Abstract
To investigate the feasibility of image-based intracavitary brachytherapy (IBICBT) for uterine cervical cancer, we evaluated the dose–volume histograms (DVHs) for the tumor and organs at risk (OARs) and compared results from the IBICBT plan and the standard Manchester system (Manchester plan) in eight patients as a simulation experiment. We performed magnetic resonance imaging (MRI) and computed tomography (CT) following MRI-adapted applicator insertion, then superimposed MR images on the planning CT images to describe the contours of high-risk clinical target volume (HR CTV) and OARs. The median volume of HR CTV was 29 cm3 (range, 21–61 cm3). Median D90 (HR CTV) and V100 (HR CTV) were 116.1% prescribed doses (PD) (90.0–150.8%) and 96.7% (84.2–100%), respectively, for the Manchester plan. In comparison, we confirmed that the median D90 (HR CTV) was 100% PD in the IBICBT plan for all patients. Mean D2cc (bladder) was 101.8% PD for the Manchester plan and 83.2% PD for the IBICBT plan. Mean D2cc (rectum) was 80.1% PD for the Manchester plan and 64.2% PD for the IBICBT plan. Mean D2cc (sigmoid) was 75% PD for the Manchester plan and 57.5% PD for the IBICBT plan. One patient with a large tumor (HR CTV, 61 cm3) showed lower D90 (HR CTV) with the Manchester plan than with the IBICBT plan. The Manchester plan may represent overtreatment for small tumors but insufficient dose distribution for larger tumors. The IBICBT plan could reduce OAR dosage while maintaining adequate tumor coverage.
Key words: Image-based intracavitary brachytherapy, MRI-adapted applicator, uterine cervical cancer, dose–volume histogram
INTRODUCTION
Intracavitary brachytherapy (ICBT) for cervical cancer is a useful modality that can deliver high dosage to the primary tumor without delivering excessive dosage to the surrounding normal tissue. Thus, the combination of external beam radiation therapy (EBRT) and ICBT is a standard treatment for cervical cancer.
However, local recurrence is still a problem in locally advanced disease and one of the strategies to obtain better local control is a technology development to attain improvement of dose distribution [1]. The dose prescription for point A (the Manchester plan) calculated from orthogonal films is commonly used for intracavitary brachytherapy, while three-dimensional (3D) treatment planning is not popular in Japan, although 3D treatment planning is routinely used for EBRT.
Western countries recently began 3D image-based treatment planning (the IBICBT plan) by computed tomography (CT) or magnetic resonance imaging (MRI) for ICBT, and published guidelines for the definition of contours and the assessment of dosage by 3D IBICBT [2–4]. It was demonstrated that 3D dose calculation and analysis of dose–volume histograms (DVHs) are required for assessment of the precise dose required for the tumor and organs at risk (OARs).
In May 2009, we began performing MRI and CT after the insertion of an MRI-adapted applicator, and superimposed MR images on the planning CT images to define the contours of high-risk clinical target volume (HR CTV) and OARs at the National Hospital Organization Osaka National Hospital (ONH) and Kyoto City Hospital (KCH). These two institutes discussed a study design, and we started a trial of MRI-based treatment planning as a preliminary step toward the IBICBT plan. In this preliminary study, we used the conventional standard Manchester plan for the actual treatment. As a simulation experiment, we aimed to adopt the IBICBT plan to facilitate better tumor coverage and to reduce OAR dosage and then compared the DVH results of both treatment planning methods.
MATERIALS AND METHODS
Between May 2009 and November 2010, eight uterine cervical cancer patients (median age, 61 years; range, 37–88 years) were treated by ICBT at the Department of Radiology and Radiation oncology, ONH (Table 1). Histological findings showed seven squamous cell carcinomas and one adenocarcinoma. Using the 2002 Union for International Cancer Control (UICC) classification, two cases of T1b, one of T2a, four of T2b and one of T3b were identified. All patients received EBRT to the whole pelvis at the median prescribed dose (PD) of 25 Gy (range, 19.8–40.0 Gy). In addition, all but one patient underwent center-shielded EBRT (median, 23 Gy; range, 0–30 Gy), and additional boost irradiation to pelvic lymph node metastasis was performed for three patients. In principle, we performed ICBT after whole pelvic EBRT.
Table 1.
