Abstract
Doctor-patient communication is a skill essential for the satisfaction of the patients’ needs and expectations. It involves an art that every practicing physician should have. The situations in health care delivery that demands good doctor-patient communication are many. Diabetes care, the management of hypertension, explaining serious disease diagnoses, prognosis, and investigative procedures are some of the common situations where good doctor-patient communication is very essential. Doctor-patient communication assumes a special status in Saudi Arabia where as a result of mixed ethnicity of the manpower in the health service and the expatriate community, there is a vast diversity of languages, health traditions and beliefs. The skill of doctor-patient communication can be developed and improved by the application of the principles of the patient-centered approach, the utilization of patient-oriented evidence that matters, and its inclusion in the undergraduate curriculum in the first few years of medical school. There should be continuous medical education programs for practicing doctors on the skills of doctor-patient communication through seminars and workshops. This would be a further step towards the improvement of the consumer's well-being.
Keywords: Doctor-patient communication, Saudi Arabia
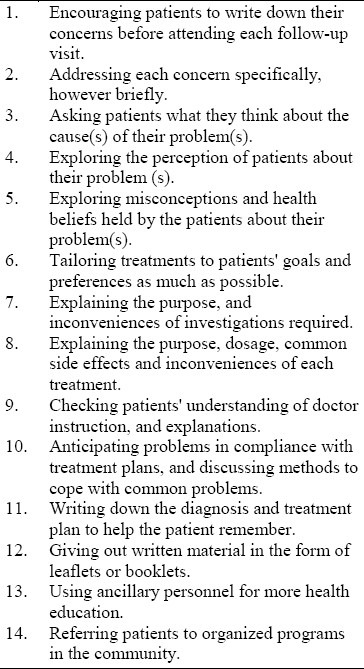
Behavioral medicine strongly stresses the impact of human behavior on illness and health and there is increasing enthusiasm for the advocacy of patient-centered medicine. Simply defined, patient centered medicine means designing patient management according to the patient's needs and expectations1,2 rather than the physician's own agenda. In other words, it is viewed as how the doctor receives the patients and puts them at their ease enough to enable them to express all of their reasons including symptoms, thoughts, feelings and expectations for seeking a consultation.3 In this regard, there is strong evidence that in most cases, physicians and patients hold different views and perceptions on the objective of the consultation.4,5 This situation is resolved by the practice of good doctor-patient communication.6 This is a skill fundamental to all other skills of patient assessment and management. The technique of good doctor-patient communication involves a series of steps (illustrated in Table 1) that must be carried out by the physician.7
Table 1.
Techniques of good doctor-patient communication
There is hardly any area of the patients’ encounter with the physician that does not require the best standard of doctor-patient communication. The process is governed by factors related to the patient, on one hand, and the physician on the other hand. Factors related to patients include, age,8 gender,9,10 language,11,12 level of education, knowledge about illness, and health- or illness-related agenda and expectations. The factors related to the physician include, gender, time of graduation, and specialty,13,14 but most important is the doctor's orientation about the skills in behavioral medicine.
The skill of doctor-patient communication, therefore, is of paramount import-ance among the skills traditionally adopted by the medical profession, yet it is particularly lacking in medical practice in Saudi Arabia. Numerous situations make this obvious, but a few common medical problems will be cited.
Diabetes mellitus is a common problem in Saudi Arabia. It is well known that the management of this problem is dependent on educating patients to acquire self-dependent skills, and the ability to manage themselves.15–17 Training of diabetic patients on self-reliance depends on efficient doctor-patient communication. However, there is evidence that inadequate or poor doctor-patient communication during the consult-ation results in a considerable number of patients leaving with views on diabetes that are different from those the physician wants to convey.18–19 Moreover, there are about 50 misconceptions, held by Saudi diabetic patients about diabetes mellitus.20 Those misconceptions are incompatible with the minimum standard of disease knowledge and control desired and undoubtedly interfere with disease control. The only way to eliminate these misconceptions is by good health education based on good doctor-patient communication.
