Abstract
Background:
“Caregiver Burden” is actually an expression addressing the adverse consequences of the care provided to the patients’ with dementia. Review of the previous studies reveals a higher rate of depression and anxiety among the caregivers as compared to the general population. This study has been designed to evaluate the caregiver burden and then the factors influencing it among caregivers of patients with dementia in Iran.
Methods:
In this cross-sectional study, 153 patients and their caregivers registered in the Memory Clinic in Roozbeh Hospital and Iranian Alzheimer Association (IAA) were included. Data collection scales were Iranian Version of Caregiver Burden, Global Deterioration scale and Barthel index. Multiple linear regression model was applied to determine the factors influencing the caregiver burden.
Results:
Out of the 153 patients, 90 were male. The mean age calculated for the patients and the caregivers was 77.1 and 53, respectively. The mean of caregiver burden was 55.2. Three variables, gender (P<0.01), education of the patient (P<0.005 for illiterate patients), and the patient's dependence on the caregiver for his/her daily tasks (P<0.000)) were correlated with a high level of burden on the caregiver. The recommended model explains 0.664% of the variance of the outcome variable.
Conclusion:
Presence of either moderate or higher levels of burden (58-116) in more than 50% of the caregivers of these patients’ highlights the need for more attention from health policy makers in Iran. Promoting the level of caregivers’ quality of life along with enabling the patients in performing their daily tasks in order to reduce the imposed burden on caregivers’ is recommended.
Keywords: Dementia, caregivers, burden, family caregivers, elderly people, caregiver burden, Iran
INTRODUCTION
Dementia lies amongst the most important health issues as a result of its high prevalence rate, its complicated consequences (e.g., disturbance of memory, speech, and daily routines), extremely high care expenses, and physical and psychological burden of the families[1–3] resulting from the chronic and long course of the disorder.[1,4] “Caregiver Burden” is actually an expression addressing the adverse consequences of the care provided to the patient suffering from dementia; these consequences might be physical, psychological, or financial in nature.[5] “Caregiver” refers to the family members and the close family who are considered the main source or in many instances the only source of care to this group of patients.[6,7] In other words, caregivers are the individuals who encounter limitations and problems in fulfilling their own individual, social, and occupational roles as they need to dedicate almost 3/4th of their time to a patient suffering from dementia.[7,8] Although “care” cannot be considered as a new entity, there have been changes in the number of individuals involved in care, the length of time allocated to care, and the nature of the roles of the individuals in care during the past half-century.[6] Recent studies have revealed significant differences between the burdens resulting from provision of care to the demented elderly as compared to the burdens caused by the pressure of the care provided to the elderly family members who are only suffering from physical ailments. These studies have been concordant with the results of the previous studies pointing out that as compared to other family care issues, in case of patients with dementia, there is need for allocation of longer times to the care of the patient with the expense of spending of leisure and free time; a fact that eventually results in spending shorter time with other family members also the presence of behavioral and Psychiatric symptoms of dementia (BPSD) may induce more stress than medical problems.[8] While new medical and care technologies have resulted in an increase in life expectancy, mean age of the population, acute ailments give their way to chronic disorders complicated by their own consequences, in certain cases the care will last for years and even more than one decade. It is evident that the caregivers will subject to increasing distresses as they have to fulfill complicated responsibilities.[6] Review of the previous studies reveals a higher rate of depression and anxiety among the caregivers as compared to the general population.[1,6,8] Meanwhile, the family members of the patients with dementia have reported a lower general health and life satisfaction level as compared to general population.[8,9] Overall, the burden caused by the care can be considered as a combination of the physical and psychological distresses and the financial constricts due to decrease of the working hours and the urge to leave the profession in order to provide the care.[10,11] These eventually contribute to negative impacts on health and occupational status as well as financial security of the caregivers. Thus, the impacts of dementia not only influence the patients but also their family members.[1,9] One should also consider that caregivers are not only responsible to provide timely and appropriate care, but also have to respond to the demands of other family members.[9] As a result of the quality of the care required for patients with dementia and the responsibility of the caregivers to meet the demands of other family members, this group are distinguished from general population and are considered as a highly vulnerable group.[12] Evidence shows that dementia alters the family interactions and increases the likelihood of mental disorders among family members.[6,9]
Meanwhile, the role of caregivers in the well being and results of care and treatment of the patients and the physical and psychological dependence of the patients on the caregivers highlights the important role of the caregivers.[1,13] As a result of the increase of the disorder and the care costs, the level of the dependence of the patient on the caregiver is also increasing.[14,15] The burden of the family members of patients with dementia is a very important issue which has not been taken into consideration in Iran. Considering the population structure in Iran where almost 31 million individuals are either in their middle age who will constitute the elderly population in the forthcoming two decades on one hand,[16] and the higher rates of dementia in old age on the other hand,[17] one can conclude that the prevalence of the disorder and its adverse effects will have an increasing trend for the next two decades. It has been recently revealed that some of the demographic characteristics of the patient and the caregiver can influence the level of the burden the caregiver experiences.
