Abstract
Background
Trauma teams improve the initial management of trauma patients. Optimal timing of trauma alerts could improve team preparedness and performance while also limiting adverse ripple effects throughout the hospital. The purpose of this study was to evaluate how timing of trauma team activation and notification affects initial in-hospital management of trauma patients.
Methods
Data from a single hospital trauma care quality registry were matched with data from a trauma team alert log. The time from patient arrival to chest X-ray, and the emergency department length of stay were compared with the timing of trauma team activations and whether or not trauma team members received a preactivation notification.
Results
In 2009, the trauma team was activated 352 times; 269 times met the inclusion criteria. There were statistically significant differences in time to chest X-ray for differently timed trauma team activations (P = 0.003). Median time to chest X-ray for teams activated 15–20 minutes prearrival was 5 minutes, and 8 minutes for teams activated <5 minutes before patient arrival. Timing had no effect on length of stay in the emergency department (P = 0.694). We found no effect of preactivation notification on time to chest X-ray (P = 0.474) or length of stay (P = 0.684).
Conclusion
Proactive trauma team activation improved the initial management of trauma patients. Trauma teams should be activated prior to patient arrival.
Keywords: emergency medical service communication systems, trauma centers, patient care team
Background
Trauma patients constitute a heterogeneous group whose injury mechanisms and premorbidity require rapid and systematic diagnostic and therapeutic measures.1 Most Norwegian hospitals that receive severely injured patients have established predefined multidisciplinary trauma teams.2 As an integrated part of regionalized trauma systems such teams have been shown to improve outcomes of severely injured patients.3 However, trauma team activation can cause ripple effects throughout a hospital, as team members have to set other work aside. For instance, imaging resources and operating rooms can be put on hold in advent of the patient’s potential need for them. Hence, much research has focused on developing optimal criteria for activation of the trauma team.4–8
Whenever a patient en route to the hospital meets trauma team activation criteria, hospitals typically use a trauma alert system to notify all team members. The intention of such a system is to ensure that team members meet on time in the resuscitation room. Liberman et al demonstrated that prehospital notification led to lower odds of death, however the effect was only for patients with mild injuries (injury severity score < 12) and not for the more severely injured (injury severity score 12–75).9 Optimal timing of trauma alerts could improve team preparedness and performance while also limiting adverse ripple effects throughout the hospital. We are not familiar with any further research on trauma alert systems and how they affect the initial management of trauma patients. Thus, the objective of this study was to evaluate the effect of prehospital trauma team notification (TTN) and differently timed trauma team activation (TTA) on in-hospital trauma team performance. We hypothesized that both prehospital TTN and proactive TTA (trauma team is activated before patient arrives) would improve the initial management of trauma patients compared to no TTN and reactive TTA (trauma team is activated when or after patient arrives).
Methods
Design
We used data from a single hospital quality registry of trauma care to conduct a retrospective observational study of trauma team activation.
Study context
St Olav’s University Hospital is a 742-bed academic, tertiary trauma referral center, serving a mixed urban and rural regional population of approximately 646,000 people. In the region of mid-Norway, seven other hospitals also admit severely injured patients; however, these hospitals have no neurosurgical, cardiothoracic or pediatric surgical services. The regional emergency communication center (ECC) is located within the hospital and is responsible for the coordination of prehospital emergency medical services (EMS), as well as communication between pre- and in-hospital services. Basic prehospital care is provided by on-call general practitioners, ambulance crews, and paramedics. Whenever advanced life support is required, a crew consisting of paramedics and an anesthesiologist responds separately by helicopter or rapid-response car.
The ECC is staffed by trained nurses and paramedics who activate the trauma team when predefined criteria are met (Table 1). Predefined criteria are based on physiological variables, sustained anatomic abnormalities, and mechanisms of injury. The trauma team is one-tiered and consists of 12 mandatory members and additional facultative members.1
Table 1.