Patient characteristics
| Patient No. | Volume of HR CTV* (cc) | Age | Histology | T-stage | N-stage | M-stage | Fraction dose of brachytherapy |
|---|---|---|---|---|---|---|---|
| 1 | 21 | 40 | SCC† | 2b | 0 | 0 | 6.5 |
| 2 | 23 | 81 | SCC | 1b1 | 0 | 0 | 6.5 |
| 3 | 28 | 86 | SCC | 2a | 0 | 0 | 7.5 |
| 4 | 29 | 56 | SCC | 2b | 1 | 1 | 6 |
| 5 | 29 | 88 | SCC | 2b | 0 | 0 | 6.5 |
| 6 | 33 | 37 | SCC | 1b1 | 0 | 1 | 7.5 |
| 7 | 44 | 52 | SCC | 2b | 1 | 0 | 6.5 |
| 8 | 61 | 66 | Ad‡ | 3b | 1 | 0 | 6 |
*HR CTV: high risk clinical target volume
† SCC: squamous cell carcinoma
‡ Ad: adenocarcinoma
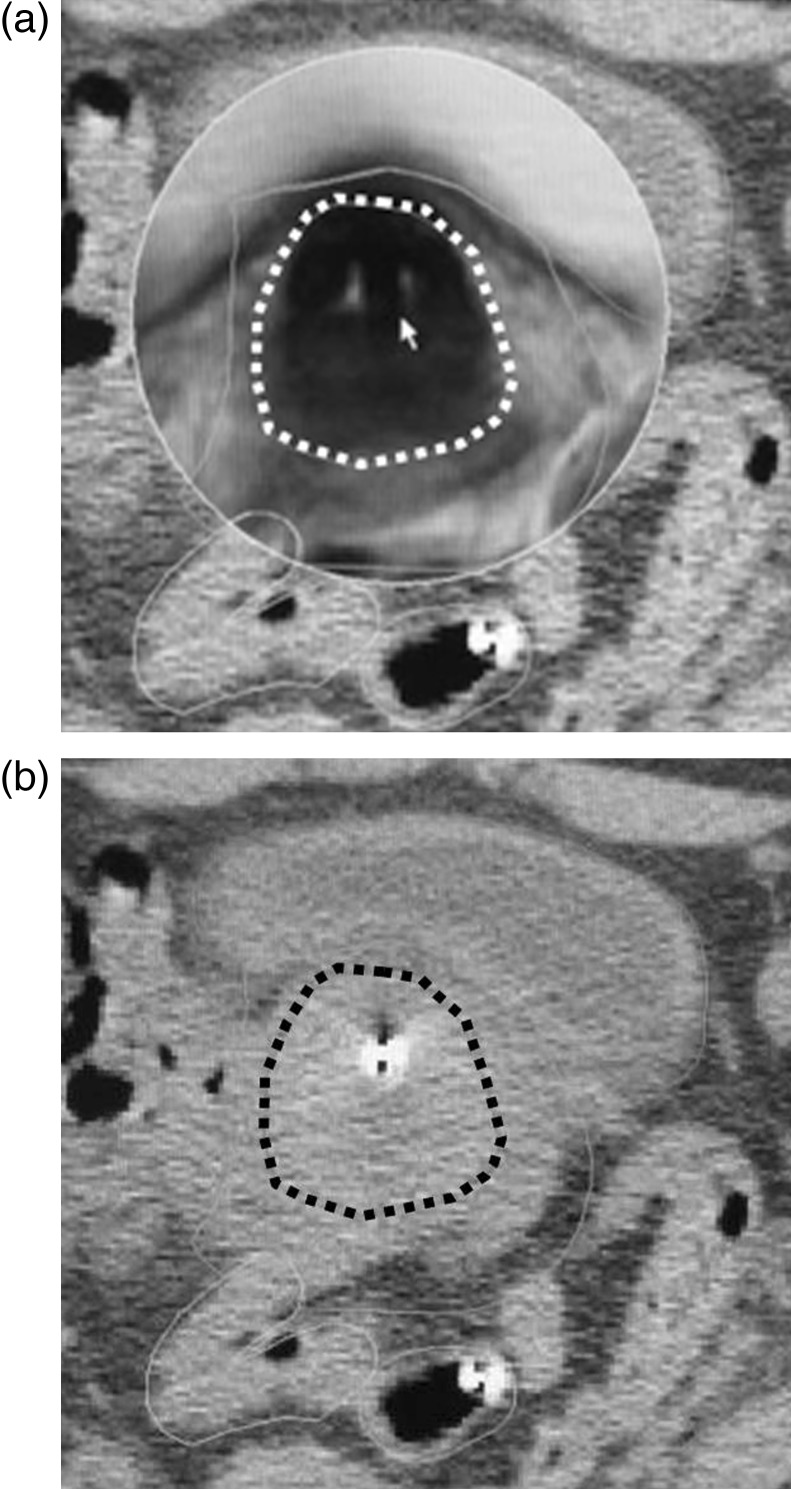
We inserted an MRI-adapted applicator (Standard CT-MR Applicator®, Nucletron, Veenendaal, the Netherlands) for all patients and performed MRI and CT immediately (Fig. 1a, b). CT scans were obtained with a section thickness of 3 mm. MRI scans were obtained with a section thickness of 2.7 mm and gap of 0.3 mm. In principle, this applicator was used at the initial brachytherapy session. At first, CT-based planning was performed according to the standard Manchester plan (Manchester plan) and treatment administered accordingly. Treatment planning was formulated by Plato® and Oncentra® Brachy (Nucletron). We used microSelectron-HDR® (Nucletron) with an 192Ir source. The median single PD was 6.5 Gy (range, 6.0–7.5 Gy) and the median total PD was 25.1 Gy (range, 18–27 Gy).