Caregivers’ burden may be higher in our society as the strong emotional bonds between the families and their elderly parents don’t let them leave the old patients in the institutional homes. In our culture, taking care of the elderly has been one of the major duties of the families; therefore, they still resist to let the elderly live in institutional homes. However, as a result of the increasing urbanization, large-scale migration, employment of both men and women, smaller size of families, and longer life expectancy of old people in the recent decades, a major change has been occurring in the public and governmental attitude toward this issue. This phenomenon is more apparent in metropolitan cities such as Tehran. In the cities with smaller population and more traditional and religious structure, there is still a negative attitude toward this issue. One study has shown that the proportion of elderly in these centers is very small in comparison to the total aged population of the country; less than 0.1% in 1986 and less than 0.2% in 1996 were living in institutional homes while 0.56% of them were 90 to 94 years of age.[18]
This study has been designed to evaluate the level of burden and then the influencing factors on imposed burden on the caregivers of patients with dementia in Iran. The results of the present study can be helpful in designing interventions with the goal of decreasing the burden of the caregivers of patients with dementia.
METHODS
This is a cross-sectional (descriptive- analytic) study conducted in Memory Clinic in Roozbeh Hospital affiliated to Tehran University of Medical Sciences and Iranian Alzheimer Association (IAA) for six months in 2009.
Study sample
A total of 153 patients and their caregivers registered in the Iranian Association of Alzheimer were included in this study. Inclusion criteria of the study dictated that the patient and the caregiver had a close family relationship, the minimum of the daily time dedicated to care was six hours. Cases where the caregiver was suffering from any cognitive disorder (e.g., dementia) were excluded. In the events where the patient had more than one caregiver or the caregiver who dedicated more time to care as compared to peers was considered as the main caregiver.
Data collection scales
Data collection scales included the following:
Iranian Version of Caregiver Burden; a 29-item questionnaire standardized for patients and caregivers considering the cultural backgrounds. Content validity and reliability of the questionnaire (in both domains of repeatability and internal consistency) have been evaluated in Iran. Relevancy, clarity, and comprehensiveness indexes of the questionnaire have been reported to be 98.6%, 99.3%, and 100%, respectively. Intraclass correlation coefficient and chronbach's alpha co-efficient of the questionnaire have been reported as 97 and 94%, respectively.[19] The caregiver burden was measured by this tool.
Global Deterioration Scale (GDS); a scale which breaks down dementia into seven stages including dementia with no cognitive disorder, very mild cognitive disorder, mild cognitive disorder, moderate cognitive disorder, almost severe cognitive disorder, severe cognitive disorder, and very severe cognitive disorder was utilized to identify the severity of the disorder in each patient.[20]
Barthel index; was utilized to measure the degree of the patient's dependence on the caregiver for daily tasks (10 tasks). Persian version of this questionnaire was provided with supervision of neurologist expert in dementia research and English language professionals through backward forward translation. This questionnaire has proved to have a high degree of validity and reliability.[21]
-
Demographic data questionnaire; to gather the date regarding age, gender, marital status, education, relationship with the patient, number of the family members of the caregiver, occupational status, economic status, co- inhabiting with the patient versus living separately, number of caregivers, and ethnicity of the caregiver. Meanwhile, age, gender, marital status, education, any medical co-morbidity, number of children residential status of the patient and insurance status of the patient were also registered. We used the average of two single questions (with likert scale) in order to measure caregiver's attitude toward his/her quality of life and health status.
Data gathering was conducted through caregivers of patient GDS scale was completed by two experienced neurologists, while the other scales were completed through interview of the caregivers by interviewers trained by professional researchers.
