Abstract
Background
There is great debate about the costs and benefits of technology-driven medical interventions such as instrumented lumbar fusion. With most analyses using charge data, the actual costs incurred by medical institutions performing these procedures are not well understood. The object of the current study was to examine the differences in hospital operating costs between open and minimally invasive spine surgery (MIS) during the perioperative period.
Methods
Data were collected in the form of a prospective registry from a community hospital after specific Institutional Review Board approval was obtained. The analysis included consecutive adult patients being surgically treated for degenerative conditions of the lumbar spine, with either an MIS or open approach for two-level instrumented lumbar fusion. Patient outcomes and costs were collected for the perioperative period. Hospital operating costs were grouped by hospitalization/operative procedure, transfusions, reoperations, and residual events (health care interactions).
Results
One hundred and one open posterior lumbar interbody fusion (Open group) and 109 MIS patients were treated primarily for stenosis coupled with instability (39.6% and 59.6%, respectively). Mean total hospital costs were $27,055.53 for the Open group and $24,320.16 for the MIS group. This represents a statistically significant cost savings of $2,825.37 (10.4% [95% confidence interval: $522.51–$5,128.23]) when utilizing MIS over traditional Open techniques. Additionally, residual events, complications, and blood transfusions were significantly more frequent in the Open group, compared to the MIS group.
Conclusions/level of evidence
Utilizing minimally invasive techniques for instrumented spinal fusion results in decreased hospital operating costs compared to similar open procedures in the early perioperative period. Additionally, patient benefits of minimally invasive techniques include significantly less blood loss, shorter hospital stays, lower complication rate, and a lower number of residual events. Long-term outcome comparisons are needed to evaluate the efficacy of the two treatments. Level of evidence: III
Clinical relevance
This work represents a true cost-of-operating comparison between open and MIS approaches for lumbar spine fusion, which has relevance to surgeons, hospitals and payers in medical decision-making.
Keywords: lumbar, degenerative, complications, MIS, residual events
Introduction
The evolution of spinal surgery over the past two decades has resulted in, and been driven by, a rapid expansion of the role of technology in the treatment of a wide variety of spinal maladies.1–5 Much controversy exists regarding the effectiveness of many interventions, although the treatment of degenerative conditions with instrumented fusion appears to have been validated in long-term studies showing positive outcomes5,6 over conservative care.2,7 As with all surgical specialties, there has been a focus on improving outcomes and decreasing morbidity. In response, surgeons have driven operative technique improvements towards minimally disruptive options to decrease soft tissue damage and hasten postoperative recovery.8 Although minimally invasive techniques have demonstrated decreased recovery time and procedural morbidities compared to open approaches with similar outcomes,8–10 these techniques are typically associated with higher instrumentation costs.11 In light of this, the drive for less invasive spine surgery is proceeding in tandem with continually stronger evidence requirements for both clinical and financial viability by those making utilization decisions.12 Similar assessments have been made in total knee and hip arthroplasty, with strong evidence of cost-effectiveness shown for quality of life gained over time,13,14 providing justification for increased costs as technological advances were made.
In the mid-nineties, simple decompressions were first shown to be cost-effective compared to medical management, based on cost per quality-adjusted life-year (QALY),15 with early reports of instrumented spinal fusion showing mixed cost-effectiveness.16,17 QALYs are typically calculated as interventional and incremental cost against improvements in quality of life over time, with costs based on reimbursement or the charged amount.18 In the United States, $100,000 per QALY gained is considered the threshold for cost-effectiveness.15,18 Cost-effectiveness of instrumented spinal fusion has since been validated, despite early mixed results, in several high quality studies.19–22 Tosteson et al and Glassman et al19–21 in particular, have shown cost per QALY at 4 and 5 years after instrumented fusion at $54,000 and $53,914, respectively, far below the national cost-effectiveness threshold.18,23 QALY analyses have shown the utility of procedure classes (decompressions and fusions),15,16,19–21 but direct comparisons of different exposure types within the classes are less common. In current practice, spinal fusion procedures are regularly carried out using both open and minimally invasive exposures, and several recent studies have shown clinical and cost benefits using minimally invasive, over open techniques, with cost assessed using charge or reimbursement data.8,9
While the “cost” of medical interventions is often lamented, the costs associated with performing these interventions are less well understood. In this case, cost represents price, which simply requires knowing the amount paid for an intervention. The amount charged for a procedure is commonly reimbursed at only a fraction of the total, so does not represent actual cost,12 but is commonly used as charge information that is more readily available. Determining costs, on the other hand, includes calculating man-hours, overheads, supply costs and utilization, as well as technical fees. Due to the high volume of interactions a patient has during even routine hospitalization, calculation of such costs in large samples is near prohibitively laborious.
The current study seeks to address the initial value of minimally invasive procedures by comparing the real costs an institution incurs when performing either a minimally invasive or an open procedure for two-level instrumented lumbar fusion, from the time of index hospitalization through 45 days postoperative (perioperative period). Our hypothesis was that patients treated with a minimally invasive approach would have lower per patient overall costs, with significantly fewer and less costly residual events, transfusions, and reoperations during the perioperative period, compared to those treated with an open approach. Additionally, treatment variables (intraoperative blood loss, operating room time, and length of hospital stay) were hypothesized to be lower in the minimally invasive group, due to the nature of the approach.