Another common situation is that of compliance with therapy in the case of chronic diseases. Non-compliance may be intentional or non-intentional. When non-compliance is intentional, the patient does not comply despite his/her knowledge about what is required. In the second group belongs the patient who does not comply unintentionally, usually because of lack of comprehension, that is, a product of doctor-patient communication.21 The list of diseases affected by non-compliance is long. Hypertension, which is as common as diabetes in most communities, Saudi Arabia not excepted, provides another clear illustration. Despite the availability of very powerful drugs for the treatment of hypertension, there is a high proportion of uncontrolled hypertensives, whose poor control is due to poor compliance. A study in Saudi Arabia has shown that a considerable proportion of these patients claim that they were never instructed by their physicians to continue taking their medications.22 Some tend to be non-compliant as a result of misunderstanding the instruction given by their physicians.23 Another important aspect of patients’ compliance is that of follow-up, where the lack of proper communication with patients tends to interfere with adherence to follow-up appointments and consequently long-term care.24,25 Again, like diabetes mellitus, hypertension is surrounded by numerous misconceptions about its presentation, natural history and prognosis. This will persist until corrected by good doctor-patient communication.
Commonly encountered in the health care service is a rather sensitive situation in which patients or their relatives are oriented about the diagnosis and prognosis of serious diseases such as cancer. The patients’ and their relatives’ suffering can be either markedly increased or avoided, by poor or good doctor-patient communication.26–28 In a conservative Islamic society such as obtains in Saudi Arabia, considerable effort should be made to ensure confidentiality and sensitivity to patients’ feelings as well as those of their relatives’ during communication between the doctor and the patient.
Even in everyday practice, some explanation needs to be given to patients on why certain investigations or procedures have been requested. Without proper or adequate explanation to the patient, these investigative procedures might be of little benefit to the patient or even result in considerable dissatisfaction.29,30 It has been shown that patient dissatisfaction with health care given to them is related in most cases to the problem of poor doctor-patient communication.31 Indeed, the commonly used term ‘the difficult patient’ may be a product of inadequate communication between doctor and patient.32 Doctor-patient communication is complex and multi-faceted. Patients usually come to the physician with specific ideas in mind, but the doctor tends to concentrate on therapeutic issues only.33 This may result in a break-down of communication. For example, often during the consultation, patients give cues on their personal life, or their feelings, but some physicians fail to pick up these cues.34 In most cases of dissatisfaction with health care, patients’ complaints are the result of communication problems rather than the quality of technical intervention offered.35
The problem of doctor-patient communication is more evident in Saudi Arabia for the following reasons: Firstly, the number of foreign personnel in health services is rather large.36 This workforce communicates with patients and with one another in a variety of languages different from the local one. In addition, not much orientation is given to them on local traditions and the prevalent health-related beliefs and culture. Secondly, this manpower deals with a sizable sector of consumers, who are themselves expatriate and speak a variety of languages, and hold health related traditions and beliefs. This situation naturally creates a complex environment for doctor-patient commun-ication. A recent study from Riyadh37 alluded to the relationship between patient satisfaction and doctor-patient commun-ication. As in other parts of the world, people in Saudi Arabia are expected to attempt to find out and understand all aspects of their health problems.38 Hence the need to train and orientate physicians in the skills related to doctor-patient commun-ication assumes greater significance. In this regard, several methods of training, especially for the situation of Saudi Arabia, can be employed.39,40
In the present era of evidence-based medicine, good doctor-patient commun-ication becomes even more important.41 A blend of evidence-based practice which has the advantages of improving patients outcome and control of the cost of health care together with the patient oriented approach with the humanistic approach to patient care,42 would certainly be an asset to the health care consumer.
In Saudi Arabia, the acquisition of the skill of doctor-patient communication hardly exists in any undergraduate or postgraduate medical curriculum. There is also paucity of research in this area. Consequently, it is vital that comprehensive research be done to clarify the needs of students and professionals, and outline the objectives and the modalities of training in this skill.