Data analysis
Where the pre-assumptions of parametric tests including normal distribution of the variables were met, T- test, Analysis of Variance (ANOVA), and correlation tests were used to determine the correlation of the different factors with the pressure on the caregivers. Principal Component Analysis was also conducted to determine the socio-economic status of the caregivers. As the criteria for linear regression were met, multiple linear regression model was applied in order to determine the factors influencing the caregiver burden. The independent variables, stage of the disorder, education, gender, age, level of patient's dependence on the caregiver for daily tasks, the insurance status of the patient from patients’ side were considered in the regression model, while education, age, state of family relationship with the patient, number of the caregivers for the patient, the mean score for quality of life of the caregiver, and caregiver's health status from his/her own perspective were taken into consideration from the caregiver's side.
RESULTS
Respondent characteristics
Out of the 153 patients included in the study, 90 were female and 63 were male. The mean (SD) age calculated for the patients and the caregivers was 77.1 ± 7.4 and 53 ± 13, respectively. The median for the number of caregivers and the stage of the disorder were 2 and 5, respectively. The mean (SD) for the stage of the disorder, the score of the severity of the disorder, the degree of patient's dependence on the caregiver for daily tasks and the caregiver's pressure was calculated to be 5.39 ± 1.1, 65.26 ± 30, and 55.24 ± 23.713. [Table 1] depicts the characteristics of the participants together with a summary of the main variables of the study.
Table 1.
Distribution of gender, age, marital status, socio-economic status, relationship of the caregiver and the patient; occupational status of the caregiver, and the number of caregiver per patient (n=153)
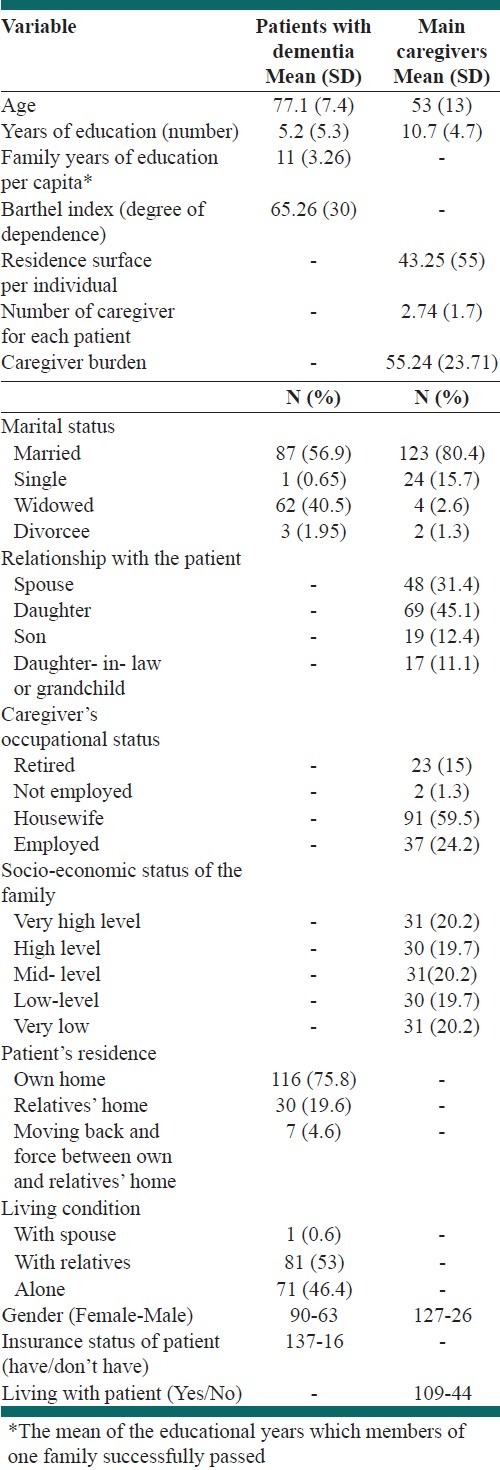
As Table 1 illustrates that 24.2% of the caregivers were employed, while the unemployed caregivers included 3.3%. Ninety percent of the patients had an insurance coverage either from Social Insurance or Medical services insurance. Only 10% of the patients had no medical insurance coverage. Based on the fact that the Iranian Version of Caregiver Burden includes 29 questions and the score of each question might range from 0 to 4, the maximum score of the scale is 116. The scores ranged from 0 to 112 in this study. Meanwhile, the mean score of the scores obtained from the same questionnaire was 55.24. It is noteworthy that the burden on the main caregiver of the patient has been reported to be either at a moderate or high level for 50% of the caregivers (ranging between 86 and 116). Since the process of data collection was performed through interview by specialists and trained interviewers, there was not any issue of missed data.
