Abstract
BACKGROUND:
Various methods have been applied to prevent maternal hypotension after spinal anesthesia for cesarean delivery. We compared the efficacy of three combinational methods in this regard in the current study.
METHODS:
In this randomized comparative trial, 150 candidates of elective cesarean delivery under spinal anesthesia were assigned to three groups: crystalloid preload and leg bandage, colloid preload and leg bandage, and ephedrine and leg bandage. Maternal hemodynamic changes during 60 minutes after spinal injection and neonatal condition were compared among the groups.
RESULTS:
The cumulative incidence of hypotension was 54%, 64%, and 36% in groups 1 to 3, respectively (p = 0.018). Spinal injection to hypotension interval was similar among the groups (p = 0.828). Heart rate in group 3 was significantly lower at the most time measures after anesthesia compared with the other two groups (p < 0.05 to <0.001). Regarding neonatal outcomes, the interval between the birth and the first breath was longer and the Apgar score at minute 1 was lower in group 3 compared with the other groups (p < 0.001 and 0.038, respectively) but it was not clinically important. Umbilical cord blood pH was similar among the three groups (p = 0.248).
CONCLUSIONS:
Among the three studied methods, administration of ephedrine plus bandage of the lower extremities was the most effective one in reducing the incidence of post-spinal hypotension. The groups were not clinically different concerning the effect of treatment on newborn health.
KEYWORDS: Hypotension, Spinal Anesthesia, Prophylaxis, Cesarean Delivery, Apgar Score
Hypotension is the most common complication following spinal anesthesia for cesarean delivery.1 In severe cases, it can have detrimental effects on both mother (unconsciousness and pulmonary aspiration) and neonate (hypoxia, acidosis, and neurological injury).2,3 Various preventive methods are currently used to prevent or minimize hypotension including left uterine displacement, prophylactic ephedrine, crystalloid or colloid preloading, and utilizing compression stocking onto the lower extremities.3 Administration of fluids before the administration of regional anesthesia can maintain adequate volume after the onset of sympathetic blockade. Administration of a large bolus of crystalloid may exacerbate the decrease in colloid osmotic pressure that occurs during the first 6-12 hours postpartum.4 Also, it redistributes to other body compartments. Some physicians prefer to give a synthetic colloid for this purpose. However, the solutions are expensive and may alter blood rheology and platelet function, which may result in increased blood lose. Leg wrapping prevents pooling of a major portion of the blood volume in the lower extremities, but the incidence of hypotension was reduced only a few percent by this method.4 However, according to systematic reviews and meta-analyses, no single method could effectively eliminate hypotension.3,5 In their systematic review, Morgan et al. introduced colloid preloading and leg wrapping as the most effective methods5 whereas Emmett et al. demonstrated that the prophylactic administration of crystalloid or colloid solutions, ephedrine, or leg wrapping could not reliably prevent hypotension.3 According to a meta-analysis by Lee et al., the efficacy of prophylactic ephedrine for the prevention of hypotension is poor at smaller doses, whereas at larger doses, the likelihood of causing hypertension is more than that of preventing hypotension with a minor decrease in umbilical arterial pH, as well. The authors, therefore, did not recommend the routine administration of prophylactic ephedrine in this regard.6
The degree of effectiveness of various preventive methods is controversial. There is no established ideal technique, and there is a lack of studies on neonatal outcome. Systematic reviews recommended future researches to be directed toward assessing a combination of the beneficial interventions, but few reports are available on the efficacy of combinational methods7–10 and more studies are needed in this regard. The present study was performed to compare the efficacy of three combinational methods on prevention of hypotension following spinal anesthesia in parturients undergoing elective cesarean delivery. Furthermore, this study evaluated the effect of these methods on neonatal outcome. The three combinational methods of the study were as follows: crystalloid preload plus leg bandage, colloid preload plus leg bandage and prophylactic ephedrine plus leg bandage.
