am Diet Assoc. doi: 10.1016/j.jada.2011.09.013. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bandura A. Social Learning Theory. Prentice Hall; Englewood Cliffs, NJ: 1977. [Google Scholar]
- 34.Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31:143–64. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- 35.Mosher CE, Fuemmeler BF, Sloane R, et al. Change in self-efficacy partially mediates the effects of the FRESH START intervention on cancer survivors’ dietary outcomes. Psychooncology. 2008;17:1014–23. doi: 10.1002/pon.1327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Glasgow RE, Klesges LM, Dzewaltowski DA, Bull SS, Estabrooks P. The future of health behavior change research: what is needed to improve translation of research into health promotion practice? Ann Behav Med. 2004;27:3–12. doi: 10.1207/s15324796abm2701_2. [DOI] [PubMed] [Google Scholar]
- 37.Orleans CT. Promoting the maintenance of health behavior change: recommendations for the next generation of research and practice. Health Psychol. 2000;19:76–83. doi: 10.1037/0278-6133.19.suppl1.76. [DOI] [PubMed] [Google Scholar]
- 38.Rothman AJ. Toward a theory-based analysis of behavioral maintenance. Health Psychol. 2000;19:64–9. doi: 10.1037/0278-6133.19.suppl1.64. [DOI] [PubMed] [Google Scholar]
- 39.Glasgow RE, Klesges LM, Dzewaltowski DA, Bull SS, Estabrooks P. The future of health behavior change research: what is needed to improve translation of research into health promotion practice? Ann Behav Med. 2004;27:3–12. doi: 10.1207/s15324796abm2701_2. [DOI] [PubMed] [Google Scholar]
- 40.Campbell MK, McLerran D, Turner-McGrievy G, et al. Mediation of adult fruit and vegetable consumption in the National 5 A Day for Better Health community studies. Ann Behav Med. 2008;35:49–60. doi: 10.1007/s12160-007-9002-y. [DOI] [PubMed] [Google Scholar]
- 41.Fuemmeler BF, Masse LC, Yaroch AL, et al. Psychosocial mediation of fruit and vegetable consumption in the body and soul effectiveness trial. Health Psychol. 2006;25:474–83. doi: 10.1037/0278-6133.25.4.474. [DOI] [PubMed] [Google Scholar]
- 42.Langenberg P, Ballesteros M, Feldman R, Damron D, Anliker J, Havas S. Psychosocial factors and intervention-associated changes in those factors as correlates of change in fruit and vegetable consumption in the Maryland WIC 5 A Day Promotion Program. Ann Behav Med. 2000;22:307–15. doi: 10.1007/BF02895667. [DOI] [PubMed] [Google Scholar]
- 43.Anderson ES, Winett RA, Wojcik JR. Self-regulation, self-efficacy, outcome expectations, and social support: social cognitive theory and nutrition behavior. Ann Behav Med. 2007;34:304–12. doi: 10.1007/BF02874555. [DOI] [PubMed] [Google Scholar]
- 44.Demark-Wahnefried W, Clipp EC, McBride C, et al. Design of FRESH START: a randomized trial of exercise and diet among cancer survivors. Med Sci Sports Exerc. 2003;35:415–24. doi: 10.1249/01.MSS.0000053704.28156.0F. [DOI] [PubMed] [Google Scholar]
- 45.Demark-Wahnefried W. Print-to-practice: Designing tailored print materials to improve cancer survivors’ dietary and exercise practices in the FRESH START trial. Nutr Today. 2007;42:131–8. doi: 10.1097/01.NT.0000277790.03666.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Macri JM, Downs SM, Demark-Wahnefried W, Snyder DC, Lobach DF. A simple, flexible and scalable approach for generating tailored questionnaires and health education messages. Comput Inform Nurs. 2005;23:316–21. doi: 10.1097/00024665-200511000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Watson MM, Law M, dos Santos M, Greer S, Baruch J, Bliss J. The Mini-MAC: Further development of the Mental Adjustment to Cancer scale. J Psychosoc Oncol. 1994;12:33–45. [Google Scholar]
- 48.Prochaska JO. Treating entire populations for behavior risks for cancer. Cancer J. 2001;7:360–8. [PubMed] [Google Scholar]
- 49.Subar AF, Thompson FE, Kipnis V, et al. Comparative validation of the Block, Willett, and National Cancer Institute food frequency questionnaires: The Eating at America’s Table Study. Am J Epidemiol. 2001;154:1089–99. doi: 10.1093/aje/154.12.1089. [DOI] [PubMed] [Google Scholar]
- 50.Thompson FE, Subar AF, Brown CC, et al. Cognitive research enhances accuracy of food frequency questionnaire reports: Results of an experimental validation study. J Am Diet Assoc. 2002;102:212–25. doi: 10.1016/s0002-8223(02)90050-7. [DOI] [PubMed] [Google Scholar]
- 51.Blair SN, Haskell WL, Ho P, et al. Assessment of habitual physical activity by a seven-day recall in a community survey and controlled experiments. Am J Epidemiol. 1985;122:794–804. doi: 10.1093/oxfordjournals.aje.a114163. [DOI] [PubMed] [Google Scholar]
- 52.Pereira MA, FitzerGerald SJ, Gregg EW, et al. A collection of Physical Activity Questionnaires for health-related research. Med Sci Sports Exerc. 1997;29:S1–205. [PubMed] [Google Scholar]
- 53.Sallis JF, Haskell WL, Wood PD, et al. Physical activity assessment methodology in the Five-City Project. Am J Epidemiol. 1985;121:91–106. doi: 10.1093/oxfordjournals.aje.a113987. [DOI] [PubMed] [Google Scholar]