Trauma team activation criteria at St Olav’s University Hospital
| Physiological and anatomical criteria |
| Airway obstruction |
| Respiratory rate: >29 or <10 breaths/min |
| Systolic blood pressure: <90 mmHg |
| Glasgow Coma Scale of <14 and one criterion of mechanism of injury |
| Severe injury to two or more organ systems |
| Severe hemorrhage |
| Flail chest |
| Dislocated pelvic injury |
| Fracture to two or more long bones |
| Penetrating injury proximal to knee/elbow |
| Traumatic neurological injury |
| Crush injury/amputation proximal to wrist/ankle |
| Burns to body surface area of >15% in adults and >10% in children |
| Increased airway obstruction |
| Increased abnormal respiration |
| Increased cyanosis |
| Mechanisms of injury |
| Ejection from vehicle |
| Injury caused by electricity |
| Pedestrian run over or thrown over vehicle at impact |
| Children hit by vehicle at >30 km/h |
| Fall of >5 m, adults |
| Fall of >3 m, children |
| Fatality in same vehicle |
| Entrapment |
| Roll-over |
| Vehicle speed of >60 km/h |
| Vehicle compartment compressed by >30 cm or substantial deformation |
| Entrapment in avalanche |
| Hypothermia |
| Interfacility transfer |
| Transfer from other hospital within <24 hours of injury |
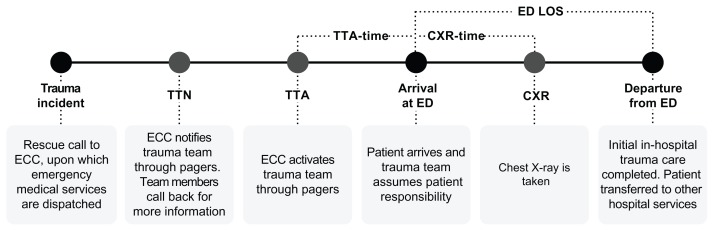
When a trauma incident occurs, the ECC informs and activates trauma team members by sending out two separate alerts on their pagers. The first alert is a TTN, sent out as soon as possible whenever trauma team criteria are met, usually after the prehospital EMS has arrived on scene. As a response to the TTN, team members call back to the ECC for more information about the incident. The intention of the TTN is to alert the involved clinicians in order to allow for timely preparations before the patient arrives. The second alert is the TTA. According to the hospital protocol, trauma team members should receive the second alert approximately 10 minutes before the patient arrives. This mandates immediate attendance in the resuscitation room. Rapid assessment and therapeutic measures according to trauma management principles are initiated upon arrival, including a structured physical examination, blood sampling, chest X-ray, and abdominal sonography.10,11 Figure 1 illustrates a typical trauma care process including the relevant time intervals for this study.
Figure 1.
Pre- and in-hospital trauma care process model including definition of time intervals.
Abbreviations: ED, emergency department; LOS, length of stay; TTN, trauma team notification; TTA, trauma team activation; CXR, chest X-ray; ECC, emergency call center.
Deviations from this typical chain of events may occur. For instance, the trauma incident may occur very close to the hospital, necessitating immediate TTA, leaving no time for first sending out a TTN. Sometimes transportation is faster or slower than expected, shortening or lengthening the expected 10-minute interval between the TTA and patient arrival. Occasionally patients might even arrive at the hospital before the TTA, and on arrival, trauma teams may, for some reason, choose not to follow the initial management protocol, for instance, not sending all patients for a chest X-ray.
Main measures
Data from the ECC paging service were matched with trauma registry data based on date and time of incident, alert pages, and patient arrival. The trauma registry consisted of manually registered data (first handwritten on paper during trauma team activation, and later manually entered into an electronic database), while the ECC paging service log was generated automatically. The primary outcome variable was time to chest X-ray (CXR-time). A secondary outcome variable was length of stay in the emergency department (ED LOS). Time intervals were calculated from patient arrival, but for situations where a patient arrived before the trauma team was activated, time was calculated from the TTA. This was performed to compare team performances (not ECC paging timeliness) between situations where the team was activated before or after patient arrival, that is, proactive and reactive TTAs. We excluded TTAs if the registry data did not permit calculation of dependent (neither CXR-time nor ED LOS) or independent (neither TTN nor TTA) variables. We also excluded multiple trauma patient instances as they usually had only one common TTN and TTA, and in such cases, hospital resources and prioritization mechanisms most likely had a significant impact on initial management.