The teaching of communication skills should be included in medical school curricula. Moreover, an awareness of the importance of good doctor-patient commun-ication can be developed among medical students by the early introduction of patient contact perhaps from the first year in medical school.43 The content of the curriculum for doctor-patient communication should include an orientation on medical humanities, to help broaden the students’ scientific perspective, and improve their awareness of social traditions. This would prepare them for a world characterized by increasing patient need for good doctor-patient communication. The early training of medical students in this skill would also improve their clinical interviewing skills in order to procure objective and reliable histories from their patients. At the same time the medical faculty should be role models for effective interaction and communication with patients. In their clinical training, students should have more exposure, in terms of time and structured training, to primary health care and family practice rather than the busy teaching hospital setting in order to give them a better environment for effective patient interaction.
At the practicing physician level, much work has to be undertaken, through continuous medical education, to update physicians on the principles of patient-oriented evidence that matters (POEM). There should be seminars and workshops on the principles and techniques of good doctor-patient communication for physicians. These should include practical aspects of communication such as the formulation of guidelines on communicating sensitive issues, such as the presentation of information on serious diseases, death and dying, or sexual aspects of health problems. The training in the use of colloquial languages, and orientation in local health traditions and health-related beliefs and misconceptions will be of an enormous benefit towards the achievement of effective communication with patients.
The overwhelming technological advan-ces in diagnostic and therapeutic tools now available to the medical profession may tend to isolate doctors from their patients. The only way to maintain that relationship is through the development, and preservation of the skills of effective doctor-patient communication.
REFERENCES
- 1.Jackson JL, Chamberlin J, Kroenke K. Predictors of patient satisfaction. Soc Sci Med. 2001;52(4):609–20. doi: 10.1016/s0277-9536(00)00164-7. [DOI] [PubMed] [Google Scholar]
- 2.Mckinley RK, Middleton JF. What do patients want from their doctors.? Content analysis of written patient agenda for the consultation. Br J Gen Pract. 1999;49(449):796–800. [PMC free article] [PubMed] [Google Scholar]
- 3.Herbert RJ, Stewart MA. Patient-centeredness in the consultation. 1: A method for measurement. Fam Pract. 1989;6(4):249–53. doi: 10.1093/fampra/6.4.249. [DOI] [PubMed] [Google Scholar]
- 4.Martin E, Russel D, Goodwin S, Chapman R, North M, Sheridan P. Why patients consult and what happens when they do? BMJ. 1991;303(6797):289–92. doi: 10.1136/bmj.303.6797.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Winefield HR, Murrell TG. Speech pattern and satisfaction in diagnosis and perspective stages of general practice consultation. Br J Med Psychol. 1992;64(pt 2):103–15. doi: 10.1111/j.2044-8341.1991.tb01648.x. [DOI] [PubMed] [Google Scholar]
- 6.Brook DW, Gordon C, Meadow H, Cohen MC. Behavioural medicine in medical education: report of a survey. Soc Work Health Care. 2000;31(2):15–29. doi: 10.1300/J010v31n02_03. [DOI] [PubMed] [Google Scholar]
- 7.Daltroy LH. Doctor-patient communication in rhematological disorders. Billiers Clin Rheumatol. 1993;7(2):221–9. doi: 10.1016/s0950-3579(05)80087-1. [DOI] [PubMed] [Google Scholar]
