Abstract
Objectives:
To assess the prevalence of some dietary misconceptions among primary health care center-registered diabetic patients in Makka City, Saudi Arabia.
Methods:
A sample of 1039 primary health care center- registered diabetic patients was interviewed using a structured questionnaire on diabetic diet -related misconceptions. A scoring system was used to document the frequency of misconceptions. The relationship of the misconceptions to socio-demographic and diabetes-related variables was assessed using chi-squared tests.
Results:
Most patients (68.7%) had a high diet misconception score. More than half of the sample had the misconception that carbohydrates were to be completely eliminated from the diet, and only dried bread and bitter foods were to be consumed. Data included the belief in the consumption of honey and dates; the omission of snacks; belief in the carcinogenicity of the sugar substitutes; and obesity as a sign of good health. The score was significantly higher among males (p<0.01), patients older than 35 years (p<0.02), and among patients whose level of education was low (p<0.01).
Conclusion:
It is important to note that the rate of diet-related misconceptions among diabetics in Makka city is high. The study pointed to the target fraction of diabetic patients among whom these misconceptions prevailed. There is a need for constant motivation and appropriate education at frequent intervals to encourage better knowledge of the disease so that there is compliance to treatment.
Keywords: Misconceptions, diabetes, diet, Saudi Arabia
INTRODUCTION
Diabetes mellitus is rapidly becoming a common condition with complications. Consequently the cost for its care is escalating. Dietary management is essential to the management of diabetes mellitus. Therefore, patients’ education about diet remains an essential part of this management.1 For various reasons, diabetic patients often do not comply with the dietary recommendations.2–4 This problem is aggravated by the common misconceptions held by different groups of people about diabetic dietary management.5 It is now recognized that patients’ education on a healthy diet and exercise is a method for the prevention of diabetes mellitus.6 Hence it is important to assess the common misconceptions among diabetic patients about diet in order to plan a good health education program. The objective of this study was to assess the prevalence of some dietary misconceptions among primary health care center-registered diabetic patients in Makka City, Saudi Arabia.
MATERIAL AND METHODS
This cross-sectional study was carried out in Holy Makka city during the year 2000. The study population was the primary health care-registered adult diabetic subjects. A sample size of 1039 patients which represented 10% of all diabetic subjects who were registered in PHCCs (Primary Health Care Centers) in Makka city was selected. This was done by means of a two-stage, stratified, random sampling technique with proportional allocation to choose about 10% of diabetic patients, from 9(70%) urban and 12(30%) rural PHCCs. At the first stage, simple random sampling technique was used to choose 9 urban and 12 rural PHCCs. At the second stage the sample of diabetic subjects from each chosen PHCC was also taken, using simple random sample.
Data were collected with a structured questionnaire which was administered to patients by pre-trained primary health care center physicians. The questionnaire included demographic information such as gender, age and nationality. Educational level was categorized as low = elementary school or below, average = high school or below, and high= university or above. It also included diabetes-related information such as family history, duration of diabetes, body mass index (calculated as the weight in kilograms divided by the square of the height in meters), continuity of care as measured by whether the patient was always seen in the same or different centers, regularity of follow up and the number of primary health care center visits made per year. Patients’ recall of compliance with diet was also recorded.
Patients were asked specifically about their belief in eight misconceptions about dietary aspects in diabetes. Those misconceptions were about the consumption of carbohydrates, bitter foods, dry bread, intake of snacks, honey and dates, the use of sugar substitutes and their opinion about obesity. The patient's responses on these aspects were scored as “1” or “0” if he/she had a misconception, or not, respectively. The sum of all scores was computed to represent a misconception score. A cut-off point of 30% chosen on the basis of the median score was used to categorize scores whereby a score equal to or less than 30% was considered low while that above 30% was considered high. This cut-off point was chosen after taking the average opinions of some experts in the field.
Data was entered and analyzed by means of an IBM-compatible computer incorporating the Statistical Package for Social Science SPSS PC Version 10. Frequency distributions were generated and a chi-squared test was used to assess the significance of difference between categories. A p-value of 0.05 or less was considered indicative of statistical significance.
