Abstract
Background
Complementary and Alternative Medicine (CAM) use is on the rise in both the US and Europe, despite questions about its safety, effectiveness and lack of national standards. We aimed to determine the prevalence and predictors of CAM and integrative medicine use (CAM-I) and perceived effectiveness compared to the standard treatment of botulinum toxin injections in patients with adult-onset primary dystonia.
Methods
This was a retrospective questionnaire study of 389 dystonia patients examining the effects age, gender, education level and number of anatomical regions affected on botulinum toxin and CAM-I use and their perceived effectiveness.
Results
53% (208) of patients reported CAM-I use, while 90% (349) used the standard treatment (botulinum toxin), and 48% used both. Education was the only significant predictor of CAM-I use – individuals with bachelor’ s degrees were more likely to try CAM-I whereas those with high school diplomas were less likely. The mean effectiveness rate for botulinum toxin injections (59%) significantly exceeded that for and CAM-I (28%, p<0.0001).
Conclusions
Our work highlights the need for scientifically sound studies to determine the safety, effectiveness and expense of CAM-I treatments for dystonia and other neurological disorders given that CAM-I use is steadily increasing, there is great variability in what is classified as CAM-I, and the effectiveness of some modalities may be significantly less than conventional medical treatments.
Keywords: Dystonia, Complementary and Alternative Medicine (CAM), Botulinum toxin, Integrative medicine, Spasmodic dysphonia
1. Introduction
The National Center for Complementary and Alternative Medicine (NCCAM) “defines CAM [Complementary and Alternative Medicine] as a group of diverse medical and health care systems, practices, and products that are not generally considered part of conventional medicine [1].” This is a necessarily broad definition that applies to anything outside of the narrowly-defined confines of conventional medicine, provided by medical doctors (MDs). As their names suggest, complementary is used to denote “along with,” whereas alternative infers that the intervention is “oppositional to conventional medicine.” Integrative medicine is a combination of conventional medicine and CAM treatments with some scientific evidence for effectiveness and safety. The boundaries that separate conventional medicine from CAM are not always clear [1].
One group of disorders that could potentially benefit from CAM (and integrative) therapy (CAM-I) are the dystonias, disorders of the nervous system that cause uncontrollable muscle contractions, often of opposing muscles, and result in distorted, twisting motions, and abnormal postures [2]. Dystonia may be painful and not adequately controlled with conventional medical treatments such as oral pharmacotherapy, injections of botulinum toxin or deep brain stimulation. The vast majority of patients with dystonia cared for by movement disorders specialists have adult-onset primary focal (e.g., blepharospasm, cervical dystonia, spasmodic dysphonia) or segmental (e.g., craniocervical) dystonia. The currently accepted treatment option for these patients is injection of botulinum toxin into dystonic muscles, which usually commence once a patient’ s diagnosis is made or confirmed by a movement disorders specialist. However, more and more general practitioners are suggesting that patients try CAM-I treatments prior to sending them to see a specialist [3,4,5,6], thus delaying established symptomatic treatments. In addition, some patients do not respond well, stop responding, or do not fully respond to botulinum toxin injections [2,7], and pursue CAM-I treatments for relief of symptoms.
In this study, we analyzed self-reported questionnaire responses to establish the prevalence, predictors, and subjective effectiveness of botulinum toxin and CAM-I usage in patients with segmental and focal adult-onset primary dystonia. We also examine specific types of CAM-I therapies employed by this patient population.
2. Methods
2.1 Study subjects
Human studies were performed in accordance with institutional review board guidelines, and all subjects gave informed consent. Data was obtained from the Neurogenetic Biorepository at University of Tennessee Health Science Center (UTHSC). Demographic, phenotypic and clinical data was housed in a secure Oracle database with a web interface. Patients were acquired at UTHSC along with local, regional and national support group meetings. All patients were examined by a movement disorders specialist (M.S.L.) and clinically diagnosed and classified according to established guidelines. The questionnaires were completed in face-to-face meetings with the subject and supervised by the senior investigator (M.S.L.). Ambiguous responses were clarified at that time or, occasionally, through telephone contact by the senior investigator or clinical research coordinator at a later date.
