Abstract
Objective:
To present a case of a patient with spinal infection (SI) and highlight the chiropractor’s role in the prevention or minimization of devastating complications of SI.
Background:
Recent literature trends suggest an increasing prevalence of SI. Patients with SI most commonly present with unremitting progressive back pain and may or may not have fever or neurological signs. To avoid negative post-infection sequelae, establishing an early diagnosis and treatment is crucial.
Clinical Features:
A 29-year-old female diagnosed with L5-S1 disc herniation with impingement of the right S1 nerve root opted for surgical management. Iatrogenic bowel perforation during her spinal surgery resulted in contamination of the spinal surgical site, and findings in keeping with disco-osteomyelitis with epidural and paraspinal phlegmon formation were visualized on contrast enhanced MRI.
Conclusion:
Recent trends of increased spinal infection urge a heightened awareness by the chiropractor. The chiropractor can provide early diagnosis and supportive multidisciplinary care for such patients.
Keywords: spinal infection, disk space infection, discitis/diskitis, vertebral osteomyelitis, pyogenic, outcome
Abstract
Objectif :
Présenter le cas d’un patient atteint d’une infection de la moelle épinière (IME) et souligner le rôle du chiropraticien dans la prévention ou l’atténuation au minimum des complications dévastatrices d’une telle infection.
Contexte :
Les tendances qui se dégagent des études récemment publiées sur le sujet suggèrent une croissance dans la prévalence des IME. Les patients qui en sont atteints présentent le plus couramment des douleurs lombaires continues et progressives accompagnées ou non de fièvre ou de signes neurologiques. Afin d’éviter toute séquelle indésirable postinfection, il est essentiel d’en effectuer le diagnostic et le traitement précoce.
Caractéristiques cliniques :
Une femme de 29 ans, dont on a diagnostiqué une hernie discale L5-S1 avec coincement à la racine nerveuse S1 droite, a opté pour la gestion chirurgicale. Une perforation intestinale iatrogène survenue lors de sa chirurgie spinale a contaminé le champ opératoire de la moelle épinière, et des constats correspondants à une ostéomyélite discale avec formation épidurale et phlegmon paraspinal ont été visualisés sur IRM à contraste amélioré.
Conclusion :
Il est impératif que les chiropraticiens soient davantage sensibilisés aux infections de la moelle épinière en raison de l’augmentation récente du nombre de cas de celles-ci. Le chiropraticien peut établir un diagnostic précoce et dispenser des soins multidisciplinaires de soutien à ces patients.
Keywords: infection de la moelle épinière, infection de l’espace intervertébral, discite, ostéomyélite vertébrale, pyogène, résultat
Introduction:
Spinal infection (SI) can be pyogenic or non-pyogenic in nature and involve any anatomical area around the spine, including but not limited to infection of the disc, vertebral body, paravertebral soft tissues and the epidural space. The most common forms include: discitis, vertebral osteomyelitis, septic arthritis, muscular involvement (psoas abscess or paraspinal abscess), pararvertebral, and epidural abscess.4 Treatment can vary considerably depending on the type of spinal infection.
Spondylodiscitis, also referred to as spinal or vertebral osteomyelitis (VO) septic discitis, or disk-space infection is a common result of a pyogenic vertebral infection. This infection involves the disc space as well as the adjacent vertebral bodies and accounts for 2–4 % of all bone and joints infections.1–3 The most common microorganism responsible for pyogenic vertebral osteomyelitis (PVO) is Staphylococcus aureus. Non-pyogenic sources of infection include: Mycobacterium and a variety of fungal organisms such as Candida or Aspergillus. Three mechanisms of spinal infection dissemination have been identified. The most common route of spread is via hematogenous dissemination. Direct inoculation from iatrogenic sources is considered to be the next most common route followed by dissemination from an adjacent contamination. 4,5,6 This case report focuses on pyogenic spinal infection of the vertebral body and disc space and emphasizes the importance of considering infection within the list of differential diagnoses for progressively worsening low back pain. It will also describe the epidemiology, clinical presentation, radiographic features and typical management of spinal infections and aim to heighten the awareness of SI by the chiropractor to assist in the prevention or minimization of devastating complications.
Case:
A 29-year-old female medical researcher presented to an outpatient orthopedic clinic with a 5-month history of sharp right-sided lower back and posterior thigh pain that extended intermittently to the right foot. Her pain was constant and she found it difficult to find a relieving position. She additionally reported decreased sensation in the calf and lateral aspect of the right foot. She denied any lower extremity weakness or change in bladder or bowel function. There was no history of fevers, weight loss, or night sweats. Her past medical history was otherwise unremarkable.