RESULTS
The total number of patients in the sample was 1039. Saudi diabetic patients formed the majority (93.7 %) compared to a small number of non-Saudis (6.3%). Males constituted (66.7 %), while females constituted (33.3 %) of the sample. The mean patient age was 54.6 ± 12.6 years. Most of the patients had a low level of education (74 %) and the majority of them (71.9%) had had diabetes for more than 5 years. Also, most of them (73.2%) had a high body mass index (higher than 25 kg/square meters). Patients who were followed up in the same center and those who stated that they were regular in their follow up were 89.0% and 83.9%, respectively. Most patients (69.8%) visited the health center more than 6 times per year. Patients who stated that they were compliant with the prescribed diet were 28.5%.
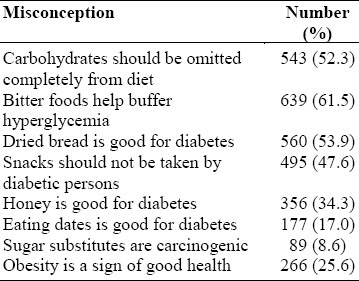
About half of the sample had the misconception that carbohydrates were to be completely removed from the diet; bitter food items were to be consumed to neutralize hyperglycemia; that dried bread was good for diabetes; that snacks were to be avoided by diabetic patients. Other misconceptions held were that honey and dates were good food items for diabetic patients (34.3% and 17.0%, respectively). Less than 10% of the patients thought that sugar substitutes could be carcinogenic, while a quarter of them thought that obesity was a sign of good health Table1.
Table 1.
Misconceptions of diet shown by 1039 diabetic patients in Makka city during the year 2000
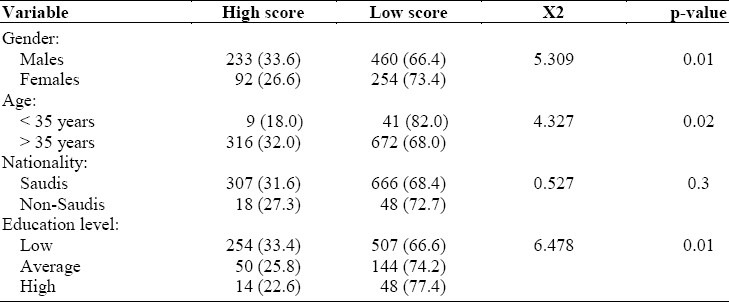
Most patients (68.7%) had a high diet misconception score. The score was significantly higher among males than females (P < 0.01), among patients older than 35 years (P < 0.02), and among patients who had a low level of education (p<0.01) (Table 2).
Table 2.
Effect of demographic variables on diet misconception score by 1039 diabetic patients in Makka city during the year 2000
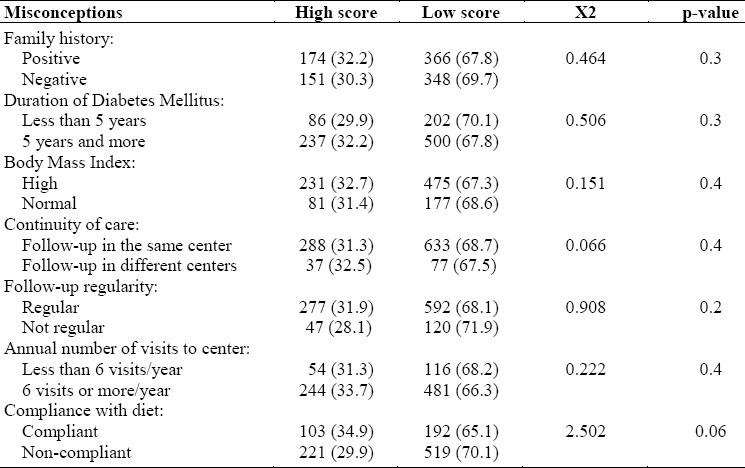
Variations of the misconception score regarding family history, duration of diabetes, body mass index, continuity of care, regularity of follow up, number of visits per annum to the health center, and with compliance to diet were not statistically significant (Table 3).
