Abstract
BACKGROUND:
Dislocated lens fragments in the vitreous cavity can cause potentially serious complications. This retrospective study aimed to evaluate the visual outcome of patients who underwent pars plana vitrectomy (PPV) for posteriorly dislocated lens fragments after cataract phacoemulsification.
METHODS:
A retrospective study was conducted on all consecutive cases (60 patients) with pars plana vitrectomy performed for retained lens fragment. In 30 eyes (50%), PPV was performed within 1 week of cataract extraction and in 30 eyes (50 %), PPV was performed more than 1 week post cataract extraction from July 2005 through August 2008.
RESULTS:
In the late vitrectomy group, 66.6% of eyes developed persistent uveitis, 53.3% of eyes showed elevated intra-ocular pressure (IOP) and 5 eyes retinal detachment. In early PPV group 16.6% developed uveitis and 20% showed elevated IOP and one eye retinal detachment. The final visual acuity was 20 ± 50 in early PPV and 20 ± 200 in late PPV group (mean ± SD, p < 0.001).
CONCLUSIONS:
The early use of PPV to remove posterior dislocated lens fragments within the first week was shown to be advantageous. The inflammatory response was less pronounced, IOP rose less significant, the incidence of retinal detachment was lower and visual recovery was faster.
KEYWORDS: Nucleus Loss, Retained Lens Fragment, Pars Plana Vitrectomy, Phacoemulsification
Dislocated lens fragment in the vitreous cavity is an uncommon event that occurs in 0.2–1.5% of cases during phacoemulsification surgery.1–3 It has been shown that its rate is inversely related to the experience of the surgeon2,4 and a rate of 0.2% for experienced surgeons against 0.65% for trainees was found. The presence of these retained lens fragments may create complications such as uveitis, corneal edema, cystoid macular edema (CME) and retinal detachment, resulting in a decrease in visual acuity.5–7 Pars plana vitrectomy (PPV) has been used successfully to retrieve the retained lens fragments in order to minimize the risk of further complications.3,8–15 Although the optimal timing of pars plana vitrectomy has remained controversial,5,10–12 histological studies showed that inflammatory reaction is more severe with longer duration of lens fragments remaining within the eye.16,17 The performance of pars plana vitrectomy to retrieve the dislocated lens fragments at the time of cataract surgery may therefore be beneficial to minimize postoperative inflam-mation and its associated morbidity as well as to eliminate the need of two separate operations. This study evaluated the visual outcome of early and late PPV to manage posteriorly dislocated lens fragments following cataract extraction.
Methods
In this retrospective, non-comparative, consecutive case series medical records of all patients who underwent pars plana vitrectomy for retained nucleus into the vitreous after complicated cataract surgery were reviewed over a 3-year period between July 2005 and August 2008 at the Department of Ophthalmology, Feiz hospital Isfahan, Iran. There was a sample of 60 eyes from 60 patients who were referred to our hospital for nucleus loss into the vitreous after complicated cataract phacoemulsification. The interval between cataract surgery and PPV was divided into 2 groups, within 1 week and more than 1 week. A minimum of 3 months of follow-up data after vitrectomy was necessary for inclusion in the study.