On her initial examination she ambulated well. Her leg pain was aggravated with the extremes of forward flexion. Her lower back pain was aggravated by extension. Neurological examination revealed an absent S1 reflex on the right. Sensation to light and sharp touch were intact, although the region of her paresthesia approximated the S1 dermatome in the posterior calf and lateral foot. Motor power in the lower extremities was graded as 5/5 bilaterally. Straight leg raise testing was negative.
An MRI of her lumbar spine revealed a L5-S1 disc herniation with impingement of the right S1 nerve root. The patient opted for surgical management and a single level unilateral posterior lumbar decompression and discectomy was performed.
On postoperative day number 1 she developed severe abdominal pain and diffuse tenderness. An abdominal x-ray and CT examination revealed free intraperitoneal gas and fluid. She was taken back to the operating room by general surgery for urgent laparotomy for presumed iatrogenic small bowel or rectal injury. Intraoperative findings at the time of the laparotomy included: a loop of proximal ileum that was leaking enteric contents into the abdominal cavity, an iatrogenic hole in the presacral peritoneum through which the L5-S1 disc level could be palpated, and a few fragments of disc material within the intraabdominal cavity. The injured short segment of small bowel was resected. She was started on a course of broad-spectrum intravenous antibiotics. A swab from the presacral space revealed moderate leukocytosis and growth of Candida albicans. Her antibiotic care was modified under the direction of the Infectious Disease consult service.
Her back pain continued in the postoperative period although she did report some initial improvement. Her abdominal pain resolved. Her antibiotics were discontinued after a three and a half week course of therapy. By the time of her postoperative 6-week follow-up clinic visit, she was experiencing dramatic increases in her back and leg symptoms, accompanied by nausea and vomiting. She denied any fevers or chills. Examination at this time revealed aggravation of pain with all directions of range of motion testing, and continued paresthesia at the lateral aspect of the right foot. Lower extremity motor power remained normal. She was afebrile with stable vital signs. Blood work revealed an elevated white blood cell count, erythrocyte sedimentation rate, and C-reactive protein. This prompted a follow-up MRI examination of her spine, and CT evaluation of her abdomen and pelvis.
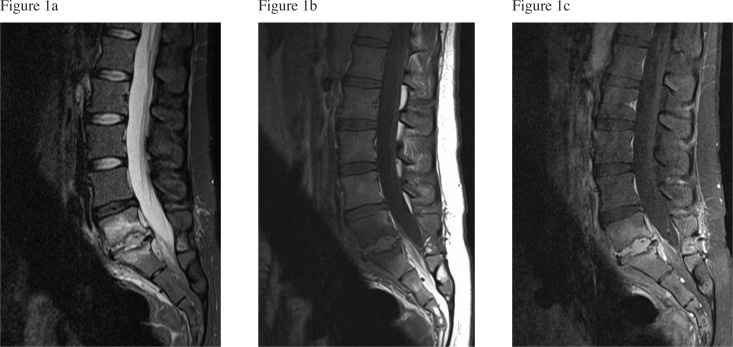
The MRI revealed endplate irregularity at the L5-S1 level. There was abnormal low T1, high T2 signal intensity and enhancement within the L5 and S1 vertebral bodies. Additional abnormal enhancing soft tissue was noted within the L5-S1 disc space, encasing the L5 and S1 nerve roots, anterior to the vertebral bodies at L5 and S1 and within the epidural space (Figure 1a–c). Imaging findings were in keeping with disco-ostemolyelitis with epidural and paraspinal phlegmon formation. CT examination of the abdomen did not reveal an additional infectious source.
Figure 1:
a) Sagital T2 weighted MR image of the lumbar spine demonstrates abnormal high T2 marrow signal intensity within the L5 and S1 vertebral bodies, and abnormal prevertebral and epidural T2 signal. Irregular inferior L5 and superior S1 endplates and loss of L5-S1 disc space are apparent b) Sagital T1 weighted image demonstrates corresponding low T1 signal intensity within the vertebral bodies c) Sagital contrast enhanced T1 weighted image reveals abnormally enhancing L5-S1 disc space, and prevertebral and epidural soft tissue.
