Abstract
Chronic granulomatous inflammation may develop after injecting foreign oily substances into the penis. The disorder affects mainly the site of administration, but regional lymphadenopathy or even systemic disease can occur. We present a 39-year-old man with petroleum jelly-induced penile lesion and unilateral inguinal lymphadenitis mimicking incarcerated inguinal hernia. At hernioplasty no hernial sac was found, but enlarged lymph nodes suspicious for malignancy were identified. The histopathologic findings of these nodes were consistent with mineral oil granuloma. Paraffinoma of the male genitalia can cause various clinical features posing a differential diagnostic dilemma. Regional lymphadenitis may be the main clinical characteristic. Patient’s history, physical and histopathological examination are required to establish the diagnosis.
Introduction
Chronic granulomatous inflammation may develop following injection of foreign oily substances into penis.1–8 The disorder affects mainly the site of administration, but regional lymphadenopathy or even systemic disease can occur.1,7,9 Establishing the diagnosis is challenging if the clinical picture is dominated by regional lymphadenitis.
Case report
A 39-year-old man was referred to our surgical department because of left inguinal swelling and pain. The symptoms developed two weeks before while he was lifting heavy objects. His medical history was unremarkable. On physical examination, a left inguinal painful mass of about 10 cm was found. The penis showed yellowish discolouration and deformity without any pain or functional disturbances (Fig. 1). The patient admitted to giving himself petroleum jelly injections into his penis 3 years before. The complete blood counts were within normal limits. On ultrasound examination the left inguinal mass was considered a hernia containing small intestinal loops filled with bowel content, without peristaltic movements. The patient was operated on because of the suspicion of an incarcerated inguinal hernia. A Bassini type hernioplasty was planned. During the operation, no hernia was found, however we found enlarged lymph nodes ranging between 1.5 and 6 cm; the operation was then converted to a lymph node biopsy. The three largest nodes, suspicious of malignancy were removed and sent for histopathological workup. Grossly the nodes were 6 cm, 5 cm and 1.5 cm, maximum, and the cut surfaces were homogeneous grayish (Fig. 2). Microscopically, the lymph nodes contained collections of epitheloid and vacuolated histiocytes (lipophages) and foreign body-type multinucleated giant cells around variously sized round empty spaces (Fig. 3). Focally, there were also neutrophil granulocytes around these spaces. No fibrosis was present. Frozen sections stained by Oil Red O demonstrated lipids in the vacuoles. No pathogens were identified using Ziehl-Neelsen, Warthin-Starry, Grocott and PAS stains. Considering the patient’s history and physical findings, the diagnosis of petroleum jelly-induced penile paraffinoma with granulomatous lymphadenitis was made.
Fig. 1.

Penile deformity firm on palpation due to injection of petroleum jelly 3 years prior to presentation.
Fig. 2.
Cut surface of one of the lymph nodes removed during surgery suspicious for malignancy.
Fig. 3.
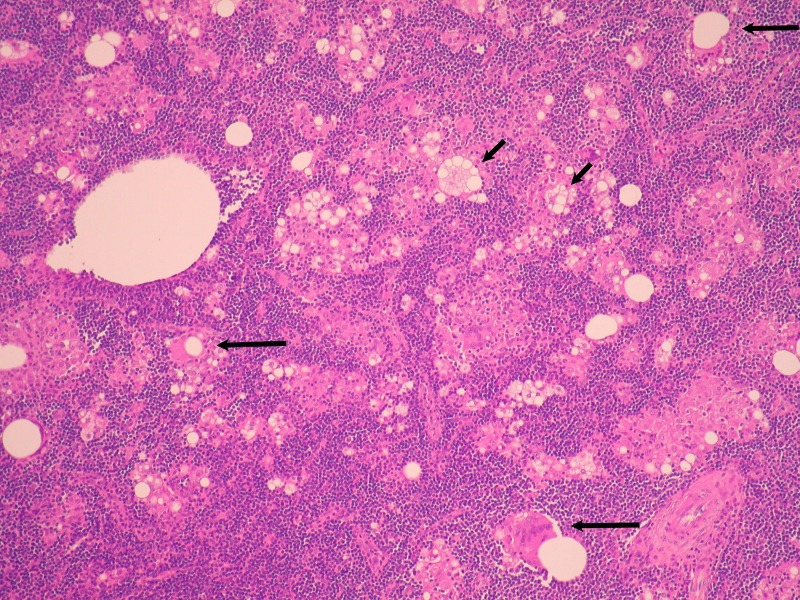
Foreign material induced granulomatous lymphadenitis consistent with paraffinoma of the lymph node. The white vacuoles represent the oily material after tissue processing. Paler pink areas among dark lymphocytic fields reflect the granuloma forming histiocytic reaction with epithelioid histiocytes, Langhans type giant cells (not clearly discernible at this magnification), multivacuolated phagocytes (short arrows) and multinucleated foreign body type giant cells engulfing the oily material in larger vacuoles (long arrows); Hematoxylin and eosin ×100.