In 30 eyes (50%), PPV was performed within 1 week of cataract extraction and in 30 eyes (50%), PPV was performed more than 1 week post cataract extraction. We excluded patients who presented only cortical fragments of the lens without nuclear material, patients who were not visited in the correct order of visits after surgery, patients with PPV previous to cataract surgery and patients with macular lesions such as myopic changes or age related macular degeneration that affects the central visual acuity. The parameters of the study included demographics, preexisting eye diseases, details of the previous cataract surgery (including date), performance of anterior vitrectomy, and intraocular lens (IOL) implantation. In addition, visual acuity using Snellen charts, IOP, anterior and posterior segment findings at presentation (including the presence of corneal edema, anterior uveitis, lens matter, vitreous and/or fibrin in the anterior chamber, hyphema and hypopyon), the approximate size of nuclear fragments in the vitreous, vitritis, vitreous hemorrhage, retinal detachment, CME, and choroidal effusion were evaluated. Other studied variables were the details of the procedure (including date), the interval between cataract extraction and vitreoretinal surgery, use of phacofragmentation (fragmatome) and/or heavy liquids, operative complications such as retinal tear or retinal detachment, final visual acuity, and complications were recorded during the follow-up. Visual acuity was measured with Snellen chart. A poor visual outcome was defined as a visual acuity worse than 20/40. An IOP value was considered high when it was 30 mmHg in cases with no history of glaucoma, with or without maximal medical therapy. Anterior uveitis was graded by the number of cells in the anterior chamber (1+ = minimum cells and 4+ = marked cells) and the posterior uveitis was graded based on the haze presented into the vitreous cavity. Anterior uveitis was recorded when an anterior chamber reaction of +2 was present. Corneal edema was considered significant when both stromal and epithelial edema were present. No patients had an implanted intraocular lens when they came to our hospital with fragments of the lens nucleus that had been lost into the vitreous.
A dilated fundus examination was performed preoperatively in order to identify the number and location of the lens fragments, and to rule out any retinal tears or breaks, in which an argon laser photocoagulation was performed if the visualization of the retina was possible. In addition, an IOP was taken, and we noted if there were any other pathologies such as vitreous or suprachoroidal hemorrhage, CME or previous glaucoma. PPV was performed as soon as a vitreo-retinal operating room became available. A standard three-port PPV is the procedure of choice after stability of the cataract wound is ensured. Any residual lens material surrounding the iris area is carefully removed; care is taken to avoid breaking the capsule remains ready for the final intraocular lens implantation. A core vitrectomy was performed, followed by the removal of the softer cortical lens material and vitreous around the nucleus. A small volume of perfluorodecalin is injected over the optic nerve in order to protect the macular area against the ultrasonic energy and mechanical trauma from the lens fragments. The phacofragmatome tip was used to aspirate the nucleus material, assisted by the tip of the endoilluminator to keep the nuclear fragments near the phacofragmatome. Low power setting was used in order to avoid the propulsion of the lens fragments.
After the vitrectomy and lensectomy are completed a peripheral examination with scleral depression is performed, and peripheral vitrectomy is done in order to eliminate any peripheral vitreous traction. If there is any break or tear, an argon endolaser treatment is done. At the end of the surgery a placement of the IOL is performed. If a small intact capsulorhexis is present, the IOL can be placed in the sulcus. An anterior chamber IOL is placed in patients who lack adequate capsular support.
After the PPV, there was a follow-up control of the patients after one week, one month, three months and every six months thereafter until the end of the study. The corrected visual acuity was measured at each visit and included in the statistical analysis with the results obtained after three months, 6 months and at the end of the study.
At the end of the study, all patients were submitted to an exploration that included corrected Snellen visual acuity, applanation tonometry, corneal pachymetry (with ORB-SCAN) and fundus retinography.
Descriptive statistics were calculated using SPSS software (version 13.5). Values are expressed as mean ± SD, and statistical significance was determined using the Student's t-test for paired data. The McNemar test was used for evaluating the qualitative data such as presence of the CME, corneal edema, retinal detachment and high IOP.
Results
Of 81 patients (81 eyes), 60 subjects (60 eyes) met the inclusion criteria and were included in the study. The mean age of the patients was 75.7 ± 10 years (ranged 57–84 years). There were 24 men (40%) and 36 women (60%). All eyes underwent phacoemulsification cataract surgery. The mean follow-up period after surgery was 6 months (ranged 3–47 months). The mean preoperative visual acuity of the 60 patients was 20/300 (ranged from LP to 20/200).
Before PPV the IOP was high in 30 patients (50.0%), corneal edema was present in 35 patients (58.3%) and uveitis in 45 patients (75%). We did not observe any cases of retinal detachment or vitreous hemorrhage (Figure 1). The size of the dropped lens fragments was estimated by the surgeon and we had 15 total nuclei, 20 two-quadrant fragments and in 25 patients there was a one-quadrant fragment (equal in two groups) which was dropped at the time of phaco surgery. Removal of lens fragment during PPV was performed using vitreous cutter, phacofragmentation, and limbal delivery in 30, 20 and 10 eyes, respectively.