Methods
This randomized, double blind clinical trial was conducted in two university hospitals (Beheshti and Shahid Sadoughi, in Isfahan and Yazd cities, respectively, Iran) from summer 2005 to spring 2009. After obtaining approval from the Ethics Committee of Isfahan University of Medical Sciences, we recruited singleton parturients with American Society of Anesthesiologists (ASA) physical status I or II who were scheduled for elective cesarean delivery under spinal anesthesia. Written informed consent was obtained from all parturients after full explanations of the goals and procedures of the study. Parturients without preexisting systemic disease or pregnancy-induced hypertension, preterm labor or signs of onset of labor, known fetal abnormalities, or without contraindications to spinal anesthesia were included in the study. Exclusion criteria were any significant history of maternal medical or obstetric illness and any fetal compromise within the current pregnancy. The patient and all staff involved in the study were blind to the protocol used. Power analysis showed that a sample size of 50 parturients per group would have 80% power at the 5% significance level to detect a difference of 30% in the incidence of hypotension among the groups. The sampling method was consecutive and eligible parturients were randomized into the following three groups using computer generated table of random numbers:11
Group 1: Ringer's lactate (RL) solution (15 ml/kg) was infused in 30 minutes before spinal injection. Also, mid thigh-high lower extremities bandage (Cobel co, Iran) was performed immediately after spinal injection.
Group 2: Prior to spinal injection, colloid solution (Hemaxel, 7 mg/kg) was infused in 30 minutes and mid thigh-high lower extremities bandage was performed immediately after spinal injection.
Group 3: Immediately after spinal injection, ephedrine (15 mg, IV, bolus) was infused in 45 seconds and also mid thigh-high bandage of lower extremities was done.
Spinal anesthesia was performed in all cases in sitting position in L3-L4 or L4-L5 spaces. The anesthesia was done with plain Marcaine (0.5%, 2.7 ml) (Curasan Co., Iran) and dextrose solution (50%, 0.3 ml) using spinal needle 25-gauge (pencil point, Braun, Melsungen, Germany). Then, the parturient was set to the left lateral position and after establishment of T4 block with pin prick test and confirmation of anesthesia, cesarean section was done. Oxytocin (20 IU in 1000 ml RL solution) was infused during one hour after delivery in order to retain the normal uteral tone. Each parturient received 10 ml/kg RL solution during anesthesia.
From entering into the operating room to discharging from the recovery room, all cases were monitored by non-invasive blood pressure monitoring, pulse oximetry, electrocardiography, and bleeding and urine volumes. If hypotension occurred, as defined by systolic blood pressure (SBP) below 90 mmHg or greater than 20% below baseline measures, rescue boluses of ephedrine (5 mg) were given each five minutes until hypotension resolved. The severity of nausea, as reported by parturient, was assessed by a nurse who was blind to the study on operation bed and also in recovery room by 100 mm Visual Analog Scale (VAS) and defined as severe if exceeded 40 mm. In case of vomiting or severe nausea, during operation atropine (0.5 mg, IV) and in recovery room metoclopramide (10 mg, IV) were administered. SBP, diastolic blood pressure (DBP), and heart rate (HR) of parturients were recorded at the admission to operating room (baseline), immediately after anesthesia (displayed as time 0), and minutes 3, 5, 15, 20, 25, 30, 35, and 60 after spinal injection. Time interval between the spinal injection and occurrence of hypotension, prolongation of hypotension (time that systolic blood pressure was less than 20 percent of baseline blood pressure), and the amount of rescue ephedrine administered were recorded. Following the delivery, the interval between neonatal birth and first breath after delivery, Apgar scores at min 1 and 5, umbilical cord blood pH (from umbilical artery isolated by proximal and distal clamp in a syringe washed with solution included 1000 unit heparin per milliliter), and neurologic and adaptive capacity score (NACS) at 15 minutes, 2 hours, and 24 hours after delivery were determined by a physician who was blind to the procedure.