Statistical analyses
Both outcome variables (CXR-time and ED LOS) were categorized as either efficient or inefficient. Threshold values were based on the median so that the number of efficient and inefficient teams was approximately equal. Independent variables were also categorized. Teams either did or did not receive a TTN in advance. TTAs were categorized into six groups based on the timing of the TTA in relation to patient arrival. We compared outcomes between groups using Pearson’s Chi-squared test. P-values less than 0.05 were considered statistically significant. Data analysis and graphical representations were done with statistical software (SPSS Statistics, Release 19.0.0.1; SPSS Inc, Chicago, IL) and spreadsheet software (Openoffice.org, version 3.2.1; Oracle Corporation, Redwood City, CA).
Ethics
The exported data from the quality registry did not contain any patient characteristics. The research protocol was presented to the regional research ethics committee, which regarded the project as a clinical audit not needing further approval.
Results
The trauma team was activated 352 times in 2009. Eighty- three of these times were excluded from our analysis, 72 of which involved multiple trauma patients, seven that had no documented time of patient arrival, three with no registration of TTN or TTA, and one with no registration of CXR-time or ED LOS, which left 269 for analysis (Table 2). Sixty-six percent of all TTAs were preceded by a TTN. Eleven patients (4%) arrived at the hospital before the trauma team was activated (reactive TTA).
Table 2.
Descriptive statistics from trauma team activations in 2009
| Total n = 269 |
Valid n | Median (minutes) | 25-percentile (minutes) | 75-percentile (minutes) |
|---|---|---|---|---|
| From incident to ED | 263 | 76.0 | 39.0 | 125.0 |
| From TTN to ED | 177 | 40.7 | 28.6 | 62.6 |
| From TTA to ED | 268 | 9.4 | 6.7 | 13.0 |
| CXR-time | 247 | 5.0 | 5.0 | 7.0 |
| ED LOS | 260 | 25.0 | 20.0 | 31.5 |
Abbreviations: ED, emergency department; TTN, trauma team notification; TTA, trauma team activation; CXR, chest X-ray; ED LOS, length of stay at the emergency department.
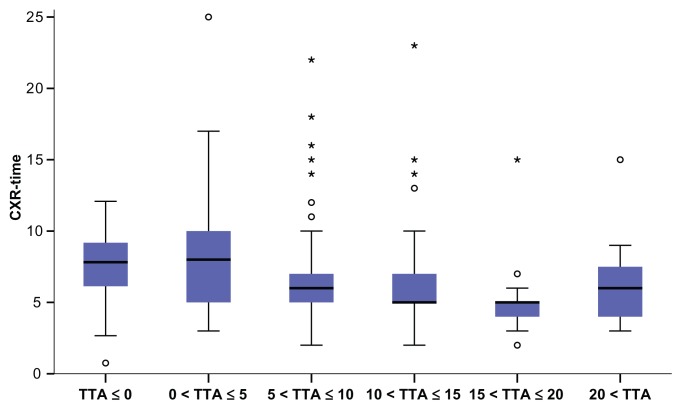
We found no association between TTN and CXR-time or ED LOS (Table 3). Similarly, timing of TTA was not associated with ED LOS, but there was a statistically significant association between the timing of TTA and CXR-time (Table 4). Box plots of this association demonstrated an inverse relationship between CXR-time and time from TTA to patient arrival, median CXR-time decreasing from 8 minutes to 5 minutes with increasing TTA time (Figure 2).
Table 3.
The effect of trauma team notification
| CXR-time | ED LOS | |||
|---|---|---|---|---|
|
|
|
|||
| ≤5 min | >5 min | ≤25 min | >25 min | |
| Without TTN | 45 | 38 | 45 | 44 |
| With TTN | 81 | 83 | 91 | 80 |
| Pearson’s Chi-squared | 0.474 | 0.684 | ||
| 0 cells (0%) have expected count less than 5. The minimum expected count is 40.66 | 0 cells (0%) have expected count less than 5. The minimum expected count is 42.45 | |||
Abbreviations: CXR, chest X-ray; LOS, length of stay; ED, emergency department; TTN, trauma team notification.
Table 4.