Fig. 1.
(a) computed tomography (CT) image of Patient 1 after insertion of treatment applicator and (b) same CT image as Fig. 1a without superimposition of MRI. (a) A magnetic resonance image (MRI) was superimposed to describe the precise contours of high-risk clinical target volume (HR CTV, white broken line). (b) It was difficult to describe the high-risk clinical target volume (HR CTV) as shown in Fig. 1a. The HR CTV described by CT imaging appears to be of larger volume than that described by MRI (black broken line).
Following treatment, we followed the IBICBT plan. We superimposed axial T2-weighted MR images on the planning CT images to define the contours of the HR CTV and OARs (bladder, rectum and sigmoid colon) (Fig. 1b). The definition of these contours was based on the recommendations of the Gynecological GEC-ESTRO Working Group for reporting 3D-sectional image-assisted brachytherapy of cervical cancer [3, 4]. The bladder, rectum and sigmoid colon were delineated as hollow organs (not organ wall only). DVH analysis was performed according to the recommendations of the Gynecological GEC-ESTRO Working Group. HR CTV and the following parameters were reported: CTV percentage covered by the PD (V100) and the dosage that covered 90% and 100% of the CTV (D90 and D100, respectively). For the OARs, we calculated the minimum dose received by the maximally irradiated 2 cm3 volume (D2cc).
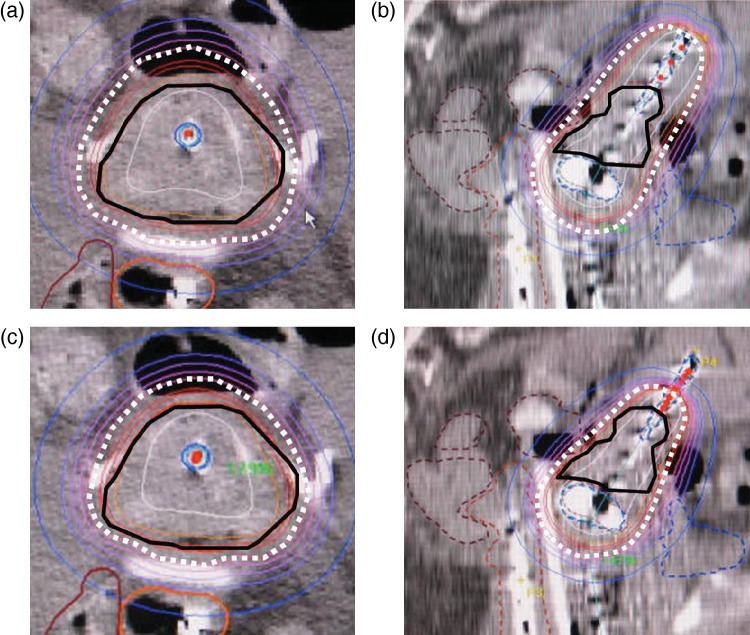
Fig. 2.
(a−d) dose distribution curves of Patient 1. We first followed the Manchester plan (a, axial image; b, sagittal image) and administered treatment to the patient. After treatment, we followed the image-based intracavitary brachytherapy (IBICBT) plan (c, axial image; d, sagittal image). HR CTV (black line) was covered by a higher isodose line than the prescribed isodose line (white broken line) in the Manchester plan (a, b). In contrast, the IBICBT plan showed better coverage of HR CTV (black line) by the prescribed isodose line (white broken line).
The Manchester (Fig. 2a, b) and IBICBT plans (Figure 2c, d) were compared on the basis of percentage of prescribed dose (% PD) for each patient. The minimum interval of dwell position was 2.5 mm for the IBICBT plan. The plan was followed by graphical optimization and/or manual modification from the Manchester plan. If we wanted to regulate a dose distribution curve by modifying dwelling time of one applicator, we used manual modification. If we wanted to regulate the dose distribution curve by modifying dwelling time of all applicators near the area of interest, we used graphical optimization. In most cases, we used manual modification for the cranial side of tandem applicator to modify the dose distribution of the uterine fundus/corpus region and used graphical optimization to modify the dose distribution of the uterine cervical region. We sometimes used graphical optimization as a final fine regulation after manual modification to achieve the goal of the planning. The goals of this planning were as follows: (i) D90 (HR CTV) became the PD, i.e. V100 (HR CTV) became 90% PD. (ii) D2cc (OARs) became smaller than those in the Manchester plan.
