Abstract
Background
There are conflicting data regarding optimal treatment of non-culprit lesions detected during primary percutaneous coronary intervention (PCI) in patients with ST-elevation myocardial infarction (STEMI) and multi-vessel disease (MVD). We aimed to investigate whether ischaemia-driven early invasive treatment improves the long-term outcome and prevents major adverse cardiac events (MACE).
Methods
121 patients with at least one non-culprit lesion were randomised in a 2:1 manner, 80 were randomised to early fractional flow reserve (FFR)-guided PCI (invasive group), and 41 to medical treatment (conservative group). The primary endpoint was MACE at 3 years.
Results
Three-year follow-up was available in 119 patients (98.3 %). There was no significant difference in all-cause mortality between the invasive and conservative strategy, 4 patients (3.4 %) died, all in the invasive group (P = 0.29). Re-infarction occurred in 14 patients (11.8 %) in the invasive group versus none in the conservative group (p = 0.002). Re-PCI was performed in 7 patients (8.9 %) in the invasive group and in 13 patients (32.5 %) in the conservative group (P = 0.001). There was no difference in MACE between these two strategies (35.4 vs 35.0 %, p = 0.96).
Conclusions
In STEMI patients with MVD, early FFR-guided additional revascularisation of the non-culprit lesion did not reduce MACE at three-year follow-up compared with a more conservative strategy. The rate of MACE in the invasive group was predominantly driven by death and re-infarction, whereas in the conservative group the rate of MACE was only driven by repeat interventions.
Keywords: Acute myocardial infarction, Multi-vessel disease, Primary percutaneous coronary intervention, Multi-vessel angioplasty, Long-term follow-up, Medical therapy
Introduction
The prevalence of multi-vessel disease (MVD) in patients presenting with acute ST-segment elevation myocardial infarction (STEMI) approaches 40 % [1]. Patients with MVD form a subgroup at high risk for major adverse cardiac events (MACE) in the first year after primary percutaneous coronary intervention (PCI) for STEMI, with a reported incidence of 14.5 % of MACE in patients with single-vessel disease, compared with 19.5 % and 23.6 % in those with two- and three-vessel disease, respectively [2]. It has been shown that the presence of multiple complex plaques is related to more adverse cardiac events during follow-up [3].
Contemporary guidelines recommend treating only the infarct-related artery (IRA) during primary PCI, leaving the other stenosed vessels untreated (culprit-only revascularisation) and to only treat these lesions during a second elective procedure (staged revascularisation) if ischaemia is documented [4]. It is not well known whether the long-term prognosis of patients with MVD can be improved by early additional revascularisation. Results from a recent randomised, not ischaemia guided, study have suggested that the rate of long-term MACE is reduced in patients with early complete revascularisation compared with culprit vessel-only angioplasty [5].
The current randomised study aimed to compare long-term clinical outcome after additional early ischaemia-guided revascularisation versus a more conservative treatment strategy of ischaemia-guided revascularisation at a later stage.
Methods
Between June 2004 and February 2007, 952 patients with MVD and STEMI treated with primary PCI were recruited in the study in a single tertiary referral centre in the Netherlands (Table 1).
Table 1.
Exclusion log
| 952 patients with multi-vessel disease underwent primary PCI for STEMI between June 2004 and February 2007 |
|---|
| 199 Already in other primary PCI study |
| 159 Logistical problems |
| 10 Died before randomisation |
| 7 Stent thrombosis before randomisation |
| 20 Not specified |
| 88 Inclusion criteria not met |
| 29 Primary PCI not successful |
| 13 Complete revascularisation by PCI not feasible |
| 46 Reference diameter of the remaining lesion(s) are <2.5 mm |
| 348 Exclusion criteria met |
| 23 Indication urgent PCI of a non-culprit lesion |
| 12 Urgent indication for CABG |
| 84 Chronic occlusion of one of the non-infarct-related vessels |
| 47 Previous CABG |
| 24 Stenosis of the left main >50 % |
| 11 Chronic atrial fibrillation |
| 119 Patient is older than 80 years |
| 15 No written informed consent obtained |
| 13 Comorbidity making follow-up unlikely |
| 121 patients randomised (13 %) |
PCI percutaneous coronary intervention, STEMI ST-elevation myocardial infarction, CABG coronary artery bypass grafting
The study was approved by the Medical Ethics Committee of the hospital. Written informed consent was obtained for all patients.
