Abstract
Pakistan is a struggling economy with poor maternal and child health indicators that have affected attainment of the United Nations Millennium Development Goals 4 and 5 (under-five child and maternal mortality). Recent health reforms have abolished the federal Ministry of Health and devolved administrative and financial powers to the provinces. Ideally, devolution tends to simplify a healthcare system's management structure and ensure more efficient delivery of health services to underserved populations, in this case women and children. In this time of transition, it is appropriate to outline prerequisites for the efficient management of maternal and child health (MCH) services.
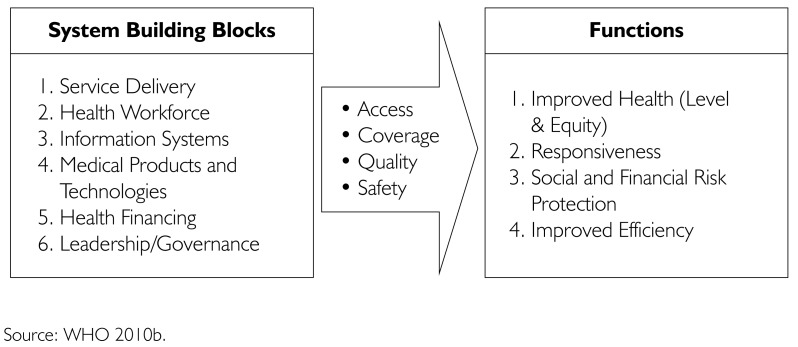
This paper examines the six building blocks of health systems in order to improve the utilization of MCH services in rural Pakistan. The targeted outcomes of recent reforms are devolved participatory decision-making regarding distribution of MCH-related services, improved deployment of the healthcare workforce, prioritization of pro-poor strategies for health financing and integration of various health information systems. Given this window of opportunity, the provinces need to guarantee fairness and equity through their stewardship of the healthcare system so as to protect vulnerable mothers and their children, especially in rural, remote and disadvantaged areas of Pakistan.
Abstract
Le Pakistan est une économie précaire où le peu d'indicateurs de santé pour les mères et les enfants a fait obstacle à l'atteinte des cibles 4 et 5 des Objectifs du millénaire pour le développement des Nations Unies (mortalité maternelle et des enfants de moins de cinq ans). Les récentes réformes de la santé ont donné lieu à l'abolition du ministère fédéral de la Santé et à la passation des pouvoirs administratifs et financiers aux provinces. En principe, ce type de passation a tendance à simplifier la structure de gestion du système de santé et à assurer une prestation plus efficace des services de santé aux populations mal desservies, dans le cas présent, les femmes et les enfants. En cette période de transition, il convient de souligner les conditions préalables à une gestion efficace des services de santé maternelle et infantile (SSMI).
Cet article examine les six éléments constitutifs d'un système de santé afin d'améliorer l'utilisation des SSMI dans le Pakistan rural. Les résultats visés par les récentes réformes sont: la passation de la prise de décision participative quant à la prestation des services liés au SSMI, l'amélioration du déploiement de la main-d'œuvre de la santé, la priorisation des stratégies de financement en faveur des plus pauvres et l'intégration de divers systèmes d'information sur la santé. Dans cette conjoncture favorable, les provinces doivent garantir l'équité au moyen d'une administration adéquate du système de santé, de sorte à protéger les mères vulnérables et leurs enfants, particulièrement dans les régions pakistanaises rurales, éloignées et défavorisées.
Decentralization of government services may take various forms: (a) de-concentration, (b) delegation, (c) devolution and (d) privatization (Rondinelli et al. 1983). Any form of decentralization ought to improve the responsiveness and quality of health services delivery by better informing decision-makers and service providers, bringing them closer to the populations they serve and making them more accountable. Decentralization tends to simplify management structures and enhance the efficient use of resources, ensuring equity in terms of improved access to health services and delivery for underserved, marginalized, vulnerable and remotely located population groups (Frenk 1994). However, in the absence of a national health services policy, current inequities in the distribution of finances, it is possible that human resources and structures could deteriorate. There is a likelihood of increased inefficiency owing to gaps in the managerial capacity of subnational tiers of government, especially when subnational capacity and overall infrastructure are weak (Roy 1994). Thus, decentralization and devolution of powers in the healthcare and social sectors have yielded mixed results in various countries around the world.