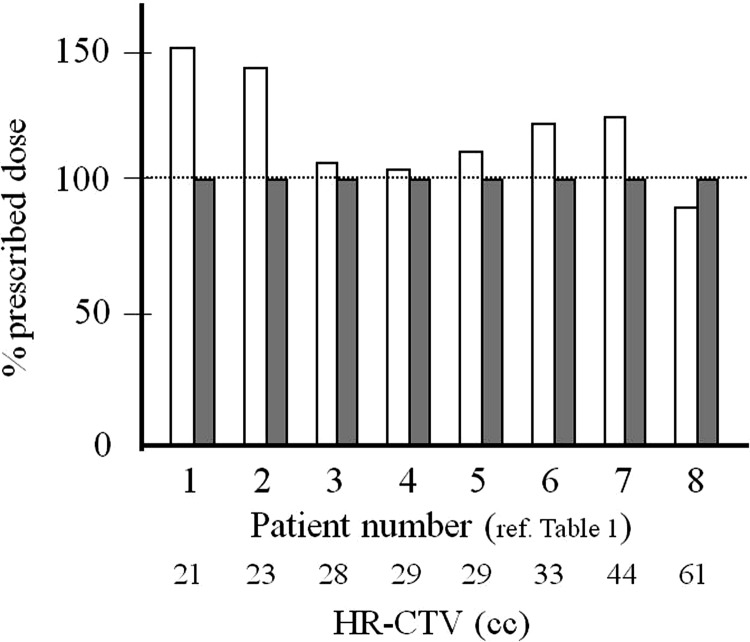
Fig. 3.
Dosages that covered 90% of the HR CTV were compared between the Manchester plan (white columns) and the IBICBT plan (gray columns) for each patient. We could control the D90 (HR CTV) values of all patients to 100% PD. In contrast, median D90 (HR CTV) per fraction was 116.1% PD (90.0–150.8%) for the Manchester plan. Seven of the eight patients showed higher values in the Manchester plan than in the IBICBT plan. However, Patient 8, whose HR CTV was >61 ml, showed a lower value.
We changed the isodose line to improve the coverage of HR CTV and recalculated to achieve (i). After recalculation, the planning stage was considered complete if we could achieve (ii). If not, we re-performed graphical optimization and/or manual modification.
Statistical analyses were performed using the StatView v5.0 software program. Student's t-test was used for normally distributed data. Statistical significance was assigned at the P < 0.05 level.
RESULTS
The median volume of HR CTV was 29 cm3 (range, 21–61 cm3). For the Manchester plan, the median D90, D100 (HR CTV) and V100 (HR CTV) values per fraction were 116.1% PD (90.0–150.8%), 80.1% PD (50.0–107.7%) and 96.7% (84.2–100%), respectively (Fig. 3). For the IBICBT plan, the median D90, D100 (HR CTV), and V100 (HR CTV) was 100% PD (100%–100%), 67.3% PD (57.3%–73.8%), and 90% (90%–90%), respectively.