Patients with MVD who underwent successful primary angioplasty for STEMI were candidates for the study. Successful PCI was defined as a residual diameter stenosis of <50 % and TIMI ≥2 flow. MVD was defined as one or more significant stenoses in at least two major epicardial coronary arteries, or the combination of a side branch and a main epicardial vessel provided that they supplied different territories [6]. A significant stenosis was defined as a diameter stenosis of ≥50 % in luminal diameter (in at least one view, on visual interpretation or preferably by QCA). The minimal luminal diameter adjacent to the lesion to be treated had to be at least 2.5 mm. Patients were excluded from the study if they had an urgent indication for additional revascularisation, were >80 years old, had a chronic occlusion of one of the non-infarct-related arteries, prior coronary artery bypass graft (CABG), left main stenosis of ≥50 %, restenotic lesions in non-infarcted arteries, chronic atrial fibrillation, limited life expectancy, or other factors that made complete follow-up unlikely. The indication for an additional revascularisation procedure outside the protocol was determined by an expert panel of interventional cardiologists and thoracic surgeons (at least one of each discipline).
Patients fulfilling both inclusion and exclusion criteria were randomised to invasive or conservative treatment strategies. Randomisation was performed by means of a computer program. Patients were allocated to an invasive or conservative treatment in a 2:1 ratio respectively (see also power calculation).
Invasive treatment strategy
In this group, ischaemia-guided additional revascularisation was performed during the in-hospital phase after primary PCI or in an outpatient setting but no later than 3 weeks after STEMI. After repeat coronary angiography, FFR was measured in the vessels with a significant stenosis and also in the IRA if re-stenosis was present. If the FFR was compatible with ischaemia (FFR < 0.75), PCI of the stenosis was performed. Otherwise, the vessel was left untreated. In severe lesions (>90 % stenosis), PCI was performed without preceding FFR measurement.
Conservative treatment strategy
In this group, further treatment after primary PCI was left to the treating physician. Aggressive revascularisation without symptoms was discouraged in this group. If symptoms did occur, a strategy of ischaemia-guided additional revascularisation was followed. Exercise testing, dobutamine stress echocardiography or myocardial scintigraphy were considered acceptable means to demonstrate ischaemia.
Endpoints
Ejection fraction at 6 months was the primary endpoint of the study. Major adverse cardiac events (MACE) after 3 years of follow-up was a prespecified secondary endpoint. MACE included death, nonfatal re-infarction and additional revascularisation procedures. Non-fatal re-infarction was defined as new Q waves on the ECG or a new creatine kinase (CK) and CK-MB rise above the upper limit of normal. This included periprocedural infarctions in the invasive treatment arm. Endpoints were analysed according to an intention-to-treat protocol.
Medication
All patients were treated with aspirin, β-blockade and an ACE inhibitor unless contraindicated. Patients who received a stent were treated with clopidogrel 75 mg once daily for at least 30 days after a loading dose of 300 mg. Use of a glycoprotein 2b/3a inhibitor during or after angioplasty was left to the discretion of the operator.
Statistics and presentation of the results
Student’s t-test was used to assess statistically significant differences between continuous variables, Chi-square was used for differences between proportions. A two-sided p-value of <0.05 was considered statistically significant. Kaplan-Meier curves were used to represent survival and cumulative incidence of events to the follow-up.
Results
Baseline
Between June 2004 and February 2007, 952 STEMI patients with MVD underwent primary PCI. A considerable number of patients could not be included in the study because of participation in other primary PCI studies (199 patients) or logistical problems (159 patients, mostly early transfers to referring hospitals, Table 1). After application of inclusion and exclusion criteria, 121 patients could be included and randomised in this period. Baseline characteristics are summarised in Table 2.
Table 2.