The primary outcome of the study was defined as the incidence of hypotension. Secondary outcomes included changes in blood pressure and HR, the incidence of bradycardia (HR < 50 bpm), hypertension (SBP > 140 mm Hg or > 20% of the baseline values), spinal injection to hypotension interval, the prolongation of hypotension, amount of rescue ephedrine administered, nausea, vomiting, the interval between birth and first neonatal breath after delivery, umbilical cord pH, Apgar scores at min 1 and 5, and NACS. The incidence and timing of hypotension were analyzed using Kaplan-Meier survival analysis and comparison among groups was performed with the log-rank test. Survival time was defined as the time from spinal injection to the first episode of hypotension. GLM repeated measures with Tukey procedure for post-hoc pairwise comparisons was used to test sequential measurements of SBP and HR. ANOVA, with Tukey for post-hoc pairwise comparisons was used for comparing quantitative variables and chi-Square and Kruskal-Wallis tests were used for comparing qualitative and ordinal variables and continuous variables without normal distribution among the groups. Data were analyzed in SPSS software for windows (version 16) and values of p < 0.05 were considered statistically significant.
Figure 1.
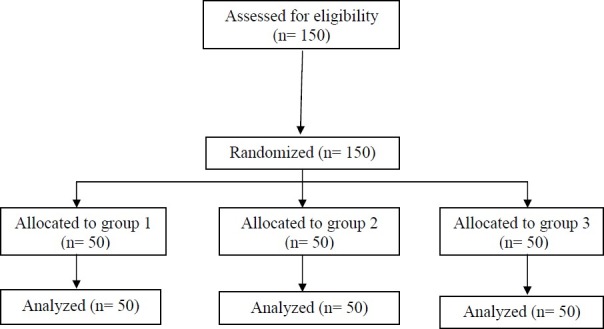
Flow diagram of enrolled study patients.
Results
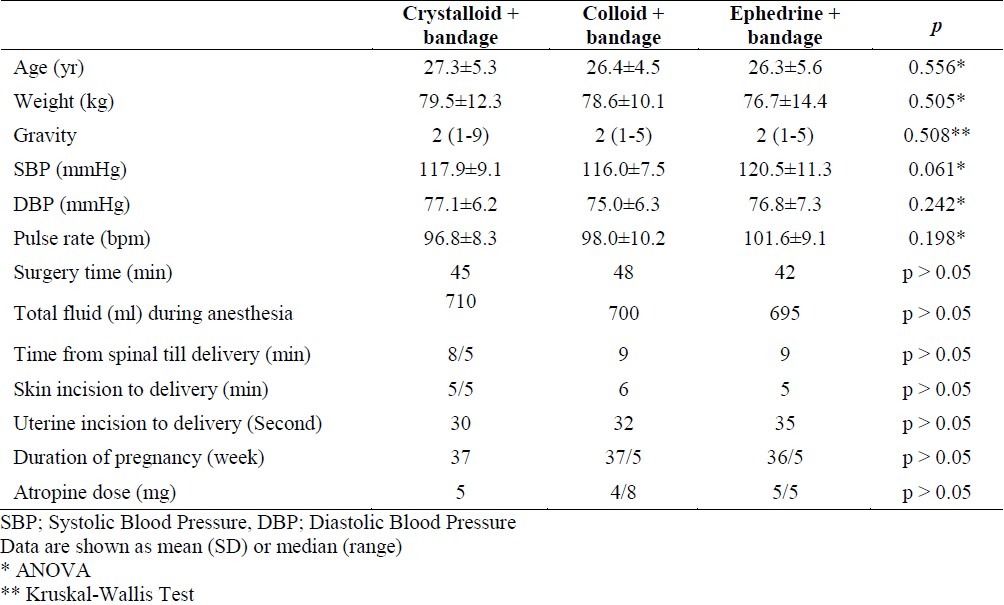
All parturients completed the study. The three groups of the study were similar in demographic and baseline characteristics, though there was a non-significant difference among the groups regarding baseline SBP (p=0.061, Table 1).