Materials and methods
In the middle part of this decade, the Spinal Surgery Service at St Mary’s Health Center (Jefferson City, MO) transitioned from using open posterior lumbar interbody fusion with pedicle screws to a minimally invasive spine surgery (MIS) platform, using lateral transpsoas interbody fusion at all spinal levels above L45 and transsacral or minimally invasive transforaminal interbody fusion at L5–S1 with minimally invasive pedicle screws. We have previously reported complications and outcomes in our experience with MIS fusion and have described the technique in detail.24–31
Following Institutional Review Board approval, we elected to study all patients treated at our institution for degenerative spinal conditions with an instrumented, two-level lumbar interbody fusion, from 2005 to 2009. Patients were grouped based on whether or not they were treated with open or minimally invasive techniques, referred to herein as Open and MIS groups. Data on demographics, comorbidity, diagnosis, and treatment were collected prospectively in the form of a registry that spanned the open and MIS periods. Residual events, however, were collected prospectively only for the MIS group, while the open group required retrospective review to populate residual events fields. Costs during the perioperative period were collected retrospectively from our institution (St Mary’s Health Center, a 160 bed community hospital) and included a rigorous adjudication process that captured actual hospital operating costs, direct patient costs, and operating overhead. Through an agreement with the hospital, these costs were determined from hospital revenue coding matched to line-item events for each patient, adjusted for inflation to 2009 dollars.
Perioperative costs were divided into four groups: the index surgical procedure and initial hospital stay (original procedure); transfusions; reoperations; and residual events. Cost analyses were performed on the four cost categories, combined and separately. The original procedure category included all costs associated with the operation and basic postoperative hospitalization. In this category, costs were further itemized and grouped into eight categories: implants and instrumentation; operating room services; surgical supplies; room and board; medications; laboratory; physical and occupational therapy; and miscellaneous. The transfusion category included the costs related to patient typing, crossmatching, and autologous donation. Reoperation costs were collected in the same manner as original procedure costs. Residual events were defined as any event that generated a cost, excluding the index procedure and hospital stay, transfusion, or reoperation that occurred during the perioperative period. These primarily included emergency room visits, hospital readmissions (excluding reoperations), postoperative rehabilitation, and additional diagnostics.
Statistical methods
Frequency analyses were used to characterize demographic, treatment, and cost data. Independent-samples t-tests were used to compare means, while chi-square tests were performed to characterize categorical differences. The level of significance was considered, for all analyses, at P < 0.05. Statistical analyses were carried out using SPSS software (v. 18.0.0; SPSS Inc, Chicago, IL).
Results
In total, 210 consecutive patients were identified as having undergone instrumental two-level lumbar fusion at our institution between 2005 and 2009. Of those, 101 were treated with an open approach and 109 were treated with an MIS approach. The mean age of the MIS and Open groups were statistically significantly different at 64.1 years and 58.0 years, respectively (F(1,208) = 0.006; P < 0.001). The Open and MIS groups were 55% (56) and 56% (61) female with a mean BMI of 31.2 (range 17.2–53.8) and 30.6 (range 17.0–46.0), respectively.
Stenosis was the most common primary diagnosis for both groups (Open, 40%; MIS, 60%), with low-grade spondylolisthesis comprising 14% and 16% of the Open and MIS groups, respectively. In total, 94 baseline comorbidities were present in the Open group (0.93 average per patient), the most common of which were tobacco use (40%), coronary artery disease (CAD; 20%), and diabetes mellitus (21%). The MIS group had 142 total comorbidities (1.3 average per patient), the most common of which were CAD (50%) and tobacco use (29%). Thirty-seven (37%) patients in the Open group and 32 (29%) in the MIS group had undergone prior lumbar spine surgery. Complete demographic information is included in Table 1.
Table 1.
Patient demographics
| Characteristic | Statistic | P | |
|---|---|---|---|
|
|
|||
| Open two-level PLIF n = 101 |
MIS two-level XLIF n = 109 |
||
| Mean age in years (SD) | 58.0 (12.0) | 64.1 (12.5) | <0.001 |
| Female (%) | 56 (55.4) | 61 (56.0) | 1.000 |
| Mean body mass index (SD) | 31.2 (6.6) | 30.6 (5.8) | 0.534 |
| Comorbidities (mean number per patient) | 94 (0.93) | 142 (1.3) | <0.001 |
| Comorbidity type | |||
| Tobacco use (%) | 40 (39.6) | 32 (29.4) | 0.156 |
| Coronary artery disease (%) | 21 (20.8) | 55 (50.5) | <0.001 |
| Diabetes (%) | 20 (19.8) | 25 (22.9) | 0.700 |
| Chronic obstructive pulmonary disease (%) | 5 (5.0) | 3 (2.8) | 0.638 |
| Any prior lumbar surgery (%) | 37 (36.6) | 31 (28.4) | 0.330 |
| Prior surgery type | n = 37 | n = 31 | |
| Discectomy (%) | 16 (43.2) | 12 (38.7) | 0.409 |
| Laminectomy (%) | 6 (16.2) | 7 (22.6) | 1.000 |
| Fusion (%) | 13 (35.1) | 11 (35.5) | 0.678 |
| ALIF (%) | 0 (0) | 1 (3.2) | 1.000 |
| PLF (%) | 2 (5.4) | 0 (0) | 0.444 |
| Diagnoses | – | ||
| Stenosis (%) | 40 (39.6) | 65 (59.6) | 0.006 |
| Spondylolisthesis (%) | 14 (13.9) | 17 (15.6) | 0.829 |
| Postlaminectomy syndrome (%) | 16 (15.8) | 8 (7.3) | 0.086 |
| DDD (%) | 14 (13.9) | 9 (8.3) | 0.281 |
| Herniated nucleus pulposus (%) | 10 (9.9) | 4 (3.7) | 0.126 |
| Degenerative scoliosis (%) | 17 (6.9) | 5 (4.6) | 0.079 |
| Infection (%) | 0 (0.0) | 1 (0.9) | 1.000 |
Notes: Demographic information for the two cohorts: those treated either an open PLIF or MIS XLIF approach for two-level instrumented lumbar interbody fusion.