- 54.Campbell MK, Reynolds KD, Havas S, et al. Stages of change for increasing fruit and vegetable consumption among adults and young adults participating in the national 5-a-Day for Better Health community studies. Health Educ Behav. 1999;26:513–34. doi: 10.1177/109019819902600409. [DOI] [PubMed] [Google Scholar]
- 55.Krebs-Smith SM, Heimendinger J, Patterson BH, Subar AF, Kessler R, Pivonka E. Psychosocial factors associated with fruit and vegetable consumption. Am J Health Promot. 1995;10:98–104. doi: 10.4278/0890-1171-10.2.98. [DOI] [PubMed] [Google Scholar]
- 56.Campbell MK, Demark-Wahnefried W, Symons M, et al. Fruit and vegetable consumption and prevention of cancer: the Black Churches United for Better Health project. Am J Public Health. 1999;89:1390–6. doi: 10.2105/ajph.89.9.1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Campbell MK, Symons M, Demark-Wahnefried W, et al. Stages of change and psychosocial correlates of fruit and vegetable consumption among rural African-American church members. Am J Health Promot. 1998;12:185–91. doi: 10.4278/0890-1171-12.3.185. [DOI] [PubMed] [Google Scholar]
- 58.Tabachnick BG, Fidell LS. Using Multivariate Statistics. 4th ed Allyn and Bacon; Needham Heights, MA: 2001. [Google Scholar]
- 59.Shrout PE, Bolger N. Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychological Methods. 2002;7:422–45. [PubMed] [Google Scholar]
- 60.Preacher KJ, Hayes AF. SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behav Res Methods Instrum Comput. 2004;36:717–31. doi: 10.3758/bf03206553. [DOI] [PubMed] [Google Scholar]
- 61.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–82. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 62.Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Sociol Methodol. 1982;13:290–312. [Google Scholar]
- 63.Briggs AH, Wonderling DE, Mooney CZ. Pulling cost-effectiveness analysis up by its bootstraps: a non-parametric approach to confidence interval estimation. Health Econ. 1997;6:327–40. doi: 10.1002/(sici)1099-1050(199707)6:4<327::aid-hec282>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- 64.Effron B. Better bootstrap confidence intervals. J Am Stat Assoc. 1987;82:171–200. [Google Scholar]
- 65.Preacher KJ, Rucker DD, Hayes AF. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivar Behav Res. 2007;42:185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- 66.Alfano CM, Day JM, Katz ML, et al. Exercise and dietary change after diagnosis and cancer-related symptoms in long-term survivors of breast cancer: CALGB 79804. Psychooncology. 2009;18:128–33. doi: 10.1002/pon.1378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Demark-Wahnefried W, Peterson B, McBride C, Lipkus I, Clipp E. Current health behaviors and readiness to pursue life-style changes among men and women diagnosed with early stage prostate and breast carcinomas. Cancer. 2000;88:674–84. [PubMed] [Google Scholar]
- 68.Gritz ER, Fingeret MC, Vidrine DJ, Lazev AB, Mehta NV, Reece GP. Successes and failures of the teachable moment: Smoking cessation in cancer patients. Cancer. 2006;106:17–27. doi: 10.1002/cncr.21598. [DOI] [PubMed] [Google Scholar]
- 69.Dishman RK, Motl RW, Saunders R, et al. Self-efficacy partially mediates the effect of a school-based physical-activity intervention among adolescent girls. Prev Med. 2004;38:628–36. doi: 10.1016/j.ypmed.2003.12.007. [DOI] [PubMed] [Google Scholar]
- 70.Lewis BA, Forsyth LH, Pinto BM, Bock BC, Roberts M, Marcus BH. Psychosocial mediators of physical activity in a randomized controlled intervention trial. J Sport Exerc Psychol. 2006;28:193–204. [Google Scholar]
- 71.Miller YD, Trost SG, Brown WJ. Mediators of physical activity behavior change among women with young children. Am J Prev Med. 2002;23:98–103. doi: 10.1016/s0749-3797(02)00484-1. [DOI] [PubMed] [Google Scholar]
- 72.Pinto BM, Lynn H, Marcus BH, DePue J, Goldstein MG. Physician-based activity counseling: intervention effects on mediators of motivational readiness for physical activity. Ann Behav Med. 2001;23:2–10. doi: 10.1207/S15324796ABM2301_2. [DOI] [PubMed] [Google Scholar]
- 73.Napolitano MA, Papandonatos GD, Lewis BA, et al. Mediators of physical activity behavior change: A multivariate approach. Health Psychol. 2008;27:409–18. doi: 10.1037/0278-6133.27.4.409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Bock BC, Marcus BH, Pinto BM, Forsyth LH. Maintenance of physical activity following an individualized motivationally tailored intervention. Ann Behav Med. 2001;23:79–87. doi: 10.1207/S15324796ABM2302_2. [DOI] [PubMed] [Google Scholar]
- 75.Williams DM, Lewis BA, Dunsiger S, et al. Comparing psychosocial predictors of physical activity adoption and maintenance. Ann Behav Med. 2008;36:186–94. doi: 10.1007/s12160-008-9054-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Collins LM, Murphy SA, Nair VN, Strecher VJ. A strategy for optimizing and evaluating behavioral interventions. Ann Behav Med. 2005;30:65–73. doi: 10.1207/s15324796abm3001_8. [DOI] [PubMed] [Google Scholar]
- 77.Bandura A. Guide for creating self-efficacy scales. In: Pajares F, Urdan T, editors. Self-efficacy Beliefs of Adolescents. Information Age Publishing; Greenwich, CT: 2006. pp. 307–37. [Google Scholar]