Abstract
Objectives:
Asthma is a common disease that is sometimes fatal. Its prevalence, morbidity and mortality are increasing. The objective of this paper was to evaluate the proficiency of primary care physicians in general knowledge, diagnosis, classification of severity and management of asthma along the guidelines of the Saudi National Asthma Protocol, and to analyze the association of their proficiency level with certain professional standards.
Methods:
This was a cross-sectional study conducted in the Department of Family Medicine and the Main Air Base Clinic at the North-West Armed Forces Hospital in Tabuk City, Saudi Arabia from the 1st to the 29th of June 2001. All 44 primary care physicians working there at the time were enrolled in the study. A self-administered true/false questionnaire prepared by the Saudi National Asthma Scientific Committee was completed by all physicians. The Passing score was ≥ 50%.
Results:
Only 39% of the physicians passed the test as a whole, with 66% passed in general knowledge, 70% in diagnosis, 48% in the classification of severity and 59% in the management of asthma. There was an association between significant achievement and Family Medicine Board Certification as well as some knowledge of the National Asthma Protocol (p ≥ 0.05). No association was observed with attendance of asthma training courses. There was positive significant correlation between the knowledge score, the management scores and the total scores of physicians.
Conclusion:
The level of awareness of the National Asthma Protocol among the primary care physicians was low (52%). Their proficiency in general knowledge, diagnosis, classification of severity and management was also low. A higher standard was associated with Family Medicine Board Certification. Further studies to identify the reasons for these deficiencies need to be carried out so that measures could be taken to rectify the situation.
Keywords: Asthma, Family physicians, National Protocol for Asthma Diagnosis and Management, Evaluation
INTRODUCTION
Asthma is a common chronic inflammatory disease.1 It causes intermittent or chronic symptoms of airflow obstruction which can be fatal. Its prevalence, morbidity and mortality are increasing for various reasons, including the improper use of medications,2 urbanization, increased exposure to indoor allergens, occupational exposure,3 delay in asthma diagnosis and incompetent medical care.4,5 In Saudi Arabia, it has reached a prevalence rate of 10-24%, which is higher than in many other countries.6
To improve the quality of asthma care, two approaches were tried: the establishment of unified clinical guidelines for its diagnosis and management; and the improvement of the knowledge and attitude of asthma patients. The Saudi National Asthma Protocol (SNAP) was first published in 1995, and was updated in 1997.8
The main objective of this study was to evaluate the competence of primary care physicians (PCP) working in the Family Medicine Department and Main Air Base Clinic in the North-West Armed Forces Hospital, in their knowledge and management of asthma. The association between certain professional characteristics of PCPs and their proficiency level were also analyzed. This study will hopefully provide useful information for the purpose of improving the health care of asthma patients.
METHODS
This is a cross-sectional descriptive and analytical study. The study subjects were all PCPs working in the Family Medicine Department and the Main Air Base Clinic in the North-West Armed Forces Hospital, Tabuk City, Saudi Arabia. Some of these PCPs had only basic MBBS, and others had the Family Medicine Board Certificate or had other training courses. PCPs who were on vacation, and those who had participated in the pilot study, five and eight respectively, were not included in the study. The evaluation was done by a self-administered true/false (T/F) questionnaire prepared by the Al Qaseem National Asthma Scientific Committee meeting held in 2001 (personal communication). The Committee derived the components of the test and standard criteria for quality judgement from the SNAP (2nd ed). The questionnaire consisted of 15 questions divided into four components, as follows: General knowledge (4 questions), diagnosis (4 questions), classification of severity (3 questions), and management of asthma (4 questions).
The minimum pass level was ≥ 50%. Validation of the questionnaire was carried out by the Asthma Scientific Committee. The associated characteristics of PCPs included age, gender, qualification and training courses attended, and awareness of the SNAP.
Data were collected from the 1st to the 29th of July 2001. The biodata and results of the test were coded and processed in a personal computer using SPSS software.10 The data were entered by a double entry method to decrease data entry errors. T-test, chi-square test and Fisher's exact test were used as tests of significance. The level of statistical significance was set at p ≤ 0.05.