Abbreviations: SD, standard deviation; MIS, minimally invasive spine surgery; XLIF, extreme lateral interbody fusion; PLIF, posterior lumbar interbody fusion; ALIF, anterior lumbar interbody fusion; PLF, posterolateral fusion; DDD, degenerative disc disease.
Patients were treated in the Open group in a total of 202 levels, mostly at L3–4 (23.8%), L4–5 (43.6%), and L5–S1 (25.2% of total levels). Of 218 total levels treated in the MIS group, the most commonly treated levels were L3–L4 (35.3%), L4–L5 (33.9%), and L5–S1 (11.9% of total levels). Blood hemoglobin (Hgb) decreased in both groups postoperatively, with a 3.1 g mean change for Open patients and 1.6 g for MIS patients. This 50% greater decrease in Hgb for the Open group was statistically significantly greater compared to the MIS group (F(1,208) = 5.312; P < 0.001). Mean operative time was 156.5 and 163.2 minutes for the Open and MIS groups, respectively (F(1,208) = 11.42; P = 0.184). Additionally, the average length of hospital stay was significantly less for MIS patients (1.2 vs 3.2 days) (F(1,208) = 25.570; P < 0.001) (Table 2).
Table 2.
Treatment summary
| Characteristic | Statistic | P | |
|---|---|---|---|
|
|
|||
| Open two-level PLIF n = 101 |
MIS two-level XLIF n = 109 |
||
| Total levels treated | 202 | 218 | – |
| Levels treated | |||
| T12–L2 (%) 1 | (1.0) | 0 (0) | |
| L1–L3 (%) | 1 (1.0) | 6 (5.5) | |
| L2–L4 (%) | 11 (10.9) | 29 (26.6) | – |
| L3–L5 (%) | 37 (36.6) | 48 (44.0) | – |
| L4–S1 (%) | 51 (50.5) | 26 (23.9) | – |
| Mean operative time (mins), (SD) | 156.5 (25.7) | 162.3 (35.8) | 0.178 |
| Mean postoperation change in hemoglobin (g), (SD) | 3.10 (1.2) | 1.56 (0.9) | <0.001 |
| Mean hospital stay (days), (SD) | 3.2 (1.7) | 1.2 (0.5) | <0.001 |
| Total complications (%) | 14 (13.9) | 5 (5.5) | 0.036 |
| Infections (%) | 3 (2.9) | 0 (0) | 0.219 |
| Transfusions (%) | 18 (17.8) | 1 (0.9) | <0.001 |
Notes: Treatment and radiographic fusion status data for patients treated with either an open or MIS approach for two-level instrumented lumbar interbody fusion. Where applicable, percentage differences between open and MIS groups are included.
Abbreviations: SD, standard deviation; MIS, minimally invasive spine surgery; XLIF, extreme lateral interbody fusion; PLIF, posterior lumbar interbody fusion; ALIF, anterior lumbar interbody fusion.
Complications were significantly more frequent in the Open group compared to the MIS group through the perioperative period (14 [14%] and 6 [6%] respectively, Yates’ chi- square = 4.410, P = 0.036). Postoperative infections occurred in three (3%) Open patients, with none (0%) in the MIS group.
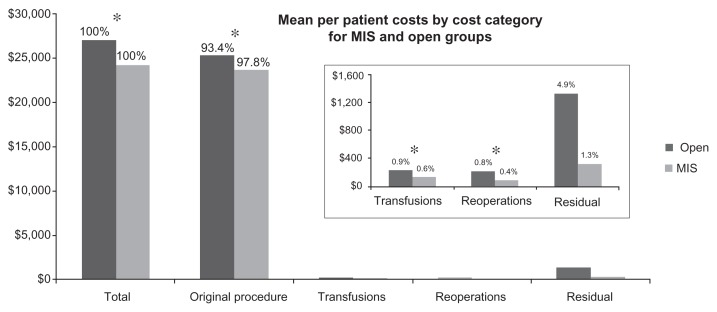
Total Open (101 patients) and MIS (109 patients) group costs were $2,732,608.75 and $2,641,087.75, respectively, or $27,055.53 and $24,230.16 per patient, respectively, for the perioperative period. The average savings for MIS over Open procedures was $2,825.37, or 10.4% of the total cost per patient, a statistically significant difference (F(1,208) = 4.854, P = 0.029; 95% confidence interval [CI] of the difference: $522.51–$5,128.23). Results for the four cost categories (original procedure, transfusions, reoperations, and residual events) are described in detail below (Figure 1).
Figure 1.
Chart showing mean per patient costs by category for minimally invasive (MIS) and open groups.
Note: *Denotes statistical significance, P < 0.05.