Figure 1.
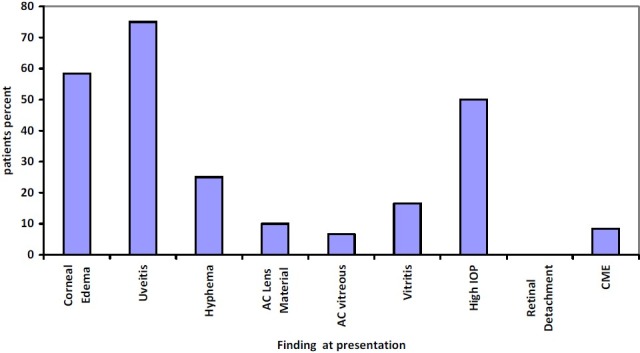
Clinical features of patients with retained lens fragments in initial examination AC: Anterior Chamber, IOP: Intra Ocular Pressure, RD: Retinal Detachment, CME: Cystoid Macular Edema
All 60 patients underwent a standard three-port PPV to remove the retained lens fragments. The median time to vitrectomy was 18 days (ranged 1-60 days). After surgery in late vitrectomy groups, 67.5% eyes had persistent uveitis, whereas 18% of early group had uveitis (p = 0.0005). IOP (30 mmHg or more) was measured in 22 patients (36.6%); It normalized without medication after vitrectomy in 16 patients (72.7%) whereas the remaining 6 patients continued to require antiglaucoma medications; however, none had filtering surgery. The time interval between cataract surgery and vitrectomy among these 6 patients was within 1 week in 1 patient and more than 1 week in 5 patients. 20% of early and 52% of late group elevated IOP (p < 0.001).
New rhegmatogenous retinal detachment macula occurred in 1 patient in early vitrectomy group and 5 patients in late vitrectomy group between 2 and 4 months after vitrectomy. No postoperative complications, such as vitreous or suprachoroidal hemorrhage or fibrinous uveitis were recorded. One patient with sulcus IOL implantation presented a subluxation of the IOL 3 weeks after surgery and needed a new PPV and an exchange of the IOL for an anterior chamber IOL.
During the first 3 months after surgery, a CME appeared in 14 patients (23.3%), 4 patients of early vitrectomy group and 10 patients of late vitrectomy group, which was resolved in 15 of them with topical treatment. Treatment was with topical prednisolone acetate and with topical cyclooxygenase inhibitor (diclofenac). The other five patients who had not recovered were given a sub-Tenon's triamcinolone injection, but both developed a chronic form of CME. At the end of the study, we observed a chronic cystoid macular edema in ten patients (16.6%).
The visual acuity generally improved after vitrectomy (Table 1). Before vitrectomy, the majority of patients presented with a visual acuity of 20/200 or worse (91.6%). None of these patients had a visual acuity of 20/40 or better.
Table 1.
Visual acuity before and after vitrectomy in all cases
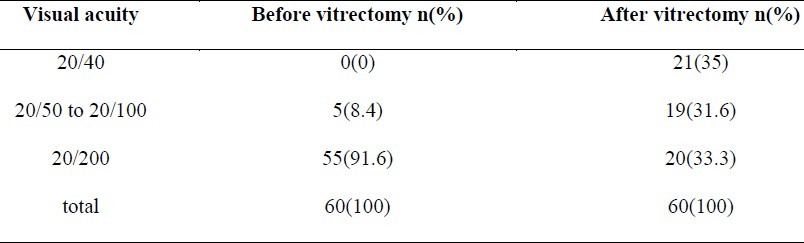
The mean final visual acuity was 20/50 in early and 20/200 in late group. With a minimum of 2 months follow up, visual acuity improved after vitrectomy in 55 patients. The median final postoperative visual acuity was 20/80 (ranged LP to 20/28). The mean improvement in visual acuity was 4 lines (ranged 2–7 lines).