Efforts towards decentralization typically result from political decisions over which health functionaries have little control, and this is the case with Pakistan. The sixth most populous country in the world, located in southern Asia, Pakistan has recently enacted constitutional reforms that shift financial and administrative powers to the four subnational/provincial governments (Government of Pakistan 2010). The federal health ministry and many other social-sector portfolios have been transferred to the four provinces with the mandate of policy making, financing, regulation, service provision, administration and governance. This political transition has many implications for healthcare provision (Nishtar and Mehboob 2011). As a result of reforms initiated in 2011, high-priority preventive programs formerly managed by the federal government – such as family planning, primary healthcare (PHC), immunization, maternal/neonatal and child health, nutrition and programs targeting specific diseases – are now managed at the provincial level (Nishtar 2011).
Pakistan has long had a mixed public–private healthcare delivery system with the conventional three tiers of primary, secondary and tertiary healthcare facilities (Shaikh 2011). Like many low-income countries, it relies on community health workers, who are a valuable resource in providing basic healthcare and MCH-related services at the community level (Kruk et al. 2009). Yet despite Pakistan's conventional healthcare system with vertically organized programs to deliver the first tier of care, 80% of the population uses the private-sector, fee-for-service system (Shaikh 2011; WHO 2007b).
Pakistan has a high fertility rate, high maternal and under-five mortality rates and a low rate of contraceptive use (National Institute of Population Studies and Macro International 2008). As a signatory to the United Nations Millennium Development Goals (MDGs), the country is lagging in terms of reducing under-five mortality by two-thirds (MDG 4) and maternal mortality by three-quarters (MGD 5) by 2015 (Lawn et al. 2011). The attainment of MDGs could become an even bigger challenge given the present political transition.
Decentralization in Pakistan is a consequence of domestic political decisions taken by the ruling party, which claims to have restored the constitution of 1973 in its original state. There are also economic, organizational and legal reasons behind the reforms, yet these have been subsumed by the overarching political environment, as have decentralization efforts in many parts of the world (Saltman et al. 2007). The variations evident within the four Pakistani provinces – in terms of population size, political and social set-up, and the structure and quality of healthcare delivery systems – have serious implications, particularly on MCH indicators.
The process of reform offers an opportunity to confront long-standing challenges, constraints and inadequacies within Pakistan's health systems. Health planning at the provincial and district levels may be more effective at problem identification, prioritization and setting clear objectives within local budgets. Moreover, decentralization should ideally result in better governance, more effective service delivery and decision-making at the grassroots level, thus providing a platform for empowering citizens (Shaikh and Rabbani 2004). With the provinces having greater autonomy, primary healthcare, which is the core approach for expanding and strengthening the essential programs for MCH in any developing country, could be incidentally revitalized (Shaikh et al. 2007). This transitional phase is also an opportune time to foster intersectoral cooperation to address social determinants of health (WHO 2010a). However, success will depend upon strengthening the basic building blocks of the health system.
Implications of Reforms and WHO Building Blocks for Health Systems
For our analysis, we used the World Health Organization's framework for strengthening the building blocks of health systems (WHO 2007a, 2010b).
FIGURE 1.
The building blocks of health systems: aims and attributes. Source: WHO 2010b.
Leadership/governance
In 2001, Pakistan's legislature introduced a local-government act to establish good governance with transparency, accountability and community participation in the health sector. This initiative failed owing to lack of political support and weak capacity of the local governing bodies (Israr and Islam 2006).
Until recently, the federal Ministry of Health was responsible for the vision, leadership and governance in the health sector. Although the reforms of 2011 may well challenge the provincial governments in creating good administrative and functional governance in their health systems (Frenk 1994), the participatory approach can nevertheless improve maternal and child health indicators through prioritizing and planning maternal and child health programs at the PHC level. Devolved decision-making with regard to the deployment and distribution of community health workers, prompt availability of logistics for MCH and equitable, high-quality MCH services can accelerate progress towards attaining MDGs 4 and 5.
Information systems
The national Health Management Information System (HMIS) and other parallel information systems – for family planning, PHC, maternal/neonatal and child health, the Expanded Program on Immunization (EPI), and data on tuberculosis, HIV/AIDS, malaria and other diseases – are operational but only minimally integrated. HMIS provides information on 18 high-priority diseases, availability of drugs, service utilization, status of medical equipment and infrastructure of health facilities (Sabih et al. 2010; Shaikh 2011).