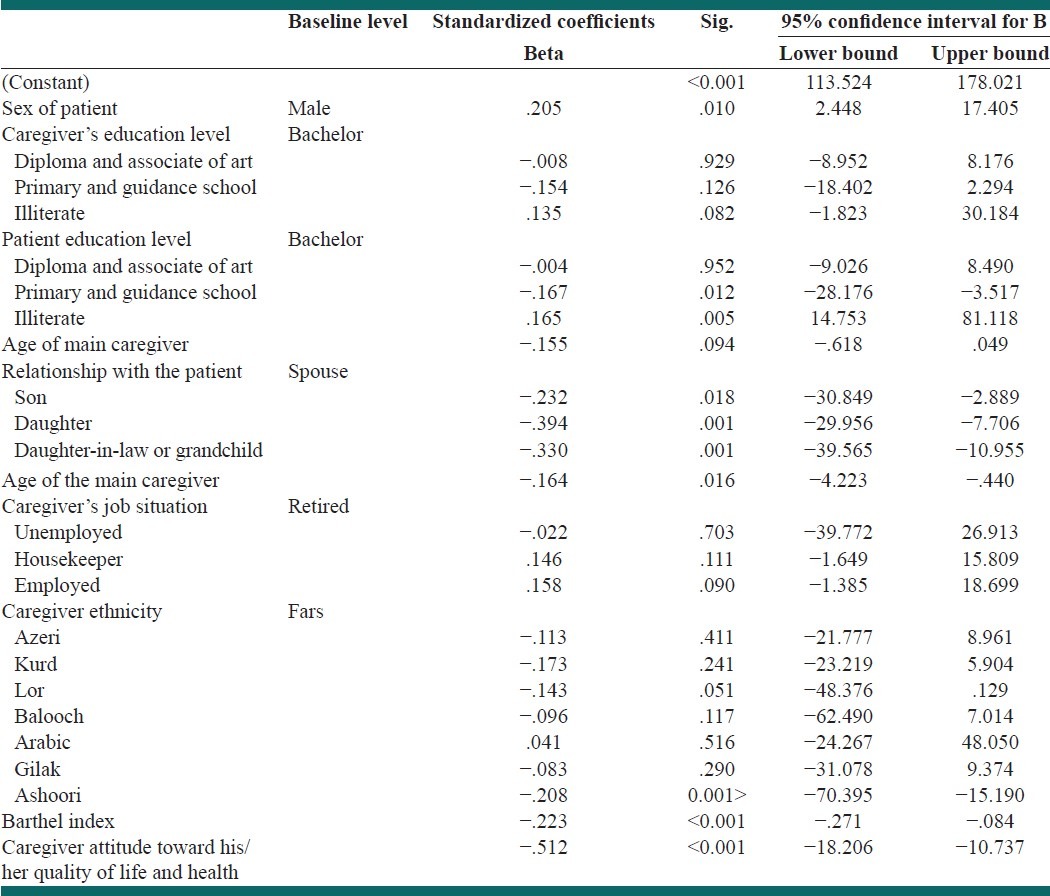
From all the remaining variables in the final regression model, three variables were correlated with a high level of burden on the caregiver; these three variables included gender (P<0.01), education of the patient (P<0.005 for illiterate patients), and patient's dependence on the caregiver for his/her daily tasks (P<0.000). On other hand, certain variables were correlated with statistically significant lower levels of burden on the caregiver. These included patient's literacy (P<0.012 for patients with either primary or junior high school level of education), being in a first degree relationship with the patient (P<0.018 for sons, P<0.001 for daughters, P<0.001 for daughter-in- laws and grandchildren), number of caregivers (P<0.016), ethnicity of the caregiver (P<0.003 for Ashuries, and the mean score of the caregiver's self perception of own quality of life and health status (P<0.000). It is noteworthy that the recommended model explains 0.664% of the variance of the outcome variable (burden of the caregiver) (R2=0.664) [Table 2].