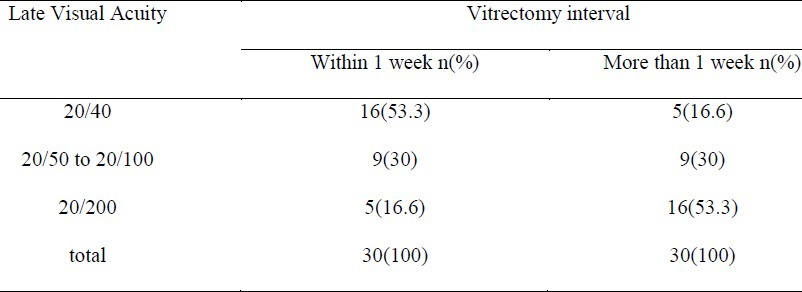
The timing of vitrectomy compared with the visual acuity outcome is shown in (Table 2). The interval between cataract surgery and vitrectomy was evaluated. Of the 30 eyes that underwent PPV within 1 week of cataract extraction, the final visual acuity was 20/40 or better in 15 eyes (50%). Of the 30 eyes that underwent PPV after 1 week, 6 (20%) achieved a visual acuity of 20/40 or better while 24 eyes (80%) had a visual acuity worse than 20/40. There was statistically significant difference in outcome between patients having PPV within the first week after cataract surgery and those having it later (p < 0.001).
Table 2.
Final visual acuity after early and late vitrectomy in eyes after retain lens fragment
Discussion
Although PPV is considered the preferred surgical procedure in the management of posteriorly dislocated lens fragments following cataract surgery, a review of the literature indicates a lack of consensus regarding the timing effect of this procedure on the final visual outcome. According to several studies, patients undergoing PPV to manage retained lens fragments experienced a higher incidence of long-term complications (e.g., corneal edema, uveitis, glaucoma and retinal detachment) when the performance of this procedure was delayed.11 In contrast, other studies found that the timing of PPV in management of patients with posteriorly dislocated lens fragments after cataract surgery did not have an effect on the final visual outcome and the rate of complications.8,18
Some studies suggested that delaying vitrectomy for 2 or more weeks can facilitate the eventual procedure by allowing for softening of nuclear material, posterior vitreous detachment, and better control of intraocular inflammation and pressure.19
The visual acuity of eyes that have undergone PPV has improved since the earlier reports, which showed a final visual acuity better than 0.5 in 42%.9,10 More recently, studies have reported final visual acuity better than 0.5 in 60%–68% of the patients.14,15,20
Al-Khaier and coauthors12 found that a delay of vitrectomy for more than 4 weeks correlated with poor visual outcome. Other large series have failed to demonstrate a statistically significant association between the timing of vitrectomy and chronic glaucoma or visual outcome.10,15
In the current series, delaying vitrectomy for more than 1 week was associated with a higher percentage of patients with poor visual outcome, whereas a higher percentage of patients who underwent vitrectomy within 1 week achieved a visual acuity of 20/40 or better. This difference was statistically significant.
One of the main findings in our study was that the development of secondary glaucoma was observed in 6 patients of early vitrectomy group and 53.3% of late vitrectomy group. Blodi et al.9 also showed that early PPV within 3 weeks decreased the rate of chronic glaucoma. In a clinicopathological study of retained intravitreal lens fragments after phacoemulsification, Yeo et al.21 found that there was significantly less inflammatory cell activity in eyes receiving early pars plana vitrectomy within 1 week. Later removal was associated with persistently elevated intraocular pressure and poorer visual outcome. Therefore, early vitrectomy at the time of cataract surgery may prevent the development of secondary glaucoma by limiting lens-induced intraocular inflam-mation. This is particularly relevant in those eyes with pre-existing compromised outflow facility or various optic neuropathies.
