Abstract
Background:
Knowing patients’ expectation for medication after each consultation is of the utmost importance in designing public education programs on the rational use of drugs.
Objective:
To determine whether patients in Riyadh, Saudi Arabia, expect drugs after each primary care consultation.
Subjects and Methods:
A sample of 985 Saudi patients aged 15 and above was randomly selected. A cross-sectional survey was carried out at five randomly selected primary care centers, using a self-administered questionnaire distributed to patients before being seen by primary care doctors.
Results:
Most patients (87.8%) always expect drug prescriptions. Eighty nine percent (88.9%) had been prescribed drugs in the previous consultation. Sixty six percent (66%) had received 2-3 drugs during their previous consultation. The majority thought it was too much. Seventy percent (70%) took all their prescribed drugs. Patients with intermediate and high school education had the highest compliance rate (32%). Twenty two percent (22%) thought it was always necessary to use a drug for an illness. The level of education of the majority of patients ranged from illiterate to various levels of pre-university education.
Conclusion:
Most Saudi patients expect drugs. General and specific health education should be given to both patients and doctors.
Keywords: Patients’ expectation, Drug prescription, Primary health care, Saudi Arabia
INTRODUCTION
Irrational use of drugs is a known factor for increased morbidity stemming from the evolution of resistant strains as result of misuse of antibiotics. In addition, irregular use of drugs is a known factor for the poor control of chronic diseases such as hypertension and diabetes mellitus. This increases the risks of complications of cerebro-vascular accidents, amputations and blindness and chronic disabilities. The prescription of medicines is one of the most important factors in the rising costs of health services in both developing and developed countries.1–2
The annual budget of the Ministry of Health (MOH) in Saudi Arabia is rising. In 1979, 2.61% of the national budget was given to the MOH. Seventeen years later it rose to 4.9%.3,4
In 1993, the prescribing rate in Riyadh ranged between 10.2 and 11.8 prescriptions per patient per year.5 This is greater than that reported for the UK: 7.0, Australia: 7.7 and Sweden: 4.7. Felimban FM5 found that 85% of consultations ended with a prescription.
Patients strive for recognition of their views in their encounter with doctors.6,8 Bradley9 found that the commonest reason given by doctors for prescribing medicine is patients’ expectations. It was also found that when doctors did not live up to the patient's expectations, there was dissatisfaction resulting in a negative effect on the outcome of the therapy.8,10–13 Some patients may thus receive prescriptions when they actually do not need them. This suggests that unwanted prescriptions might be responsible for drug wastage.11
The concept of patients’ demands for prescriptions is familiar to many General Practitioners (GPs). Current research evidence shows that doctors cite patients’ demands as a factor in their prescribing habits.9,11,14,15 Stimson16 showed a linear relation between the doctors’ estimations of their patients’ expectation for drugs and their own prescribing rates.
Though many studies have been conducted in the far East17 and in the West9,11,14,15,18,19 around patient's expectations and their effect on doctor's prescriptions,9,11,14,15 only a few have been done in Saudi Arabia.1,5,20
The aim of the current study is to find out whether patients expect a medication with each primary care consultation.
SUBJECTS AND METHODS
There are 68 primary health care centers (PHCC) in Riyadh city. The current cross-sectional survey was conducted at five, randomly selected, PHCC, representing different geographical areas (north, south, west, east & center) of Riyadh city during the month of January 1997. A systematic random sampling was used to select every third Saudi patient aged 15 and above. A self-administered anonymous questionnaire was given to the selected patients before they consulted their primary care doctors.
The questionnaire included nine questions, divided into two parts. The first part represented patient's expectations for the present consultation, while the second part represented questions related to the previous consultation. Non-Saudis were excluded from the study. Only medical cases were included.
A pilot study was conducted among (20) patients (10 males and 10 females) at King Khalid University Academic Primary Care Clinics. The questionnaire was modified according to the responses received.
Among the illiterate, the questionnaire was completed through an interview, so patients’ responses may have been influenced by the interviewer.
The data were analyzed using SPSS/PC statistical package.21 Chi-square statistical test was used to compare the categorical variables. P-value <0.05 was considered as significant.