Table 2.
Evaluation of the factors influencing the level of the burden of the caregivers of patients with dementia using a linear regression model
DISCUSSION
Considering the high prevalence rate of dementia among the elderly population and its impact on activity daily living, functional capabilities, and patient behavior and also its adverse consequences together with the financial distress due to high cost of treatment caused by the severity and chronicity of the disorder, we can conclude that further to the fact that patients need support for their daily activities, the disorder has significant impact on both patients and their caregivers. Due to its high impact, dementia is considered amongst major health issues in the community.[1,4] Multiple behavioral and mental disturbances caused by the disorder on one hand and the distress on the family on the other hand reflect the importance of caregiver burden in dementia. So there are not only the patients who are influenced by the disorder; family members and the caregivers also do suffer from the implications of dementia.
It seems factors such as social and family status of the caregiver, his/her education level, and the level of satisfaction regarding the caregiver role (which we did not assess some of them) should be considered as very important factors which play a role in the level of the distress on the caregiver. As a result of the multifaceted nature of the phenomenon, different caregivers do not experience the same level of distress in similar situations.[5] For sure, a better understanding of the consequences of the disorder and reduction of the adverse implications will only be achieved through understanding of the factors influencing the involved factors.
Socio-demographic factors of the patient
The only socio-demographic factors of the patients which were found to have a role in the level of the caregiver burden in this study included gender and education level. The mean score of the burden reported by the caregivers of the female patients has been rated to be ten degrees higher as compared to the caregivers of the of male patients. This finding has not received much attention in previous studies. While the mean score of the burden of the caregivers of the illiterate patients has been 48 scores more than the patients with a bachelor or higher university degree, the mean score of the burden reported by the caregivers of the patients with either primary or junior high school has been 15.8 scores higher as compared to the caregivers of the second group. Although the caregiver burden had a statistically significant correlation (P<0.001) with patient's insurance status, the bi-variant test in the final regression model failed to prove such a correlation.
Socio-demographic factors of the caregiver
Among the socio-demographic factors considered in this study, the family relationship of the caregiver and the patient and the number and the ethnicity of caregiver(s) have been found to have a statistically significant correlation with the burden felt by the caregiver(s). Among the family members, spouses of the patients were reported to be suffering from the highest degree of burden. The higher level of burden among them has been reported to be statistically significant. The mean burden score of the daughters, sons, daughter-in-laws or grandchildren of the patients have been 16.9, 18.8, and 25.3 scores lower than the spouses, respectively. A study conducted in Turkey has also highlighted a higher burden among the spouses of the patients.[12] Taking the physical health status and the age of the spouses into consideration, one might conclude that due to their higher age, their physical and mental capacity might have been deteriorated as compared to other family members. Thus, this can be counted as a logical finding of the present study. The other explanation for this phenomenon is the quality of family interaction and its related factors. As a very common practice, the spouse lives with the patient and has to spend a longer time for the care. Consequently, they are at a higher risk for an increase in physical and mental health issues. On the other hand, it is most likely that the children of the patients do not reside with him/her (as they have their own family, etc).
The lack of significant effect of the gender of the caregiver in this study is seems to be concordant with the finding of the other previous studies.[7,12,22] It must be noted that at least in Iran, women take more responsibility of the personal care of the patients (taking to shower, toilet, etc) as compared to men.
Taking the multicultural infrastructure of the Iranian community and presence of different ethnic groups in this country into consideration, ethnicity of the caregiver was amongst the factors which were evaluated for its influence on the level of the burden of the caregiver. As it was found that ethnicity of the caregiver caused a statistically significant role in the level of burden of the caregiver, it was taken into consideration in the final regression model. The lowest level of burden belongs to Ashuri ethnicity. This is the group with a statistically significant difference in their level of burden. No other ethnicity has been found to be an influential factor in decreasing the level of burden. In this study, we found 2.3 unit decrease in caregiver burden for one increase in the caregiver number. This finding could be considered as a reasonable one.
Patient's clinical factors
The stage of the disorder should be mentioned as another factor considered in this study. The lack of statistically significant role of this factor on the level of the burden of the caregiver might be explained by the results of some previous studies which have pointed out the fact that some caregivers do adopt better coping styles as the time passes and the patient steps into the more advanced stage of the disorder.[23,24] On the other hand, there are caregivers who experience a higher pressure as the patient goes through the different stages of the disorder.[25,26] Meanwhile, as the disorder turns to be more advanced, patient's capacity to conduct physical activities decline, a fact that results in decreased behavioral disturbance and psychological issues in the patient.