Similarly, lens-induced prolonged intraocular inflammation may theoretically increase vitreoretinal traction and cause retinal detachment.5 A trend of increased incidence of retinal detachment in eyes of delayed vitreous surgery was observed by Margherio et al.11
The commonest postoperative complication in our series was retinal detachment that occurred in six patients (10%). This rate of retinal detachment is within the range reported in other studies in which vitrectomy was performed later for retained lens fragment, which ranged from 0 to 21.5%.4–14 This suggests that early vitrectomy does prevent the problem of development of retinal detachment. The reattachment rate for retinal detachment after vitrectomy for retained lens fragment is usually favorable, but visual outcomes are often poor due to other comorbidities particularly cystoid macular oedema.22 Non-excessive manipulation during the cataract operation, and appropriate maneuver during the vitrectomy procedure are of utmost importance in preventing this complication. Borne et al.10 and Al-Khaier et al.12 observed a trend toward higher rates of retinal detachment among patients in whom phacofragmentation was used. However, other large series have not confirmed these observations.11,15 Preoperative retinal detachment is a major risk factor related to the manipulation of vitreous during the primary cataract surgery, therefore correct postoperative care of cataracts may decrease the risk. Cystoid macular edema is another complication associated with lens-induced inflammation and has been found to be a major cause for poor final vision after surgery for retained intravitreal fragments.8,11–14 Margherio et al.11 found that 27% of patients developed postoperative cystoid macular edema after vitrectomy as a late postoperative complication. When vitrectomy was performed on the same setting of cataract surgery, Kageyama et al.3 reported a lower rate of postoperative cystoid macular edema (12%). In our series, 16 patients (26.6%) developed cystoid macular edema postoperatively and this was similar to the findings by Kim et al.8 in which none of the eight eyes, which underwent vitrectomy on the same day as the complicated cataract surgery, developed postoperative cystoid macular edema. Early vitrectomy may therefore have a role in reducing the incidence of postoperative cystoid macular edema by minimizing lens-induced inflammation.
Our findings showed 53.3% of patients in early vitrectomy group had vision of 0.4 or higher, but in late vitrectomy group 16.6% were with vision 0.4 or higher. We should take into account that we have seen changes over time. In the course of the study, visual acuity has decreased and the final visual acuity higher than 0.4 was achieved by only 40% of the early group. The major decrease was observed in the six months postoperative period, a possible explanation being that during the first six months postoperative period, CME appeared and many patients suffered a decrease in their vision that many cannot recover. This finding is similar to Greve et al.23
In the postoperative period a major visual decrease is attributed to the cystoid macular edema.24 In the present study, CME was the major cause of visual impairment, but there are several important considerations when studying eyes with CME after PPV for retained lens nucleus. Because CME can occur several months after surgery, adequate follow-up is important.25,26 In our study fifteen patients (31.91%), suffered CME in the first six months of the PPV, and we should take into account that in six patients (12.76%) the CME has still not been resolved 4.56 ± 1.34 years later and continues as a chronic problem.
Whereas early vitrectomy is desirable, converting a complicated cataract surgery into a PPV during the same session may not be ideal. Lengthening an already prolonged case can be difficult for the patient. Achieving adequate anesthesia can also become a problem, particularly in the modern era of topical anesthesia.
Although the posterior dislocation of lens material is a serious complication of phacoemulsification, appropriate intraoperative and postoperative management of this complication can result in good visual outcome. Early involvement of the retinal surgeon facilitates the evaluation and timing for vitrectomy and lensectomy based on the clinical course.27
Our series consisted of 60 patients, to the best of our knowledge, was the largest series describing early vitrectomy versus late vitrectomy performed for dislocated lens fragments during cataract surgery in the literature. In conclusion, there was statistically significant difference in outcome between patients undergoing vitrectomy within the first week after cataract surgery and those underwent it lately.
The main limitation of our study was being retrospective in nature. Nevertheless, our study demonstrated that early vitrectomy (during 1 week) performed for retained lens fragments was a viable option and may decrease the risk of secondary glaucoma and cystoid macular edema. Further prospective clinical trial in this area may provide us with more insight in determining the optimal timing of vitrectomy. Being retrospective, our study findings were not conclusive, despite the initial good results of these patients after PPV surgery, so follow-up should be accurate and continued, in order to minimize postoperative complications such as retinal detachment, retinal breaks, secondary glaucoma and CME.
Authors’ Contributions
AS and HR designed the study and did the final approval of the article, ANB and ZNB did data collection, analysed and interpretated the data, and did the final approval of the article.
