Abstract
Background:
Reducing wait times is a key goal of Canadian health planners and policy makers. Using data from the EMRs of 23 family physicians across southwestern Ontario, we present data on wait times to see a specialist, and evaluate these data for equity.
Methods:
Cross-sectional analysis of EMR database of 29,303 patients and 544,398 encounters from October 2005 to July 2010. Wait time was calculated as the difference between the specialist appointment date and the family physician's referral date. Multilevel regression analysis was used to assess equity in waiting times.
Results:
The median wait was 53 days, with female patients having a slightly longer wait than males (55 vs. 51 days), and younger patients (median = 45 days) having the shortest wait. Differences were noted among practices, with a range of 42–63 days. The longest waits were for neurosurgery (median = 103 days) and the shortest for paediatricians (median = 28 days). There was no correlation between wait times and income, but significant associations were noted for patient age, sex and referral urgency.
Interpretation:
This is the first study to present data on actual wait times for a broad array of specialists over a five-year period. There is variation among specialties and by practice, and further research is needed to understand reasons for these. From a policy perspective, there is equity in wait times in southwestern Ontario, as waits are not correlated with SES. Future work should model the patient-, physician- and contextual-level factors that determine specialist wait times.
Abstract
Contexte:
La réduction des temps d'attente est un objectif clé des planificateurs de la santé et des responsables de politiques au Canada. À l'aide de données provenant des dossiers médicaux électroniques (DME) de 23 médecins de famille du sud-ouest ontarien, nous présentons des données sur les temps d'attente pour consulter un spécialiste, et nous évaluons ces données pour ce qui est de l'équité.
Méthodes:
Nous avons effectué l'analyse transversale de la base de données des DME de 29 303 patients et de 544 398 visites, d'octobre 2005 à juillet 2010. Le temps d'attente a été calculé en fonction de la différence entre la date du rendez-vous chez le spécialiste et la date d'aiguillage par le médecin de famille. Pour évaluer l'équité des temps d'attente, nous avons procédé à une analyse de régression multiniveaux.
Résultats:
La médiane de l'attente était de 53 jours, légèrement un peu plus long pour les femmes que pour les hommes (55 contre 51 jours); il y a moins d'attente pour les patients les plus jeunes (médiane = 45 jours). Il y a des différences entre les pratiques, dont l'étendue varie entre 42 et 63 jours. On observe les plus longs temps d'attente en neurochirurgie (médiane = 103 jours) et les plus courts en pédiatrie (médiane = 28 jours). Il n'y a pas de corrélation entre les temps d'attente et le revenu, mais il existe des associations significatives pour ce qui est de l'âge, du sexe et de l'urgence de l'aiguillage.
Interprétation:
Il s'agit de la première étude qui présente des données sur les temps d'attente réels pour une vaste gamme de spécialités sur une période de cinq ans. Il y a des variations selon les spécialités et les pratiques; plus de recherches sont nécessaires pour en comprendre les raisons. Du point de vue politique, il y a équité dans les temps d'attente dans le sud-ouest ontarien, puisqu'il n'y a pas de corrélation avec le statut socioéconomique. Les travaux à venir devraient modéliser les facteurs – liés aux patients, aux médecins et aux contextes – qui déterminent les temps d'attente pour une visite chez le spécialiste.
Reducing wait times for healthcare is a key goal of Canadian health planners and policy makers. Broadly speaking, patients may encounter three types of waits during their interaction with the healthcare system. The first wait is the interval between the time the patient perceives the symptoms and decides to seek care, and the actual visit to the family physician or another provider of primary care. While most healthcare encounters can be satisfactorily resolved by the family physician, sometimes a specialist consultation is sought. The second wait occurs between the time a family physician makes a referral and the actual patient visit to the specialist. The specialist may order further tests (such as an MRI) as a prelude to treatment, and the patient may then encounter a third wait (for the MRI and/or treatment).
It is this third wait that attracts the attention of almost all policy efforts in Canada today (CIHI 2006, 2008; Wait Time Alliance 2011). The 2004 Health Accord allocated $5.5 billion for wait times reduction across Canada, focusing on five priority areas – cancer and cardiac diagnostic imaging, hip and knee replacement and cataract surgery. This was followed by a further $612 million in 2007 to help provinces establish and meet wait times for one provincially selected procedure. Provinces have also developed their own initiatives (e.g., Ontario's Wait Times Strategy) to address wait times within their own jurisdictions (Trypuc et al. 2006).