The patient was restarted on IV antibiotics and symptoms gradually resolved after a second 8 week course of antibiotic therapy. At this point she was referred for physiotherapy for rehabilitation exercises and back education with no leg pain reported, and intermittent back pain. Examination revealed full range of motion, with normal sensation and motor power to the lower extremities. Six-month follow-up MRI examination demonstrated a reduction of both the abnormal vertebral body T2 signal intensity as well as the degree of abnormal epidural and prevertebral enhancement (Figure 2a–b). As she was clinically improved the remaining findings were thought to represent residual of previous infection and post-surgical changes.
Figure 2:
a) Follow up sagital T2 weighted image and b) contrast enhanced sagital T1 reveal a reduction in both the abnormal T2 signal and abnormally enhancing prevertebral and epidural soft tissue.
Discussion
Epidemiology
Several recent European epidemiological studies examining the incidence of spinal infection suggest an increasing trend of spinal pyogenic infections in adults.9,10,11,12,13 These retrospective studies retrieved hospital records of all patients who had an ICD code diagnosis of vertebral osteomyelitis (VO) and reported an incidence range from 0.70 to 2.4 per 100,000.9,10,11,12,13 Differences among studies can be partly explained by the different patient populations, with some studies including post-operative cases while others included non-pyogenic cases.
Recent trends also suggest that the diagnosis of both pyogenic and non-pyogenic spinal infection have been steadily on the rise.4,7–11,13,15 Most recently, Nagashima et al conducted a 50-year retrospective analysis of patients treated for spinal infection in Japan.7 There was approximately a 6.8-fold increase in diagnosed spinal infection from 1996–2005 compared to 1976–1985.7 According to Nagashima et al, the advancement of highly sensitive imaging modalities, such as contrast MRI and CT guided biopsy, create a heightened ability to diagnose spinal infection. As a result, this likely explains some of the recent increase in spinal infections observed. Other authors identify increasing rates of patients with compromised immune systems and IV drug use as culprits to the recent increase in spinal infection as they are associated with increased vulnerability to opportunistic organisms and consequent infection.4,7–11,15
The incidence of spinal infection increases with age.1,8,10,14,15 Several studies confirm that those individuals aged 50 to 80 years are the most susceptible.7,12,15 Grammatico et al observed an incidence rate of VO of approximately 9 per 100,000 in males aged 70 to 80 years.12 His colleagues also note that there is a male to female predominance of 1.5 – 3:1, an observation that is widely accepted.1,8,10,14,15 Interestingly, Grammatico et al observed an equal incidence rate in male and females up until the age of 20. At the age of 20 there is an increase in incidence rates in males as they progress in age. The authors speculate that one possible explanation to this observation may be the higher frequency of co-morbidities in men aged > 60 years, however, they did not draw any firm conclusions about this potential association.12 The literature suggests that patients with underlying diabetes, cancer, renal failure requiring hemodialysis or those who have had previous surgery appear to be at most risk for developing SI.10,15,16,17,18 Other potential risk factors include coronary heart disease, immunosuppressive disorders, liver disease, long term steroid use, IV drug users, severe trauma and advanced age.10,15,16,17,18
Clinical Presentation
Spinal infection such as vertebral osteomyelitis appears to have a predilection for the lumbar spine. Approximately 58% of cases noted in Mylona et al’s recent review15 occurred in the lumbar region.15 The extensive lumbar spine anastomosing veins and arteries, which favour infectious seeding via the hematogenous route of spread, offer some explanation for this observation.16 The thoracic spine (30%), cervical spine (11%) and sacrum (0.1%) are all less common sites for spinal infection.15
The clinical presentation of patients with early stage spinal infection varies widely among individuals, and the condition can be difficult to differentiate from other diagnoses. Patients in the sub-acute stage may present with vague symptoms often mimicking other common conditions. Atypical symptoms of chronic chest, abdominal, or hip pain may be present and often mask or overshadow the underlying back pain.15,19,20 Back pain and fever are the most common symptoms reported. Back pain at onset has a prevalence ranging from 91 – 100%.15 The nature of the pain is often unremitting and progressive and may lead to the patient becoming completely bed ridden. Paraspinal muscle spasms are also very common.15,16,20 The back pain may be relieved in recumbency and aggravated by activity, a presentation that can be confused with simple mechanical back pain and can lead to a delay in diagnosis.