All subjects with adult-onset primary focal or segmental dystonia and sufficient data were included in our study. Insufficient data was defined as lacking any of the main independent (gender, age, diagnosis, or education level) or dependent (use of botulinum toxin or CAM-I) variables. Subjects were selected for inclusion irrespective of gender, race, or ethnicity. Anatomical regions of involvement were derived from the Unified Dystonia Rating Scale [8] and included eyes and upper face (blepharospasm); lower face; jaw and tongue (oromandibular); larynx (spasmodic dysphonia); neck (cervical dystonia); and distal arm and hand [9]. Subjects reported treatment with (1) both CAM-I and standard botulinum toxin injections, (2) CAM-I only, (3) botulinum toxin injections only, or (4) neither.
2.2 Dystonia medical questionnaire
The dystonia medical questionnaire was designed to gather demographic details, medical history, prescription medication use, social history, employment history, education, family medical history, neurological and psychiatric history, and document abnormal findings on the neurological examination. Additional information was specific to dystonia: UDRS scores, sensory tricks, response to injections of botulinum toxin (bodily location, brand name, initial treatment date, final or most recent treatment date, average duration of benefit during most recent year of treatment, and maximal subjective percent improvement). CAM-I use was classified as “Dystonia Treatments: Other,” with headings for description of treatment, dates of treatment, and subjective percentage improvement in dystonia, for each body area. No further instructions were given for this section.
2.3 CAM-I Classification
The most common types of CAM-I were designated as general categories, whereas infrequently used but similar techniques were grouped into a common general category or into a category entitled “other.” The major CAM categories were acupuncture, biofeedback, chiropractic, exercise and massage therapy. Integrative categories included modalities which may be prescribed by MDs such as drops for dry eyes, physical therapy, speech therapy and tinted glasses.
2.4 Education Classification
Education was grouped into eight categories: did not graduate high school, high school graduate or GED equivalent, some college, associate’ s degree, bachelor’ s degree, graduate work, master’ s degree, or professional degree.
2.5 Statistical Analyses
SAS® 9.2 (Cary, NC, USA) was used for all statistical evaluations. The level of significance (α) was set at 0.05. First, we examined the prevalence of CAM-I and botulinum toxin usage in subjects with dystonia. All integrative treatments (e.g., physical therapy, speech therapy) were included in the CAM category for statistical analyses. The null hypotheses were defined as no differences in demographics between those who chose to use botulinum toxin or not nor between those who chose to use CAM-I treatments or not. Our dependent variable, use of CAM-I and/or botulinum toxin, was binary (0-no/1-yes). Differences in use of botulinum toxin verses CAM-I were examined with the χ2 statistic. In order to determine the effect of each independent variable (age, gender, education level, number of anatomical regions) on CAM-I and botulinum toxin usage we used a 2-sample t-test for the continuous variable age, Fisher’ s exact test for number of anatomical dystonia regions affected (given that some cells contained a very small number of subjects), the χ2 statistic for the binomial variable gender, logistic regression for education, and multiple logistic regression for the combined effect of age, number of anatomical regions, gender, and education level. Finally, a Fisher’ s exact test was used to assess the effect of gender on the number of CAM-I treatment types used by patients.
Next, we analyzed the maximal subjective percent improvement associated with CAM-I and botulinum toxin treatments using the null hypothesis that predictor variables (age, gender, education level, and number of anatomical regions) have no effect on perceived treatment effectiveness. We also used a one-sample t-test to compare the effectiveness of CAM-I versus botulinum toxin. Regression analysis was used to calculate the effect of age and number of anatomical regions on botulinum toxin effectiveness, and the effect of age, number of anatomical regions, and number of treatments on CAM-I effectiveness. Factorial ANOVAs were used to evaluate the effects of gender, education, and their interaction on the effectiveness of botulinum toxin and CAM-I. Finally, we describe the self-reported effectiveness of specific forms of CAM-I usage in subjects with dystonia, and associations among anatomical region of involvement and type of CAM-I usage.