Footnotes
Conflict of Interests Authors have no conflict of interests.
References
- 1.Leaming DV. Practice styles and preferences of ASCRS members--1995 survey. J Cataract Refract Surg. 1996;22(7):931–9. doi: 10.1016/s0886-3350(96)80194-5. [DOI] [PubMed] [Google Scholar]
- 2.Aasuri MK, Kompella VB, Majji AB. Risk factors for and management of dropped nucleus during phacoemulsification. J Cataract Refract Surg. 2001;27(9):1428–32. doi: 10.1016/s0886-3350(01)00784-2. [DOI] [PubMed] [Google Scholar]
- 3.Kageyama T, Ayaki M, Ogasawara M, Asahiro C, Yaguchi S. Results of vitrectomy performed at the time of phacoemulsification complicated by intravitreal lens fragments. Br J Ophthalmol. 2001;85(9):1038–40. doi: 10.1136/bjo.85.9.1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schwartz SG, Holz ER, Mieler WF, Kuhl DP. Retained lens fragments in resident-performed cataract extractions. CLAO J. 2002;28(1):44–7. [PubMed] [Google Scholar]
- 5.Monshizadeh R, Samiy N, Haimovici R. Management of retained intravitreal lens fragments after cataract surgery. Surv Ophthalmol. 1999;43(5):397–404. doi: 10.1016/s0039-6257(99)00022-3. [DOI] [PubMed] [Google Scholar]
- 6.Kim IK, Miller JW. Management of dislocated lens material. Semin Ophthalmol. 2002;17:162–6. doi: 10.1076/soph.17.3.162.14779. [DOI] [PubMed] [Google Scholar]
- 7.Amri AM. Visual outcome of pars plana vitrectomy for retained lens fragments after phacoemulsification. Middle East Afr J Ophthalmol. 2008;15(3):107–11. doi: 10.4103/0974-9233.51984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kim JE, Flynn HW, Jr, Rubsamen PE, Murray TG, Davis JL, Smiddy WE, et al. Endophthalmitis in patients with retained lens fragments after phacoemulsification. Ophthalmology. 1996;103(4):575–8. doi: 10.1016/s0161-6420(96)30651-9. [DOI] [PubMed] [Google Scholar]
- 9.Blodi BA, Flynn HW, Jr, Blodi CF, Folk JC, Daily MJ. Retained nuclei after cataract surgery. Ophthalmology. 1992;99(1):41–4. doi: 10.1016/s0161-6420(92)32003-2. [DOI] [PubMed] [Google Scholar]
- 10.Borne MJ, Tasman W, Regillo C, Malecha M, Sarin L. Outcomes of vitrectomy for retained lens fragments. Ophthalmology. 1996;103(6):971–6. doi: 10.1016/s0161-6420(96)30577-0. [DOI] [PubMed] [Google Scholar]
- 11.Margherio RR, Margherio AR, Pendergast SD, Williams GA, Garretson BR, Strong LE, et al. Vitrectomy for retained lens fragments after phacoemulsification. Ophthalmology. 1997;104(9):1426–32. doi: 10.1016/s0161-6420(97)30120-1. ot Found!! [DOI] [PubMed] [Google Scholar]
- 12.Al-Khaier A, Wong D, Lois N, Cota N, Yang YC, Groenewald C. Determinants of visual outcome after pars plana vitrectomy for posteriorly dislocated lens fragments in phacoemulsification. J Cataract Refract Surg. 2001;27(8):1199–206. doi: 10.1016/s0886-3350(01)00750-7. [DOI] [PubMed] [Google Scholar]
- 13.Romero-Aroca P, Fernández-Ballart J, Méndez-Marín I, Salvat-Serra M, Baget-Bernaldiz M, Buil-Calvo JA, et al. Management of nucleus loss into the vitreous: long term follow up in 63 patients. Clin Ophthalmol. 2007;1(4):505–12. [PMC free article] [PubMed] [Google Scholar]