Reports on the prevalence of fever at onset varies widely and ranges from 16.2% to 79.6%.21,22 The large discrepancy in prevalence rates that exists within the literature is believed to be due to variations in definition of what constitutes a fever as well as poor documentation of antipyretic analgesic use.15,19 The presence or absence of fever alone is insufficient to rule in or rule out spinal infection. Neurological impairment is also common, but similar to fever its presence varies widely, ranging from 14.3% to 51.7% of cases.23,24
Diagnosis
Establishing an early diagnosis in spinal infection patients is paramount but often difficult to confirm. In fact, Mc-Henry et al noted that only 28% of patients with VO were diagnosed within the first month of onset of symptoms.14 They also reported that only 24% of attending physicians included VO in their initial differential diagnosis.14 The importance of establishing a broad differential diagnosis early cannot be overlooked. As with all patients one must always rule out red flags for back pain that could indicate a significant medical illness.
Considering an active broad differential list with repeated careful neurological examination is important. Employing this strategy facilitates early diagnosis and results in prompt appropriate management, both of which are critical in suspected spinal infection.14
Imaging Features:
When spinal infection is first suspected, baseline conventional radiographs are indicated. Radiographs are relatively easy to access, are cost effective and give good visualization of bone tissue, which provide rationale for their use. In their review, Mylona et al noted that 95% of the included studies used radiography as a baseline and revealed radiographic abnormalities in 89% of the cases.15 However, Quinones-Hinojosa et al urge clinicians to beware of the 2–3 week lag in the initial presentation of radiographic signs of spinal infection. Radiographs during this 2–3 week latent period rarely exhibit diagnostic clues.20 Typically, the earliest radiographic sign is narrowing of the disc space. Blurring, irregularity and even destruction of the adjacent endplates tends to occur later.15,20
MRI is the imaging modality of choice for early detection and confirmation of spinal infection diagnosis since it closely reflects the pathological changes during the evolution of spinal infection.1,15 It has been reported to have 96% sensitivity, 94% specificity with 92% accuracy in correctly identifying spinal infection.1 Gadolinium contrast-enhanced MRI is considered the imaging gold standard1,4 and it has been reported to be capable of detecting spondylodiscitis as early as 48 hours after the initial inoculation 9. Typical MRI findings include, ill defined hypointense T1 and hyperintense T2 vertebral body marrow signal intensity with loss of the vertebral endplate on both sides of the partially or completely destroyed disc with associated loss of disc height. Paraspinal or epidural soft tissue infiltrations of edema, infection and/or fluid collections are often present.
The final diagnosis is a combination of clinical, imaging and biochemical findings.20 In the acute/subacute phase conventional radiographs should be ordered. Laboratory analysis, including ESR, CRP, and WBC is often ordered and may, in some cases be normal.20 Blood cultures should be retrieved preferably during a fever spike to identify the causal microorganism. It should be emphasized, however, that the accuracy of blood cultures to identify such organism varies.9,15,19,20 MRI and CT imaging should follow, including CT guided biopsy of the vertebral body or disc to successfully identify the causal organism and thus guide an appropriate antibiotic treatment regimen. In the absence of positive cultures of blood, spine biopsy is critical for the etiological diagnosis of spinal infection.9
If the diagnosis is delayed, serious complications are common. Delayed time to diagnosis usually results in greater degrees of neurologic impairment. Neurological impairment is more common in infections of the cervical spine. Acosta et al. reported that in the cervical spine there is a 60% chance of neurological deficit versus a 5–20% chance in the thoracic and lumbar spine.4 This is believed to be due to the decreased cross–sectional diameter of the cervical spinal canal in relation to the spinal cord compared with the thoracic or lumbar spine.4 The formation of epidural or paraspinal abscess may further compromise the spinal cord, thecal sac or intervertebral foramina which lead to more extensive neurological impairment and the development of these abscesses may require surgical drainage.15,16,25 Treatment can vary considerably depending on the type of spinal infection. For instance, an uncomplicated discitis with an intact neurological system can be treated medically with antibiotics while an epidural abscess causing progressive neurological compromise necessitates urgent surgical intervention.15,20
The mortality rate of spinal infection ranges from 6–20%.4,14,15,20,25 Early diagnosis, identification of causative agents, and early initiation of specific treatments dramatically reduces the mortality rate.15,20,25 McHenry and his colleagues examined the largest number of microbiologically diagnosed pyogenic VO cases to date, following these patients for a median of 6.5 years (range 2 days to 38 years). In 255 episodes, 146 (57%) recovered fully and 31% had qualified recovery defined as improvement with persistent pain, motor weakness or paralysis, and/or bowel/bladder dysfunction. The remaining 11% of patients died. For those patients who had qualified recovery, disability caused by pain was the most prevalent long-term poor outcome (66%), followed by motor weakness or paralysis (34%).14
Lindholm and Pylkkanen reported that up to 50% of patients with postoperative discitis who had been followed for longer periods, had severe chronic back pain and an inability to work or perform the normal activities of daily living.26 It is apparent that effective co-management of these post-infection problems must be important considerations for clinicians.