3. Results
3.1 Demographics and prevalence
Table 1 presents demographic data on the 389 patients with dystonia extracted from the Neurogenetic Biorepository. As shown in Table 2, many patients used both botulinum toxin and CAM-I treatments, whereas others used botulinum toxin only, CAM-I only, or neither. Botulinum toxin usage had no effect on CAM-I usage (χ2 =0.02, df=1, p=0.90). Table 2 shows the percentages of botulinum toxin and CAM-I usage. Some type of CAM-I usage was reported by 208/398 patients (53%).
Table 1.
Patient Demographics
| Characteristics | Botulinum toxin use | CAM-I use | All patients | ||||
|---|---|---|---|---|---|---|---|
| No | Yes | p value | No | Yes | p value | Total | |
| Population, n (%) | 40 (10) | 349 (90) | NA | 181 (47) | 208 (53) | NA | 389 |
| Age, years | |||||||
| Mean SD | 61±14.3 | 59.9±11.8 | 0.5632a | 61.1 ±12.9 | 59 ±11.3 | 0.0821a | 60.0 ±12.1 |
| Gender, n (%) | 0.9190b | 0.4515b | |||||
| Male | 9 (2.3) | 81 (20.8) | NA | 45 (11.6) | 45 (11.6) | NA | 90 (23.1) |
| Female | 31 (8.0) | 268 (68.9) | NA | 136 (35.0) | 163 (41.9) | NA | 299 (76.9) |
| Education, n (%) | 33 | 296 | 0.9628c | 190 | 139 | 0.0002c | 329 |
| <HS diploma | 0 | 6 (1.8) | 0.9768c | 4 (1.2) | 2 (0.6) | 0.2842c | 6 (1.8) |
| High school/GED | 5 (1.5) | 38 (11.6) | 0.9537c | 29 (8.8) | 14 (4.3) | 0.0087c | 43 (13.1) |
| Some college | 8 (2.4) | 57 (17.4) | 0.9527c | 34 (10.4) | 31 (9.4) | 0.4139c | 65 (19.8) |
| Associate’s degree | 5 (1.5) | 30 (9.1) | 0.9501c | 15 (4.5) | 20 (6.1) | 0.6402c | 35 (10.6) |
| Bachelor’s degree | 7 (2.1) | 72 (21.9) | 0.9584c | 17 (5.2) | 62 (18.8) | <.0001c | 79 (24.0) |
| Some graduate | 0 | 10 (3.0) | 0.9703c | 5 (1.5) | 5 (1.5) | 0.8212c | 10 (3.0) |
| Master’s degree | 7 (2.2) | 60 (18.2) | 0.9556c | 26 (7.9) | 41 (12.5) | 0.2320c | 67 (20.4) |
| Professional degree | 1 (0.3) | 23 (7.0) | NA | 9 (2.7) | 15 (4.6) | NA | 24 (7.3) |
| Anatomical regions, n (%) | 40 | 349 | 0.6332d | 181 | 208 | 0.8138d | 389 |
| One | 31 (8.0) | 275 (70.9) | NA | 141 (36.3) | 165 (42.6) | NA | 306 (78.9) |
| Two | 5 (1.2) | 47 (12.0) | NA | 25 (6.4) | 27 (6.8) | NA | 52 (13.2) |
| Three | 4 1(.0) | 21 (5.4) | NA | 11 (2.8) | 14 (3.6) | NA | 25 (6.4) |
| Four | 0 | 6 (1.5) | NA | 4 (1.0) | 2 (0.5) | NA | 6 (1.5) |
| Type of dystonia | 389 | ||||||
| Eyes/upper face | 2 (0.5) | 35 (9.0) | NA | 25 (6.4) | 12 (3.1) | NA | 37 (9.5) |
| Neck | 11 (2.8) | 90 (23.2) | NA | 35 (9.0) | 66 (17.0) | NA | 101 (26.0) |
| Larynx | 10 (2.6) | 135 (34.7) | NA | 63 (16.2) | 82 (21.1) | NA | 145 (37.3) |
| Segmental craniocervical | 7 (1.8) | 72 (18.5) | NA | 43 (11.0) | 36 (9.3) | NA | 79 (20.3) |
| Hand-forearm | 7 (1.8) | 9 (2.3) | NA | 11 (2.8) | 5 (1.3) | NA | 16 (4.1) |
| Other segmental | 1 (0.2) | 0 | NA | 0 | 1 (0.2) | NA | 1 (0.2) |
| Other dystonia | 2 (0.5) | 8 (2.1) | NA | 4 (1.0) | 6 (1.6) | NA | 10 (2.6) |
t test.