Baseline characteristics
| Invasive (n = 80) | Conservative (n = 41) | p-value | |
|---|---|---|---|
| Male gender | 80.0 % | 80.5 % | 0.94 |
| Age | 62 ± 10 | 61 ± 11 | 0.66 |
| Hypertension | 26.3 % | 42.5 % | 0.07 |
| Diabetes mellitus | 6.3 % | 5.0 % | 1.00 |
| Smoking | 44.2 % | 47.5 % | 0.73 |
| Hypercholesterolaemia | 15.0 % | 30.0 % | 0.05 |
| Family history of CAD | 40.3 % | 43.6 % | 0.73 |
| Previous MI | 6.3 % | 4.9 % | 1.00 |
| Previous PCI | 3.8 % | 2.4 % | 1.00 |
| Previous CABG | 0 % | 0 % | 1.00 |
| Previous CVA | 0 % | 2.4 % | 0.34 |
| Killip class on admission | |||
| I | 93.8 % | 97.6 % | 0.31 |
| II | 5.0 % | 0 % | |
| III | 1.3 % | 2.4 % | |
| Systolic blood pressure | 132 ± 24 | 137 ± 24 | 0.26 |
| Diastolic blood pressure | 78 ± 17 | 84 ± 17 | 0.08 |
| Heart rate | 71 ± 16 | 73 ± 16 | 0.48 |
CABG coronary artery bypass grafting, CAD coronary artery disease, CVA cerebrovascular accident, MI myocardial infarction, PCI percutaneous coronary intervention
Hypertension and hypercholesterolaemia were more frequent in the conservative group. The prevalence of diabetes, heart failure and previous cardiac events were comparable in both groups. Most patients had two-vessel disease (Table 3); the number of non-culprit lesions per patient was comparable in both groups (1.3 ± 0.5 vs 1.2 ± 0.4, p = NS). The right coronary artery was the infarct-related artery in the majority of cases.
Table 3.
Angiographic data of primary PCI
| Invasive (n = 80) | Conservative (n = 41) | p-value | |
|---|---|---|---|
| Vessel disease | |||
| - Two | 75.0 % | 80.5 % | 0.498 |
| - Three | 25.0 % | 19.5 % | |
| Infarct-related artery | |||
| - RCA | 55.0 % | 46.3 % | 0.571 |
| - CX | 23.8 % | 24.4 % | |
| - LAD | 21.3 % | 29.3 % | |
| TIMI pre | |||
| - 0 | 65.0 % | 63.4 % | 0.754 |
| - 1 | 6.3 % | 9.8 % | |
| - 2 | 11.3 % | 14.6 % | |
| - 3 | 17.5 % | 12.2 % | |
| TIMI post | |||
| - 2 | 1.3 % | 4.9 % | 0.224 |
| - 3 | 98.8 % | 95.1 % | |
| MBG | |||
| - 0 | 0 % | 2.8 % | 0.563 |
| - 1 | 2.9 % | 2.8 % | |
| - 2 | 40.0 % | 36.1 % | |
| - 3 | 57.1 % | 58.3 % | |
| Treatment | |||
| PCI balloon only | 7.5 % | 17.1 % | 0.107 |
| PCI with stent | 92.5 % | 82.9 % | |
| PCI with DES | 22.5 % | 17.1 % | 0.435 |
| GP 2b/3a blocker | 45.0 % | 46.3 % | 0.888 |
Cx circumflex artery, DES drug-eluting stent, GP glycoprotein, LAD left descending branch, MBG PCI percutaneous coronary intervention, MBG myocardial blush grade, RCA right coronary artery, TIMI thrombolysis in myocardial infarction
Angiography and revascularisation
Almost all patients had TIMI 3 flow after the procedure, and myocardial blush grade was 2 or 3 in over 90 %. The majority of the patients received a stent, 20 % of which were drug-eluting. The use of glycoprotein 2b/3a inhibitors was similar in both groups.
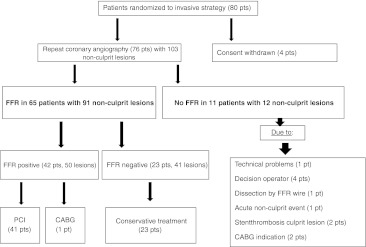
In the invasive group, repeat coronary angiography was performed in 76/80 patients (95 %) at a median of 7.5 days (interquartile range 5–20) after primary PCI. FFR analysis of the non-culprit lesions was available in 65/80 (81 %) patients. In 15/80 (19 %) FFR was not performed for various reasons (Fig. 1). Of the 65 patients who underwent FFR, PCI of non-culprit lesion was performed in 41 patients (63 %), 1 (1.5 %) patient underwent CABG and the remaining patients were treated conservatively (35 %). In the conservative group, testing for residual ischaemia was postponed until after discharge.
Fig. 1.