Summary:
Overall, spinal infection is not a common presentation, but can be devastating and the diagnosis of both pyogenic and non-pyogenic types appears to be increasing over time. Any patient with progressively unremitting back or leg pain with or without fever should receive a comprehensive evaluation for spinal infection. Heightened suspicion should be given to those patients who are elderly males with concomitant chronic illnesses such as immunosuppression, diabetes mellitus Type 2 and IV drug use. In these high-risk patients, clinicians should consider a broad differential diagnosis including spinal infection supplemented with comprehensive repeated neurological testing. Clinicians should also be aware of the high probability of long-term poor outcome and should work in a multidisciplinary fashion to co-manage these patients.
References:
- 1.Jevtic V. Vertebral infection. European Radiology. 2004;14(Suppl. 3):E43–E52. doi: 10.1007/s00330-003-2046-x. [DOI] [PubMed] [Google Scholar]
- 2.Khan IA, Vaccaro AR, Zlotolow DA. Management of vertebral diskitis and osteomyelitis. Orthopedics. 1999;22:758–765. doi: 10.3928/0147-7447-19990801-07. [DOI] [PubMed] [Google Scholar]
- 3.Tali ET. Spinal infections. European J Radiology. 2004;50:120–133. doi: 10.1016/j.ejrad.2003.10.022. [DOI] [PubMed] [Google Scholar]
- 4.Acosta FL, Galvez LF, Aryan HE, Ames CP. Recent advances: infections of the spine. Current Infectious Disease Reports. 2006;8(5):390–3. doi: 10.1007/s11908-006-0050-4. [DOI] [PubMed] [Google Scholar]
- 5.Falade OO, Antonarakis ES, Kaul DR, Saint S, Murphy PA. Beware of First Impressions. Spinal Cord. 2008;359(6):628–34. doi: 10.1056/NEJMcps0708803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim PSY, Hsu W. Discitis in an adult following acupuncture treatment: a case report. JCCA. 2004;48(2):132–6. [PMC free article] [PubMed] [Google Scholar]
- 7.Nagashima H, Yamane K, Nishi T, Yanjo Y, Teshima R. Recent trends in spinal infections: retrospective analysis of patients treated during the past 50 years. International Orthopaedics. 2010;34:395–399. doi: 10.1007/s00264-009-0741-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gasbarrini AL, Bertoldi E, Mazzetti M, Fini L, Terzi S, Gonella F. Clinical features, diagnostic and therapeutic approaches to haematogenous vertebral osteomyelitis. Eur Rev Med Pharmacol Sci. 2005;9:53–66. [PubMed] [Google Scholar]
- 9.Luzzati R, Giacomazzi D, Danzi MC, Tacconi L, Concia E, Vento S. Diagnosis, management and outcome of clinically-suspected spinal infection. Journal of Infection. 2009;58(4):259–65. doi: 10.1016/j.jinf.2009.02.006. [DOI] [PubMed] [Google Scholar]
- 10.Krogsgaard MR, Wagn P, Bengtsson J. Epidemiology of acute vertebral osteomyelitis in Denmark: 137 cases in Denmark 1978–1982, compared to cases reported to the National Patient Register 1991–1993. Acta Orthopaedica Scandinavica. 1998;69(5):513–7. doi: 10.3109/17453679808997789. [DOI] [PubMed] [Google Scholar]