Chi-squared test.
Logistic regression comparing use by those with professional degrees versus other education levels.
Fisher’s exact test. Abbreviations: SD, standard deviation; HS, high school; GED, general education degree; NA, not applicable.
Bold = p <.05.
Table 2.
Botulinum Toxin and CAM-I Use
| No botulinum toxin | Botulinum toxin | Total | |
|---|---|---|---|
| CAM-I, n (%) | 19 (5) | 162 (42) | 181 (47) |
| No CAM-I | 21 (5) | 187 (48) | 208 (53) |
| Total | 40 (10) | 349 (90) | 389 (100) |
Each cell includes the number of subjects and the percent: n (%).
Age had no effect on either botulinum toxin (t=0.58, p=0.56) or CAM-I (t=1.74, p=0.08) usage. Although our population was skewed toward females, there was no effect of gender on either botulinum toxin (χ2 = 0.01, df = 1, p = 0.92) or CAM-I (χ2 = 0.57, df = 1, p = 0.45) usage.
Of the 208 subjects using CAM-I, 134 used one type of CAM-I treatment, 40 tried two types, and 34 tried three or more. The maximum reported number of different CAM-I treatments was 6. Table 3 shows the number of CAM-I treatments broken down by gender and number of affected anatomical regions. There were no significant effects of gender or number of affected anatomical regions on the number of CAM-I treatments employed by subjects (FISHERS = 0.00, df = 1, p= 0.52).
Table 3.
CAM-I Treatments by Gender and Number of Anatomical Regions
| Number of treatment types, n (%) |
Female | Male | Number of Number of treatment Anatomical Regions |
|||
|---|---|---|---|---|---|---|
| One | Two | Three | Four | |||
| 0 | 136 (35.0) | 45 (11.6) | 141 (36.3) | 24 (6.2) | 11 (2.8) | 4 (1.0) |
| 1 | 103 (26.5) | 31 (8.0) | 111 (28.6) | 14 (3.6) | 7 (1.8) | 2 (0.5) |
| 2 | 31 (0.8) | 9 (2.3) | 29 (7.5) | 9 (2.3) | 2 (0.5) | 0 |
| 3 | 15 (3.8) | 3 (0.8) | 15 (3.9) | 1 (0.3) | 2 (0.5) | 0 |
| 4 | 12 (3.1) | 1 (0.2) | 8 (2.1) | 3 (0.8) | 2 (0.5) | 0 |
| 5 | 2 (0.5) | 0 | 1 (0.3) | 0 | 1 (0.3) | 0 |
| 6 | 0 | 1 (0.2) | 1 (0.3) | 0 | 0 | 0 |
| Total | 299 (76.9) | 90 (23.1) | 306 (78.9) | 51 (13.2) | 25 (6.4) | 6 (1.5) |
Each cell includes the number of subjects and percentage: n (%).