Following the 2011 reforms, HMIS data now flow from peripheral health facilities to district centres and then to the provincial HMIS cell. Lack of integration of health information and irregular reporting practices are key impediments to informed decision-making by district and provincial health managers. Yet, this transitional period offers opportunities for the provinces to reorganize and integrate the district HMIS and program-specific information systems to create efficient and timely reporting mechanisms. Such reorganization would support evidence-based decision-making and a rational allocation of resources for the high-priority MCH interventions. Another missing link in the information chain is data from the private health sector, which serves 80% of the population. Integrating private-sector data with the HMIS is crucial for creating relevant policy and planning processes (Nishtar 2007).
Service delivery
Programs for family planning, PHC, EPI, nutrition, and maternal/neonatal and child health (MNCH) focus on vulnerable segments of the Pakistani population, i.e., women and children, especially in rural and remote areas of the country. These programs are now the responsibility of the provincial governments.
A recent demographic survey on health status shows improvements in maternal and child health indicators in those regions covered by community health workers deployed under these programs (Hafeez et al. 2011). MNCH initiatives have the potential to prevent about 25% of maternal deaths, 20% of neonatal deaths and 29%–40% of under-five child mortality (Bhutta et al. 2008). The devolution of administrative and financial powers in these programs can actually help community-based health workers meet the needs of these vulnerable groups across the provinces (Solberg 2010). Devolved decision-making can simplify the management of, and augment access to, essential MCH services such as antenatal and postnatal care, delivery by skilled birth attendants and family planning. Better-informed and more timely decisions will improve the responsiveness and quality of services.
The federal government needs to ensure a swift transfer of financial resources, as well as interim technical assistance, for effective implementation of MCH programs in the provinces (Nishtar 2011). It should further consider coordinating its efforts with NGOs with respect to resource mobilization because the NGOs have relatively flexible planning and the ability to design population-based projects for health education, health promotion, social marketing, community development and advocacy (Ejaz et al. 2011). Such modalities could go a long way towards dealing with the weighty burden of disease in the country.
Medical products and technologies
Overpayment for medicines and medical technologies is commonly observed in the public sector of developing countries (Transparency International 2006). Evidence suggests that many countries have centralized authorities for controlling the quality, price and intellectual property rights of drugs and medical devices (Nishtar 2011). The stewardship role of the federal drug regulatory authority can ensure all these aspects.
Unavailability of essential medicines at PHC facilities is a key contributor to citizens' underutilization of the public healthcare system (Shafiq and Shaikh 2012). Inappropriate inventory management, lack of storage capacity and weak distribution mechanisms are considered major barriers to availability of essential medicines in Pakistan's health facilities (Abbasi et al. 2012). Unavailability leads to high out-of-pocket payments by clients who purchase essential drugs from private retail pharmacies.
The 2011 reforms offer an opportunity for local authorities to improve supply and distribution mechanisms for essential MCH drugs. Improved coordination, and the introduction of a logistic management information system for regulating MCH-related drugs specifically, would protect this segment of the population from incurring catastrophic expenses.
Besides addressing the lack of supplies, there is also a dire need to strengthen emergency obstetric care services at the district level in order to ensure that deliveries occur at healthcare facilities and not in the hands of traditional birth attendants.
Health financing
Consistently low allocations to public health services by the federal government have resulted in poor-quality care and, consequently, underutilization of public facilities compared to private-sector providers, which offer excellent care but at much higher cost. Out-of-pocket payments place a considerable burden on citizens, the majority of whom live below the poverty line. The social security and private health insurance systems, along with the Zakat fund and Bait-ul-Maal1 for marginalized people, cannot practically serve large segments of the poor population (Ahmed and Shaikh 2008; WHO 2007b).
What is needed now is an exploration of innovative healthcare financing models. A prerequisite, however, would be that the provinces review their budgets and consider allocating more funds towards high-priority MCH issues. Pakistan spends the major portion of its health budget on secondary and tertiary care compared to primary care. Experience in other developing countries suggests that greater investment to revamp PHC facilities and amplify community outreach services improves MNCH status (WHO 2008). Many governments have succeeded in sustaining health reforms that improve maternal and child health, even in times of financial austerity (Shaikh and Rabbani 2004; WHO 2010c). Social protection schemes, such as vouchers with pre-payment mechanisms, cash transfers and micro-financing strategies, have been used to improve regional health services utilization and to address issues of equity (Agha 2011). To prevent those in lower economic quintiles from incurring catastrophic out-of-pocket expense while seeking MCH care in Pakistan, the provincial governments must envision and implement pro-poor strategies, given the increase in poverty in the country in recent years.
Health workforce
Trained and skilled human resources are essential to fortify the administrative and technological capacity of robust health systems. The role of health workers in PHC becomes even more critical because they interact with people who have low literacy levels, compromised living conditions and least exposure to health information (WHO 2008).