However, from a patient's perspective, this is only one of the three waits he or she encounters, and the true waiting time for care should (at the very least) also include the second wait – from the family physician's referral to the specialist visit. Data from the 2005 Canadian Community Health Survey (CCHS) reveal that close to 30% of surveyed Canadians said their waits to see a specialist for a new illness or condition were “unacceptable” (Statistics Canada 2006). In the Canadian context, actual data on the extent of this wait is sparse; existing studies focus on a specific condition or procedure (Johnston et al. 2004; Lau et al. 2007; Leung et al. 2007; Simunovic et al. 2001; Singh et al. 2010; Wright and Menaker 2011), have small sample sizes (Leung et al. 2007; Olson and de Gara 2002) or report data from a limited number of facilities (Leung et al. 2007; Massel 1999; Olson and de Gara 2002; Snider et al. 2005).
A bedrock principle of the healthcare system is equity. An equitable health system ensures that utilization is based on need and not on socio-economic factors (e.g., income); thus by extension, waiting times should also be equitable, conditional on need (Aday and Andersen 1981). Literature examining equity in wait times is also scant, and conflicting. While Alter and colleagues (1999) did find waiting times for coronary angiography to be inversely related to neighbourhood income quintiles in Ontario, Shortt and Shaw's (2003) analyses of patients undergoing elective surgery at an academic health centre in Kingston did not find any evidence that residing in a region with low socio-economic status (SES) was associated with longer waiting times for surgery. Similarly, in breast cancer, some studies have found an association of SES with longer waits for radiotherapy in Ontario (Paszat et al. 1998), but others evidenced equity in receipt of surgery and radiotherapy (Gorey et al. 2009).
Using data from an innovative project that has created a researchable database of clinical data abstracted from the electronic medical records (EMRs) of 23 family physicians in southwestern Ontario, we present data on wait times to see a specialist and assess the equity in this wait. To the best of our knowledge, this is the first study in Canada that analyzes data from five years of EMRs from 10 family practices, and analyzes waiting times for 26,942 referrals made during the study period.
Methods
Study design and data source
This was a cross-sectional study using the Deliver Primary Healthcare Information (DELPHI) electronic medical record-derived database. Twenty-three family physicians and allied health professional staff, forming 10 group practices, participated in the DELPHI project. The practices are located in southwestern Ontario, from Windsor in the south to Kincardine in the north and Brantford in the east, including the city of London, with a catchment area of approximately 30,000 square kilometres. The age and sex distribution of the DELPHI family physicians is broadly similar to that of Ontario family physicians, except that the DELPHI sample is less urban (Stewart et al. 2009). With a population of approximately 2.5 million, southwestern Ontario accounts for 20% of Ontario's population. The age and sex distribution of patients in the DELPHI database resembles the Canadian population as a whole.
The DELPHI database contains de-identified data for 29,303 patients and 544,398 encounters from the period October 2005 to July 2010. The project was approved by the University of Western Ontario's Review Board for Health Sciences Research Involving Human Subjects. For reasons of privacy, the DELPHI database does not contain the notes or narrative portion of the patient record. Further details about the DELPHI project and database have been published elsewhere (Stewart et al. 2009).
Variable specification and data analysis
For each referral in the patient chart, we abstracted patient demographics from the EMR: name of referring physician, specialist to whom the patient was referred and his or her specialty, dates of referral and specialist appointment and urgency. Urgency was coded as “priority” if the family physician indicated to the specialist that the patient should be seen quicker; all other referrals were coded as “regular.”
After data cleaning, which consisted of removing (a) duplicates, (b) specialties with <100 referrals in the entire period and (c) referrals with a missing/incorrectly entered specialist appointment date, the sample consisted of 26,942 referrals. For reasons of privacy, we abstracted only the first three digits of the patient's postal code. This code was linked to the Statistics Canada Census file to obtain median family income at the forward sortation area (FSA) level.