The number of anatomical regions affected made no difference on botulinum toxin (FISHERS = 0.015, df = 3, p = 0.63) or CAM-I usage (FISHERS = 0.0038, df = 3, p = 0.81). The relationship between education and botulinum toxin was not significant (Wald χ2 = 1.94, df = 7, p = 0.96), but the relationship between education and CAM-I usage was significant (Wald χ2 = 27.81, df = 7, p = 0.0002). The overall effect of age, number of anatomical regions affected, gender, and education was non-significant for botulinum toxin (Wald χ2 = 2.34, df = 4, p = 0.67), but was significant for CAM-I usage (Wald χ2 = 14.47, df = 4, p = 0.0059). However, education was the only significant individual predictor (Wald χ2 = 11.62, df = 1, p = 0.0007) of CAM-I use. Patients with bachelor’ s degrees (p < 0.0001, odds ratio [OR] = 2.19, 95% confidence interval [CI; 0.82, 5.86]) were more likely to try CAM-I treatments, whereas those with high school diplomas (p = 0.0087, OR = 0.290, 95% CI [0.102, 0.823]) were less likely to try CAM-I treatments as compared to those with professional degrees.
3.2 Perceived effectiveness
Responses regarding the effectiveness of botulinum toxin injections were available from 310 out of 349 subjects reporting use of botulinum toxin. The mean overall effectiveness of botulinum toxin was 59%. CAM-I perceived effectiveness had 173 responses out of 208 patients reporting CAM-I therapy and the mean effectiveness was 28%. The difference between these percentages was highly significant (t = 13.2, p < 0.0001).
With multiple linear regression, we found no significant effect of age and number of affected anatomical regions on the effectiveness of botulinum toxin (F = 1.21, df = 2, p = 0.29), whereas the overall effect of age, number of affected anatomical regions, and number of CAM-I treatments on CAM-I effectiveness was highly significant (F = 9.44, df = 3, p < 0.0001). Post-hoc analysis showed that the number of CAM-I treatments was the only important predictor of CAM-I effectiveness (t = 5.23, df = 1, p < 0.0001). The average effectiveness of CAM-I interventions increased by 11.2% with each additional CAM-I treatment used by subjects with dystonia.
Factorial ANOVAs were used to examine the effects of gender and education on the effectiveness of botulinum toxin injections and CAM-I. The overall effect of gender and education on CAM-I was non-significant (F = 1.04, p = 0.42). In contrast, the overall effect of gender and education on the effectiveness of botulinum toxin was highly significant (F = 2.36, df = 14, p = 0.0043). Post-hoc analyses showed that education (F = 2.94, df = 7, p = 0.0056) had a greater effect than gender (F = 4.09, df = 1, p = 0.0442). The interaction between age and education did not reach statistical significance (F = 1.95, df = 6, p = 0.073). Injections of botulinum toxin tended to show more subjective effectiveness in females, whereas men with some graduate work reported significantly lower effectiveness.