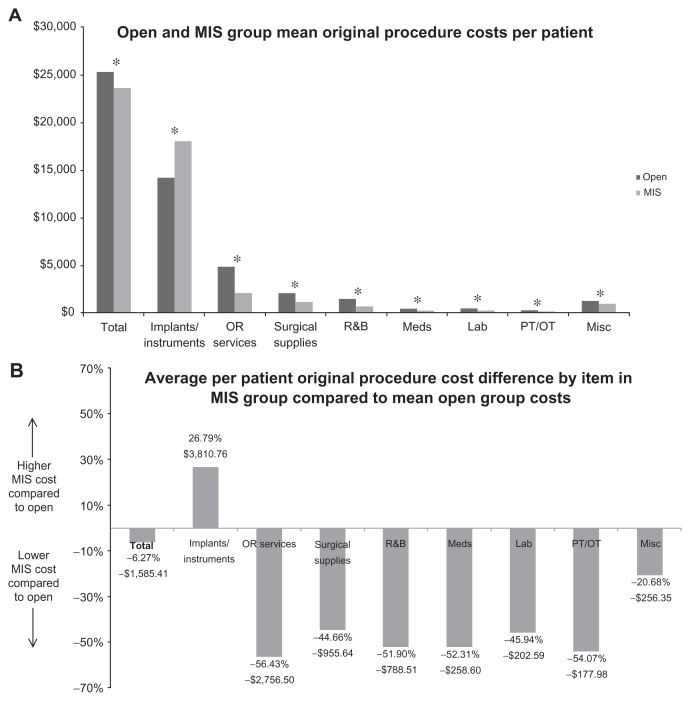
The total original procedure cost for the Open group (101 patients) was $2,552,503.48 and $2,581,871.77 for the MIS group (109 patients), which represented 94% and 98% of the total costs, respectively. Average per patient original procedure costs were significantly less for MIS than for Open patients, at $25,272.31 and $23,686.90 respectively, a $1,585.41 (6%) difference (F(1,208) = 3.107; P = 0.026; 95% CI: $193.19–$2,977.64). Comparisons of line item Open and MIS average per patient in-hospital costs showed MIS implant/instrumentation costs exceeding the Open group by $3,810.76 (27%), with operating room services, surgical supplies, and room and board costs less for the MIS group by $2,756.50 (56%), $955.64 (45%) and $788.51 (52%) respectively. Complete itemized original procedure costs are included in Figure 2A and B.
Figure 2.
(A) Average open and minimally invasive (MIS) line item original procedure costs. (B) Average percent difference between open and minimally invasive (MIS) groups for line item index hospitalization costs.
Note: *Denotes statistical significance, P < 0.05.
Abbreviations: OR, open residual; PT/OT, physical therapy/occupational therapy; R&B, room and board (Hospital stay costs).
Eighteen (18%) transfusions occurred in the Open group, with only one (1%) in the MIS group, a statistically significant difference (Yates’ chi-square = 16.208; P < 0.001). Per patient transfusion costs were also significantly lower for the MIS compared to the Open group at $211.52 and $133.92, respectively (F(1,208) = 15.481; P < 0.001; 95% CI: $46.24–$139.10). A 55% higher cost in general inventory crossmatching was observed in the MIS group, with autologous crossmatching, and general inventory and autologous transfusion costs for Open patients exceeded those for MIS patients by 100%, 83%, and 100%, respectively. In total, transfusion costs accounted for 0.9% and 0.6% of total costs for the MIS and Open groups respectively.
Reoperations during the perioperative period were rare, with two (2%) instances in the Open group and one (1%) instance in the MIS group. In the Open group, one patient underwent two debridements and washes for a persistent deep wound infection, resulting in $22,040.00 in additional costs. In the MIS group, one patient underwent posterior decompression for herniated nucleus pulposus that resulted in a cost of $9,369.62 for the MIS group.
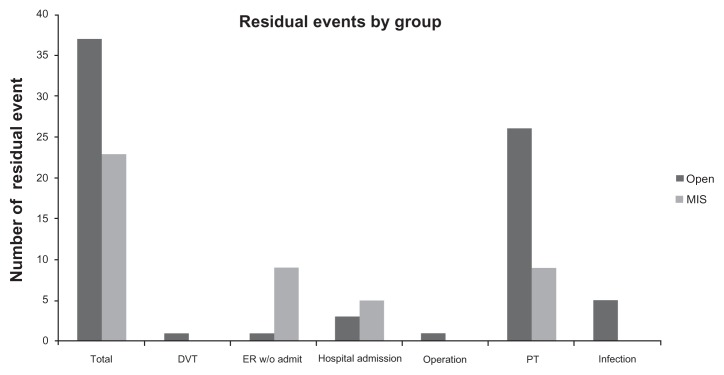
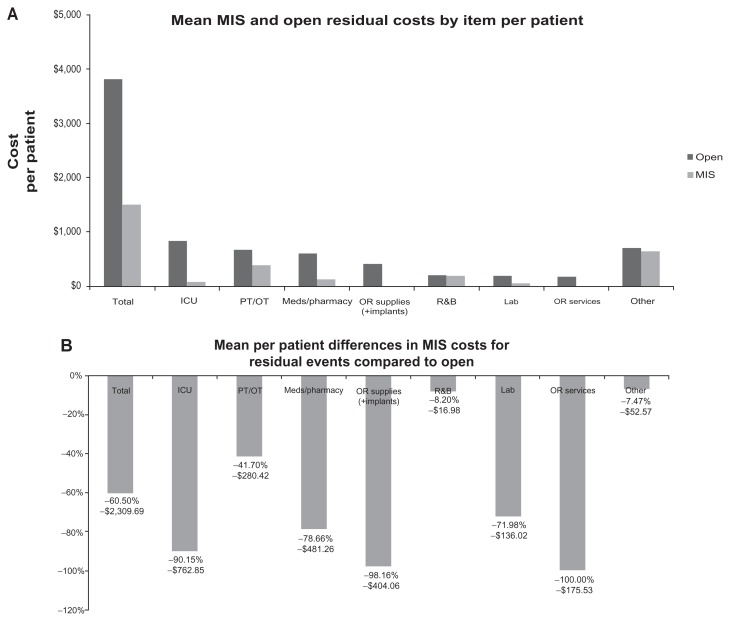
Perioperative residual events represented the most consequential cost category after the original procedure. A total of 37 (37%) residual events were observed in the Open group, with 23 (21%) in the MIS group, a statistically significant difference (Yates’ chi-square = 5.460; P = 0.019) (Figure 3). Residual events for the Open group included five hospital readmissions (three for severe pain, one for nausea/urine retention, and one for deep vein thrombosis); 26 physical therapy evaluations; five consultations for possible infections; and one operative procedure. For the MIS group, residual events included three hospital admissions (one each for ileus, pneumonia, and pulmonary embolism); 11 nonadmission emergency room visits for pain (8), esophageal reflux (2), and atrial fibrillation (1); and nine evaluations with physical therapy (Figure 3). Total costs for residual events in the Open and MIS groups were $134,652.27 and $34,677.33, respectively, which represented cost savings of $99,974.94 overall, and $2,131.54 (58.6%) per patient experiencing a residual event, in the MIS compared to the Open group (95% CI: $–653.11–$2,683.21). Itemized listings and comparisons of costs between Open and MIS groups for residual events are included in Figure 4A and B.
Figure 3.
Number of residual events observed for open and minimally invasive (MIS) groups.
Note: *Denotes statistical significance, P < 0.05.
Abbreviations: ER, emergency room; DVT, deep venous thrombosis; PT, physical therapy.
Figure 4.
(A) Average open and residual line-item costs for open and minimally invasive (MIS) groups. (B) Average percent difference between open and minimally invasive (MIS) groups for line item residual costs.
Abbreviations: ICU, intensive care unit; OR, open residual; R&B, room and board (Hospital stay costs).
Discussion