The unit of analysis for this paper is an individual referral. Wait time was calculated as the difference between the specialist appointment date and the date of family physician referral. For the descriptive analyses, we report the median wait times by patient sex, patient age, practice, urgency of referral, calendar year, specialty and specialty by practice; non-parametric tests were conducted to test for group differences.
To assess equity in waiting times, we conducted a multilevel regression analysis to examine the impact of neighbourhood median family income on wait times. Because the distribution of wait times was skewed, we log-transformed the dependent variable. Multilevel regression was utilized because the data were clustered at the individual patient and practice level; in addition, we controlled for need by including patient age, sex, specialty referral, referral urgency and calendar year. Stata version 11 was used for the statistical analyses (Statacorp 2010).
Results
There were 13,316 patients in our wait times data set, with a mean age of 50 years. The mean number of referrals per patient was 2 (range, 1–19); females accounted for a majority of the referrals (57.3%). The mean number of referrals per practice was 2,694 (range, 1,143–4,568).
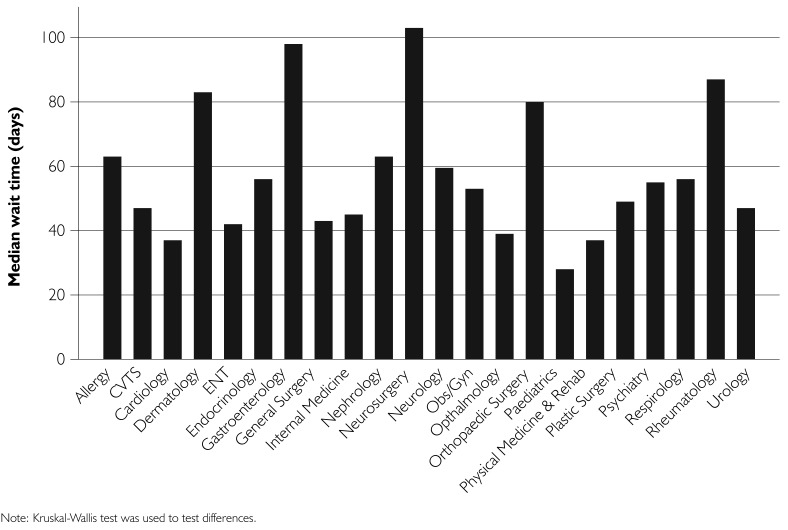
The median wait in our sample was 53 days. In the absence of possible confounders, males had a slightly shorter median wait compared to females (Table 1). Similarly, younger patients had the shortest waits (median wait = 45 days), and the waiting time increased with age, but decreased for the oldest age group of 65+ years (median wait = 50 days). As expected, waiting times varied by practice, and ranged from a low of 42 days to a high of 63 days. Referrals categorized as “priority” had a shorter median wait than regular referrals (28 days vs. 55 days). Median waits declined to a low of 50 days in 2007, but then increased to 56 days in 2010. These differences were statistically significant. Statistically significant variations were also noted by specialty (Figure 1), with the shortest waits being for paediatrics (median wait = 28 days) and the longest being for neurosurgery (median wait = 103 days).
TABLE 1.
Median wait times by patient and practice characteristics
| Median wait time (95% CI) | N | |
|---|---|---|
| Sex: | ||
| Male | 51 (64–56) | 11,490 |
| Female | 55 (50–52) | 15,439 |
| Age: | ||
| 0–19 years | 45 (42–47) | 2,341 |
| 20–44 years | 55 (53–56) | 6,930 |
| 45–64 years | 56 (55–58) | 10,563 |
| 65+ years | 50 (49–52) | 7,107 |
| Practice ID: | ||
| 1 | 57 (52–60) | 1,273 |
| 2 | 45 (44–47) | 4,439 |
| 3 | 42 (40–46) | 1,376 |
| 4 | 58 (56–62) | 3,191 |
| 5 | 62 (56–66) | 1,143 |
| 6 | 54 (44–57) | 1,484 |
| 7 | 63 (59–67) | 2,202 |
| 8 | 61 (59–64) | 4,099 |
| 9 | 49 (47–51) | 4,568 |
| 10 | 52 (54–56) | 3,167 |
| Urgency of referral: | ||
| Regular | 55 (54–56) | 25,698 |
| Urgent | 28 (26–30) | 1,244 |
| Year | ||
| 2005 | 55 (50–60) | 805 |
| 2006 | 51 (49–53) | 4,741 |
| 2007 | 50 (48–52) | 5,583 |
| 2008 | 54 (51–56) | 6,130 |
| 2009 | 56 (54–57) | 6,430 |
| 2010 | 56 (54–59) | |
Note: All comparisons are significant at the .01 level or better, as tested by the Mann-Whitney U-test, or Kruskal-Wallis test, as appropriate.