Repeat coronary angiography and FFR measurements
Outcome
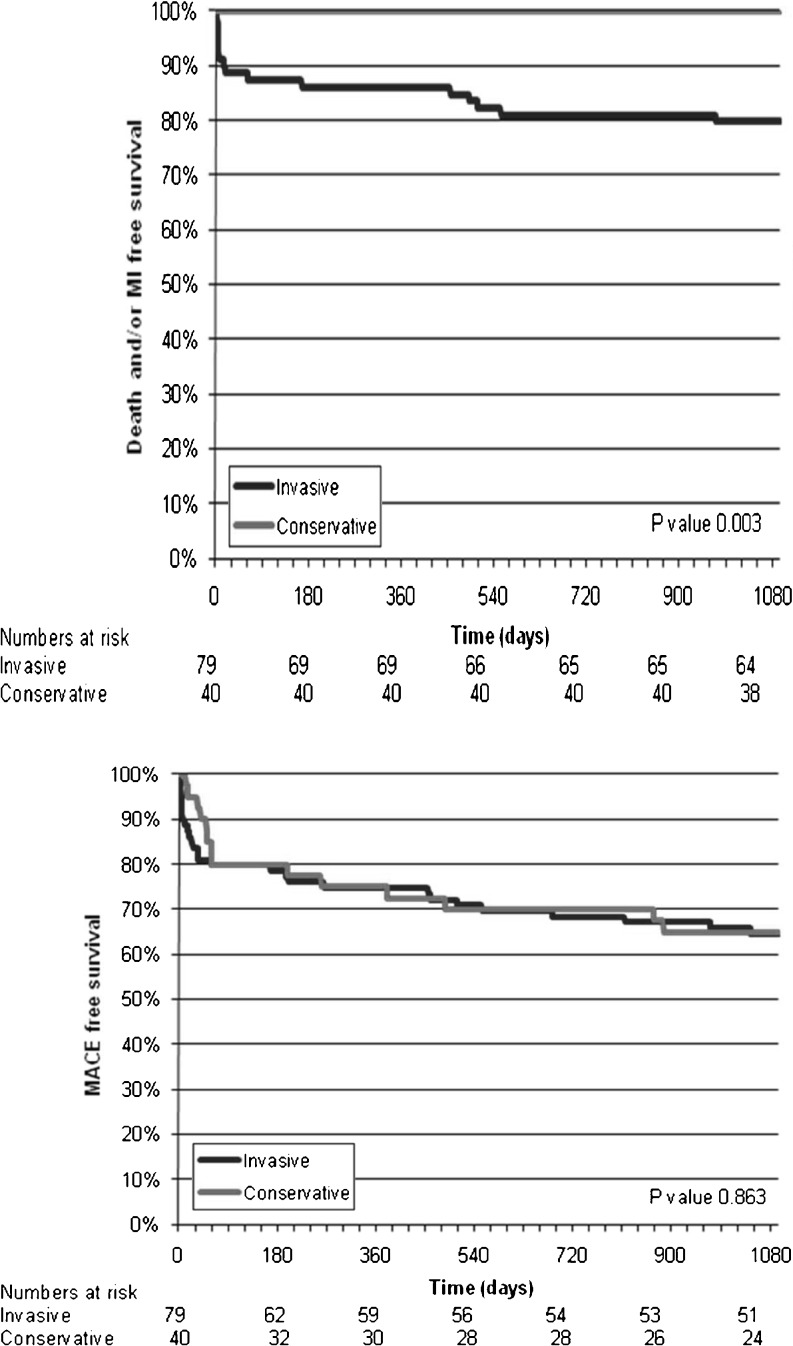
Previously we reported the results of the primary endpoint [7]. Three-year follow-up was available in 119 of 121 patients. One patient was lost to follow-up and one patient withdrew his informed consent. There was no significant difference in all-cause mortality between the invasive and conservative strategy. Throughout the follow-up 4 patients (3.4 %) died, all in the invasive group (P = 0.30). Concerning death and/or re-infarction, re-hospitalisation and re-PCI, there were significant differences. Sixteen patients (13.4 %) experienced death and/or nonfatal re-infarction, all in the invasive group (P = 0.002). Twenty patients (8.9 %) underwent PCI in a non-culprit vessel, 7/79 (8.9 %) in the invasive group and 13/40 (32.5 %) in the conservative group (P = 0.001). There was a significant difference in repeat PCI of the culprit vessel between the invasive and conservative group. In the invasive group 8 patients (10.1 %) underwent repeat PCI versus none in the conservative group. With respect to CABG there was a borderline significant difference between the two strategies. In the invasive group, 12/79 (15.2 %) patients underwent CABG whereas in conservative group only 1 (2.5 %) patient had surgery. (Table 4 and Fig. 2).