Table 3.
Effect of diabetes-related variables on diet misconception score by 1039 diabetic patients in Makka city during the year 2000
DISCUSSION
The subjects of this study sample were patients who were mostly past middle age, afflicted with type 2 diabetes, mostly males and with not much education. Moreover, most of them were overweight or obese, with poorly controlled diabetes; and held many misconceptions about diabetes. They therefore, represented a target group for the proper management of diabetes mellitus, especially in respect of health education, because of the possible morbidity and mortality risk factors they were exposed to.
The theme of health education needed in the light of the study findings, should be dietary management considering that 25.6% of the sample believed that obesity was a sign of good health, contrary to all basic information on the hazards of obesity and overweight.7 It is vital to use behavior-modifying education,8,9 to help them get rid of this misconception and correct the status of their risk factors. However, such efficacy of this education might be diminished if not carried out with the proper educator-patient communication.10
The study also revealed some misconceptions related to the types of food eaten by diabetic subjects. A sizable proportion of the sample believed that carbohydrates should be omitted from their diet. This is a genuine misconception since carbohydrates are now known to be an essential component of diabetic diet, for 40–60 % of the diet content should be in that form to maintain adequate energy, and as far as possible, an ideal body weight. However, it is important to educate patients on how to count carbohydrates, a process that was tried successfully on a sample of patients in a recent study.12 Patients also expressed a preference for bitter foods, in the false hope that these would neutralize hyperglycemia. Of course, this is absolutely unfounded, and needs correction with the appropriate health education. Another important misconception expressed by the sample was their ignorance of the benefits of snacks in meal planning for diabetic patients. It has been shown that snacks are associated with better glucose tolerance and physical as well as psychological functioning.12 It is, therefore, necessary to correct this misconception among diabetic patients. The study also revealed a preference for honey and to a lesser extent dates. This arises out of religion and culture since honey and dates are local products. These two items might not interfere with diabetes control as along as they were taken in moderation as part of their carbohydrate intake. Therefore, patients need to be educated on this. This study revealed the patients’ poor basic knowledge of the fundamentals of treating diabetes, although 72% of them had had the disease for more than five years. The consequences of these misconceptions may be fatal, or at least may have a negative effect on patients’ compliance and control.13,14 In Saudi Arabia, this situation may be related to deficiencies in the structures and the process of the health education programs directed at diabetic patients, for only 33% of diabetic patients were found to have adequate health education.15 Barriers to effective health education may include such factors as low educational level,16 inaccurate culture-bound beliefs,13 time required for patient education,17 the educator's poor knowledge of the disease;18,19 and language16,17 or cultural barriers.17 Studies have shown that the impact of effective health education and behavioral intervention reflect on the patients’ compliance, metabolic control and knowledge about the management of the disease.20,21 The outpatient visit for diabetes mellitus should be different from other chronic and acute diseases as more time should be invested in patients’ education.22,23 The dietary management of diabetic patients has evolved from the concepts of ‘simple’ and ‘complex’ carbohydrates to that of the glycemic index, and eventually to the hypocaloric diet and carbohydrates counting. Physicians should translate these developments into practical instructions for patients and correct patients’ misconceptions through well-organized health education.
The main variables that were revealed as significantly related to the diet misconception score in this study were male gender, older age and low education. This finding identifies the population of diabetic patients at whom health education should be targeted in order to help them control this serious disease effectively.