The effect of differently timed trauma team activations on CXR-time and ED LOS
| CXR-time | ED LOS | |||
|---|---|---|---|---|
|
|
|
|||
| ≤5 min | >5 min | ≤25 min | >25 min | |
| TTA–time ≤ 0 min | 2 | 7 | 6 | 5 |
| TTA–time 0.01–5 min | 8 | 21 | 13 | 13 |
| TTA–time 5.01–10 min | 48 | 49 | 48 | 51 |
| TTA–time 10.01–15 min | 42 | 32 | 41 | 38 |
| TTA–time 15.01–20 min | 21 | 6 | 18 | 14 |
| TTA–time 20 min | 5 | 6 | 9 | 3 |
| Pearson’s Chi-squared | 0.003 | 0.649 | ||
| 2 cells (16.7%) have expected count less than 5. The minimum expected count is 4.41 | 0 cells (0%) have expected count less than 5. The minimum expected count is 5.27 | |||
Abbreviations: CXR, chest X-ray; LOS, length of stay; ED, emergency department; TTA, trauma team activation.
Figure 2.
Box plots of CXR-times (minutes) for groups of differently timed TTA (minutes).
Notes: *More than three box lengths from the box; °between 1.5–3 box lengths from the box.
Abbreviations: CXR, chest X-ray; TTA, trauma team activation.
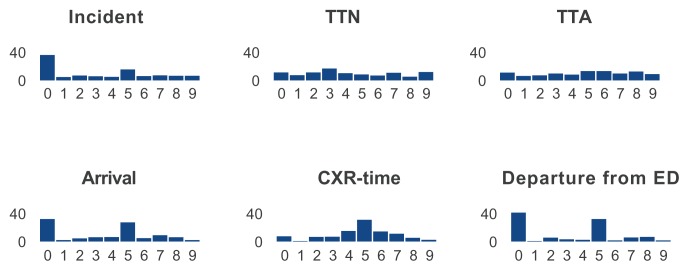
Data quality
Analysis of data quality showed that amongst the manually recorded time data (incident, arrival, chest X-ray, and departure from ED) there were considerably more 5-minute interval recordings compared with the automatically registered time data (TTN and TTA). That is, for manually recorded data, the last digit was more often 0 or 5, while for automatically recorded data the last digit was evenly distributed between all numbers from 0 to 9 (Figure 3).
Figure 3.
Distribution (%) of last digits in recorded time data.
Notes: Incident, arrival, CXR-time, and departure from ED were recorded manually. TTN and TTA were recorded automatically.
Abbreviations: ED, emergency department; TTN, trauma team notification; TTA, trauma team activation; CXR, chest X-ray.
Discussion
Summary of main findings
The results from this study demonstrate that proactive TTA improved the initial management of trauma patients as measured by a reduction in CXR-time. We are not aware of any other study that describes the association between timing of trauma team activation and trauma team performance.
A preactivation TTN did not have any effect on team performance as measured by CXR-time. ED LOS was not associated with TTN or the timing of TTA, indicating that other factors are more important for determining the ED LOS. Visual inspection of the data indicates that trauma teams at our hospital should be notified at least 10 minutes before the patient arrives at the resuscitation room, perhaps even as much as 20 minutes prearrival. This finding is probably not directly transferable to other hospitals as composition, coordination, and experience of trauma team members may vary both between and within hospitals.12–14 It is reasonable to assume that the ideal time between TTA and patient arrival, at least depends on hospital architecture and organization. To identify the ideal time between TTA and patient arrival for a particular hospital, one can plot local CXR-times against TTA time. Trauma care quality registries should include these variables.
Other studies
There are few other studies to compare and contrast our results with. Driscoll and Vincent found through both observational and interventional studies, that proactive measures such as preallocation of tasks and the establishment of horizontal organization improved trauma patient resuscitation times compared to ad hoc allocation and the sequential execution of tasks.15 Although different from our study, their results point in the same direction, namely that proactive measures improve team performance.
Several efforts must be undertaken to achieve adequate proactivity in trauma management. To ensure that necessary knowledge and skills are present on patient arrival, trauma teams should be multidisciplinary. Written procedures and simulation training support shared understanding of what should be done, when and by whom, instead of coming to an ad hoc understanding of how to cooperate.16,17 Finally, appropriate communication between prehospital and in-hospital teams is vital in mounting an adequate clinical response to the arrival of the trauma patient. Interestingly we found no association between TTN and CXR-time or ED LOS, thus questioning the need for prearrival communication for preparation of trauma teamwork. Even though the TTN had no effect on our measures, it does not mean that the TTN did not have any effect at all. A TTN may have enhanced trauma team members’ situational awareness and enabled them to better sequence their nontrauma clinical activities, so as to minimize adverse ripple effects through the hospital when the TTA required their presence in the resuscitation room (or it might have stressed them and maximized ripple effects!). The TTN may also have been more important when several trauma patients arrived simultaneously, requiring more resources and preparations than usual. Furthermore, the TTN might have improved the quality of work and potentially improved patient outcomes in other measures not reflected through CXR-times or ED LOS. An alternative to sending a TTN to all team members could be to notify only the team leader who subsequently could choose who else should be notified before the TTA.