Table 4.
Intention to treat analysis, events within 3 years (n = 121)
| Total | Invasive | Conservative | P value | |
|---|---|---|---|---|
| Death | 4/119 (3.4 %) | 4/79 (5.1 %) | 0/40 | 0.30 |
| Re-PCI | 28/119 (23.5 %) | 15/79 (19.0 %) | 13/40 (32.5 %) | 0.10 |
| Re-PCI NCL | 20/119 (8.9 %) | 7/79 (8.9 %) | 13/40 (32.5 %) | 0.001 |
| Re-PCI CL | 8/119 (6.7 %) | 8/79 (10.1 %) | 0/40 | 0.05 |
| CABG | 13/119 (10.9 %) | 12/79 (15.2 %) | 1/40 (2.5 %) | 0.05 |
| Re-MI | 14/119 (11.8 %) | 14/79 (17.7 %) | 0/40 | 0.002 |
| MACE | 42/119 (35.3 %) | 28/79 (35.4 %) | 14/40 (35.0 %) | 0.96 |
| Death and/or MI | 16/119 (13.4 %) | 16/79 (20.3 %) | 0/40 | 0.002 |
CL culprit lesion, MACE major adverse cardiac events, MI myocardial infarction, NCL non-culprit lesion, PCI percutaneous coronary intervention
Fig. 2.
Kaplan-Meier curves describing survival-free death and/or MI (upper panel), and survival free of major adverse cardiac events (MACE) (bottom panel)
Discussion
To the best of our knowledge, this is the first study which compared early FFR-guided additional revascularisation after primary PCI with the more conservative strategy that is currently recommended by the guidelines. The main finding of the study was that after a follow-up of 3 years, early FFR-guided additional revascularisation did not reduce the incidence of MACE compared with the more conservative strategy.
Previously we reported that FFR-guided early additional revascularisation resulted in more death and MI compared with culprit-only revascularisation (14 vs 0 %, p = 0.015) and found no difference in MACE between the invasive and conservative group (21 vs 22 %, p = 0.93) at 6-months follow-up [7]. In the present study we demonstrated that FFR-guided early additional revascularisation (invasive approach) reduced the number of non-culprit related PCI procedures after discharge compared with the conservative strategy. However, death or re-infarction was more common in the FFR-guided group. In the invasive group the rate of MACE was predominantly driven by death and re-infarction, whereas in the conservative group the rate of MACE was only driven by more PCI procedures. This underlines that an invasive strategy leads to a reduction in the need for later revascularisation of non-culprit lesions but this is offset by more other cardiac events, mostly myocardial infarctions. In the present study we also observed that most MACE occurred during the first 6 months of follow-up (Table 5). This is in line with our previous conclusion that an early ischaemia-guided additional revascularisation prevents later PCI procedures but does not result in a reduction of total MACE [7].
Table 5.
Events in 6 months versus 3 years
| 6-month follow-up (n = 121) | 3-year follow-up (n = 119) | |||||
|---|---|---|---|---|---|---|
| Invasive (n = 80) | Conservative (n = 41) | P value | Invasive (79) | Conservative (40) | P value | |
| Death/Re-MI | 14 % (11) | 0 % | 0.015 | 20 % (16) | 0 % | 0.002 |
| Re-PCI | 13 % (10) | 22 % (9) | ns | 19 % (15) | 32.5 % (14) | ns |
| - Re- PCI NCL | 7.5 % (6) | 22 % (9) | 0.004 | 8.9 % (7) | 32.5 % (13) | 0.001 |
| - Re-PCI CL | 5.5 % (4) | 0 % | ns | 10 % (8) | 0 % | 0.05 |
| CABG | 6.3 %(5) | 0 % | ns | 15 %(12) | 2.5 %(1) | 0.05 |
| MACE | 21 %(17) | 22 %(9) | ns | 35 %(28) | 35 %(14) | ns |
CABG coronary artery bypass graft, MACE major adverse cardiac events, MI myocardial infarction, PCI percutaneous coronary intervention
Our findings are in contrast with those of Hannan et al. [8], who showed a significantly lower 12-month mortality rate in patients undergoing staged multi-vessel (MV) PCI within 60 days after index procedure than patients undergoing culprit PCI only (1.3 % vs 3.3 %, p = 0.04). However, this was an observational study and revascularisation was not ischaemia driven, and therefore subject to selection bias. Our findings also differ from the HELP AMI study [9], in which the 1-year incidence of repeated revascularisation in 69 STEMI patients treated with primary PCI was similar in single and multi-vessel strategies. However, in this study the additional PCI was performed without ischaemia detection.