Discussion
Paraffinoma is a foreign body reaction incited by exogenous oily substances. Other frequently used names of the disorder include slerosing lipogranuloma, mineral oil granuloma, oleogranuloma. The first paraffin injection into the male genitalia was reported by Gersuny in 1899 when mineral oil was injected into the scrotum of a boy who had undergone bilateral orchidectomy for genital tuberculosis.10 Adverse effects from the injection of oils were reported as early as 1906 by Heidingsfeld who described disfiguring subcutaneous nodules in two patients receiving paraffin injections for facial wrinkles.11 Based on the resulting complications, this practice is very rare in western countries; however, it is still performed in Eastern European and Asian countries.2–6,8 A wide variety of oils, including paraffin, petroleum jelly, silicone and cod liver oil, have been injected into the penis for augmentation.5,6 The body lacks the enzymes to break down these oils and consequently foreign body reaction develops.
From a histologic point of view, petroleum jelly injection into the skin causes an acute purulent inflammation, followed by a typical granulomatous reaction. After several months, this lesion is replaced by chronic, fibrotic inflammatory tissue.1 The latency period between the initial injection and the clinical symptoms has been documented anywhere from 2 days to 37 years.4,7
In most cases, the disorder is localized to the penis, with or without scrotal involvement. Sometimes locoregional disease develops with regional lymphadenitis.6 Our case was a locoregional process dominated by the inflammation of unilateral regional lymph nodes. To the best of our knowledge, this is the first report of a locoregional paraffinoma with the predominance of inguinal lymphadenitis. Systemic dissemination causing death is also on record.9
Conclusion
We propose that paraffinoma can be classified into local, locoregional and systemic forms; this also reflects their incidence, systemic disease being the least common. The knowledge of patient’s history, and physical and histopathological examination is necessary to establish the correct diagnosis. This presentation underscores the importance of full physical examination, including the genitalia and also highlights how clinico-pathological cooperation is important to establish some diagnoses.
Footnotes
Competing interests: None declared.
This paper has been peer-reviewed.
References
- 1.Nyirádi P, Kelemen Z, Kiss A, et al. Treatment and outcome of vaseline-induced sclerosing lipogranuloma of the penis. Urology. 2008;71:1132–7. doi: 10.1016/j.urology.2007.12.081. [DOI] [PubMed] [Google Scholar]
- 2.Cohen LC, Keoleian CM, Krull E. Penile paraffinoma. J Am Acad Dermatol. 2001;45:S222–4. doi: 10.1067/mjd.2001.103995. [DOI] [PubMed] [Google Scholar]
- 3.Lee T, Choi HR, Lee YT, et al. Paraffinoma of the penis. Yonsei Medical Journal. 1994;35:344–8. doi: 10.3349/ymj.1994.35.3.344. [DOI] [PubMed] [Google Scholar]
- 4.Eandi JA, Yao AP, Javidan J. Penile paraffinoma: delayed presentation. Int Urol Nephrol. 2007;39:553–5. doi: 10.1007/s11255-006-9058-9. [DOI] [PubMed] [Google Scholar]
- 5.Al-Ansari AA, Shamsodini A, Talib RA, et al. Subcutaneous cod liver oil injection for penile augmentation: Review of literature and report of eight cases. Urology. 2010;75:1181–4. doi: 10.1016/j.urology.2009.11.023. [DOI] [PubMed] [Google Scholar]
- 6.Bjurlin MA, Carlsen J, Grevious M, et al. Mineral oil-induced scerosing lipogranuloma of the penis. J Clin Aesthet Dermatol. 2010;3:41–4. [PMC free article] [PubMed] [Google Scholar]
- 7.Picozzi SCM, Carmignani L. Paraffinoma of the penis. Int J Emerg Med. 2010;3:507–8. doi: 10.1007/s12245-010-0221-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Akkus E, Iscimen A, Tasli L, et al. Paraffinoma and ulcer of the external genitalia after self-injection of vaseline. J Sex Med. 2006;3:170–2. doi: 10.1111/j.1743-6109.2005.00096.x. [DOI] [PubMed] [Google Scholar]
- 9.Rollins CE, Reiber G, Guinee DG, et al. Disseminated lipogranulomas and sudden death from self-administered mineral oil injection. Am J Forensic Pathol. 1997;18:100–3. doi: 10.1097/00000433-199703000-00019. [DOI] [PubMed] [Google Scholar]
- 10.Gersuny R. Harte und weiche Paraffinprothesen. Zentralbl Chir. 1903;30:1–5. [Google Scholar]
- 11.Heidingsfeld ML. Histopathology of paraffin Prosthesis. J Cutan Dis. 1906;24:513–21. [Google Scholar]