- 11.Colmenero JD, Jimenez-Mejias ME, Sanchez-Lora FJ, Reguera JM, Palomino-Nicas J, Martos F, et al. Pyogenic, tuberculous, and brucellar vertebral osteomyelitis: a descriptive and comparative study of 219 cases. Annals Rheumatic Diseases. 1997;56(12):709–715. doi: 10.1136/ard.56.12.709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grammatico L, Baron S, Rusch E, Lepage B, Surer N, Desenclos JC, et al. Epidemiology of vertebral osteomyelitis (VO) in France: analysis of hospital-discharge data 2002–2003. Epidemiology and Infection. 2008;136(5):653–60. doi: 10.1017/S0950268807008850. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hopkinson N, Stevenson J, Benjamin S. A case ascertainment study of septic discitis: clinical, microbiological and radiological features. QJM : monthly journal of the Association of Physicians. 2001;94(9):465–70. doi: 10.1093/qjmed/94.9.465. [DOI] [PubMed] [Google Scholar]
- 14.Mchenry MC, Easley KA, Locker GA. Vertebral Osteomyelitis : Long-Term Outcome for 253 Patients from 7 Cleveland-Area Hospitals. Clinical Infectious Diseases. 2002;44195 doi: 10.1086/340102. [DOI] [PubMed] [Google Scholar]
- 15.Mylona E, Samarkos M, Kakalou E, Fanourgiakis P, Skoutelis a. Pyogenic vertebral osteomyelitis: a systematic review of clinical characteristics. [Internet] Seminars in arthritis and rheumatism. 2009;39(1):10–7. doi: 10.1016/j.semarthrit.2008.03.002. [DOI] [PubMed] [Google Scholar]
- 16.Priest DH, Peacock JE. Hematogenous vertebral osteomyelitis due to staphylococcus aureus in the adult: clinical features and therapeutic outcomes ?????? 2005;98:854–862. doi: 10.1097/01.smj.0000168666.98129.33. [DOI] [PubMed] [Google Scholar]
- 17.Stoeckle M, Kaech C, Trampuz A, Zimmerli W. The role of diabetes mellitus in patients with bloodstream infections. Swiss Med Wkly. 2008;138:512–9. doi: 10.4414/smw.2008.12228. [DOI] [PubMed] [Google Scholar]
- 18.Butler JS, Shelly MJ, Timlin M, Powderly WG, O’Byrne JM. Nontuberculous pyogenic spinal infection in adults: a 12-year experience from a tertiary referral center. Spine. 2006;31(23):2695–700. doi: 10.1097/01.brs.0000244662.78725.37. [DOI] [PubMed] [Google Scholar]
- 19.Zimmerli W. Vertebral osteomyelitis. J Medicine (Cincinnati) 2010;362:1022–1029. doi: 10.1056/NEJMcp0910753. [DOI] [PubMed] [Google Scholar]
- 20.Quiñones-Hinojosa A, Jun P, Jacobs R, Rosenberg WS, Weinstein PR. General principles in the medical and surgical management of spinal infections: a multidisciplinary approach. Neurosurgical Focus. 2004;17(6):E1. doi: 10.3171/foc.2004.17.6.1. [DOI] [PubMed] [Google Scholar]
- 21.Carragee EJ. Pyogenic vertebral osteomyelitis. J Bone Joint Surg (Am) 1997;79(6):874–80. doi: 10.2106/00004623-199706000-00011. [DOI] [PubMed] [Google Scholar]
- 22.Nolla JM, Ariza J, Gomez-Vaquero C. Spontaneous pyogenic vertebral osteomyelitis in nondrug users. Semin Arthritis Rheum. 2002;31:271–8. doi: 10.1053/sarh.2002.29492. [DOI] [PubMed] [Google Scholar]
- 23.Zarrouk V, Feydy A, Sallés F, Dufour V, Guigui P, Redondo A. Imaging does not predict the clinical outcome of bacterial vertebral osteomyelitis. Rheumatology. 2007;46(2):292–295. doi: 10.1093/rheumatology/kel228. [DOI] [PubMed] [Google Scholar]
- 24.Chelsom J, Solberg CO. Vertebral osteomyelitis at a Norwegian University Hospital 1987–97: clinical features, laboratory findings and outcome. Scand J Infect Dis. 1998;30:147–51. doi: 10.1080/003655498750003537. [DOI] [PubMed] [Google Scholar]
- 25.Sendi P, Bregenzer T, Zimmerli W. Spinal epidural abscess in clinical practice. QJM: monthly journal of the Association of Physicians. 2008;101(1):1–12. doi: 10.1093/qjmed/hcm100. [DOI] [PubMed] [Google Scholar]
- 26.Lindholm TS, Pylkkanen P. Discitis following removal of intervertebral disc. Spine. 1982;7:618–22. doi: 10.1097/00007632-198211000-00018. [DOI] [PubMed] [Google Scholar]