Table 1.
Baseline and surgical characteristics among the three groups
Changes in SBP during 60 minutes after the spinal injection are shown in Figure 2. Analyses showed that changes in SBP were significantly influenced by time (p < 0.001), but the difference among the groups was not statistically significant in this regard (time × group; F = 2.6, p = 0.074). In regard to HR, analyses showed that changes in HR were significantly influenced by time (p < 0.001) and the combined effect of time and intervention type (time × group; F = 5.2, p = 0.007). Post-hoc tests showed that HR in group 3 was significantly lower immediately after anesthesia (p < 0.05) and at minutes 20 (p < 0.001), 25 (p < 0.001), 30 (p < 0.001), 35 (p < 0.05), and 60 (p = 0.001) after anesthesia compared with the other two groups.
Figure 2.

Systolic blood pressure changes during 60 minutes after spinal injection
Group 1: Crystalloid+leg bandage
Group 2: Colloid+leg bandage
Group 3: Ephedrine+leg bandage
p < 0.001
Primary and secondary maternal outcome variables are summarized in Table 2. The cumulative incidence of hypotension was 54%, 64%, and 36% in groups 1 to 3, respectively (p = 0.018). Cumulative survival, proportion of patients who did not become hypotensive during 60 minute monitoring after spinal injection is presented in Figure 3. The interval between spinal injection and occurrence of hypotension was not different among the groups (p = 0.828). The differences among groups in the continuation of hypotension was also not statistically significant (p = 0.212).
Table 2.
Comparison of primary and secondary maternal outcome variables among the three groups
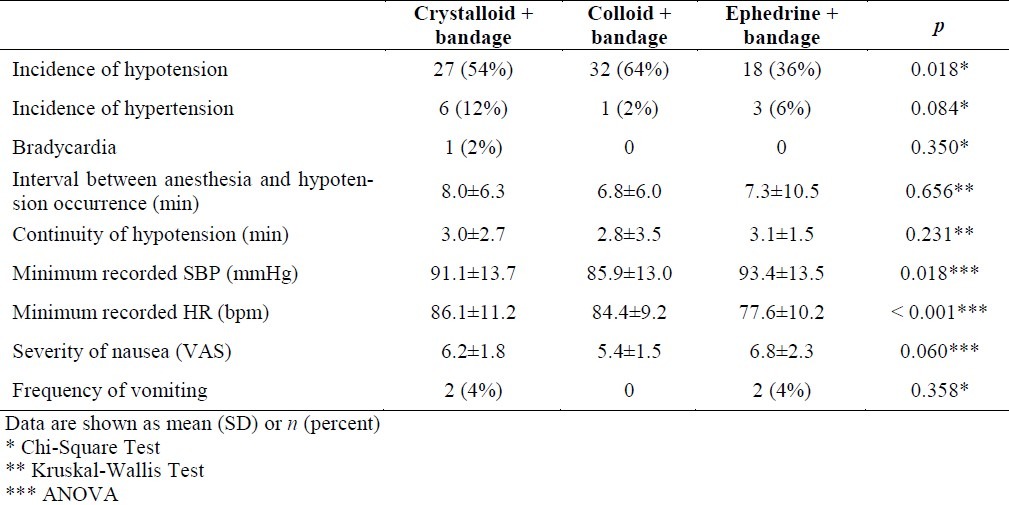
Figure 3.