RESULTS
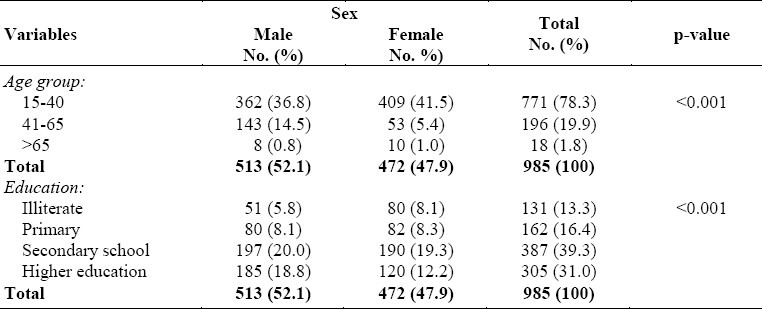
One thousand and fourteen patients (1014) were enrolled in the study. All responded. However, 29 questionnaires were excluded because they were either dental cases or the information given was incomplete. Questionnaires included in the final analysis were 985 (97.1%). About half (52.1%) of the 985 patients were males. The demographic characteristics of the study sample are shown in Table 1.
Table 1.
The sociodemographic characteristics of patients attending PHC centers in Riyadh, Saudi Arabia
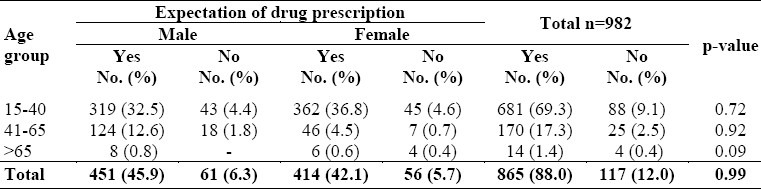
Most patients (88.0%), 46.0% of whom were males expected drug prescriptions (Table 2). The most frequent reasons given for not expecting drugs were reassurance and request for laboratory tests (36.9% and 15.5% respectively). Whereas the least frequent reason for not expecting drugs was that the participants were already on medication (2.4%).
Table 2.
Patient's expectations of drug prescription in relation to age and sex in Riyadh PHC centers, Saudi Arabia
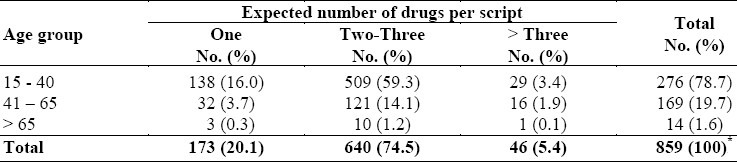
The majority (74.5%) of patients expected two to three drugs per prescription. A prescription of more than three drugs were expected by the lowest number of patients (5.4%) (Table 3).
Table 3.
Patients’ expectations of drugs per prescription in relation to age at Riyadh PHC centers, Saudi Arabia
Twenty two percent of the patients thought that it was always necessary to use a drug for any illness. Their educational level was below university level (Table 4).
Table 4.
Medication behavior of PHC patients in relation to education level at Riyadh, Saudi Arabia
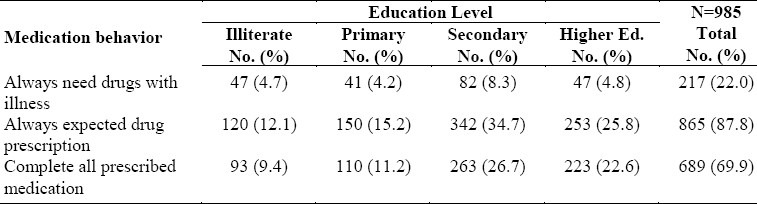
The percentage of patients who completed their prescribed drugs was (69.6%). In this category those with university or higher education was 22.6% as shown in Table 4.
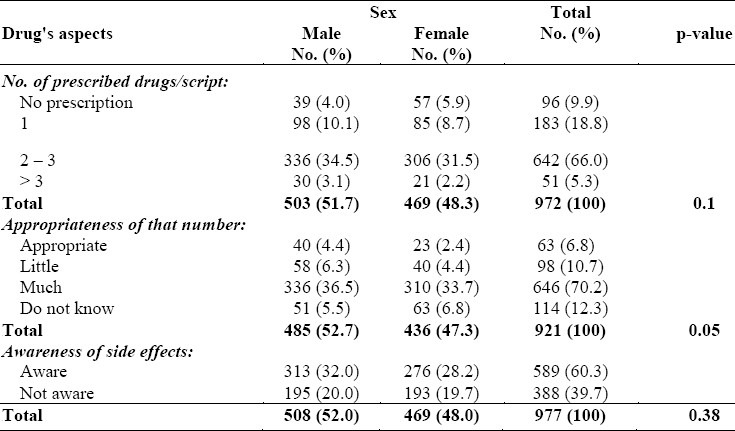
Two thirds (66%) of the patients were given two to three drugs per prescription during their previous consultation. The majority of them (70.2%) thought that the drugs prescribed were too many.