Our findings differ from a more recent randomised trial by Politi et al. [5] They showed that culprit vessel-only angioplasty was associated with the highest rate of long-term MACE compared with multi-vessel treatment. The patients scheduled for staged revascularisation (SR) experienced a similar rate of MACE compared with patients undergoing complete simultaneous (CR) treatment of non-culprit lesion. Politi et al. did not explain whether the patients in the culprit-only revascularisation group underwent routine non-invasive testing for ischaemia after discharge, as is currently advocated by the guidelines. Moreover, it is not clear in how many patients complete revascularisation in the CR or SR groups was actually achieved. Since about 30 % of STEMI patients with MVD have at least one chronic total occlusion, it is unlikely that complete revascularisation was achieved in all patients.
Our findings are in line with the recommendations of the most recent meta-analysis by Biondi-Zoccai et al. [10] in which 10 controlled clinical trials were included. They recommend multi-vessel revascularisation only in patients with features of instability or very high risk, deferring intervention and awaiting results of ischaemia-proving tests in most other subjects.
Our findings are also in line with a recent review paper by Widimsky et al. in which the authors proposed to treat only the IRA during the acute phase of STEMI [11]. The authors also proposed that the non-culprit arteries should be treated either medically or by staged revascularisation procedures. Our long-term follow-up supports the more conservative approach.
Our findings are also in line with the most recent meta-analysis by Vlaar et al. in which 14 studies with more than 40,000 patients were included [12]. They demonstrated that staged PCI was associated with lower short- and long-term mortality as compared with culprit PCI and MV-PCI and that MV-PCI was associated with highest mortality rates at both short- and long-term follow-up.
Our findings support the current guidelines [4, 13] to defer treatment of non-culprit lesions until about 6 weeks after hospital discharge if ischaemia is documented.
Strengths and limitations
The current study is a relatively small, single-centre trial which was stopped prematurely because of a slow inclusion rate, resulting in an inadequate power for primary endpoint. This study was not powered for secondary endpoints. Moreover, only 13 % of eligible patients were randomised which can lead to selection bias. The relative complexity of the study has led to a selection towards relatively more stable patients with relatively preserved LVEF and therefore low-risk patients. However, until now there are no other studies available that have investigated the effects of early ischaemia-driven additional revascularisation in a randomised design. Obviously there is a clear need for larger studies including higher-risk patients to confirm our findings.
In this study we chose 0.75 as FFR cut-off value whereas the FAME study used 0.80 as cut-off. At the time of the inclusion the FAME study had not yet been published. A 0.75 as FFR cut-off was chosen based on studies in the pre-FAME period.
In addition, patients with a chronic occlusion were excluded from the study to allow FFR measurements. It has been shown that patients with a remaining chronic occlusion after acute myocardial infarction form a subgroup at high risk for new cardiac events [14]. Other studies are underway to investigate the effects of additional revascularisation in this specific subgroup.
Conclusion
After 3 years of follow-up, FFR-guided additional revascularisation of non-culprit lesions early after primary PCI resulted in more deaths and/or re-infarctions compared with a more conservative strategy of ischaemia-guided revascularisation at a later stage. The conservative strategy did result in more additional PCI procedures compared with the invasive strategy. In terms of MACE, there were no differences between invasive versus conservative strategy throughout the follow-up period.