FIGURE 1.
Wait time by specialty Note: Kruskal-Wallis test was used to test differences.
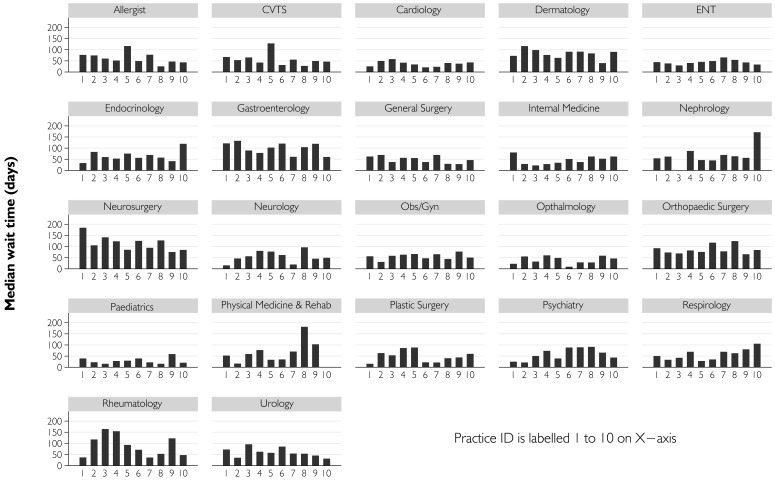
In addition, wide variations were also noted for referrals to each specialty by individual practices (Figure 2). For example, waits for neurosurgery are uniformly high across all practices, but are lower in Practice 9. Whereas cardiology and paediatrics wait times do not seem to vary among practices, variations can be seen among practices in wait times for neurology and rheumatology.
FIGURE 2.
Median wait times for specialty, by practice
The results of the multilevel regression analysis suggest that FSA median household income is not associated with wait time. However, statistically significant associations are noted for patient age, sex and referral urgency; with increasing age, female sex and a priority referral are associated with shorter waits (Table 2). The majority of variation in wait times (85%) is accounted for at the patient level, with the practice level accounting for only 15%.
TABLE 2.
Multilevel regression results of the determinants of wait time
| Coefficient | p-Value | 95% CI | |
|---|---|---|---|
| Fixed effects | |||
| FSA median household income | |||
| Quintile1 | — | — | — |
| Quintile 2 | −0.0193 | .405 | −0.064 to 0.0261 |
| Quintile 3 | 0.0084 | .714 | −0.036 to 0.0539 |
| Quintile 4 | 0.0105 | .730 | −0.049 to 0.070 |
| Quintile 5 | 0.0265 | .319 | −0.025 to 0.788 |
| Patient age | −0.001 | .003 | −0.001 to −0.0003 |
| Patient sex | |||
| Female | — | — | — |
| Male | −0.0298 | .045 | −0.059 to −0.0006 |
| Urgency of referral | |||
| Regular | — | — | — |
| Priority | −0.685 | .001 | −0.748 to −0.621 |
| Random effects | Variance | 95% CI | |
| Level 2: Practice | 0.010 | 0.003–0.027 | |
| Level 1: Patient | 0.058 | 0.045–0.075 | |
Note: Model has been adjusted for specialty and year.