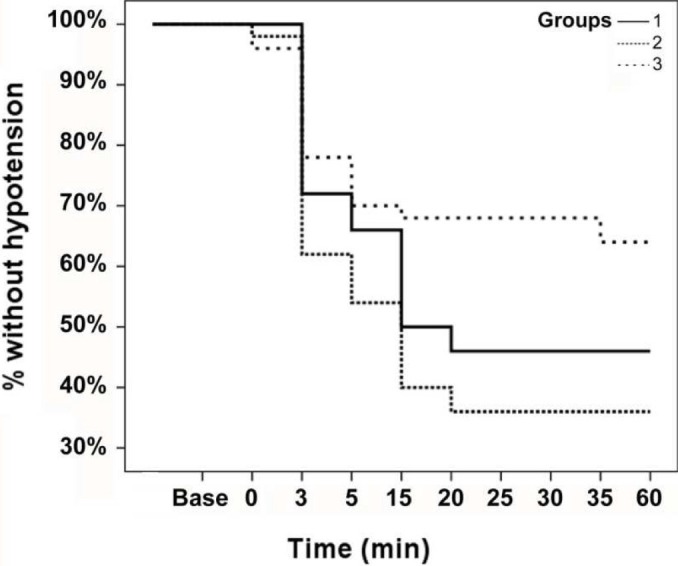
Kaplan-Meier survival curves showing the proportion of patients who remained not hypotensive until 60 minutes after anesthesia
Group 1: Crystalloid+leg bandage
Group 2: Colloid+leg bandage
Group 3: Ephedrine+leg bandage
p = 0.828
There was no significant difference among the groups in cumulative incidence of hypertension (p = 0.084). Only one parturient in group 1 experienced bradycardia. The lowest recorded SBP was different among the three groups (p = 0.018); this value was lower in group 2 compared with group 3 (p = 0.016). The lowest recorded HR was also different among the groups (p < 0.001); this value was lower in group 3 compared with the other two groups (p = 0.003 and < 0.001). There were not significant differences in supplementary ephedrine requirement between groups 1 and 2, which did not receive prophylactic ephedrine (8.7±5.1 vs. 9.2±5.6, p = 0.641). Considering the severity of nausea and the frequency of vomiting, there were no significant differences among the study groups (p > 0.05).
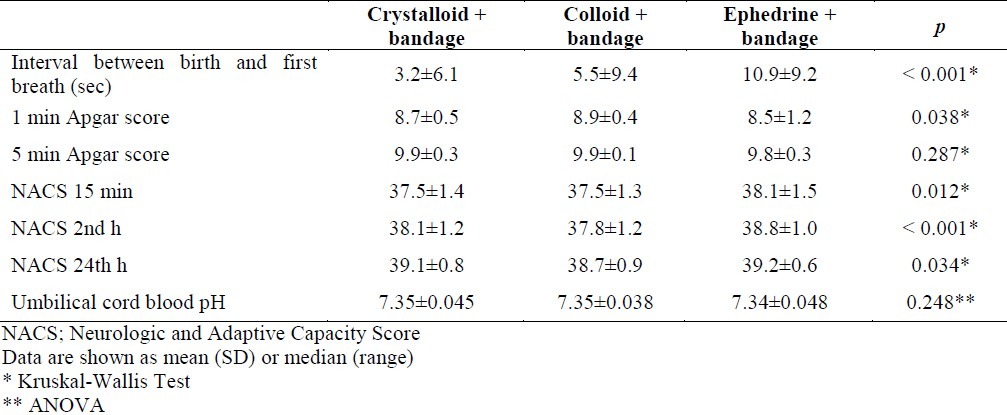
Regarding neonatal outcomes, the interval between birth and first breath was longer in group 3 compared with the other groups (p < 0.001, Table 3). There was a significant difference among the groups in Apgar scores at minute 1 (p = 0.038). Apgar scores at minute 1 were 7 or above in groups 1 and 2, but one neonate in group 3 had Apgar score of 1 at minute 1. No Apgar scores were below 7 at 5 min and there were no significant differences among the groups in Apgar scores at minute 5. Groups were significantly different in NACS of 15 minute and 2nd and 24th hours; group 2 had lower scores compared with group 3 at measured times (p = 0.007, < 0.001 and 0.010, respectively). Umbilical cord blood pH was not below 7.2 in any case and no significant difference was found among the three groups in this regard (p = 0.248, Table 3).
Table 3.