Sixty percent of the patients were aware of the side effects, but there was no statistically significant difference between male and female patients (p 0.38) (Table 5).
Table 5.
PHC patient's views toward previously prescribed drugs in relation to sex at Riyadh, Saudi Arabia
The main source of awareness was personal experience with drugs (23.7%), followed by the media or the reading of medical books (21.0%). However, only 13.5% of the information was given by doctors.
DISCUSSION
One part of the questionnaire concerned the previous consultation, giving rise to recall bias.
The finding that most patients were below 65 years of age is consistent with demographic picture of Saudi Arabia as a young population.
The majority of patients thought that it was not always necessary to take a drug for an illness. However, most Saudi patients expected to be given a prescription when they went to consult their primary care doctors. This is higher than that found in Western11,16,22,23 and Eastern17 populations.
The high drug-prescription rate might be due to doctor's habits and patients’ beliefs. Doctors may contribute to this by their prescribing habits, prescribing too readily because of over estimation of patients’ expectations for drugs.11,16,17,22,23 Generally, doctors prescribe to satisfy their patients since they believe that the patients might go to another doctor to seek the advice. Also, high prescribing rate may be because drugs are prescribed free of charge in Saudi PHCC.5,24 Hence, over-prescribing makes life easier for doctors as it reduces consultation time and increases the number of patients seen every day.5,11
However, low education level of the patients was found to be associated with this high expectation percentage, as the majority of those who expected drugs ranged between illiterate to having pre-university level of education.
This belief in medication decreased with the higher level of education i.e., the groups with higher education.
Although the majority of patients had been given 2-3 drugs per prescription in the previous consultation, they thought they were too many. This may explain why about 2/3 of patients expected 2-3 drugs in the current consultation. Physicians usually prescribed 2-3 drugs because according to the quality assurance manual of MOH, they could write up to a maximum of three drugs per prescription.25
A high percentage of patients were not aware of the side effects of drugs, which indicates inadequate health education. This may be because of the faith patients had in doctors. “A doctor could not possibly harm me!”
Among those who were aware of side effects, only 13.5% of them obtained their information from doctors. This reflects the lack of information from doctors.5
Among those who did not expect drugs, the most frequent reason was reassurance. This is consistent with the finding of other studies.11
In conclusion, this study has shown that most patients always expect drug prescriptions. Most of the patients had been prescribed drugs in previous consultations. About a quarter of the patients thought it was always necessary to use a drug for any illness. The majority of these ranged from illiterate to those with various degrees of pre-university education. It is recommended that primary care physicians should play a major role in patients’ education, particularly on the optimal use of drug therapy in patient care, and the harmful effects of drugs. There should be better doctor-patient communication to improve the awareness of patients’ expectations. It is also recommended that physicians restrict their prescriptions to what the patient really needs. General and specific health education measures should be given to patients, assistant pharmacists and doctors.
ACKNOWLEDGMENT
I would like to thank the following students; Hatem A. Kalantan, Thamer A. Nouh, Khaldoon A. Al-Jerian, Aous A. Mansouri and Riyadh M. Al-Bgumi, for their great assistance.