In this study, dietary-related misconceptions were significantly higher among males which could be explained by the variation in age, as more females were younger and better educated. However, studies have shown that knowledge is not influenced by the gender of the patient when the difference in the level of education of both genders is not significant.24 Our results support earlier findings that correct knowledge of the disease is associated with younger age groups.24 The rate of misconceptions found in this study appears to be universal to all strata of the diabetic community of the study sample, with insignificant differences among Saudi nationals and non-Saudis. Similar to our findings, studies have shown that the higher the level of education of the patient, the better the knowledge about diabetes.16 Others have, however, found that non-adherence to treatment is greater among this group of patients.25 The association between positive family history of diabetes and higher rate of misconceptions in this study, supports an earlier finding that the characteristics of the family determine the self-care practices.26 Similar to our findings, studies have shown that the rate of the misconception is not associated with the duration of the disease.24 Results of this study suggest that misconception scores are not affected by the number of visits to the health center per year, continuity, or regularity of care. Results reported from Saudi Arabia have shown that compliance to appointments in primary health care centers by diabetics is good in 60% and poor in 30%. Only 33% of diabetic patients had adequate health education; 27% of the patients had not had any at all.10 Elsewhere, compliance with appointment was found to be associated with good care score.13,14,20,21 It was surprising to find that the sample compliance with diet was only 28.5%. This may explain why 73.2% of the sample had high body mass index. This finding stresses the importance of compliance to diet in addition to drugs to attain a good diabetic control.2
In conclusion, the results of this study revealed rather importantly, that there was a high rate of diet-related misconceptions among diabetics in Makka city. The study identified the target fraction of diabetic patients among whom such misconceptions prevailed. It is necessary to constantly motivate and give appropriate education at frequent intervals to promote better knowledge about the disease and consequent compliance to treatment.
REFERENCES
- 1.Parkin T. An audit of the theoretical basis of education during dietetic consultations with diabetic subjects. J Hum Nutr Diet. 2001;14(1):33–42. doi: 10.1046/j.1365-277x.2001.00269.x. [DOI] [PubMed] [Google Scholar]
- 2.Khattab MS, Abolfotouh MA, Khan MY, Humaidi MA, Al-Kaldi YM. Compliance and control of diabetes in a family practice setting, Saudi Arabia. East Mediterranean Health Journal. 1999;5(4):755–65. [PubMed] [Google Scholar]
- 3.Zilli F, Croci M, Tufano A, Caviepzel F. The compliance of hypocaloric diet in type 2 diabetic obese patients: a brief-term study. Eat I Weight Disord. 2000;5(4):217–22. doi: 10.1007/BF03354449. [DOI] [PubMed] [Google Scholar]
- 4.Bernal H, Woolley S, Schensul JJ, Dickinson JK. Correlates of self-efficacy in diabetes self-care among Hispanic adults with diabetes. Diabetes Educ. 2000;26(4):673–80. doi: 10.1177/014572170002600415. [DOI] [PubMed] [Google Scholar]
- 5.Fisher EB, Walker EA, Bostrom A, Fischhoff B, Haire-Joshu D, Johnson SB. Behavioral Science Research in the Prevention of Diabetes: Status and Opportunities. Diabetes Care. 2002;25(3):599–606. doi: 10.2337/diacare.25.3.599. [DOI] [PubMed] [Google Scholar]
- 6.Kao PC, Wu TJ, Ho LL, Li XJ. Current trends and new approaches in the management of diabetes mellitus. Ann Clin Lab Sci. 2000;30(4):339–45. [PubMed] [Google Scholar]
- 7.Saw SM, Rajan U. The epidemiology of obesity: a review. Ann Acad Med Singapore. 1997;26(4):489–93. [PubMed] [Google Scholar]