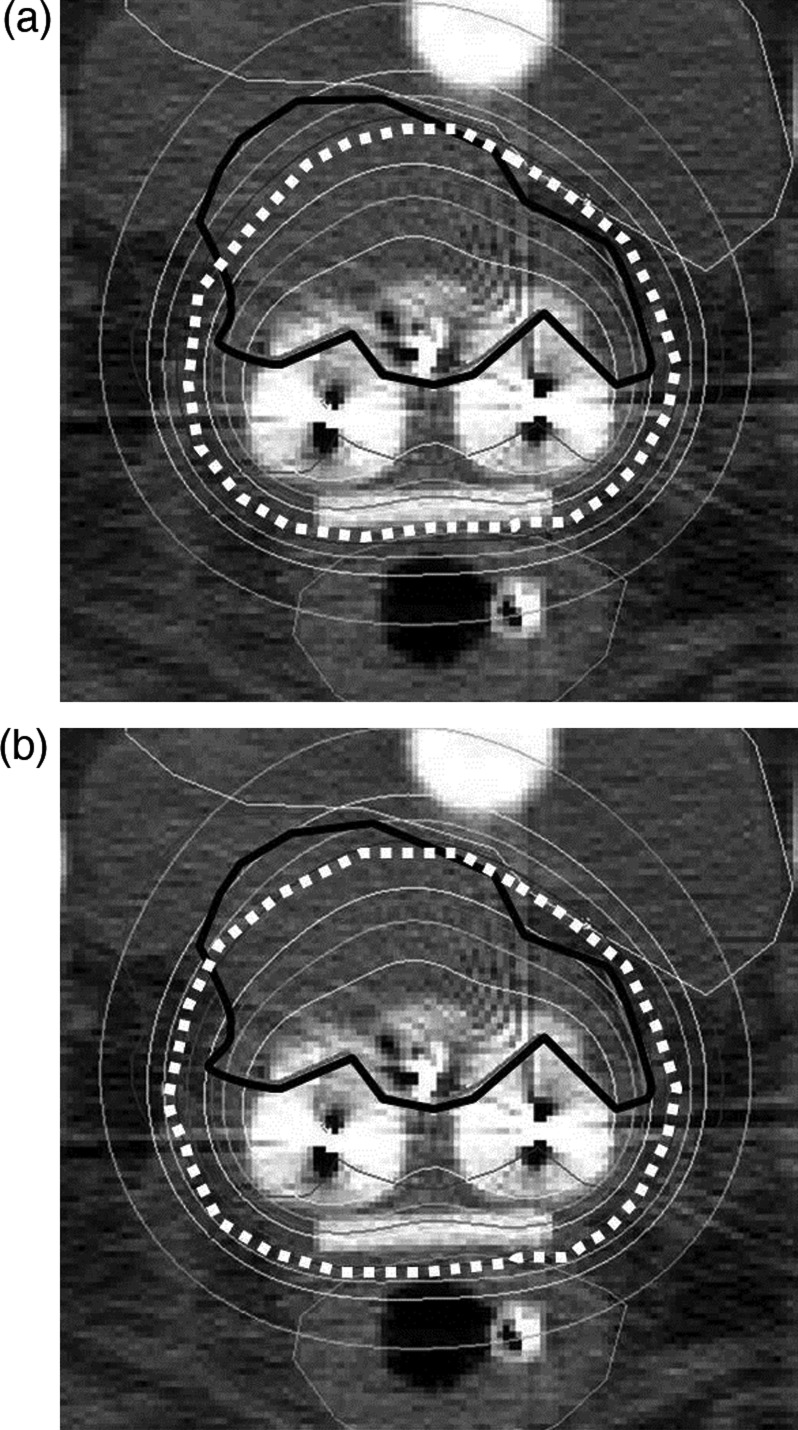
Fig. 4.
(a, b) dose distribution curves of Patient 8. We first followed the Manchester plan (a) and administered treatment to the patient. After treatment, we modified the Manchester plan and followed the IBICBT plan (b). HR CTV (black line) could not be covered by the prescribed isodose line (white broken line) in the Manchester plan (a). In the IBICBT plan, we extended the dwell time of the right ovoid applicator and enhanced the right side of HR CTV (white broken line). However, we compromised at this point to maintain the maximally irradiated 2 cm3 volume for the bladder within tolerable levels.
In D90 (HR CTV), seven of eight patients showed higher values in the Manchester plan than in the IBICBT plan. Patients 1 and 2 (Table 1) showed more than 140% PD in the Manchester plan (Fig. 3). In contrast, only Patient 8 (HR CTV = 61 cm3) showed a lower value (90% PD) in the Manchester plan (Figs 3 and 4a, b) than in the IBICBT plan, which implies that the Manchester plan generates insufficient coverage in larger tumors. We were able to control the D90 (HR CTV) values of all patients to 100% PD.
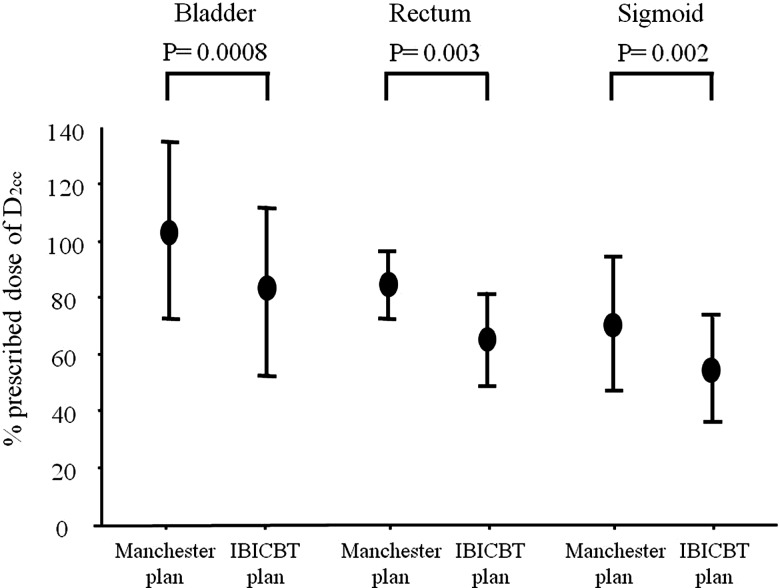
Fig. 5.