Comparison of neonatal outcome among the three groups
Discussion
Considering the results of the present study, none of the combinational methods were completely successful in the prevention of hypotension. However, those who received ephedrine plus bandage (group 3) experienced better maternal outcomes compared with those who received crystalloid or colloid plus bandage. Regarding the neonatal outcomes, those who received ephedrine in their prophylactic method (groups 3) experienced greater intervals between the birth and the first breath and lower Apgar scores at minute 1. Other differences among the groups in neonatal outcome, though statistically significant, were not clinically important.
Limited studies have been carried out on the effectiveness of combinational treatments in preventing hypotension following spinal anesthesia in cesarean delivery. In the study by Riley and colleagues, the prevalence of hypotension occurrence was 45% in parturients who received Hetastarch solution plus RL solution, compared with 85% of the control group which received RL solution.8 Another study by Mathru et al. demonstrated that adding albumin to RL solution significantly reduced the frequency and severity of hypotension.7 Moreover, rapid infusion of crystalloid solution plus phenylephrine (100 micg/min) proved to be more effective in reducing the frequency of hypotension that their slow infusion.10 Results of another study demonstrated that prophylactic administration of ephedrine in combination with Hetastarch and RL solution compared with the combination treatment which used placebo instead of ephedrine in mentioned regimen, decreased the occurrence rate of hypotension from 58% to 25%. Moreover, only 8% of the parturients who received ephedrine experienced severe hypotension (SBP < 90 mmHg), while 42% of the control group experienced severe hypotension.9
In our study, 51.3% of all cases who received bandage experienced hypotension. Adsumelli et al. reported that using leg compression device solely reduced the frequency of hypotension occurrence from 92% to 52%.12 Some other studies indicated that leg wrapping significantly reduced the frequency of hypotension, even equal to that of phenylephrine.13–15 Our results, however, implied that combinational treatment of crystalloid/colloid solution plus leg bandage did not have significant prophylactic effect on the occurrence of hypotension. Although in one study, colloids were more effective than crystalloids for prevention of hypotension (cyna), balanced salt solutions remained the preferred volume expander in the United States. Also, another study evaluated the efficacy of crystalloid and colloid preload in patients receiving spinal anesthesia for elective cesarean section. Although the incidence of hypotension was lower in patients who received 1 L of hydroxyethyl starch solution, the authors concluded that the augmentation of blood volume with preloading, regardless of the fluid used, must be large enough to result in a significant increase in cardiac output for effective prevention of hypotension.3
The observed difference can be due to the amount of administered solutions, more rapid administration, and also using a different type of bandage (Esmarch's bandage).
Evidence has shown that ephedrine has effects on cardiac beta receptors indirectly, which lead to sinus node stimulation and consequently preventing decrease in heart rate following spinal anesthesia. In some cases, this led to increase in heart rate.16 Prophylactic ephedrine has been shown to prevent bradycardia in previous studies.17 However, the results of our study showed that prophylactic ephedrine without crystalloid/colloid solution is not effective in preventing the decrease in HR after spinal anesthesia. In our study, the groups were not significantly different in the relative frequency of nausea, vomiting, the severity of nausea, and the frequency of administration of atropine or metoclopramide. This was in agreement with the results of some previous studies.17 However, relative frequency of post-operation nausea and vomiting was 30% to 46%, which was higher than that in other studies.1
In our study, newborns of the three groups were different, considering the interval between the birth and the first breath, Apgar score at minute 1 and NACS at 15 minute and 2nd and 24th hours. Shearer et al. reported fetal acidosis following the administration of prophylactic ephedrine,17 but we did not find significant effects of ephedrine on umbilical cord blood pH. The observed effects of ephedrine on neonatal outcomes (Apgar score) in our study were reported in previous studies too. Hughes et al. showed that ephedrine even with high dosage had no deleterious effects on fetal well being or neonatal outcome in patients undergoing cesarean section with epidural anesthesia.18 It is suggested that small doses of IV ephedrine given to the mother to prevent hypotension during spinal anesthesia have short-lived effects on the neonate's central nervous system, which will be detected in the spectral EEG, but not in neurobehavioral tests.19 Also, it has been shown that there was no true fetal acidosis (i.e., umbilical arterial blood PH<7.2) with ephedrine.4 Although our results indicated that newborns were different in some variables, all were in an acceptable range and we believe that these differences were not of clinical importance.