Deployed all across Pakistan, local health workers are an effective conduit between communities and the district health system. Only 25% of PHC facilities are served by duly qualified, female community health providers; a catchment area of 20,000 people is typically served by only 50 public-sector health workers (Sabih et al. 2010; Shaikh 2011). Because community health workers are the principal caregivers for MCH in the rural sector, issues of critical shortage and service protection need serious attention (Hafeez et al. 2011).
Provincial and district health management authorities must strategize towards motivating, recruiting and retaining this essential human resource, as well as these workers' equitable geographic distribution according to community needs. Likewise, governments must not overlook capacity development and career advancement of community health workers who provide MCH services.
Conclusion
The devolution of decision-making from the federal government to Pakistan's provinces gives the latter increased control over health governance and enhanced administrative and financial powers. This process of reform must confront the long-standing challenges, constraints and inadequacies of the country's health systems. Although health planning at the provincial and district levels offers potential gains in identifying problems and prioritizing and implementing objectives, success will depend on the adoption of evidence-based strategies and interventions.
Pakistan's provincial health systems must ensure fairness in financing to spare the poor from incurring catastrophic expenses, particularly while seeking MCH care. Better integration of HMIS and program-specific information systems must be achieved to ensure equitable distribution of human and material resources in MCH care. Further, the provinces must develop and implement effective policies and other concerned stakeholders should advocate for evidence-based interventions for maternal, newborn and child health in Pakistan.
Two different charity systems among Muslims, managed by the state.
Contributor Information
Arslan Mazhar, Research Associate, Department of Health Systems & Policy, Health Services Academy, Islamabad, Pakistan.
Babar Tasneem Shaikh, Associate Professor, Department of Health Systems & Policy, Health Services Academy, Islamabad, Pakistan.
References
- Abbasi A.S.K., Mazhar A., Khan S.A., Rehman R. 2012. “Assessment of Logistic Mechanism of Anti-Tuberculosis Drugs in District Bagh, Azad Jammu and Kashmir.” Pakistan Journal of Public Health 2(1): 30–35 [Google Scholar]
- Agha S. 2011. “Changes in the Proportion of Facility-Based Deliveries and Related Maternal Health Services among the Poor in Rural Jhang, Pakistan: Results from a Demand-Side Financing Intervention.” International Journal for Equity in Health 10: 57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmed J., Shaikh B.T. 2008. “An All-Time Low Budget for Health Care in Pakistan.” Journal of College of Physicians and Surgeons Pakistan 18(6): 388–91 [PubMed] [Google Scholar]
- Bhutta Z.A., Ali S., Cousens S., Ali T.M., Haider B.A., Rizvi A. 2008. “Alma-Ata: Rebirth and Revision – 6 Interventions to Address Maternal, Newborn and Child Survival: What Difference Can Integrated Primary Health Care Strategies Make?” Lancet 372(9642): 972–89 [DOI] [PubMed] [Google Scholar]
- Ejaz I., Shaikh B.T., Rizvi N. 2011. “NGOs and Government Partnership for Health Systems Strengthening: A Qualitative Study Presenting Viewpoints of Government, NGOs and Donors in Pakistan.” BMC Health Services Research 11: 122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frenk J. 1994. “Dimensions of Health System Reform.” Health Policy and Planning 27: 19–34 [DOI] [PubMed] [Google Scholar]
- Government of Pakistan. The 18th Amendment to the Constitution of the Islamic Republic of Pakistan. 2010. Retrieved June 9, 2012. < http://www.pakistani.org/pakistan/constitution/amendments/18amendment.html>.
- Hafeez A., Mohamud B.K., Shiekh M.R., Shah S.A., Jooma R. 2011. “Lady Health Workers Programme in Pakistan: Challenges, Achievements and the Way Forward.” Journal of Pakistan Medical Association 61(3): 210–15 [PubMed] [Google Scholar]
- Israr S.M., Islam A. 2006. “Good Governance and Sustainability: A Case Study from Pakistan.” International Journal of Health Planning and Management 21(4): 313–25 [DOI] [PubMed] [Google Scholar]
- Kruk M.E., Prescott M.R., de Pinho H., Galea S. 2009. “Are Doctors and Nurses Associated with Coverage of Essential Health Services in Developing Countries? A Cross-Sectional Study.” Human Resources for Health 7: 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lawn J.E., Blencowe H., Pattinson R., Cousens S., Kumar R., Ibiebele I. 2011. “Stillbirths: Where? When? Why? How to Make the Data Count.” Lancet 377: 1448–63 [DOI] [PubMed] [Google Scholar]
- National Institute of Population Studies Macro International. 2008. Pakistan Demographic and Health Survey 2006–07. Islamabad: Government of Pakistan. [Google Scholar]
- Nishtar S.“Health Indicators of Pakistan – Gateway Paper II.”. 2007. Retrieved June 9, 2012. < http://www.heartfile.org/pdf/GWP-II.pdf>.