3.3 Types of CAM and integrative treatments
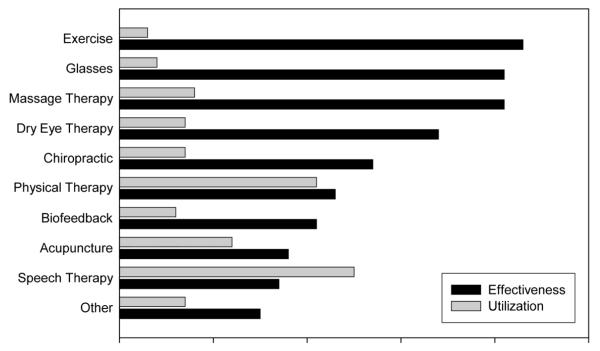
For subjective effectiveness, there were 272 responses for a total of 335 treatments among our cohort. The average effectiveness rate for individual CAM-I treatments was 24% in comparison to the overall 28% CAM-I effectiveness reported by patients. Fig. 1 shows the types of CAM-I utilized by patients with dystonia along with the average subjective effectiveness of each. Although exercise was only used by 9 patients, its average effectiveness was the highest at 43% (range 0-75%, median 50%). Next, in order of effectiveness, were glasses (mean 41%, range 0-90%, median 40%, n = 10), massage therapy (mean 41%, range 0-100%, median 35%, n = 21), dry eye therapy (mean 34%, range 0-100%, median 15%, n = 18), chiropractic (mean 27%, range 0-100%, median 17.5%, n = 20), physical therapy (mean 23%, range 0-100%, median 10%, n = 58), biofeedback (mean 21%, range 0-100%, median 10%, n = 15), and acupuncture (mean 18%, range 0-80%, median 0%, n = 33). Speech therapy, used specifically by patients with spasmodic dysphonia, was tried by the largest number of patients, yet had the lowest effectiveness (17%) shown among the major categories of CAM-I (range 0-100%, median 5%, n = 69).
Fig. 1.
Effectiveness and utilization of CAM-I modalities.
3.4 Types of CAM-I use by anatomical regions of involvement
For anatomical regions of involvement, 125 patients were diagnosed with blepharospasm, 235 with cervical dystonia, 75 with oromandibular dystonia, 217 with spasmodic dysphonia, and 28 with distal arm and hand dystonia. Patients with focal or segmental dystonia were categorized into each anatomical region affected, thereby providing a total of 680 regions for inclusion in the analysis of CAM-I types by region of involvement. Dry eye treatments and tinted glasses were used by 19% and 14% of blepharospasm patients, respectively. Cervical dystonia patients were more likely to try physical therapy (27%) than any other treatment. Speech therapy was used by 34% of subjects with spasmodic dysphonia. Individuals with distal arm and hand dystonia were more likely to try physical therapy than other types of CAM-I treatments.
4. Discussion
Our results show that over half of a US study population (53%) tried at least one CAM-I form of therapy at some point in their search for relief of dystonia symptoms. One individual tried six different types of CAM-I therapies. In our US cohort, the most commonly used CAM-I modalities were speech therapy, physical therapy, acupuncture and massage therapy. The overall average perceived subjective effectiveness of individual CAM-I treatments was 24%, with some therapies such as exercise, tinted glasses, and massage showing effectiveness rates in excess of 40%. Among 180 members of the German Dystonia society, acupuncture, relaxation techniques, homeopathy and massages were the most frequently used CAM options [3].
As expected, the majority of our population (90%) used the standard treatment of botulinum toxin injections. However, nearly half (48%) of the patients used both botulinum toxin and CAM-I therapies. Unfortunately, our dataset did not permit us to determine temporal relationships among CAM-I usage and botulinum toxin injections.
The limitations of our retrospective questionnaire-based study are readily recognized. Then again, it may be difficult to design a controlled trial assessing particular CAM-I modalities due to the individualized nature of these interventions and their practitioners [8]. In this study, we used data from a questionnaire that queried the use and percent effectiveness of each CAM-I and botulinum toxin treatment with 0% denoting absolutely no benefit and 100% corresponding to complete relief of all signs and symptoms. Our sample might not accurately represent the entire dystonia population since patients attending support group meetings may not have obtained adequate control of their dystonia with standard medical interventions and/or CAM-I. Furthermore, self-reported studies always have the possibility of recall bias and subjects may overstate the effectiveness of medical interventions to avoid offending their treating physician.
Other confounds should be considered when examining our results. For instance, 90% of the patients in this study received injections of botulinum toxin, which could increase the perceived effectiveness of CAM-I if both were being used simultaneously. Another potential limitation of our approach was the lumping of specific types of CAM-I treatments in larger groups that could employ highly variable individual techniques. To adequately power our analyses, different anatomical variants of adult-onset dystonia were also grouped together, which limits our ability to determine which anatomical subtypes are more conducive to injections of botulinum toxin or certain CAM-I treatments.