Conclusion
In conclusion, employing all mentioned combination treatments reduced the rate of hypotension occurrence following spinal anesthesia in parturients undergoing cesarean delivery; the rate was lower than the reported rates in most of the previous literatures. Among the three studied methods, administration of ephedrine plus bandage of the lower extremities was the most effective one in reducing the incidence of hypotension. The groups were not clinically different concerning the effect of treatment on newborn health, and maternal post-operational nausea or vomiting.
Authors’ Contributions
All authors participated in generating the idea and designing and conducting the study. MJ managed the study and prepared the draft of the report. All authors studied and edited the draft, and approved the final version of the manuscript.
Acknowledgement
This study was supported by the Isfahan University of Medical Sciences (Project No. 83036, IRCT number: IRCT201107062405N7). Authors are thankful to Dr. Ali Gholamrezaei who helped us in data analysis and editing this report.
Footnotes
Conflict of Interests Authors have no conflict of interests.
References
- 1.Klohr S, Roth R, Hofmann T, Rossaint R, Heesen M. Definitions of hypotension after spinal anaesthesia for caesarean section: literature search and application to parturients. Acta Anaesthesiol Scand. 2010;54(8):909–21. doi: 10.1111/j.1399-6576.2010.02239.x. [DOI] [PubMed] [Google Scholar]
- 2.Reynolds F, Seed PT. Anaesthesia for Caesarean section and neonatal acid-base status: a meta-analysis. Anaesthesia. 2005;60(7):636–53. doi: 10.1111/j.1365-2044.2005.04223.x. [DOI] [PubMed] [Google Scholar]
- 3.Cyna AM, Andrew M, Emmett RS, Middleton P, Simmons SW. Techniques for preventing hypotension during spinal anaesthesia for caesarean section. Cochrane Database Syst Rev. 2006;(4):CD002251. doi: 10.1002/14651858.CD002251.pub2. [DOI] [PubMed] [Google Scholar]
- 4.Kuczkopwski KM, Reisner LS, Lin D. Anesthesia for cesarean section. In: Chestnut DH, Polley LS, Tsen LC, Wong CA, editors. Chestnut's Obstetric Anesthesia: Principles and Practice. 4th ed. Philadelphia: Mosby; 2009. pp. 422–5. [Google Scholar]
- 5.Morgan PJ, Halpern SH, Tarshis J. The effects of an increase of central blood volume before spinal anesthesia for cesarean delivery: a qualitative systematic review. Anesth Analg. 2001;92(4):997–1005. doi: 10.1097/00000539-200104000-00036. [DOI] [PubMed] [Google Scholar]
- 6.Lee A, Ngan Kee WD, Gin T. A dose-response meta-analysis of prophylactic intravenous ephedrine for the prevention of hypotension during spinal anesthesia for elective cesarean delivery. Anesth Analg. 2004;98(2):483–90. doi: 10.1213/01.ANE.0000096183.49619.FC. table. [DOI] [PubMed] [Google Scholar]
- 7.Mathru M, Rao TL, Kartha RK, Shanmugham M, Jacobs HK. Intravenous albumin administration for prevention of spinal hypotension during cesarean section. Anesth Analg. 1980;59(9):655–8. [PubMed] [Google Scholar]
- 8.Riley ET, Cohen SE, Rubenstein AJ, Flanagan B. Prevention of hypotension after spinal anesthesia for cesarean section: six percent hetastarch versus lactated Ringer's solution. Anesth Analg. 1995;81(4):838–42. doi: 10.1097/00000539-199510000-00031. [DOI] [PubMed] [Google Scholar]