Strengths and limitations
We used a single hospital trauma care quality registry as our main source for data, supplied by an automatically generated trauma paging alert log. The data in the quality registry was documented on paper by an emergency ward nurse during the initial management of trauma patients, and later entered into an electronic database by a secretary. In terms of data quality, the manually recorded data clearly illustrated the human propensity to smoothen data. We have only succeeded in finding one scientific article mentioning this particular phenomenon pertaining to registration of time data,18 but many studies have demonstrated smoothing and inaccuracies in manually recorded medical data.19 Although this phenomenon impedes data quality, we are of the opinion that it is more likely that this reduction in data granularity would mask any differences rather than produce artificial ones between groups of differently timed TTAs. Regardless of this particular study, we think trauma care quality registries should endeavor towards automatic sampling of time data.
Our outcome measures were not directly related to patient outcomes, but were measures on how fast the trauma team managed the patient within the resuscitation room. There is poor scientific support for the validity of trauma care time measurements as indicators of patient outcomes, as for other proposed quality indicators for evaluating trauma care.20,21 However, time or time savings from patient arrival to radiological investigations have been reported in previous studies of trauma team quality.15,22,23
Conclusion
Proactive activation of the trauma team improved trauma team performance. For this particular hospital trauma team activation 10–20 minutes before arrival of the patient was associated with a statistically significant reduction in CXR-time. More research on the effects of notification and proactive activation of trauma teams is needed. Such research has the potential to improve the quality of trauma management, reducing the adverse ripple effects of trauma care on other hospital activities.
Acknowledgment
The authors acknowledge the contribution of Prof Grethe Albrektsen, Unit of Applied Clinical Research, Faculty of Medicine, Norwegian University of Science and Technology, for valuable advice on statistical methods.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Uleberg O, Vinjevoll OP, Eriksson U, Aadahl P, Skogvoll E. Overtriage in trauma – what are the causes? Acta Anaesthesiol Scand. 2007;51(9):1178–1183. doi: 10.1111/j.1399-6576.2007.01414.x. [DOI] [PubMed] [Google Scholar]
- 2.Larsen KT, Uleberg O, Skogvoll E. Differences in trauma team activation criteria among Norwegian hospitals. Scand J Trauma Resusc Emerg Med. 2010;18:21. doi: 10.1186/1757-7241-18-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cohen MM, Fath JA, Chung RS, Ammon AA, Matthews J. Impact of a dedicated trauma service on the quality and cost of care provided to injured patients at an urban teaching hospital. J Trauma. 1999;46(6):1114–1119. doi: 10.1097/00005373-199906000-00028. [DOI] [PubMed] [Google Scholar]
- 4.American College of Surgeons, Committee on Trauma. Resources for Optimal Care of the Injured Patient: 1999. Chicago, IL: American College of Surgeons; 1999. [Google Scholar]
- 5.American College of Surgeons, Committee on Trauma. Resources for Optimal Care of the Injured Patient: 2006. Chicago, IL: American College of Surgeons; 2006. [Google Scholar]
- 6.Henry MC, Alicandro JM, Hollander JE, Moldashel JG, Cassara G, Thode HC., Jr Evaluation of American College of Surgeons trauma triage criteria in a suburban and rural setting. Am J Emerg Med. 1996;14(2):124–129. doi: 10.1016/S0735-6757(96)90117-5. [DOI] [PubMed] [Google Scholar]