RESULTS
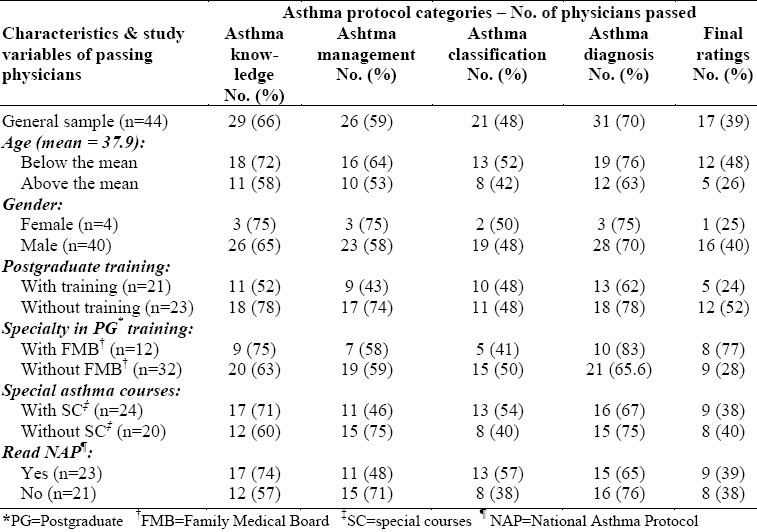
Forty-four physicians constituting all the doctors working in the PC facilities at that time were included in the study. They all completed the self-administered questionnaire, which included the T/F test and the demographic variables. The results are shown in Table 1.
Table 1.
Frequency distribution of the characteristics of the 17 passing physicians by the asthma protocol test categories
Of the 44 physicians in the study, 40 (90%) were males and 4 (10%) were females. Their ages ranged from 29 to 53, with a mean age of 37.9 years (± 3.2).
Twelve (27%) were Family Medicine Board Certified, 21 (48%) had GP post-graduate training, 24 (55%) GPs had attended other education courses, and only 23 (52%) were aware of and had read SNAP.
Using ≥ 50% as the minimum pass level, only seventeen (39%) GPs passed the test. The scores achieved in the four components of the asthma test and the scores of the physicians who had taken extra educational courses are detailed in Table 1. GPs who had the Family Board Certificate scored better in general knowledge (75%), and in diagnosis of asthma (83%), in management (58%), and in the total (70%) than those who did not have the board certification. The scores in knowledge were correlated with the achievement scores in management, the total test, in the classification of severity of asthma, and those on diagnosis.
Multiple regression tests showed a statistically significant positive correlation at the p≤0.05 level between the management scores (outcome variable) and the knowledge score percentages. A positive correlation also existed between the percentage of the knowledge score and the percentage total score at the statistical significance level of 0.01. Other factors, like classification of severity of asthma score percentage and the diagnosis score percentage, showed no statistically signifi-cant correlation with the knowledge score.
DISCUSSION
The PCPs’ overall level of achievement in the test was low, for only 17 (39%) passed at the cut-off point of 50%. This is an important finding. Since asthma is a common disease that can be serious and life-threatening, fast treatment is crucial.1 Achievement in asthma knowledge was highest (72%) in the younger age group below the mean of 37.9 years. The number of females was too small4 for any valid conclusions to be drawn on gender. The PCPs who were Family Medicine Board Certified got statistically significantly better scores (p < 0.05), in both the general knowledge of asthma (75%), and in the diagnosis of asthma (83%) than those who were not. There was no satisfactory significant impact on the two components “classification of severity” and “the management of asthma” (Table 1).
The low achievement level on the “diagnosis of asthma problem” among doctors is supported by Al-Haddad, et al, in the Medina region of Saudi Arabia.11 Attendance of training courses on asthma was not associated with greater achievement in any of the four components of the test. These results contradict the findings of Al-Haddad and colleagues’ after they had launched a training course on asthma management.11 However in the present study, there was no indication of time lapse after training. This may have distorted the study findings.
The PCPs (74%) who had read the NAP attained higher scores on the general knowledge of asthma and the classification of the severity of asthma components (Table 1). No significant impact was observed on the components of diagnosis and management of asthma. Many studies support the positive impact of educational programmes,12 short, concise summaries with frequent reminders,13 and other types of training programs had on the knowledge of asthma.14,15 In this study, the lack of learning in diagnosis and management of asthma components may be due to the fact that these were concerned with practice, rather than knowledge only.
Kibbe et al, Gergen and Goldstein pointed out that in order to be effective in controlling variations in clinical practice, guidelines should be integrated into the total clinical process design, rather than focus on physicians, since patients play a major role in the success of chronic asthma control.12,16
Mobureek et al, reported that four major Riyadh hospitals did not follow the Saudi NAP guidelines.17 Reasons were not given for their findings. However, studies similar to the Mobureek et al study and to the present one, need to be repeated after the Saudi NAP has been distributed to all PCPs working in the Kingdom, and after appropriate training programs on the management of asthma have been given. Khoja and Al-Ansary18 emphasized the major role played by PCPs in the management of asthma stating that they should be provided with the essential equipment and facilities to carry out their duties effectively.