Patient's dependence on the caregiver for daily tasks
One of the factors considered in this study is the level of the dependence of the patient to conduct daily tasks which was measured by means of Barthel index. The level of dependence of the patient to the caregiver can be considered as one of the factors influencing the level of burden perceived by the caregiver (P<0.001). As the score of this questionnaire decreases, the level of the capability of the patient to perform daily tasks declines and the burden of the caregiver increases due to the higher pressure caused by his/her more involvement in supporting the patient for daily tasks.
Limitations
Due to the special psychological and physical conditions of the patients and their caregivers, random sampling could not be considered for this study. This might be one of the main limitations of the study which might decrease the possibility of generalization of the result to the whole community.
CONCLUSION
The demographic change of Iran population together with the increase in elderly ratio reflects the importance of the increase in the rate of dementia prevalence in the future years and its adverse consequences on Iranian families who are supposed to care an old patient with dementia.
Along with the aforementioned factors, the culture of Iranian families, their attitude toward their old parents, and the lack of appropriate resources in the nursing homes in Iran, highlights the impacts of dementia on caregivers. Presence of either moderate or higher levels of burden (58-116) in more than 50% of the caregivers of the patients with dementia together with the intense financial and psychological distress highlights the need for more attention from health policy makers in Iran and other developing countries, while dementia should be considered among the mental health priorities. Promoting the level of caregiver's quality of life along with enabling the patients in performing daily tasks in order to reducing imposed burden on caregivers is recommended.
ACKNOWLEDGEMENT
The authors appreciate the cooperation of the staff members of the Iranian Alzheimer Association (IAA). This project has been a part of the dissertation of Ibrahim Abdollahpour for M.Sc in epidemiology, with the dissertation number of 88-03-27-9165.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Alzheimer's disease facts and figures Alzheimer's Association. Chicago: Alzheimer's Association; 2010. pp. 158–94. [DOI] [PubMed] [Google Scholar]
- 2.Garre-Olmo J, Hernandez-Ferrandiz M, Lozano-Gallego M, Vilalta-Franch J, Turón-Estrada A, Cruz-Reina MM, et al. Burden and quality of life in carers of patients with Alzheimer type dementia. Rev Neurol. 2000;31:522–7. [PubMed] [Google Scholar]
- 3.Association AS. Alzheimer's disease facts and figures Alzheimer's Association. Chicago: Alzheimer's Association; 2010. pp. 158–94. [DOI] [PubMed] [Google Scholar]
- 4.Conde-Sala J, Garre-Olmo J, Turró-Garriga O, López-Pousa S S, Vilalta-Franch J. Factors related to perceived quality of life in patients with Alzheimer's disease: The patient's perception compared with that of caregivers. Int J Geriatr Psychiatry. 2009;24:585–94. doi: 10.1002/gps.2161. [DOI] [PubMed] [Google Scholar]
- 5.Allegri RF, Sarasola D, Serrano CM, Taragano FE, Arizaga RL, Butman J, et al. Neuropsychiatric symptoms as a predictor of caregiver burden in Alzheimer's disease. Neuropsychiatr Dis Treat. 2006;2:105–10. [PMC free article] [PubMed] [Google Scholar]
- 6.Schulz R, Martire LM. Family caregiving of persons with dementia: Prevalence, health effects, and support strategies. Am J Geriatr Psychiatry. 2004;12:240–9. [PubMed] [Google Scholar]
- 7.Serrano-Aguilar PG, Lopez-Bastida J, Yanes-Lopez V. Impact on health-related quality of life and perceived burden of informal caregivers of individuals with Alzheimer's disease. Neuroepidemiology. 2006;27:136–42. doi: 10.1159/000095760. [DOI] [PubMed] [Google Scholar]