- 8.Stewart, Meridith L, Brown JB, Galajda J. The influence of older patients-physician communication on health and health-related outcome. Clin Geriatr Med. 2000;16(1):25–36. doi: 10.1016/s0749-0690(05)70005-7. [DOI] [PubMed] [Google Scholar]
- 9.Anderson SO, Mattsson B. Features of good consultation in general practice: is the time important? Scand J Prim Health Care. 1994;12(4):227–32. doi: 10.3109/02813439409029245. [DOI] [PubMed] [Google Scholar]
- 10.Roter D, Lipkin M, Korsgaard A. Sex differences in patient's and physician's communication during primary care medical visits. Med Care. 1991;29(11):1083–93. doi: 10.1097/00005650-199111000-00002. [DOI] [PubMed] [Google Scholar]
- 11.Rowland-Morin PA, Caroll JG. Verbal communication skills and patient satisfaction.A study of doctor-patient interview. Eval Health Prof. 1990;13(2):168–85. doi: 10.1177/016327879001300202. [DOI] [PubMed] [Google Scholar]
- 12.Holden P, Serrano AC. Language barriers in paediatric care. Clin Paediatr (Phila) 1989;28(4):193–4. doi: 10.1177/000992288902800408. [DOI] [PubMed] [Google Scholar]
- 13.Banrnsley L, Williams AP, Cockerill R, Turner J. Physician characteristics and the physician-patient relationship.Impact of sex, year of graduation and specialty. Can Fam Physician. 1999;45:935–42. [PMC free article] [PubMed] [Google Scholar]
- 14.Roter Dl, Hall JA. Why physician gender matters in shaping the physician-patient relationship? J Women Health. 1998;7(9):1093–7. doi: 10.1089/jwh.1998.7.1093. [DOI] [PubMed] [Google Scholar]
- 15.Elzubier AG, Al-Amri AA, Al-Haraka EA, Abu-Samara IO. Self-care, self-reliance and knowledge of diabetes among diabetics in Qassim Region, Saudi Arabia. Saudi Med J. 1996;17(5):598–603. [Google Scholar]
- 16.Alleyne SL, Grregg R, Grel K, Cruckshank JK, Morrison EY. Jamaican patients’ understanding of diabetes mellitus. West Indian Med J. 1991;40(2):60–4. [PubMed] [Google Scholar]
- 17.Van den Arned IJ, Stolk RP, Krans HM, Grobbee DE, Schrjvers AJ. Management of type 2 diabetes: a challenge for patient and physician. Patient Educ Couns. 2000;40(2):187–94. doi: 10.1016/s0738-3991(99)00067-1. [DOI] [PubMed] [Google Scholar]
- 18.Freeman J, Loewe R. Barriers to communication about diabetes mellitus. Patients’ and physicians’ different view of the disease. J Fam Pract. 2000;49(6):507–12. [PubMed] [Google Scholar]
- 19.Loewe R, Freeman J. Interpreting diabetes mellitus: differences between patients and providers models of disease and their implication for clinical practice. Cult Med Psychiatry. 2000;24(4):379–401. doi: 10.1023/a:1005611207687. [DOI] [PubMed] [Google Scholar]
- 20.Health education for people with diabetes. Alexandria: Egypt; 1996. Regional Office for the East Mediterranean Region, World Health Organization. [Google Scholar]
- 21.Cochrane GM, Horne R, Chanez P. Compliance in asthma. Respir Med. 1999;93(11):763–9. doi: 10.1016/s0954-6111(99)90260-3. [DOI] [PubMed] [Google Scholar]
- 22.Salim Ak, Elzubier AG. Drug compliance among hypertensive patients in Tabuk, Saudi Arabia. J Hypertens. 1997;15:561–5. doi: 10.1097/00004872-199715050-00013. [DOI] [PubMed] [Google Scholar]
- 23.Britten N, Stevenson FA, Barry CA, Barber N, Bradley CP. Misunderstandings in prescribing decisions in general practice: qualitative study. BMJ. 2000;320(7233):448–84. doi: 10.1136/bmj.320.7233.484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kosoko O, Quigley HA, Vitale S, Enger C, Kerrigan L, Tielsch JM. Risk factors for non-compliance with follow up visits in a resident's eye clinic. Ophthalmology. 1998;105(11):2105–11. doi: 10.1016/S0161-6420(98)91134-4. [DOI] [PubMed] [Google Scholar]