Percentage of prescribed doses for organs at risk were compared between the Manchester and IBICBT plans. Shown here are average values with standard deviation for the minimum dose received by the maximally irradiated 2 cm3 volume (D2cc) for bladder, rectum and sigmoid colon. Significant differences were observed between the two plans for bladder (P = 0.0008), rectum (P = 0.003) and sigmoid colon (P = 0.002).
In D100 (HR CTV), a similar tendency was observed. Values for six of the eight patients were higher in the Manchester plan than in the IBICBT plan. Patient 1 showed > 100% PD in the Manchester plan. Patients 3 and 8, whose HR CTV values were 28 and 61 ml, respectively, showed lower values in the Manchester plan. Stability of D100 (HR CTV) values was maintained in the IBICBT plan.
Mean D2cc (bladder) was 101.8% PD (range, 68.3–157.3%) in the Manchester plan and 83.2% PD (range, 46.2–141.3%) in the IBICBT plan. D2cc (bladder) values were lower in the IBICBT plan in all patients. IBICBT achieved significantly lower D2cc (bladder) (P = 0.0008) (Fig. 5).
Mean D2cc (rectum) was 80.1% PD (range, 72.0–106.2%) in the Manchester plan and 64.2% PD (range, 36.9–84.0%) in the IBICBT plan. D2cc (rectum) values were lower in the IBICBT plan for all patients. A significant difference was observed between the two plans (P = 0.003) (Fig. 5).
Mean D2cc (sigmoid) was 75% PD (range, 26.2–98.7%) in the Manchester plan and 57.5% PD (range, 13.8–73.3%) in the IBICBT plan. D2cc (sigmoid) values were significantly lower in the IBICBT plan for all patients (P = 0.002) (Fig. 5).
DISCUSSION
The Manchester plan is a very simple method and has sufficient reproducibility for worldwide use. However, it contains a potentially serious problem with regard to dose distribution, because this applies to HR CTV only when the edge of the HR CTV is located close to point A. If the tumor is larger than this ideal size, tumor coverage is reduced and a marginal low-dose area is created, resulting in local recurrence. Moreover, if the tumor is smaller than the ideal size, the complication of OAR overdose occurs. To resolve these problems, IBICBT was proposed by the gynecological GEC ESTRO working group [3, 4]. However, to date there has been no report comparing DVH results between the Manchester plan and the IBICBT plan using MRI-assisted treatment planning according to recommendations from the GEC ESTRO working group in Japan.
We tried the IBICBT plan in this study and we could accomplish the values of the DVH results as our goal of the planning for all eight patients although their HR CTV had various volumes (range, 21–61 cm3). With the IBICBT plan, the D90 values of all patients became 100% PD without increasing the dose to OARs. The mean D2cc (bladder) reduced from 101.8% PD for the Manchester plan to 83.2% PD for the IBICBT plan. The mean D2cc (rectum) reduced from 80.1% PD for the Manchester plan to 64.2% PD for the IBICBT plan. The mean D2cc (sigmoid) reduced from 75% PD for the Manchester plan to 57.5% PD for the IBICBT plan. We could reduce D2cc by about 20% for all these OARs.
Graphical optimization and/or manual modification from the Manchester plan were useful. This result showed that the IBICBT plan could deliver stable treatment doses for various sizes of tumor, although the Manchester plan showed lower coverage for large tumors and higher coverage for small tumors.
For larger tumors, interstitial brachytherapy (ISBT) is also recommended [5–9]. ISBT is a useful treatment modality because treatment applicators can be implanted in and/or around the CTV, and ISBT has the potential to achieve better tumor coverage regardless of the size of the vaginal and uterine cavity in the case of cervical cancer. The American Brachytherapy Society recommends that ISBT should be used in situations such as bulky lesions, narrow vagina, inability to enter the cervical os, extension to the lateral parametrium or pelvic side wall and lower vaginal extension [5]. Pötter et al. [6] reported their single institute's findings that MR image-based ICBT with or without ISBT was validated and showed better treatment results and fewer complications than previous treatment methods. They compared treatment results between treatment planning with MRI (2001–2003) and without MRI (1998–2000). The 3-year local control rate for tumors larger than 5 cm improved from 71% (1998–2000) to 90% (2001–2003) with MRI-aided treatment planning. However, some patients have high-risk diseases for needle implantation or anesthesia and are not good candidates for ISBT. In such cases, we could not use ISBT and would try to do our best to save the patient's life with ICBT alone. In this study, the D90 (HR CTV) value for larger tumors (61 cm3) could be improved to 100% PD for the IBICBT plan although the Manchester plan showed a lower D90 (HR CTV) value (90% PD). Therefore, we considered that the IBICBT plan should be adopted when it is not possible to perform ISBT for a large tumor.