REFERENCES
- 1.Al-Nasser A. Prescribing Patterns in Primary Health Care in Saudi Arabia DICP. The Annals of Pharmacotherapy. 1991;25:90–3. doi: 10.1177/106002809102500116. [DOI] [PubMed] [Google Scholar]
- 2.Jolleys J. How to prescribe efficiently. Practice Update. 1989;3:411–5. [Google Scholar]
- 3.Annual Health Report. Riyadh: Ministry of Health; 1979. Ministry of Health (Saudi Arabia) [Google Scholar]
- 4.Annual Health Report. Riyadh: Dar Al-Hilal Printing Press; 1995. Ministry of Health (Saudi Arabia) [Google Scholar]
- 5.Felimban FM. The prescribing practice of primary health care physicians in Riyadh City. Saudi Medical J. 1993;14(4):353–8. [Google Scholar]
- 6.Neville R, Robertson F, Livingstone S, Crombie I. A classification of prescribing errors. J R Coll Gen Pract. 1989;39:110–2. [PMC free article] [PubMed] [Google Scholar]
- 7.Calnan M. Health and Illness: The lay perspective. London: Tavistock Publications; 1987. [Google Scholar]
- 8.Verbeek-Heida PM. How patients look at drug therapy: consequences for therapy negotiations in medical consultations. Family Practice. 1993;10(3):326–9. doi: 10.1093/fampra/10.3.326. [DOI] [PubMed] [Google Scholar]
- 9.Bradley CP. Uncomfortable prescribing decisions: a critical incident study. BMJ. 1992;304:294–6. doi: 10.1136/bmj.304.6822.294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Britt H, Harris M, Driver B, et al. Reasons for encounter and diagnosed health problems: convergence between doctors and patients. Fam Pract. 1992;9:191–4. doi: 10.1093/fampra/9.2.191. [DOI] [PubMed] [Google Scholar]
- 11.Britten N. patient demand for prescriptions: a view from the other side. Family Practice. 1994;11(1):62–6. doi: 10.1093/fampra/11.1.62. [DOI] [PubMed] [Google Scholar]
- 12.Salisbury C. How do people choose their doctor? BMJ. 1989;299:608–10. doi: 10.1136/bmj.299.6699.608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Billinghurst B, Whitfield M. Why do patients change their general practitioner. A postal questionnaire study of patients in Avon? Br J Gen Pract. 1993;43:336–8. [PMC free article] [PubMed] [Google Scholar]
- 14.Schwartz RK, Soumerai SB, Avorn J. Physician motivations for non-scientific drug prescribing. Soc Sci Med. 1989;28:577–82. doi: 10.1016/0277-9536(89)90252-9. [DOI] [PubMed] [Google Scholar]
- 15.Comaroff J. A bitter pill to swallow: placebo therapy in general practice. Soc Rev. 1976;24:79–96. doi: 10.1111/j.1467-954x.1976.tb00574.x. [DOI] [PubMed] [Google Scholar]
- 16.Stimson GV. General Practitioners’ estimates of patient expectations, and other aspects of their work. Swansea: Medical Sociology Research Centre; 1975. [Google Scholar]
- 17.Lam CLK, Catarivas MG, Lauder IJ. A pill for every ill? Family practice. 1995;12(2):171–5. doi: 10.1093/fampra/12.2.171. [DOI] [PubMed] [Google Scholar]
- 18.Kravitz RL. Patients expectation for Medical care: an expanded formulation based on review of the literature. Medical Care Research and Review. 1996;53:3–27. doi: 10.1177/107755879605300101. [DOI] [PubMed] [Google Scholar]
- 19.Kravitz RL. Prevalence and Sources of patient unmet expectations for care: an examination of the factors, that influence a patient's expectations for care in office practice. Ann Intern Med. 1996;125:730–7. doi: 10.7326/0003-4819-125-9-199611010-00004. [DOI] [PubMed] [Google Scholar]
- 20.Al-Abbasi HM, Madani KA. A survey of outpatient prescriptions dispensed in Saudi Arabia. Aust J Hosp Pharm. 1987;3:211–2. [Google Scholar]
- 21.Statistical Package for Social Science. Windows - Version 6.0; Microsoft. 1993 [Google Scholar]
- 22.Virji A, Britten N. A study of the relationship between patients’ attitudes and doctors’ prescribing. Fam Prac. 1991;8:314–9. doi: 10.1093/fampra/8.4.314. [DOI] [PubMed] [Google Scholar]
- 23.Cartwright A, Anderson R. General Practice revisited - a second study of patients and their doctors. London: Tavistock; 1981. [Google Scholar]
- 24.McBride CA, Shugars D.A, DiMatteo, et al. The physician's Role: Views of the public and the profession on seven aspects of patient care. Archives of Family Medicine. 1994;3(11):948–95. doi: 10.1001/archfami.3.11.948. [DOI] [PubMed] [Google Scholar]
- 25.Quality Assurance in Primary Health Care Manual. Riyadh: Dar Al-Hilal Printing Press; 1994. Ministry of Health (Saudi Arabia) [Google Scholar]