- 8.Cabrera-Piveral CE, Gozalez-Perez G, Vega-Lopez G, et al. Effects of behavior-modifying education in the metabolic profile of the type 2 diabetes mellitus patients. J Diabetes Complications. 2000;14(6):322–6. doi: 10.1016/s1056-8727(00)00077-5. [DOI] [PubMed] [Google Scholar]
- 9.Schalch A, Ybarra J, Adler D, Deletraz M, Lehmann T, Golay A. Evaluation of a psycho-educational nutritional peogram in diabetic patients. Patient Educ Couns. 2001;44(2):171–8. doi: 10.1016/s0738-3991(00)00188-9. [DOI] [PubMed] [Google Scholar]
- 10.Shultz JA, Sprague MA, Branen LJ, Lambeth S. A comparison of views of individuals with type 2 diabetes mellitus and diabetes educators about barriers to diet and exercise. J Health Commun. 2001;6(2):99–115. doi: 10.1080/108107301750254457. [DOI] [PubMed] [Google Scholar]
- 11.Bruttomesso D, Piñata A, Crazzolara D, et al. Teaching and training programme on carbohydrates counting in Type 1 diabetic patients. Diabetes Nutr Metab. 2001;14(5):259–67. [PubMed] [Google Scholar]
- 12.Benton D, Slater O, Donohoe RT. The influence of breakfast and a snack on psychological functioning. Physiol Behav. 2001;74(4):559–71. doi: 10.1016/s0031-9384(01)00601-1. [DOI] [PubMed] [Google Scholar]
- 13.Philis TA, Walker C. Improved care for diabetes in underserved populations. J Ambulatory Care Manage. 2001;24:39–43. doi: 10.1097/00004479-200101000-00005. [DOI] [PubMed] [Google Scholar]
- 14.Duran VB, Rivera CB, Franco GE. Pharmacological therapy compliance in diabetes. Salud Publica Mex. 2001;43:233–6. [PubMed] [Google Scholar]
- 15.Al-Khaldi YM, Khan MY. Audit of a diabetic health education program at a large primary health care center in Asir region. Saudi Med J. 2000;21:838–42. [PubMed] [Google Scholar]
- 16.Larsen IF. Diabetes among immigrants from non-western countries. Tidsskr Nor Laegeforen. 2000;120:2804–6. [PubMed] [Google Scholar]
- 17.Chin MH, Cook S, Jin L, Drum ML, Harisson JF, Koppert J, et al. Barriers to providing diabetes care in community health centers. Diabetes Care. 2001;24:268–74. doi: 10.2337/diacare.24.2.268. [DOI] [PubMed] [Google Scholar]
- 18.Speight J, Bradley C. The ADKnowl : identifying knowledge deficits in the diabetes care. Diabet Med. 2001;8:626–33. doi: 10.1046/j.1464-5491.2001.00537.x. [DOI] [PubMed] [Google Scholar]
- 19.Muhlhauser I, Berger M. Evidence-based patient information in diabetes. Diabet Med. 2000;7:823–9. doi: 10.1046/j.1464-5491.2000.00383.x. [DOI] [PubMed] [Google Scholar]
- 20.Gagliardino JJ, Etchegoyen G, Pendid LA Research Group. A model educational program for people with type 2 diabetes: a cooperation Latin American implementation study (PENDID-LA) Diabetes Care. 2001;24:1001–7. doi: 10.2337/diacare.24.6.1001. [DOI] [PubMed] [Google Scholar]
- 21.Matam P, Kumaraiah V, Munichoodappa C, Kumar KM, Aravind S. Behavioural intervention in the management of compliance in young type-1 diabetics. J Assoc Physicians India. 2000;48:967–71. [PubMed] [Google Scholar]
- 22.Yawn B, Zyzanski SJ, Goodwin MA, Golter RS, Stange KC. Is diabetes treated as an acute or chronic illness in community family practice? Diabetes Care. 2001;24:1390–6. doi: 10.2337/diacare.24.8.1390. [DOI] [PubMed] [Google Scholar]
- 23.Bamgboye EA, Jarallah JS. Long-waiting outpatients : target audience for health education. Patient Educ Couns. 1994;23:49–54. doi: 10.1016/s0738-3991(05)80021-7. [DOI] [PubMed] [Google Scholar]
- 24.Ford S, Mai F, Manson A, Rukin N, Dunne F. Diabetes knowledge-are patients getting the message? Int J Clin Pract. 2000;54:535–6. [PubMed] [Google Scholar]
- 25.Shobhana R, Begum R, Snehalatha C, Vitjay V, Ramachandran A. Patients’ adherence to diabetes treatment. J Assoc Physicians India. 1999;47:1173–5. [PubMed] [Google Scholar]
- 26.Fisher L, Chesla CA, Skaff MM, et al. The family and disease management in Hispanic and Europian-American patients with type 2 diabetes. Diabetes Care. 2000;23:267–72. doi: 10.2337/diacare.23.3.267. [DOI] [PubMed] [Google Scholar]