In smaller tumors, IBICBT is recommended [10, 11]. Because we can shrink the dose distribution curve to fit the smaller tumor, we expect to reduce the likelihood of complications without compromising local tumor control. Zwahlen et al. reported that the average D2cc (bladder, rectum and sigmoid) values were 30, 16 and 26 Gy for the conventional plan and 26, 14 and 19 Gy for the IBICBT plan, respectively, with patients whose HR CTV was less than 16.1 cm3. Such reductions of 12–32% were statistically significant. In the Manchester plan, D90 (HR CTV) values for smaller tumors were excessive compared with the PD. Therefore, the IBICBT plan is useful in reducing the likelihood of complications involving normal tissue. In our study, D90 (HR CTV) values were >140% PD for two patients whose CTVs were less than 25 cm3. Therefore, we expected that the IBICBT plan could achieve a ∼30% reduction of the doses to OARs without reducing the D90 (HR CTV) values to less than 100% PD. It is a similar result to that found in the studies of Zwahlen et al. We considered that this study is meaningful because there are no studies from Japan supporting the preceding DVH studies of the MRI-based IBICBT plan using GEC ESTRO recommendation from western countries. Because Japanese women have smaller body frames than western women, point A may exist relatively far from the external os of the uterus for Japanese women. The life-span of Japanese women is long and we often treat patients who are old, with poor performance status and a smaller body frame. To reduce severe complications for such patients, the IBICBT plan may be more useful compared with the dose prescription to point A that is typically 2 cm lateral from the external os.
In Japan, a remarkable piece of research was performed before the GEC ESTRO recommendation was reported [12], which was one of the most rapidly conducted IBICBT trials worldwide. The authors reported that MRI-IBICBT resulted in better tumor coverage. The mean V100 was 95.85% (range, 80.8–100%) in the IBICBT plan, and the mean point A dose was reduced to 85.6% (range, 46.1–106.0%) of PD. Although such pioneering work was done in Japan, subsequent progress was delayed because only a few institutes conducted the IBICBT trial. Wadasaki et al. reported that their conventional 2D treatment plans had been recalculated using CT images during applicator insertion, to produce DVH results [13]. Kato et al. investigated their DVH results for the rectum and reported that the late rectal complication rate correlated well with D0.1cc, D1cc and D2cc values [14]. They suggested that CT-based 3D dose–volume rectal parameters may be effective in predicting late rectal complications. In this study, the mean D2cc (bladder), D2cc (rectum) and D2cc (sigmoid) showed a ∼20% reduction with the IBICBT plan. We consider that the IBICBT plan may reduce late complications, however, further investigation is necessary because this study has only eight patients.
Although we could not actually treat patients using the IBICBT plan in this preliminary study, we hope to accumulate data in the near future showing which patients would be suitable candidates for the IBICBT plan. The other problem associated with the IBICBT plan is time constraints: three additional processes were required compared with the Manchester plan (CT and MRI scanning time, uploading and superimposition of CT, and MRI imaging and calculation time). To overcome this issue, we aimed to reduce the time required for superimposition and calculations. We believe that the IBICBT plan is a practical alternative plan to the Manchester plan.
In conclusion, our preliminary study of the IBICBT plan showed that the Manchester plan may be an overtreatment for small tumors, and it has insufficient dose distribution for larger tumors. The IBICBT plan could reduce the OAR dose while maintaining adequate tumor coverage.
ACKNOWLEDGEMENTS
This study was supported in part by the Ministry of Education, Culture, Sports, Science and Technology (Grant-in-Aid for Young Scientists (A) 21689034). We would like to thank Shunsuke Miyake, RTT, Mari Ueda, RTT, Keiko Kuriyama, MD, Yasushi Yoshimura, RTT, Hiroshi Yamada, RTT, Toshiro Kajihara, RTT, Shinichi Murata, RTT, Tadaaki Uegaki, RTT, Toshiaki Tarui, RTT, Miyuki Sakemi, Yoshiko Miki, the other staff of the departments of radiology and gynecology and nursing staff for helping us in many ways during the completion of this paper.
