Abstract
Primary vitreoretinal lymphoma is a high-grade in-traocular malignancy that presents as a vitritis with creamy subretinal lesions. In cases where the vitritis is dense, the characteristic subretinal lesions can be dif-ficult to see on clinical examination. Novel high-definition imaging techniques that allow for deeper penetration through opaque media could have diagnostic utility in such cases. The authors present a case of a patient who presented with a dense vitritis that precluded visualization of fundus details. Spectral-domain optical coherence tomography using high-definition raster imaging demonstrated subretinal deposits along with outer retinal atrophy. These findings were suggestive of primary vitreoretinal lymphoma and prompted diagnostic vitrectomy. Pathological examination of the vitreous specimen confirmed the diagnosis of primary vitreoretinal lymphoma.
INTRODUCTION
Primary vitreoretinal lymphoma (PVRL), also known as primary intraocular lymphoma, is a high-grade lymphoma that can masquerade as uveitis. The fundus features of this tumor can be characteristic, consisting of multifocal, creamy subretinal lesions with associated vitritis.1,2 Furthermore, fluorescein angiography typically shows absence of inflammatory leakage.1 These classic features can prompt further investigation with diagnostic vitrectomy. Molecular analysis, flow cytometry, and cytokine studies can be useful adjuncts to cytology for confirming the diagnosis.1,2 However, in some cases the presence of dense vitritis can obscure fundus features and potentially delay the diagnosis. We present a case of a patient presenting with dense vitritis precluding clear visualization of fundus details. High-definition (HD) spectral-domain optical coherence tomography (SD-OCT) helped prompt the decision to perform diagnostic vitrectomy, leading to the diagnosis of PVRL.
CASE REPORT
A 63-year-old man presented with a 3-month history of decreased vision and floaters in the left eye. On examination, best-corrected visual acuity was 20/20 in the right eye and 20/60 in the left eye. Intraocular pressures were normal in both eyes. The left eye demonstrated 1+ aqueous cells/flare, 1+ vitreous cells, and 3+ vitreous haze. The fundus details could not be clearly discerned (Fig. 1). The fluorescein angiography images were suboptimal secondary to vitreous haze, but no obvious leakage was appreciated. Serum angiotensin-converting enzyme, fluorescent treponemal antibody absorption, chest x-ray, purified protein derivative skin testing, and Lyme serology were negative.
Figure 1.
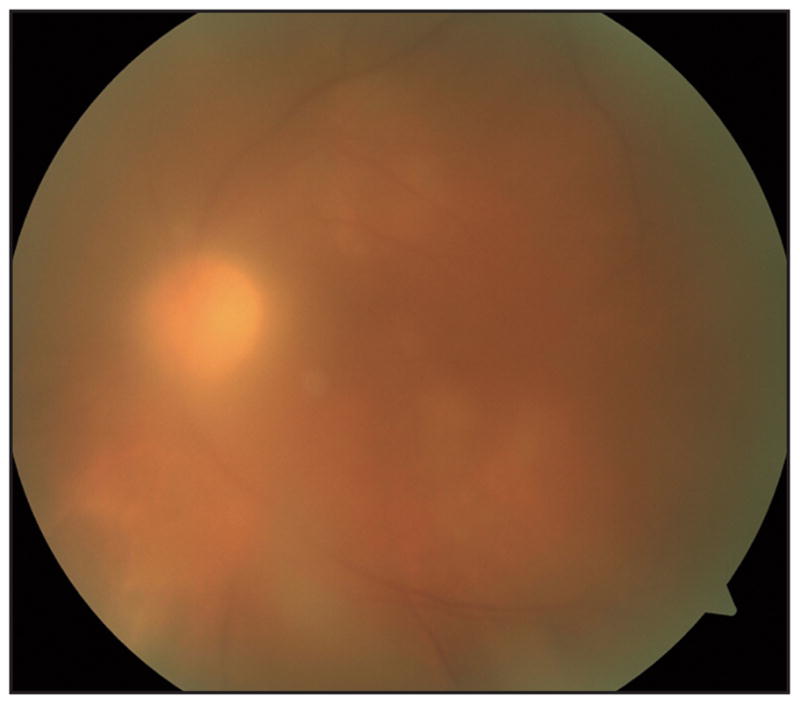
Color fundus image of patient at presentation. Fundus photography demonstrates dense vitritis, precluding clear visualization of fundus features.
SD-OCT was performed using the Cirrus HD-OCT (software version 5.1; Carl Zeiss Meditec, Dub-lin, CA). Although OCT images of the right eye were normal using the routine protocols, the left eye could only be imaged using the HD raster images. HD imaging of the left eye demonstrated subretinal deposits and outer retinal atrophy (Fig. 2). Because these features were suggestive of PVRL, diagnostic vitrectomy was performed. Cytological examination and molecular analysis of the vitrectomy sample confirmed PVRL. SD-OCT imaging performed after vitrectomy demonstrated focal outer retinal atrophy (Fig. 3).
Figure 2.