The purpose of this study was to collect comprehensive institutional costs for patients treated with two-level, instrumented spinal fusion and to compare the results based on the extent of exposure to the approach: minimally invasive or open. Of the four cost categories examined (original procedure, transfusions, reoperations, and residual events), per patient costs were greater in the Open, compared to the MIS group. Residual events, for those who experienced them, showed the greatest per patient relative difference in costs, with Open patients on average incurring $2,131.54 greater institutional costs than MIS patients, though without statistical significance. This lack of significance may be the result of small samples and widely variable costs per event, as residual events did not occur in all patients, nor did they occur with the same frequency in both groups. As an example, a single outlying residual event in the open group resulted in an extended hospitalization and a total cost of $83,739.90. The difference in number of residual events, however, was statistically significant, with fewer occurring in the MIS group. Transfusion costs were significantly greater per patient and in frequency in the Open group, though the difference in cost was small compared to the total (0.9% and 0.6% for Open and MIS, respectively). In total, MIS procedures resulted in statistically significant 10.4% ($2,825.37 per patient) cost savings over Open procedures. Based on these results, we reject the null hypothesis, that total and categorical costs as well as number of residual events would not be statistically different for all measurements (cost and frequency), except for number and cost of reoperations and per patient costs for residual events. Our secondary endpoints, to evaluate operative variables and the resultant length of hospital stay, showed significant decreases in blood loss and length of hospital stay for MIS patients, with no difference in operating room time.
The unfortunate reality of spinal surgery, and all surgery in general, is that complications occur despite the best endeavors.32 Procedures with higher blood loss and extended postoperative hospitalization are associated with increased risk of postoperative complication, namely infections. Those complications have a tendency to cascade, with mortality and costs increasing at each subsequent step.33,34 Baseline conditions, namely advanced age and the presence of multiple medical comorbidities, further exacerbate the likelihood and effects of in-hospital complications.33,35,36 In this study, despite a significantly older MIS cohort (58.0 vs 64.1 years), complications were more than twice as frequent for Open patients. This result contrasts with that of Kalanithi et al who in 2009 reported that patients aged 65 years and older were 70% more likely, when undergoing traditional spinal orthopedic surgery, to have complications when compared to those patients between 44 and 65 years.33
In this study, operating room time, Hgb change, and length of hospital stay measurements were used to infer differences in the extent of soft tissue disruption between the minimally invasive and open approaches used.8 While mean operating room time was similar for the groups (157 and 162 minutes), mean Hgb change and length of stay were 50% and 63% less for MIS patients, respectively, showing surgical efficiency with respect to surrounding soft tissue and postoperative recovery. We had anticipated that the MIS patients would have shorter operating room times than the Open patients, though this lack of difference is likely due to the added time required for repositioning MIS patients.
Transfusions in spinal orthopedic procedures are common, with rates commonly ranging from 50% to 81% of cases in the literature.37 Elevated intraoperative blood loss and the use of transfusions are correlated with increased complications and postoperative infections.38–40 We observed significantly higher blood loss, significantly more transfusions, and elevated per patient transfusion costs for Open compared to MIS patients, with higher rates of postoperative residual events and infections in the Open group. While absolute per patient cost savings for MIS over Open were only $72.35, all patients in both groups were typed and crossmatched for donors, which is now only performed on a case-by-case basis for MIS patients, due to the infrequent need for transfusion. Eliminating typing and crossmatching protocols for MIS patients would bring total savings for MIS over Open transfusion costs to $206.48.