- 14.Rossetti A, Doro D. Retained intravitreal lens fragments after phacoemulsification: complications and visual outcome in vitrectomized and nonvitrectomized eyes. J Cataract Refract Surg. 2002;28(2):310–5. doi: 10.1016/s0886-3350(01)01079-3. [DOI] [PubMed] [Google Scholar]
- 15.Oruc S, Kaplan HJ. Outcome of vitrectomy for retained lens fragments after phacoemulsification. Ocul Immunol Inflamm. 2001;9(1):41–7. doi: 10.1076/ocii.9.1.41.3979. [DOI] [PubMed] [Google Scholar]
- 16.Srinivasan S, van der Hoek J, Green F, Atta HR. Tractional ciliary body detachment, choroidal effusion, and hypotony caused by severe anterior lens capsule contraction following cataract surgery. Br J Ophthalmol. 2001;85(10):1261–2. doi: 10.1136/bjo.85.10.1260a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yeo LM, Charteris DG, Bunce C, Luthert PJ, Gregor ZJ. Retained intravitreal lens fragments after phacoemulsification: a clinicopathological correlation. Br J Ophthalmol. 1999;83(10):1135–8. doi: 10.1136/bjo.83.10.1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stilma JS, van der Sluijs FA, van Meurs JC, Mertens DA. Occurrence of retained lens fragments after phacoemulsification in The Netherlands. J Cataract Refract Surg. 1997;23(8):1177–82. doi: 10.1016/s0886-3350(97)80312-4. [DOI] [PubMed] [Google Scholar]
- 19.Ross WH. Management of dislocated lens fragments after phacoemulsification surgery. Can J Ophthalmol. 1996;31(5):234–40. [PubMed] [Google Scholar]
- 20.Eifrig CW, Scott IU, Flynn HW, Jr, Smiddy WE, Newton J. Endophthalmitis after pars plana vitrectomy: Incidence, causative organisms, and visual acuity outcomes. Am J Ophthalmol. 2004;138(5):799–802. doi: 10.1016/j.ajo.2004.06.035. [DOI] [PubMed] [Google Scholar]
- 21.Yeo LM, Charteris DG, Bunce C, Luthert PJ, Gregor ZJ. Retained intravitreal lens fragments after phacoemulsification: a clinicopathological correlation. Br J Ophthalmol. 1999;83(10):1135–8. doi: 10.1136/bjo.83.10.1135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moore JK, Scott IU, Flynn HW, Jr, Smiddy WE, Murray TG, Kim JE, et al. Retinal detachment in eyes undergoing pars plana vitrectomy for removal of retained lens fragments. Ophthalmology. 2003;110(4):709–13. doi: 10.1016/S0161-6420(03)00020-4. [DOI] [PubMed] [Google Scholar]
- 23.Greve MD, Peyman GA, Mehta NJ, Millsap CM. Use of perfluoroperhydrophenanthrene in the management of posteriorly dislocated crystalline and intraocular lenses. Ophthalmic Surg. 1993;24(9):593–7. [PubMed] [Google Scholar]
- 24.Cohen SM, Davis A, Cukrowski C. Cystoid macular edema after pars plana vitrectomy for retained lens fragments. J Cataract Refract Surg. 2006;32(9):1521–6. doi: 10.1016/j.jcrs.2006.04.019. [DOI] [PubMed] [Google Scholar]
- 25.Nelson ML, Martidis A. Managing cystoid macular edema after cataract surgery. Curr Opin Ophthalmol. 2003;14(1):39–43. doi: 10.1097/00055735-200302000-00007. [DOI] [PubMed] [Google Scholar]
- 26.Tranos PG, Wickremasinghe SS, Stangos NT, Topouzis F, Tsinopoulos I, Pavesio CE, et al. Macular edema. Surv Ophthalmol. 2004;49(5):470–90. doi: 10.1016/j.survophthal.2004.06.002. [DOI] [PubMed] [Google Scholar]
- 27.Rofagha S, Bhisitkul RB. Management of retained lens fragments in complicated cataract surgery. Curr Opin Ophthalmol. 2011;22(2):137–40. doi: 10.1097/ICU.0b013e3283436fc5. [DOI] [PubMed] [Google Scholar]