Conflict of interest
No conflict of interest, no funding
References
- 1.Hasdai D, Behar S, Wallentin L, et al. A prospective survey of the characteristics, treatments and outcomes of patients with acute coronary syndromes in Europe and Mediterranean basin. The Euro Heart survey of acute coronary syndromes. Eur Heart J. 2002;23:1190–201. doi: 10.1053/euhj.2002.3193. [DOI] [PubMed] [Google Scholar]
- 2.Sorajja P, Gersh BJ, Cox DA, et al. Impact of multivessel disease on reperfusion success and clinical outcomes in patients undergoing primary percutaneous coronary intervention for acute myocardial infarction. Eur Heart J. 2007;28:1709–16. doi: 10.1093/eurheartj/ehm184. [DOI] [PubMed] [Google Scholar]
- 3.Goldstein JA, Demetriou D, Grines CL, et al. Multiple complex coronary plaques in patients with acute myocardial infarction. N Engl J Med. 2000;343:915–22. doi: 10.1056/NEJM200009283431303. [DOI] [PubMed] [Google Scholar]
- 4.Werf F, Ardissino D, Betriu A, et al. Management of acute myocardial infarction in patients presenting with ST-segment elevation. The task force on the management of acute myocardial infarction of the European society of cardiology. Eur Heart J. 2003;24:28–66. doi: 10.1016/S0195-668X(02)00618-8. [DOI] [PubMed] [Google Scholar]
- 5.Politi L, Sgura F, Rossi R, et al. A randomized trial of target-vessel versus multi-vessel revascularisation in ST-elevation myocardial infarction: major adverse cardiac events during long-term follow-up. Heart. 2010;96:662–7. doi: 10.1136/hrt.2009.177162. [DOI] [PubMed] [Google Scholar]
- 6.Serruys PW, Unger F, Hout BA, et al. The ARTS study (Arterial Revascularization Therapies Study) Semin Interv Cardiol. 1999;4:209–19. doi: 10.1006/siic.1999.0107. [DOI] [PubMed] [Google Scholar]
- 7.Dambrink JHE, Debrauwere JP, Hof AWJ, et al. Non-culprit lesions detected during primary PCI: treat invasively or follow the guidelines? EuroIntervention. 2010;5:968–75. doi: 10.4244/EIJV5I8A162. [DOI] [PubMed] [Google Scholar]
- 8.Hannan EL, Samadashvili Z, Walford G, et al. Culprit vessel percutaneous coronary intervention versus multivessel and staged percutaneous coronary intervention for ST-segment elevation myocardial infarction patients with multivessel disease. JACC Cardiovasc Interv. 2010;3:22–31. doi: 10.1016/j.jcin.2009.10.017. [DOI] [PubMed] [Google Scholar]
- 9.Mario C, Mara S, Flavio A, et al. Single vs multivessel treatment during primary angioplasty: results of the multicentre randomised HEpacoat for cuLPrit or multivessel stenting for Acute Myocardial Infarction (HELP AMI) Study. Int J Cardiovasc Intervent. 2004;6:128–33. doi: 10.1080/14628840310030441. [DOI] [PubMed] [Google Scholar]
- 10.Biondi-Zoccai G, Lotrionte M, Sheiban I. Management of multivessel coronary disease after ST-elevation myocardial infarction treated by primary coronary angioplasty [Review] Am Heart J. 2010;160:S28–35. doi: 10.1016/j.ahj.2010.10.013. [DOI] [PubMed] [Google Scholar]
- 11.Widimsky P, Holmes DR. How to treat patients with ST-elevation acute myocardial infarction and multi-vessel disease? Eur Heart J. 2011;32:396–403. doi: 10.1093/eurheartj/ehq410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vlaar PJ, Mahmoud KD, Holmes DR, et al. Culprit vessel only versus multivessel and staged percutaneous coronary intervention for multivessel disease in patients presenting with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2011;58:692–703. doi: 10.1016/j.jacc.2011.03.046. [DOI] [PubMed] [Google Scholar]
- 13.Silber S, Albertsson P, Aviles FF, et al. Guidelines for percutaneous coronary interventions. The task force for percutaneous coronary interventions of the european society of cardiology. Eur Heart J. 2005;26:804–47. doi: 10.1093/eurheartj/ehi564. [DOI] [PubMed] [Google Scholar]
- 14.Schaaf RJ, Vis MM, Sjauw KD, et al. Impact of multivessel coronary disease on long-term mortality in patients with ST-elevation myocardial infarction is due to the presence of a chronic total occlusion. Am J Cardiol. 2006;98:1165–9. doi: 10.1016/j.amjcard.2006.06.010. [DOI] [PubMed] [Google Scholar]