Costs of postoperative hospitalization are skewed towards the first 3 days of the postoperative period, with decreases in length of stay under that threshold having the greatest impact on overall cost.41 Our results, showing in-hospital recovery for MIS patients being significantly shorter (3.2 days Open; 1.2 days MIS) with fewer residual events, support those findings, as well as the benefits of decreasing in-hospital recovery time through minimally disruptive techniques.
Residual events, whether surgical complications or basic medical follow-up needs, were significantly more common in Open compared to MIS patients and, on average, were more costly per event. There was a 41% decrease in number and 59% decrease in cost per residual event for MIS patients, representing an institutional cost savings of $2,131.54 per residual event, or $1,015.05 per patient across all patients treated. Residual events are yet another indirect measure of procedural impact on patients, with patients treated with a minimally invasive approach experiencing significantly fewer medical encounters.
The purpose of this study was to study costs specifically, as opposed to health utility indices such as QALY, in an effort to characterize where actual costs lie and where they differ between minimally invasive and openly treated spinal fusion procedure patients. In this respect, we believe that we have been successful in executing the study design. We have shown the cost and clinical benefits for institutions and for patients in using minimally invasive over open techniques.
There were several weaknesses in this paper, namely that patient data were collected in the form of a registry, without randomization. Despite this, several elements of homogeneity were present, including all patients having been treated at a single institution by the same immediate staff under consistent hospital procedures, care pathways, and protocols. The two patient groups were fairly similar but, as mentioned previously, did differ in age (the MIS group was older), prevalence of comorbidities (more common in the MIS group), and incidence of prior surgery (38% in the open group against 29% in the MIS cohort). Any of these differentiators could predispose one group to a greater risk of complications or residual events but, interestingly, two of the higher risk predisposing factors (age, medical comorbidities) fell in the MIS group while the other (incidence of prior surgery) fell in the Open cohort. While the effects may offset one another, there is no way to be certain what the effect might be.
Another weakness is that Open and MIS procedures differed in both the extent of exposure and the technique of the procedure. Specifically, the differences between MIS and Open approach procedures and the instrumentation that they use may have also impacted costs, rather than the differences being due solely to the extent of exposure. While this is a concern, the significant differences in original procedure variables in favor of the MIS technique suggest that the morbidities associated with the extent of exposure were the salient factor impacting cost, despite the MIS procedures often requiring additional incisions for posterior instrumentation. Additionally, evidence of radiographic fusion at 12 months between the two groups was not statistically different, which potentially indicates similarities in long-term outcomes of the techniques and, thus, similarities in their ability to treat the underlying pathologies. Data on long-term fusion rates of MIS procedures in comparison to their open counterparts are still being collected. Assessment of postprocedural differences in incidence of pseudarthrosis or adjacent segment disease could significantly affect the economic impact of MIS procedures. Preliminary observations at 1 and 2 years are so far favorable towards maintaining the economic efficiency of MIS surgery.
The cost-effectiveness of orthopedic spinal surgery has been proven.8,16,19–21 As these interventions continue to be refined through technological innovation, however, they will have a similarly rigorous scrutiny of value. This value basis should, in our argument, account for QALY as well as the actual costs to institutions, to avoid mismatching between reimbursements and costs and to ensure the long-term financial viability of medical institutions. This mismatch is seen in recent reports showing that approximately 50% of hospitals in the United States are operating at a loss, in part due to reimbursements not covering costs.42 In this study, the statistically significant cost savings using MIS over Open procedures of $2,825.37 (10.4%) may seem small compared to the total cost. However, if the benefit of minimally invasive over open techniques seen in this study is shown in other surgical fields, implementation on a society-wide basis may have profound impacts on collective institutional costs.
Lastly, the authors note that we have previously discussed this information in the form of an editorial in another journal.43 That article, based on a preliminary review of the data presented here in more detail, reported a difference of $2,563 per patient (9.6%) between the two cohorts. Our more complete evaluation resulted in the revised figure of $2,825 per patient.
Footnotes
Disclosure
Dr WB Rodgers receives royalties from and is a consultant for a company with instrumentation utilized in patients in the study. The other authors report no conflicts of interest in this work.