CAM medicine, or therapy, is becoming an increasingly popular treatment option for a variety of medical disorders [3,4,10]. Several studies show that its use is on the rise in both the US and Europe with a relatively high rate of CAM use among patients with chronic symptoms such as dystonia [3]. In some cases, primary care physicians suggest that patients try CAM treatments prior to sending them to a specialist for evaluation whereas some patients are not satisfied with symptomatic relief and seek out CAM for potential cures [2,11]. Our study showed just over half of the cohort used CAM. According to the National Health Interview Survey in 2007, CAM is used by 38% of Americans [1].
Doubts remain within the established medical community about the overall effectiveness of CAM, as there are still few conclusive, well-designed clinical trials that show CAM treatments to be generally effective [1,12,13]. Despite this lack of evidence, health insurance companies are now including some of these modalities as covered treatments [10,12,14]. According to CAM practitioners, traditional studies do not accurately reflect CAM effectiveness due to the specificity and personalization required in CAM medicine. Oftentimes, patients try several CAM therapies to determine which, if any, result in improvement. In addition, many practitioners regard perceived subjective effectiveness as more beneficial information than the results of traditional clinical trials [11], which is a subject that NCCAM is seeking to address by encouraging scientifically acceptable studies to evaluate evidence for the effectiveness, safety, and correct application of individual CAM modalities. One issue to overcome is the overt lack of nationwide standards related to CAM. In particular, there are no national standards for certifying CAM practitioners or what qualifies as a specific therapy [1]. Similarly, the Consortium of Academic Health Centers for Integrative Medicine is seeking to create “a seamless integration of effective complementary and conventional approaches to promote healing and health in every individual and community [15].” This consortium is made up of 51 academic health centers and institutions with a common goal to share ideas, increase academia’ s curricula, research, and clinical care related to integrative medicine, and inform others on research that supports the use of integrative medicine [15].
Some studies have shown that a greater percentage of females than males use CAM [14,16], but in our study, gender did not exert a significant impact on CAM-I usage. Age and number of affected anatomical regions also showed no effect on CAM-I or botulinum toxin use. Education level did have an effect on CAM-I usage, but not on botulinum toxin usage. Patients with a bachelor’ s degree were more likely to use CAM-I treatments, and those with a high school diploma were less likely to use CAM-I treatments when compared to individuals with professional degrees.
Regarding the perceived effectiveness of botulinum toxin and CAM-I, there was no effect of age or number of anatomical segments. However, the number of CAM-I treatments tried was a highly significant predictor of CAM’ s effectiveness, which could help support the argument of CAM practitioners regarding the specific and personal nature of CAM therapies. It could be argued that those trying multiple therapies experienced a higher level of effectiveness once they found a specific treatment that worked for them. One such example in our study was a patient who reported three different CAM-I treatments with subjective percentage effectiveness rates of 30%, 50%, and 70%.
Certain forms of focal dystonia utilized some very specific CAM-I therapies, such as tinted glasses and dry eye therapy in subjects with blepharospasm, and speech therapy in individuals with spasmodic dysphonia. Exercise appeared to have the greatest effectiveness, but the sample size was small, and, as with many CAM-I modalities, the exercise category is broad and includes modalities such as yoga, distance running, aerobic classes, and strength training.
5. Conclusions
The front-line treatment for focal and segmental dystonia, botulinum toxin, is an effective symptomatic treatment that generally lasts 2-4 months in duration before another injection session is required. Patients who cannot tolerate botulinum toxin, do not respond to it, or cannot afford to pay for treatments every 2-4 months continue to look for alternatives. Even those individuals who do tolerate and respond to injections of botulinum may not consistently respond to a satisfactory degree. It is possible that these patients may also seek CAM-I treatments to supplement the effects of botulinum toxin injections [2,18].