- 8.Papastavrou E, Kalokerinou A, Papacostas SS, Tsangari H, Sourtzi P. Caring for a relative with dementia: Family caregiver burden. J Adv Nurs. 2007;58:446–57. doi: 10.1111/j.1365-2648.2007.04250.x. [DOI] [PubMed] [Google Scholar]
- 9.Salguero RH, Kohn R, Salguero LF, Marotta CA. Caregivers of persons with Alzheimer's Disease: Cultural differences in perceived caregiver burden in Guatemala and Rhode Island. J Cross Cult Gerontol. 1998;13:229–40. doi: 10.1023/a:1006534521253. [DOI] [PubMed] [Google Scholar]
- 10.Biegel D, Sales E, Schulz R. Family Caregiving in Chronic Illness. Heart Disease, Cancer, Stroke, Alzheimer's disease, and Chronic Mental Illness. Newbury Park, CA: Sage Publications; 1991. [Google Scholar]
- 11.Schulz R. Handbook on dementia caregiving: Evidence-based interventions in family caregiving. Berlin, Heidelberg: Springer Publishing Company; 2000. [Google Scholar]
- 12.Karlikaya G, Yukse G, Varlibas F, Tireli H. Caregiver burden in dementia: A study in the Turkish population. Internet J Neurol. 2005;4:12–26. [Google Scholar]
- 13.Chan TS, Lam LC, Chiu HF. Validation of the Chinese version of the Zarit Burden Interview. Hong Kong J Psychiatry. 2005;15:9–13. [Google Scholar]
- 14.Ernst RL, Hay JW. The US economic and social costs of Alzheimer's disease revisited. Am J Public Health. 1994;84:1261–4. doi: 10.2105/ajph.84.8.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rice DP, Fox PJ, Max W, Webber PA, Lindeman DA, Hauck WW, et al. The economic burden of Alzheimer's disease care. Health Aff (Millwood) 1993;12:164–76. doi: 10.1377/hlthaff.12.2.164. [DOI] [PubMed] [Google Scholar]
- 16.Iran Manual Statistical 2007. [Last accessed on 2009 Nov 23]. Available from: http://www.sci.org.ir/portal/faces/public/census85/
- 17.Wimo A, Winblad B, Aguero-Torres H, von Strauss E. The magnitude of dementia occurrence in the world. Alzheimer Dis Assoc Disord. 2003;17:63–7. doi: 10.1097/00002093-200304000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Noroozian M. The Iranian Old Population: A Growing Health Concern. IPA Bull. 2009;30:8–9. [Google Scholar]
- 19.Abdollahpour I, Nedjat S, Noroozian M, Golestan B, Majdzadeh R. Development of a Caregiver Burden Questionnaire for the Patients with Dementia in Iran. Int J Prev Med. 2010;1:233–41. [PMC free article] [PubMed] [Google Scholar]
- 20.Reisberg B, Ferris SH, de Leon MJ, Crook T. The Global Deterioration Scale for assessment of primary degenerative dementia. Am J Psychiatry. 1982;139:1136–9. doi: 10.1176/ajp.139.9.1136. [DOI] [PubMed] [Google Scholar]
- 21.Collin C, Wade DT, Davies S, Horne V. The Barthel ADL Index: A reliability study. Int Disabil Stud. 1988;10:61–3. doi: 10.3109/09638288809164103. [DOI] [PubMed] [Google Scholar]
- 22.Annerstedt L, Elmstãhl S, Ingvad B, Samuelsson SM. Family caregiving in dementia–an analysis of the caregiver's burden and the “breaking-point” when home care becomes inadequate. Scand J Public Health. 2000;28:23–31. doi: 10.1177/140349480002800106. [DOI] [PubMed] [Google Scholar]
- 23.Johnson CL, Catalano DJ. A longitudinal study of family supports to impaired elderly. Gerontologist. 1983;23:612–8. doi: 10.1093/geront/23.6.612. [DOI] [PubMed] [Google Scholar]
- 24.Rabins PV, Fitting MD, Eastham J, Zabora J. Emotional adaptation over time in care-givers for chronically ill elderly people. Age Ageing. 1990;19:185–90. doi: 10.1093/ageing/19.3.185. [DOI] [PubMed] [Google Scholar]
- 25.Townsend A, Noelker L, Deimling G, Bass D. Longitudinal impact of interhousehold care-giving on adult children's mental health. Psychol Aging. 1989;4:393–401. doi: 10.1037//0882-7974.4.4.393. [DOI] [PubMed] [Google Scholar]
- 26.Zarit S, Zarit J. Dementia and the family: A stress management approach. Clin Psychol. 1986;39:103–5. [Google Scholar]