References
- 1.Turner JA, Ersek M, Herron L, et al. Patient outcomes after lumbar spinal fusions. JAMA. 1992;268(7):907–911. [PubMed] [Google Scholar]
- 2.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical versus nonsurgical treatment for lumbar degenerative spondylolisthesis. N Engl J Med. 2007;356(22):2257–2270. doi: 10.1056/NEJMoa070302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cahill KS, Chi JH, Day A, et al. Prevalence, complications, and hospital charges associated with use of bone-morphogenetic proteins in spinal fusion procedures. JAMA. 2009;302(1):58–66. doi: 10.1001/jama.2009.956. [DOI] [PubMed] [Google Scholar]
- 4.Deyo RA, Ciol MA, Cherkin DC, et al. Lumbar spinal fusion. A cohort study of complications, reoperations, and resource use in the Medicare population. Spine. 1993;18(11):1463–1470. [PubMed] [Google Scholar]
- 5.Glassman SD, Carreon LY, Djurasovic M, et al. Lumbar fusion outcomes stratified by specific diagnostic indication. Spine J. 2009;9(1):13–21. doi: 10.1016/j.spinee.2008.08.011. [DOI] [PubMed] [Google Scholar]
- 6.Penta M, Fraser RD. Anterior lumbar interbody fusion. A minimum 10-year follow-up. Spine. 1997;22(20):2429–2434. doi: 10.1097/00007632-199710150-00021. [DOI] [PubMed] [Google Scholar]
- 7.Weinstein JN, Lurie JD, Tosteson TD, et al. Surgical compared with nonoperative treatment for lumbar degenerative spondylolisthesis. Four-year results in the Spine Patient Outcomes Research Trial (SPORT) randomized and observational cohorts. J Bone Joint Surg Am. 2009;91(6):1295–1304. doi: 10.2106/JBJS.H.00913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wang MY, Cummock MD, Yu Y, et al. An analysis of the differences in the acute hospitalization charges following minimally invasive versus open posterior lumbar interbody fusion. J Neurosurg Spine. 2010;12(6):694–699. doi: 10.3171/2009.12.SPINE09621. [DOI] [PubMed] [Google Scholar]
- 9.Gray R, Fehlings M, Massicotte E, et al. Direct economic impact of posterior minimally invasive compared to conventional open fusion procedures for lumbar spondylolisthesis. Spine J. 2009;9(10):48S. doi: 10.1016/j.esas.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dhall SS, Wang MY, Mummaneni PV. Clinical and radiographic comparison of mini-open transforaminal lumbar interbody fusion with open transforaminal lumbar interbody fusion in 42 patients with long-term follow-up. J Neurosurg Spine. 2008;9(6):560–565. doi: 10.3171/SPI.2008.9.08142. [DOI] [PubMed] [Google Scholar]
- 11.Gerszten PC, Welch WC. Spine: minimally invasive techniques. Prog Neurol Surg. 2006;19:135–151. doi: 10.1159/000095188. [DOI] [PubMed] [Google Scholar]
- 12.Deyo RA, Mirza SK, Martin BI, et al. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010;303(13):1259–1265. doi: 10.1001/jama.2010.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Laupacis A, Bourne R, Rorabeck C, et al. The effect of elective total hip replacement on health-related quality of life. J Bone Joint Surg Am. 1993;75(11):1619–1626. doi: 10.2106/00004623-199311000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Rorabeck CH, Murray P. Cost effectiveness of revision total knee replacement. Instr Course Lect. 1997;46:237–240. [PubMed] [Google Scholar]
- 15.Malter AD, Larson EB, Urban N, et al. Cost-effectiveness of lumbar discectomy for the treatment of herniated intervertebral disc. Spine. 1996;21(9):1048–1054. doi: 10.1097/00007632-199605010-00011. [DOI] [PubMed] [Google Scholar]
- 16.Tosteson AN, Skinner JS, Tosteson TD, et al. The cost effectiveness of surgical versus nonoperative treatment for lumbar disc herniation over two years: evidence from the Spine Patient Outcomes Research Trial (SPORT) Spine. 2008;33(19):2108–2115. doi: 10.1097/brs.0b013e318182e390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kuntz KM, Snider RK, Weinstein JN, et al. Cost-effectiveness of fusion with and without instrumentation for patients with degenerative spondylolisthesis and spinal stenosis. Spine. 2000;25(9):1132–1139. doi: 10.1097/00007632-200005010-00015. [DOI] [PubMed] [Google Scholar]
- 18.Laupacis A, Feeny D, Detsky AS, et al. How attractive does a new technology have to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. CMAJ. 1992;146(4):473–481. [PMC free article] [PubMed] [Google Scholar]
- 19.Glassman SD, Polly DW, Dimar JR, et al. The cost effectiveness of single-level instrumented posterolateral lumbar fusion at five years after surgery. Spine. 2012;37(9):769–774. doi: 10.1097/BRS.0b013e3181e03099. [DOI] [PubMed] [Google Scholar]
- 20.Tosteson AN, Lurie JD, Tosteson TD, et al. Surgical treatment of spinal stenosis with and without degenerative spondylolisthesis: cost-effectiveness after 2 years. Ann Intern Med. 2008;149(12):845–853. doi: 10.7326/0003-4819-149-12-200812160-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tosteson AN, Tosteson TD, Lurie JD, et al. Factors affecting 4-year cost-effectiveness of surgery for stenosis with or without degenerative spondylolisthesis in the Spine Patient Outcomes Research Trial (SPORT) [abstract] Spine. 2010 Oct;:62. Affiliated Society Meeting Abstracts. [Google Scholar]
- 22.Rasanen P, Ohman J, Sintonen H, et al. Cost-utility analysis of routine neurosurgical spinal surgery. J Neurosurg Spine. 2006;5(3):204–209. doi: 10.3171/spi.2006.5.3.204. [DOI] [PubMed] [Google Scholar]