- Nishtar S.“Health and the 18th Amendment – Need for a National Structure.”. 2011. Retrieved June 9, 2012. < http://www.heartfile.org/pdf/HEALTH_18AM_FINAL.pdf>.
- Nishtar S., Mehboob A.B. 2011. (August 20). “Pakistan Prepares to Abolish Ministry of Health.” Lancet 378(9792): 648–49 doi: 10.1016/S0140-6736(11)60606-5. [DOI] [PubMed] [Google Scholar]
- Rondinelli D., Cheema G.S., Nellis J. 1983. Decentralization in Developing Countries: A Review of Recent Experience. World Bank Staff Working Paper No. 581. Washington, DC: World Bank. [Google Scholar]
- Roy A. 1994. “Efficiency and Equity Implications of the Health Care Reforms.” Social Science and Medicine 39(9): 189–201 [DOI] [PubMed] [Google Scholar]
- Sabih F., Bile K.M., Buehler W., Hafeez A., Nishtar S., Siddiqi S. 2010. “Implementing the District Health System in the Framework of Primary Health Care in Pakistan: Can the Evolving Reforms Enhance the Pace towards the Millennium Development Goals?” Eastern Mediterranean Health Journal 16: s132–s144. [PubMed] [Google Scholar]
- Saltman R.B., Bankauskaite V., Vrangbaek K. 2007. “Introduction: The Question of Decentralization.” In Saltman R.B., Bankauskaite V., Vrangbaek K., eds., Decentralization in Health Care: Strategies and Policies. European Observatory on Health Systems and Policies Series (pp. 1–6). Maidenhead, England: Open University Press. [Google Scholar]
- Shafiq Y., Shaikh B.T. “Availability and Affordability of Essential Medicines: Exploring the Health-Seeking Behaviours and Health Service Utilization for Children Under 5 Years, Living in Squatter Settlement of Karachi, Pakistan.”. Journal of Ayub Medical College. 2012 (in press). [PubMed] [Google Scholar]
- Shaikh B.T. 2011. “Health Care System in Pakistan.” In Rout H.S., ed., Health Care Systems: A Global Survey (pp. 434–54). New Delhi: New Century Publications. [Google Scholar]
- Shaikh B.T., Kadir M.M., Pappas G. 2007. “Thirty Years of Alma-Ata Pledges: Is Devolution in Pakistan an Opportunity for Rekindling Primary Health Care?” Journal of Pakistan Medical Association 57(5): 259–61 [PubMed] [Google Scholar]
- Shaikh B.T., Rabbani F. 2004. “The District Health System: A Challenge that Remains.” Eastern Mediterranean Health Journal 10(1/2): 208–14 [PubMed] [Google Scholar]
- Solberg K.E. 2010. “New Laws Could Improve Women's Health in Pakistan.” Lancet 375(9730): 1956. [DOI] [PubMed] [Google Scholar]
- Transparency International. 2006. Global Corruption Report 2006. Berlin: Author. [Google Scholar]
- World Health Organization (WHO). 2007a. Everybody's Business: Strengthening Health Systems to Improve Health Outcomes: WHO's Framework for Action. Geneva: Author. [Google Scholar]
- World Health Organization (WHO). 2007b. Health Systems Profile – Pakistan. Regional Health Systems Observatory. Cairo: WHO–EMRO. [Google Scholar]
- World Health Organization (WHO). 2008. The World Health Report 2008: Primary Health Care – Now More Than Ever. Geneva: Author. [Google Scholar]
- World Health Organization (WHO). Workshop on Decentralization of Health Services in the Eastern Mediterranean Region. 2010a;8–11 November, Amman. [Google Scholar]
- World Health Organization (WHO). 2010b. Monitoring the Building Blocks of Health Systems: A Handbook of Indicators and Their Measurement Strategies. Geneva: Author. [Google Scholar]
- World Health Organization (WHO). 2010c. The World Health Report 2010: Health Systems Financing – The Path to Universal Coverage. Geneva: Author. [DOI] [PMC free article] [PubMed] [Google Scholar]