The NAP itself will be more useful and reader-friendly for PCPs if it were condensed or supplemented with a pocket guide or summaries. It will also be helpful for other health workers for it to be translated into Arabic.
REFERENCES
- 1.Chesnutt MS, Prendergast TJ. Lung. In: Tierney LM, McPhee SJ, Papadakis MA, editors. Current medical diagnosis and treatment. 2001 ed. New York: Lange Medical Books/McGraw-Hill; 2001. p. 272. [Google Scholar]
- 2.Tsang K, Lam W, Ip M, et al. Inability of physicians to use metered dose inhalers”. Journal of Asthma. 1997;34(6):493–8. doi: 10.3109/02770909709055393. [DOI] [PubMed] [Google Scholar]
- 3.Creticos PS, Reed CE, Norman PS, et al. Ragweed immunotherapy in adult asthma. N Eng J Med. 1996;334:501–6. doi: 10.1056/NEJM199602223340804. [DOI] [PubMed] [Google Scholar]
- 4.Gallert AR, Gellert SL, Illife SR. Prevalence and management of asthma in a London inner city general practice. Br J Gen Practice. 1990:4097–201. [PMC free article] [PubMed] [Google Scholar]
- 5.Wilson SR, Scamagas P, German DF, et al. A controlled trial of two forms of self-management education for adults with asthma”. Am J Med. 1993;94:564–74. doi: 10.1016/0002-9343(93)90206-5. [DOI] [PubMed] [Google Scholar]
- 6.Alfrayah A, Hasnain S, Gadelrab M, Alsedaairy S. Prevalence of asthma in three regions of Saudi Arabia. European Respiratory J. 1998;12(suppl 29):52s. [Google Scholar]
- 7.National Asthma Campaign (UK) National asthma audit 1999/2000. 1999 Aug [Google Scholar]
- 8.2nd ed. Riyadh, Saudi Arabia: Ministry of Health Publication; 1997. National Protocol for the Diagnosis and Management of Asthma. [Google Scholar]
- 9.Barbin B, Kelly Y. Prevalence of childhood asthma in tropics. Annals of Tropical Medicine. 1998;18(Suppl):s33–s39. doi: 10.1080/02724936.1998.11747978. [DOI] [PubMed] [Google Scholar]
- 10.Statistical Package for Social Sciences (computer program), Windows version 6.0, Microsoft. 1993 [Google Scholar]
- 11.Al-Haddad N, Al-Ansari S, Al-Shari A, et al. Impact of asthma education program on asthma knowledge of general practitioner. Saudi Med J. 1996;175:347–50. doi: 10.5144/0256-4947.1997.550. [DOI] [PubMed] [Google Scholar]
- 12.Gergen PJ, Goldstein RA. Does asthma education equal asthma intervention? Int Arch Allergy Immunol. 1995;107:166–8. doi: 10.1159/000236966. [DOI] [PubMed] [Google Scholar]
- 13.Resnick DJ, Gold RL, Lee-Wong, et al. Physicians’ metered dose inhaler techniques after a single teaching session. Ann Allergy Asthma Immunol. 1996;76:145–8. doi: 10.1016/S1081-1206(10)63413-8. [DOI] [PubMed] [Google Scholar]
- 14.Lantner RR, Ros SP. Emergency management of asthma in children: impact of NIH guidelines. Ann Allergy Asthma Immunol. 1995;74:188–91. [PubMed] [Google Scholar]
- 15.Duke T, Kellerman A, Ellis R, et al. Asthma in the emergency department impact of a protocol on optimizing therapy. Am J Emerg Med. 1991;9:432–5. doi: 10.1016/0735-6757(91)90208-2. [DOI] [PubMed] [Google Scholar]
- 16.Kibbe DC, Kallzny AD, McLaughlin CP. Integrating guidelines with continuous quality improvement: doing the right thing the right way to achieve the right goals”. J Comm J Qual Improv. 1994;20:181–91. doi: 10.1016/s1070-3241(16)30060-8. [DOI] [PubMed] [Google Scholar]
- 17.Mobeireek A, Gee J, Al-Mobeireek K, et al. Prescribing for asthma in the outpatient clinics in Riyadh: does it follow the guidelines? Ann Saudi Med. 1996;16:497–500. doi: 10.5144/0256-4947.1996.497. [DOI] [PubMed] [Google Scholar]
- 18.Khoja TA, Al Ansany LA. Asthma in Saudi Arabia: is the system appropriate for optimal primary care?”. J Public Health Management Protocol. 1998;4(3):64–72. doi: 10.1097/00124784-199805000-00008. [DOI] [PubMed] [Google Scholar]