- 7.Sasser SM, Hunt RC, Faul M, et al. Guidelines for field triage of injured patients: recommendations of the National Expert Panel on Field Triage, 2011. MMWR Recomm Rep. 2009;61(RR-1):1–20. [PubMed] [Google Scholar]
- 8.Lerner EB. Studies evaluating current field triage:1966–2005. Prehosp Emerg Care. 2006;10(3):303–306. doi: 10.1080/10903120600723921. [DOI] [PubMed] [Google Scholar]
- 9.Liberman M, Mulder DS, Jurkovich GJ, Sampalis JS. The association between trauma system and trauma center components and outcome in a mature regionalized trauma system. Surgery. 2005;137(6):647–658. doi: 10.1016/j.surg.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 10.Kortbeek JB, Al Turki SA, Ali J, et al. Advanced trauma life support, 8th edition, the evidence for change. J Trauma. 2008;64(6):1638–1650. doi: 10.1097/TA.0b013e3181744b03. [DOI] [PubMed] [Google Scholar]
- 11.Wisborg T, Brattebø G, Brattebø J, Brinchmann-Hansen A. Training multiprofessional trauma teams in Norwegian hospitals using simple and low cost local simulations. Educ Health (Abingdon) 2006;19(1):85–95. doi: 10.1080/13576280500534768. [DOI] [PubMed] [Google Scholar]
- 12.Ahmed JM, Tallon JM, Petrie DA. Trauma management outcomes associated with nonsurgeon versus surgeon trauma team leaders. Ann Emerg Med. 2007;50(1):7–12. doi: 10.1016/j.annemergmed.2006.09.017. [DOI] [PubMed] [Google Scholar]
- 13.Driscoll PA. Trauma: today’s problems, tomorrow’s answers. Injury. 1992;23(3):151–158. doi: 10.1016/s0020-1383(05)80033-6. [DOI] [PubMed] [Google Scholar]
- 14.Ringen AH, Hjortdahl M, Wisborg T. Norwegian trauma team leaders – training and experience: a national point prevalence study. Scand J Trauma Resusc Emerg Med. 2011;19:54. doi: 10.1186/1757-7241-19-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Driscoll PA, Vincent CA. Organizing an efficient trauma team. Injury. 1992;23(2):107–110. doi: 10.1016/0020-1383(92)90043-r. [DOI] [PubMed] [Google Scholar]
- 16.Brattebo G, Wisborg T, Høylo T. Organization of trauma admissions at Norwegian hospitals. [Article in Norwegian] Tidsskr Nor Laegeforen. 2001;121(20):2364–2367. [PubMed] [Google Scholar]
- 17.Wisborg T, Brattebo G, Brinchmann-Hansen A, Uggen PE, Hansen KS. Norwegian BEST FoundationBEST: Better and Systematic Trauma Care. Effects of nationwide training of multiprofessional trauma teams in norwegian hospitals. J Trauma. 2008;64(6):1613–1618. doi: 10.1097/TA.0b013e31812eed68. [DOI] [PubMed] [Google Scholar]
- 18.Loach D, Carter M. Scheduling According to Physician Average Procedure Times in Endoscopy Suites. 21th Annual Conference of the Production and Operations Management Society; May 7–10, 2010; Vancouver, Canada. [Google Scholar]
- 19.van Schalkwyk JM, Lowes D, Frampton C, Merry AF. Does manual anaesthetic record capture remove clinically important data? Br J Anaesth. 2011;107(4):546–552. doi: 10.1093/bja/aer163. [DOI] [PubMed] [Google Scholar]
- 20.Stelfox HT, Bobranska-Artiuch B, Nathens A, Straus SE. Quality indicators for evaluating trauma care: a scoping review. Arch Surg. 2010;145(3):286–295. doi: 10.1001/archsurg.2009.289. [DOI] [PubMed] [Google Scholar]
- 21.Lerner EB, Billittier AJ, Dorn JM, Wu YW. Is total out-of-hospital time a significant predictor of trauma patient mortality? Acad Emerg Med. 2003;10(9):949–954. doi: 10.1111/j.1553-2712.2003.tb00650.x. [DOI] [PubMed] [Google Scholar]
- 22.Lu WH, Kolkman K, Seger M, Sugrue M. An evaluation of trauma team response in a major trauma hospital in 100 patients with predominantly minor injuries. Aust N Z J Surg. 2000;70(5):329–332. doi: 10.1046/j.1440-1622.2000.01820.x. [DOI] [PubMed] [Google Scholar]
- 23.Ruchholtz S, Waydhas C, Lewan U, et al. A multidisciplinary quality management system for the early treatment of severely injured patients: implementation and results in two trauma centers. Intensive Care Med. 2002;28(10):1395–1404. doi: 10.1007/s00134-002-1446-8. [DOI] [PubMed] [Google Scholar]