REFERENCES
- 1.Nakano T, Ohno T, Ishikawa H, et al. Current advancement in radiation therapy for uterine cervical cancer. J Radiat Res. 2010;51:1–8. doi: 10.1269/jrr.09132. [DOI] [PubMed] [Google Scholar]
- 2.Nag S, Cardenes H, Chang S, et al. Proposed guidelines for image-based intracavitary brachytherapy for cervical carcinoma: report from image-guided brachytherapy working group. Int J Radiat Oncol Biol Phys. 2004;60:1160–72. doi: 10.1016/j.ijrobp.2004.04.032. [DOI] [PubMed] [Google Scholar]
- 3.Haie-Meder C, Pötter R, Van Limbergen E, et al. Gynaecological (GYN) GEC-ESTRO Working Group. Recommendations from Gynaecological (GYN) GEC-ESTRO Working Group (I): concepts and terms in 3D image based 3D treatment planning in cervix cancer brachytherapy with emphasis on MRI assessment of GTV and CTV. Radiother Oncol. 2005;74:235–45. doi: 10.1016/j.radonc.2004.12.015. [DOI] [PubMed] [Google Scholar]
- 4.Pötter R, Haie-Meder C, Van Limbergen E, et al. Recommendations from gynaecological (GYN) GEC ESTRO working group (II): concepts and terms in 3D image-based treatment planning in cervix cancer brachytherapy-3D dose volume parameters and aspects of 3D image-based anatomy, radiation physics, radiobiology. Radiother Oncol. 2006;78:67–77. doi: 10.1016/j.radonc.2005.11.014. [DOI] [PubMed] [Google Scholar]
- 5.Nag S, Erickson B, Thomadsen B, et al. The American Brachytherapy Society recommendations for high-dose-rate brachytherapy for carcinoma of the cervix. Int J Radiat Oncol Biol Phys. 2000;48:201–11. doi: 10.1016/s0360-3016(00)00497-1. [DOI] [PubMed] [Google Scholar]
- 6.Pötter R, Dimopoulos J, Georg P, et al. Clinical impact of MRI assisted dose volume adaptation and dose escalation in brachytherapy of locally advanced cervix cancer. Radiother Oncol. 2007;83:148–55. doi: 10.1016/j.radonc.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 7.Wakatsuki M, Ohno T, Yoshida D, et al. Intracavitary combined with CT-guided interstitial brachytherapy for locally advanced uterine cervical cancer: introduction of the technique and a case presentation. J Radiat Res. 2011;52:54–8. doi: 10.1269/jrr.10091. [DOI] [PubMed] [Google Scholar]
- 8.Saitoh J, Ohno T, Sakurai H, et al. High-dose-rate interstitial brachytherapy with computed tomography-based treatment planning for patients with locally advanced uterine cervical carcinoma. J Radiat Res. 2011;52:490–5. doi: 10.1269/jrr.10189. [DOI] [PubMed] [Google Scholar]
- 9.Yoshida K, Yamazaki H, Takenaka T, et al. A dose-volume analysis of magnetic resonance imaging-aided high-dose rate image-based interstitial brachytherapy for uterine cervical cancer. Int J Radiation Oncology Biol Phys. 2010;77:765–72. doi: 10.1016/j.ijrobp.2009.05.027. [DOI] [PubMed] [Google Scholar]
- 10.Zwahlen D, Jezioranski J, Chan P, et al. Magnetic resonance imaging-guided intracavitary brachytherapy for cancer of the cervix. Int J Radiat Oncol Biol Phys. 2009;74:1157–64. doi: 10.1016/j.ijrobp.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 11.Tanderup K, Nielsen SK, Nyvang GB, et al. From point A to the sculpted pear: MR image guidance significantly improves tumour dose and sparing of organs at risk in brachytherapy of cervical cancer. Brachytherapy. 2010;94:173–80. doi: 10.1016/j.radonc.2010.01.001. [DOI] [PubMed] [Google Scholar]
- 12.Hatano K, Sekiya Y, Araki H, et al. MRI-based intracavitary high dose rate brachytherapy for carcinoma of the uterine cervix is the ‘Manchester’ system golden standard in the era of 3-D treatment planning and MRI? Int J Radiat Oncol Biol Phys. 1998;42(suppl316) [Google Scholar]
- 13.Wadasaki K, Monzen Y, Kurose T, et al. Computed tomography-based three-dimensional dosimetry of intracavitary brachytherapy for cervical cancer. Jpn J Radiol. 2010;28:740–5. doi: 10.1007/s11604-010-0504-3. [DOI] [PubMed] [Google Scholar]
- 14.Kato S, Tran DN, Ohno T, et al. CT-based 3D dose-volume parameter of the rectum and late rectal complication in patients with cervical cancer treated with high-dose-rate intracavitary brachytherapy. J Radiat Res. 2010;51:215–21. doi: 10.1269/jrr.09118. [DOI] [PubMed] [Google Scholar]