- 25.Leduc N, Tannenhaum TN, Bergman H, Champagne F, Clarfield AM, Kogan S. Compliance of frail elderly with health services prescribed at discharge from an acute geriatric ward. Med Care. 1998;36(6):904–14. doi: 10.1097/00005650-199806000-00013. [DOI] [PubMed] [Google Scholar]
- 26.Skelton JR, Murray J, Hobbs FD. Imprecision in medical communication: study of a doctor talking to patients with serious illness. J R Soc Med. 1999;92(12):620–5. doi: 10.1177/014107689909201204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rogers MS, Todd CJ. The ‘right kind of pain’: talking about symptoms in outpatient oncology consultations. Palliat Med. 2000;14(4):299–307. doi: 10.1191/026921600669288537. [DOI] [PubMed] [Google Scholar]
- 28.Winter JA. Can we talk? Physician-patient communication issues that could jeopardize patient trust in physicians. S D Med. 2000;53(7):273–6. [PubMed] [Google Scholar]
- 29.Younge D, Moreau P, Ezzat A, Gray A. Communicating with cancer patients in Saudi Arabia. Ann N Y Acad Sci. 1997;808:309–16. doi: 10.1111/j.1749-6632.1997.tb48094.x. [DOI] [PubMed] [Google Scholar]
- 30.Slater DN. Are women sufficiently well informed to provide valid consent to the cervical smear test? Cytopathology. 2000;11(3):166–70. doi: 10.1046/j.1365-2303.2000.00248.x. [DOI] [PubMed] [Google Scholar]
- 31.Gorney M. The role of communication in the physician's office. Clin Plast Surg. 1999;49(447):796–800. [PubMed] [Google Scholar]
- 32.Shapiro J, Lie D. Using the literature to help physicians learners understand and manage “difficult patients”. Acad Med. 2000;75(7):765–8. doi: 10.1097/00001888-200007000-00026. [DOI] [PubMed] [Google Scholar]
- 33.Smith S. Dealing with the difficult patient. Postgrad Med J. 1995;71(841):653–7. doi: 10.1136/pgmj.71.841.653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Levinson W, Gorawara-Bjat R, Lamb J. A study of patient clues and physician responses in primary care and surgical settings. JAMA. 2000;284(8):1021–7. doi: 10.1001/jama.284.8.1021. [DOI] [PubMed] [Google Scholar]
- 35.Stewarty M, Brown JB, Boon H, Galajda J, Meridith L, Sangster M. Evidence on patient-doctor communication. Cancer Prev Control. 1999;3(1):25–30. [PubMed] [Google Scholar]
- 36.Annual Health Report. Riyadh: Alhilal House press; 1418H. Ministry of Health. [Google Scholar]
- 37.Weis R, Stuker R. When patients and doctors don’t speak the same language: concepts of interpretation practice. Soz Preventmed. 1999;44(6):257–63. doi: 10.1007/BF01358974. [DOI] [PubMed] [Google Scholar]
- 38.Saeed AA, Mohammed BA, Magzoub ME, Al-Doghaither AH. Satisfaction and correlates of patient's satisfaction with physicians’ services in primary health care centers. Saudi Med J. 2001;22(3):262–7. [PubMed] [Google Scholar]
- 39.Dube CE, O’Donnell JF, Novack DH. Communication skills for preventive intervention. Acad Med. 2000;75(7 suppl):S45–54. doi: 10.1097/00001888-200007001-00007. [DOI] [PubMed] [Google Scholar]
- 40.Hongladarom S, Phaosavasdi S, Tneepanichskul S, Tannirandon Y, Wilde H, Prukspong C. Humanistic learning in medical curriculum. Med Assoc Thai. 2000;83(8):969–74. [PubMed] [Google Scholar]
- 41.Maulhauser L, Berger M. Evidence-based patient information in diabetes. Diabet Med. 2000;17(12):823–9. doi: 10.1046/j.1464-5491.2000.00383.x. [DOI] [PubMed] [Google Scholar]
- 42.Bensing J. Bridging the gap. The separate words of evidence-based medicine and patient centered medicine. Patient Educ Couns. 2000;39(1):17–25. doi: 10.1016/s0738-3991(99)00087-7. [DOI] [PubMed] [Google Scholar]
- 43.Cade J. An evaluation of early patient contact for medical students. Med Educ. 1993;27(3):205–10. doi: 10.1111/j.1365-2923.1993.tb00258.x. [DOI] [PubMed] [Google Scholar]