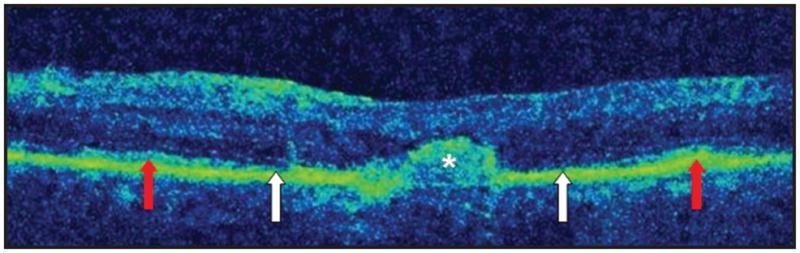
High-definition spectral-domain optical coherence tomography raster image of patient at presentation. Image shows subretinal deposit (asterisk) with an adjacent area of retinal pigment epithelium loss. Areas of outer retinal atrophy (white arrows) are shown, flanked by areas of relatively normal outer retina (red arrows).
Figure 3.
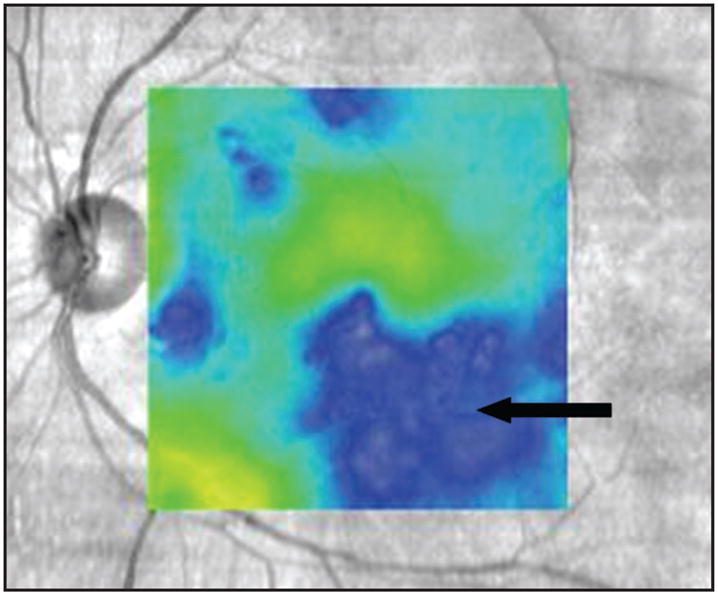
Spectral-domain imaging of patient following vitrectomy. Image obtained using macular cube protocol shows areas of macular atrophy (black arrow), consistent with the outer retinal atrophy observed on previous high-definition raster scans.
DISCUSSION
PVRL has characteristic fundus features that, when clearly visible, can prompt the decision to perform diag-nostic vitrectomy. When the vitritis is dense and precludes adequate visualization of fundus details, HD SD-OCT can be a useful diagnostic tool. The HD raster function on the Cirrus HD-OCT, which generates raster lines taken from 20 B-scans at a single location, allows for enhanced imaging of posterior pole anatomy.3 Despite inadequate visualization of fundus details in our case, the subretinal deposits and outer retinal atrophy on the HD SD-OCT raster image suggested PVRL and prompted further investigation with diagnostic vitrectomy. Because this tumor originates in the subretinal space,1 these SD-OCT features would be expected with PVRL.
Using time-domain OCT, investigators have described hyperreflective nodular subretinal lesions in patients with PVRL.4 In a recent report, Yeh and Wilson5 described the SD-OCT features of a patient with PVRL with clear visualization of fundus details. The subretinal lesions were seen to resolve on SD-OCT following treatment. Thus, in addition to aiding in the diagnosis of PVRL, SD-OCT can be useful for monitoring response to treatment. Our case highlights the importance of recognizing characteristic features of PVRL on SD-OCT such as subretinal deposits and outer retinal atrophy, as well as the use of HD raster images when fundus details are obscured, to aid in the diagnosis of PVRL.
Footnotes
The authors have no financial or proprietary interest in the materials presented herein.
References
- 1.Faia LJ, Chan CC. Primary intraocular lymphoma. Arch Pathol Lab Med. 2009;133:1228–1232. doi: 10.5858/133.8.1228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Coupland SE, Chan CC, Smith J. Pathophysiology of retinal lym-phoma. Ocul Immunol Inflamm. 2009;17:227–237. doi: 10.1080/09273940903168696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Manjunath V, Taha M, Fujimoto JG, et al. Choroidal thickness in normal eyes measured using Cirrus HD optical coherence tomography. Am J Ophthalmol. 2010;150:325–329. doi: 10.1016/j.ajo.2010.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fardeau C, Lee CP, Merle-Beral H, et al. Retinal fluorescein, indo-cyanine green angiography, and optic coherence tomography in non-Hodgkin primary intraocular lymphoma. Am J Ophthalmol. 2009;147:886–894. doi: 10.1016/j.ajo.2008.12.025. [DOI] [PubMed] [Google Scholar]
- 5.Yeh S, Wilson DJ. Combination intravitreal rituximab and methotrex-ate for massive subretinal lymphoma. Eye (Lond) 2010;24:1625–1627. doi: 10.1038/eye.2010.111. [DOI] [PubMed] [Google Scholar]