- 9.Vercauteren MP, Coppejans HC, Hoffmann VH, Mertens E, Adriaensen HA. Prevention of hypotension by a single 5-mg dose of ephedrine during small-dose spinal anesthesia in prehydrated cesarean delivery patients. Anesth Analg. 2000;90(2):324–7. doi: 10.1097/00000539-200002000-00016. [DOI] [PubMed] [Google Scholar]
- 10.Ngan Kee WD, Khaw KS, Ng FF. Prevention of hypotension during spinal anesthesia for cesarean delivery: an effective technique using combination phenylephrine infusion and crystalloid cohydration. Anesthesiology. 2005;103(4):744–50. doi: 10.1097/00000542-200510000-00012. [DOI] [PubMed] [Google Scholar]
- 11.Saghaei M. Random allocation software for parallel group randomized trials. BMC Med Res Methodol. 2004;4:26. doi: 10.1186/1471-2288-4-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Adsumelli RS, Steinberg ES, Schabel JE, Saunders TA, Poppers PJ. Sequential compression device with thigh-high sleeves supports mean arterial pressure during Caesarean section under spinal anaesthesia. Br J Anaesth. 2003;91(5):695–8. doi: 10.1093/bja/aeg248. [DOI] [PubMed] [Google Scholar]
- 13.Sun HL, Ling QD, Sun WZ, Wu RS, Wu TJ, Wang SC, et al. Lower limb wrapping prevents hypotension, but not hypothermia or shivering, after the introduction of epidural anesthesia for cesarean delivery. Anesth Analg. 2004;99(1):241–4. doi: 10.1213/01.ANE.0000121346.33443.5A. [DOI] [PubMed] [Google Scholar]
- 14.Bjornestad E, Iversen OE, Raeder J. Wrapping of the legs versus phenylephrine for reducing hypotension in parturients having epidural anaesthesia for caesarean section: a prospective, randomized and double-blind study. Eur J Anaesthesiol. 2009;26(10):842–6. doi: 10.1097/EJA.0b013e328329b028. [DOI] [PubMed] [Google Scholar]
- 15.Kaya S, Karaman H, Erdogan H, Akyilmaz A, Turhanoglu S. Combined use of low-dose bupivacaine, colloid preload and wrapping of the legs for preventing hypotension in spinal anaesthesia for caesarean section. J Int Med Res. 2007;35(5):615–25. doi: 10.1177/147323000703500506. [DOI] [PubMed] [Google Scholar]
- 16.Moss J, Glick D. The autonomic nervous system. In: Miller RD, editor. Miller's Anesthesia. 7th ed. New York: Churchill Livingstone; 2009. pp. 79–84. [Google Scholar]
- 17.Shearer VE, Ramin SM, Wallace DH, Dax JS, Gilstrap LC., III Fetal effects of prophylactic ephedrine and maternal hypotension during regional anesthesia for cesarean section. J Matern Fetal Med. 1996;5(2):79–84. doi: 10.1002/(SICI)1520-6661(199603/04)5:2<79::AID-MFM6>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 18.Hughes SC, Ward MG, Levinson G, Shnider SM, Wright RG, Gruenke LD, et al. Placental transfer of ephedrine does not affect neonatal outcome. Anesthesiology. 1985;63(2):217–9. doi: 10.1097/00000542-198508000-00023. [DOI] [PubMed] [Google Scholar]
- 19.Kangas-Saarela T, Hollmen AI, Tolonen U, Eskelinen P, Alahuhta S, Jouppila R, et al. Does ephedrine influence newborn neurobehavioural responses and spectral EEG when used to prevent maternal hypotension during caesarean section? Acta Anaesthesiol Scand. 1990;34(1):8–16. doi: 10.1111/j.1399-6576.1990.tb03033.x. [DOI] [PubMed] [Google Scholar]