- 23.Laupacis A, Feeny D, Detsky AS, et al. Tentative guidelines for using clinical and economic evaluations revisited. CMAJ. 1993;148(6):927–929. [PMC free article] [PubMed] [Google Scholar]
- 24.Rodgers WB, Cox CS, Gerber EJ. Early complications of extreme lateral interbody fusion in the obese. J Spinal Disord Tech. 2010;23(6):393–397. doi: 10.1097/BSD.0b013e3181b31729. [DOI] [PubMed] [Google Scholar]
- 25.Rodgers WB, Cox CS, Gerber EJ. Experience and early results with a minimally invasive technique for anterior column support through extreme lateral interbody fusion (XLIF®) US Musculoskeletal Review. 2007;(1):28–32. [Google Scholar]
- 26.Rodgers WB, Gerber EJ, Patterson JR. Fusion after minimally disruptive anterior lumbar interbody fusion: analysis of extreme lateral interbody fusion by computed tomography. SAS J. 2010;4(2):63–66. doi: 10.1016/j.esas.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rodgers WB, Gerber EJ. Clinical and radiographic outcome in less invasive lumbar fusion: XLIF at one year follow-up. 2010. Submitted for publication. [Google Scholar]
- 28.Rodgers WB, Gerber EJ, Rodgers JA. Lumbar fusion in octogenarians: The promise of minimally invasive surgery. Spine. 2010;35(26S):S355–S360. doi: 10.1097/BRS.0b013e3182023796. [DOI] [PubMed] [Google Scholar]
- 29.Rodgers WB, Gerber EJ, Patterson JR. 2010. Grade 2 spondylolisthesis at L4–5 treated by XLIF: safety and mid-term results in the “worst case scenario”. Submitted for publication. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rodgers WB, Gerber EJ, Patterson JR. Intraoperative and early postoperative complications in extreme lateral interbody fusion (XLIF): An analysis of 600 cases. Spine. 2011;36(1):26–32. doi: 10.1097/BRS.0b013e3181e1040a. [DOI] [PubMed] [Google Scholar]
- 31.Rodgers WB, Cox CS, Gerber EJ. Minimally invasive treatment (XLIF) of adjacent segment disease after prior lumbar fusions. [Accessed April 21, 2012];The Internet Journal of Minimally Invasive Spinal Technology [serial on the Internet] 2009 3(4) [about 6p.]. Available from: http://www.ispub.com/journal/the-internet-journal-of-minimally-invasive-spinal-technology/volume-3-number-4/minimally-invasive-treatment-xlif-of-adjacent-segment-disease-after-prior-lumbar-fusions.html. [Google Scholar]
- 32.Andersson GB, Chapman JR, Dekutoski MB, et al. Do no harm: the balance of “beneficence” and “non-maleficence”. Spine. 2010;35(Suppl 9):S2–S8. doi: 10.1097/BRS.0b013e3181d9c5c5. [DOI] [PubMed] [Google Scholar]
- 33.Kalanithi PS, Patil CG, Boakye M. National complication rates and disposition after posterior lumbar fusion for acquired spondylolisthesis. Spine. 2009;34(18):1963–1969. doi: 10.1097/BRS.0b013e3181ae2243. [DOI] [PubMed] [Google Scholar]
- 34.Khan NA, Quan H, Bugar JM, et al. Association of postoperative complications with hospital costs and length of stay in a tertiary care center. J Gen Intern Med. 2006;21(2):177–180. doi: 10.1111/j.1525-1497.2006.00319.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dekutoski MB, Norvell DC, Dettori JR, et al. Surgeon perceptions and reported complications in spine surgery. Spine. 2010;35(Suppl 9):S9–S21. doi: 10.1097/BRS.0b013e3181d830de. [DOI] [PubMed] [Google Scholar]
- 36.Dettori JR, Norvell DC, Dekutoski M, et al. Methods for the systematic reviews on patient safety during spine surgery. Spine. 2010;35(Suppl 9):S22–S27. doi: 10.1097/BRS.0b013e3181d70494. [DOI] [PubMed] [Google Scholar]
- 37.Elgafy H, Bransford RJ, McGuire RA, et al. Blood loss in major spine surgery: are there effective measures to decrease massive hemorrhage in major spine fusion surgery? Spine. 2010;35(Suppl 9):S47–S56. doi: 10.1097/BRS.0b013e3181d833f6. [DOI] [PubMed] [Google Scholar]
- 38.Rampersaud YR, Moro ER, Neary MA, et al. Intraoperative adverse events and related postoperative complications in spine surgery: implications for enhancing patient safety founded on evidence-based protocols. Spine. 2006;31(13):1503–1510. doi: 10.1097/01.brs.0000220652.39970.c2. [DOI] [PubMed] [Google Scholar]
- 39.Schuster JM, Rechtine G, Norvell DC, et al. The influence of perioperative risk factors and therapeutic interventions on infection rates after spine surgery: a systematic review. Spine. 2010;35(Suppl 9):S125–S137. doi: 10.1097/BRS.0b013e3181d8342c. [DOI] [PubMed] [Google Scholar]
- 40.O’Toole JE, Eichholz KM, Fessler RG. Surgical site infection rates after minimally invasive spinal surgery. J Neurosurg Spine. 2009;11(4):471–476. doi: 10.3171/2009.5.SPINE08633. [DOI] [PubMed] [Google Scholar]
- 41.Taheri PA, Butz DA, Greenfield LJ. Length of stay has minimal impact on the cost of hospital admission. J Am Coll Surg. 2000;191(2):123–130. doi: 10.1016/s1072-7515(00)00352-5. [DOI] [PubMed] [Google Scholar]
- 42.Pickens G. About 50% of hospitals in the red for Q3, profit margin falling. Thomson Reuters; Mar, 2010. [Accessed on March 2010]. Available from: http://www.reuters.com/article/2009/08/19/us-hospitals-usa-idUSTRE57I0IS20090819. [Google Scholar]
- 43.Deluzio KJ, Lucio JC, Rodgers WB. Editorial: Value and cost in less invasive spinal fusion surgery: lessons from a community hospital. SAS J. 2010;4(2):37–40. doi: 10.1016/j.esas.2010.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]