FSA=Forward sortation area
Discussion
Waiting times for specialist care are a concern across the developed world, with countries such as the United Kingdom taking the lead in setting explicit wait time targets (Appleby 2011; Pletcher et al. 2010; Stanway et al. 2004). In the Canadian context, the two sources of specialist wait times most often cited in the literature are the CCHS and the Fraser Institute's annual report (Waiting Your Turn) (Barua et al. 2010; Carriere and Sanmartin 2010). While the 2007 CCHS found that the median wait time for a specialist visit for a new illness or condition was 4.3 weeks, the Fraser Institute reported that the median waiting time between referral by a general practitioner and consultation with a specialist averaged 8.9 weeks across Canada in 2010 (Barua et al. 2010; Carriere and Sanmartin 2010). It is important to note that these surveys do not report the actual wait time, but reflect estimates by patients (CCHS) or specialist physicians (Fraser Institute). Both are subject to recall bias, and the Fraser Institute's survey has a response rate of only 16%, raising questions about its bias. To the best of our knowledge, ours is the first study to present data on actual wait times for a broad array of specialists over a five-year period. Encompassing practices from across southwestern Ontario, our data give an estimate of the waiting times to see a specialist in this geographic region.
The median wait time across all specialties and practices in our study was 53 days. Among the age categories, the shortest wait was for the 0- to 19-year age group; this finding was driven by the waiting time for paediatrics referrals, which was the shortest among all specialties (at 28 days). Thus, while a 53-day (or nearly 2-month) median wait may seem inordinately long, a vulnerable population (i.e., children) faced much shorter waits in the region.
How do our wait times compare to those reported in the literature? For gastroenterology, our median wait times (98 days) are comparable to those of the Practice Audit in Gastroenterology (PAGE) program. This program collected data from 199 gastroenterologists and 5,559 referrals across Canada for 10 months; it found the median wait in Ontario to be 110 days (Armstrong et al. 2008). Although not directly comparable, our median waiting time across all orthopaedic surgery consultations (80 days) is in line with Ontario studies, which report that mean wait times for initial orthopaedic consultation for patients undergoing total hip arthroplasty (THA) was 5.4 weeks (∼38 days) and 8.5 weeks (∼60 days), and 13.5 weeks (∼95 days) and 15.6 weeks (∼109 days) for patients undergoing total knee arthroplasty (TKA) (Coyte et al. 1994; Ho et al. 1994). A smaller study (with data from the Ontario cities of London and Stratford) found a mean wait time of 77 days for patients undergoing THA and TKA at these centres (Snider et al. 2005).
The majority of variation in wait times was attributable to the patient level (85%), with only 15% being accounted for at the practice level. This finding is understandable, as it is the patient's condition that is the genesis of a referral, and practice-level factors can be seen at best as facilitators of this referral. As expected, there were wide variations in wait times among practices, and for each specialty by practice. These variations could reflect differences in local specialist supply and availability, family physician case-mix and referral patterns or patient-level factors (such as type of care needed).
How do these waits compare to the much more publicized wait times for surgery or specialized investigations? Using data from the Canadian Joint Replacement Registry, CIHI (2006) estimated that specialist waits account for approximately 30% of a patient's total wait for joint replacement, with the largest wait (accounting for 60% of the total wait) occurring between the time a decision to operate was made and the actual date of surgery. Similarly, data from Nova Scotia show that 30% of the total wait for cardiac surgery occurs from the referral to a specialist visit (Legare et al. 2010). A CIHI (2008) publication reported that there is a wait of 210 days in Ontario from the time a decision is made to treat, to joint replacement surgery. Our data (for an orthopaedic wait of 80 days) corroborate CIHI's assertion that specialist waits account for close to a third of a patient's total wait for treatment.
From a policy perspective, the good news is that waiting time in our sample is not associated with SES. Instead, patient age, sex and severity – which can be considered proxies for need – are associated with wait times, providing evidence that there is equity in waiting times in our sample.
Over the long term, our analysis provides a baseline view of specialist waits in southwestern Ontario, and can be used to track progress in decreasing such waits over time, subsequent to policy interventions. The advantage of our method is that it focuses on the originating practice, thus enabling us to track multiple types of specialist visits. In contrast, studies that assess such wait times using specialist medical records (or EMR data) are able to track waits only for that particular specialty. Our analyses can also inform the discussion about the setting up of medically acceptable wait times – for example, as has been done by some specialty societies (albeit by using a consensus methodology) (Farrell et al. 2008; Paterson et al. 2006). We can also assess waits against recommended benchmarks. For example, our data show that nearly 30% of women in our sample who were referred to specialists because of abnormal uterine bleeding waited longer than the period of time recommended by the Society of Obstetricians and Gynaecologists of Canada, with younger women more likely to wait longer (Bondy et al. 2010).
Our results can also help to identify areas where wait times are relatively long – such as gastroenterology and orthopaedics, which can then be evaluated to ascertain the reason(s) why. Last, but certainly not least, by analyzing variations in specialty waits by practice, practices with low waits can be identified for further study. For example, while neurosurgery waits were uniformly long in all practices (Figure 2), Practice 9 had a comparatively shorter wait. Similarly, Practice 9 had a shorter wait for orthopaedic surgery, compared to the other practices in the sample. These practices could be studied further to ascertain the reasons these waits are shorter and whether best practices are identified (for example, have they implemented the “advanced access” or pooled referrals model?), and this information could be shared across all practices.
Strengths and limitations
Certain caveats should be kept in mind as one interprets our findings. Our results are not adjusted for specialist supply. One would expect that practices located in areas with limited specialist availability would have longer waits, and if FSAs in these areas also tended to have higher average incomes, a tendency to give faster access to higher-income patients could be countered by limited availability, resulting in similar wait times. Although this may seem somewhat improbable, our data did not allow us to adjust for this potential confounder. For reasons of privacy, we were able to abstract only the first three digits of the postal code and thus were able to obtain only median income at the FSA level. In addition, physicians who adopt EMRs may not be fully representative of the average family physician, and only a minority of primary healthcare physicians use EMRs in Canada (Schoen et al. 2006). Nonetheless, we feel our data are valuable in that they provide a baseline for future discussion and analysis.
Conclusion
Data from our EMR-based researchable database indicate that the median wait to see a specialist in southwestern Ontario is 53 days, with longer waits for neurosurgery and orthopaedic surgery visits, and shorter waits for paediatrician visits. There are significant variations between specialties and by practice, and further research is needed to understand the specific reasons for these. Future work should model the patient-, physician- and contextual-level factors that determine specialist wait times.
Acknowledgements
Dr. Thind is funded by a Canada Research Chair in Health Services Research. Dr. Moira Stewart is funded by the Dr. Brian W. Gilbert Canada Research Chair. The DELPHI project was funded by the Canada Foundation for Innovation and Primary Health Care Transition Fund; the E-WAITS Project was funded by the Canadian Institutes of Health Research.
Contributor Information
Amardeep Thind, Associate Professor & Canada Research Chair in Health Services Research, Department of Epidemiology & Biostatistics, Department of Family Medicine, Schulich School of Medicine & Dentistry, University of Western Ontario, London, ON.
Moira Stewart, Professor & Canada Research Chair in Primary Care, Department of Family Medicine, Schulich School of Medicine & Dentistry, University of Western Ontario, London, ON.
Douglas Manuel, PHAC/CIHR Chair in Applied Public Health Sciences & Senior Scientist, Ottawa Health Research Institute, Ottawa, ON.
Tom Freeman, Professor, Department of Family Medicine, Schulich School of Medicine & Dentistry, University of Western Ontario, London, ON.
Amanda Terry, Assistant Professor, Department of Family Medicine, Schulich School of Medicine & Dentistry, University of Western Ontario, London, ON.
Vijaya Chevendra, Systems Analyst, DELPHI Project, Department of Family Medicine, Schulich School of Medicine & Dentistry, University of Western Ontario, London, ON.
Heather Maddocks, Data Analyst, DELPHI Project, Department of Family Medicine, Schulich School of Medicine & Dentistry, University of Western Ontario, London, ON.
Neil Marshall, Liaison Physician, Department of Family Medicine, Schulich School of Medicine & Dentistry, University of Western Ontario, London, ON.
References
- Aday L.A., Andersen R.M. 1981. “Equity of Access to Medical Care: A Conceptual and Empirical Overview.” Medical Care 19(12): 4–27 [PubMed] [Google Scholar]
- Alter D.A., Naylor C.D., Austin P., Tu J.V. 1999. “Effects of Socioeconomic Status on Access to Invasive Cardiac Procedures and on Mortality After Acute Myocardial Infarction.” New England Journal of Medicine 341(18): 1359–67 [DOI] [PubMed] [Google Scholar]
- Appleby J. 2011. “What's Happening to Waiting Times?” British Medical Journal 342: d1235. [DOI] [PubMed] [Google Scholar]
- Armstrong D., Barkun A.N., Chen Y., Daniels S., Hollingworth R., Hunt R.H., Leddin D. 2008. “Access to Specialist Gastroenterology Care in Canada: The Practice Audit in Gastroenterology (PAGE) Wait Times Program.” Canadian Journal of Gastroenterology 22(2): 155–60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barua B., Rovere M., Skinner B. 2010. Waiting Your Turn: Wait Times for Health Care in Canada (20th ed.). Vancouver: Fraser Institute. [Google Scholar]
- Bondy J.N., Thind A., Stewart M., Manuel D., Freeman T. 2010. “Wait Times for Women with Abnormal Uterine Bleeding in South-Western Ontario.” Journal of Obstetrics and Gynaecology Canada 32(7): 703–07 [DOI] [PubMed] [Google Scholar]
- Canadian Institute for Health Information (CIHI). 2008. Wait Times Tables – A Comparison by Province (p. 25). Toronto: Author. [Google Scholar]
- Canadian Institute for Health Information (CIHI). 2006. Waiting for Health Care in Canada: What We Know and What We Don't Know. Toronto: Author. [Google Scholar]
- Carriere G., Sanmartin C. 2010. “Waiting Time for Medical Specialist Consultations in Canada, 2007.” Health Reports 21(2): 7–14 [PubMed] [Google Scholar]
- Coyte P.C., Wright J.G., Hawker G.A., Bombardier C., Dittus R.S., Paul J.E., Freund D.A., Ho E. 1994. “Waiting Times for Knee-Replacement Surgery in the United States and Ontario.” New England Journal of Medicine 331(16): 1068–71 [DOI] [PubMed] [Google Scholar]
- Farrell S., Roye C., Crane J., Davis D., Heywood M., Lalonde A., Leyland N., Senikas V., Menard C., Lefebvre G. 2008. “Statement on Wait Times in Obstetrics and Gynaecology.” Journal of Obstetrics and Gynaecology Canada 30(3): 248–70 [DOI] [PubMed] [Google Scholar]
- Gorey K.M., Luginaah I.N., Holowaty E.J., Fung K.Y., Hamm C. 2009. “Wait Times for Surgical and Adjuvant Radiation Treatment of Breast Cancer in Canada and the United States: Greater Socioeconomic Inequity in America.” Clinical & Investigative Medicine 32(3): E239–49 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ho E., Coyte P.C., Bombardier C., Hawker G., Wright J.G. 1994. “Ontario Patients' Acceptance of Waiting Times for Knee Replacements.” Journal of Rheumatology 21(11): 2101–05 [PubMed] [Google Scholar]
- Johnston G.M., MacGarvie V.L., Elliott D., Dewar R.A., MacIntyre M.M., Nolan M.C. 2004. “Radiotherapy Wait Times for Patients with a Diagnosis of Invasive Cancer, 1992–2000.” Clinical & Investigative Medicine 27(3): 142–56 [PubMed] [Google Scholar]
- Lau R., Vair B.A., Porter G.A. 2007. “Factors Influencing Waiting Times for Elective Laparoscopic Cholecystectomy.” Canadian Journal of Surgery 50(1): 34–38 [PMC free article] [PubMed] [Google Scholar]
- Legare J.F., Li D., Buth K.J. 2010. “How Established Wait Time Benchmarks Significantly Underestimate Total Wait Times for Cardiac Surgery.” Canadian Journal of Cardiology 26(1): e17–21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung A.K., DeAngelis D.D., Hurwitz J.J., Simpson E.R., Oestreicher J.H., Ing E., Hurwitz G. 2007. “Surgical Waiting Times for Ocular and Periocular Cancer Patients in Toronto.” Canadian Journal of Ophthalmology 42(6): 826–31 [DOI] [PubMed] [Google Scholar]
- Massel D. 1999. “Access to an Outpatient Cardiology Consultation in Southwestern Ontario.” Canadian Journal of Cardiology 15(8): 879–83 [PubMed] [Google Scholar]
- Olson D.W., de Gara C.J. 2002. “How Long Do Patients Wait for Elective General Surgery?” Canadian Journal of Surgery 45(1): 31–33 [PMC free article] [PubMed] [Google Scholar]
- Paszat L.F., Mackillop W.J., Groome P.A., Zhang-Salomons J., Schulze K., Holowaty E. 1998. “Radiotherapy for Breast Cancer in Ontario: Rate Variation Associated with Region, Age and Income.” Journal of Clinical Investigation 21(3): 125–34 [PubMed] [Google Scholar]
- Paterson W.G., Depew W.T., Pare P., Petrunia D., Switzer C., Veldhuyzen S.J., van Zanten, Daniels S. 2006. “Canadian Consensus on Medically Acceptable Wait Times for Digestive Health Care.” Canadian Journal of Gastroenterology 20(6): 411–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pletcher B.A., Rimsza M.E., Cull W.L., Shipman S.A., Shugerman R.P., O'Connor K.G. 2010. “Primary Care Pediatricians' Satisfaction with Subspecialty Care, Perceived Supply, and Barriers to Care.” Journal of Pediatric Gastroenterology and Nutrition 156(6): 1011–15 [DOI] [PubMed] [Google Scholar]
- Schoen C., Osborn R., Huynh P.T., Doty M., Peugh J., Zapert K. 2006. “On the Front Lines of Care: Primary Care Doctors' Office Systems, Experiences, and Views in Seven Countries.” Health Affairs 25(6): w555–71 [DOI] [PubMed] [Google Scholar]
- Shortt S.E., Shaw R.A. 2003. “Equity in Canadian Health Care: Does Socioeconomic Status Affect Waiting Times for Elective Surgery?” Canadian Medical Association Journal 168(4): 413–16 [PMC free article] [PubMed] [Google Scholar]
- Simunovic M., Gagliardi A., McCready D., Coates A., Levine M., DePetrillo D. 2001. “A Snapshot of Waiting Times for Cancer Surgery Provided by Surgeons Affiliated with Regional Cancer Centres in Ontario.” Canadian Medical Association Journal 165(4): 421–25 [PMC free article] [PubMed] [Google Scholar]
- Singh H., De Coster C., Shu E., Fradette K., Latosinsky S., Pitz M., Cheang M., Turner D. 2010. “Wait Times from Presentation to Treatment for Colorectal Cancer: A Population-Based Study.” Canadian Journal of Gastroenterology 24(1): 33–39 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snider M.G., MacDonald S.J., Pototschnik R. 2005. “Waiting Times and Patient Perspectives for Total Hip and Knee Arthroplasty in Rural and Urban Ontario.” Canadian Journal of Surgery 48(5): 355–60 [PMC free article] [PubMed] [Google Scholar]
- Stanway A., Oakley A., Rademaker M., Duffill M. 2004. “Audit of Acute Referrals to the Department of Dermatology at Waikato Hospital: Comparison with National Access Criteria for First Specialist Appointment.” New Zealand Medical Journal 117(1192): U849. [PubMed] [Google Scholar]
- Statacorp. 2010. Stata Statistical Software: Release 11.0 (Version 10.0). College Station, TX: Author. [Google Scholar]
- Statistics Canada. 2006. (July). Access to Health Care Services in Canada, January to December 2005 (p. 25). Ottawa: Author. [Google Scholar]
- Stewart M., Thind A., Terry A.L., Chevendra V., Marshall J.N. 2009. “Implementing and Maintaining a Researchable Database from Electronic Medical Records: A Perspective from an Academic Family Medicine Department.” Healthcare Policy 5(2): 26–39 [PMC free article] [PubMed] [Google Scholar]
- Trypuc J., Hudson A., MacLeod H. 2006. “Ontario's Wait Time Strategy: Part 1.” Healthcare Quarterly 9(2): 44–51, 42 [DOI] [PubMed] [Google Scholar]
- Wait Time Alliance. Time Out! Report Card on Wait Times in Canada. 2011. Retrieved June 11, 2012. < http://www.waittimealliance.ca/media/2011reportcard/WTA2011-reportcard_e.pdf>.
- Wright J.G., Menaker R.J. 2011. “Waiting for Children's Surgery in Canada: The Canadian Paediatric Surgical Wait Times Project.” Canadian Medical Association Journal 183(9): E559–64 [DOI] [PMC free article] [PubMed] [Google Scholar]