Patients with high school diplomas are less likely to try CAM-I therapies than those with bachelor’ s or professional degrees. This could be due to the technical abilities of educated patients to research CAM-I modalities and pursuing treatment modalities without relying on physician referrals. However, patients with bachelor’ s degrees are more likely to try CAM-I therapies than those with professional degrees. Another possibility for the difference between those with high school diplomas versus those with professional degrees could be due to socioeconomic status as well as insurance coverage. Those with greater incomes and better insurance coverage would be more likely to be able to seek out their own types of treatment.
Some insurance companies are now covering limited CAM therapies depending on diagnosis or doctor referral [10]. Due to the high level of CAM usage, as well as the high cost of therapies, it is imperative that scientific studies determine the safety, effectiveness, and expense of these treatments. Randomized controlled clinical trials are needed to specifically address the utility of CAM-I treatments, either as standalone therapy or in combination with standard medical interventions such as injection of botulinum toxin. For most of these interventional studies, specific types of focal dystonia must be targeted since this can greatly affect the practical application of certain types of CAM-I modalities as well as the overall effectiveness of CAM-I treatments [13].
Acknowledgements
This study was supported by the Neuroscience Institute at the University of Tennessee Health Science Center (M.S.L.), Dystonia Medical Research Foundation (M.S.L.), NIH grants R01NS048458 and R01NS069936 (M.S.L.), NIH U54 Dystonia Coalition (1U54NS065701) Pilot Projects Program (M.S.L.), and the Parkinson’s & Movement Disorder Foundation (M.S.L.).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].Harlan WR., Jr. New opportunities and proven approaches in complementary and alternative medicine research at the National Institutes of Health. J Altern Complement Med. 2001;7(Suppl 1):S53–9. doi: 10.1089/107555301753393814. [DOI] [PubMed] [Google Scholar]
- [2].Jankovic J. Treatment of dystonia. Lancet Neurol. 2006;5:864–72. doi: 10.1016/S1474-4422(06)70574-9. [DOI] [PubMed] [Google Scholar]
- [3].Junker J, Oberwittler C, Jackson D, Berger K. Utilization and perceived effectiveness of complementary and alternative medicine in patients with dystonia. Mov Disord. 2004;19:158–61. doi: 10.1002/mds.10684. [DOI] [PubMed] [Google Scholar]
- [4].Flannery MA, Love MM, Pearce KA, Luan JJ, Elder WG. Communication about complementary and alternative medicine: perspectives of primary care clinicians. Altern Ther Health Med. 2006;12:56–63. [PubMed] [Google Scholar]
- [5].Tilburt JC, Curlin FA, Kaptchuk TJ, Clarridge B, Bolcic-Jankovic D, Emanuel EJ, et al. Alternative medicine research in clinical practice: a US national survey. Arch Intern Med. 2009;169:670–7. doi: 10.1001/archinternmed.2009.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Ben-Arye E, Frenkel M, Klein A, Scharf M. Attitudes toward integration of complementary and alternative medicine in primary care: Perspectives of patients, physicians and complementary practitioners. Patient Educ Couns. 2008;70:395–402. doi: 10.1016/j.pec.2007.11.019. [DOI] [PubMed] [Google Scholar]
- [7].Cloud LJ, Jinnah HA. Treatment strategies for dystonia. Expert Opin Pharmacother. 2010;11:5–15. doi: 10.1517/14656560903426171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Comella CL, Leurgans S, Wuu J, Stebbins GT, Chmura T, Dystonia Study Group Rating scales for dystonia: a multicenter assessment. Mov Disord. 2003;18:303–12. doi: 10.1002/mds.10377. [DOI] [PubMed] [Google Scholar]
- [9].Fahn S. Classification of movement disorders. Mov Disord. 2011;26:947–57. doi: 10.1002/mds.23759. [DOI] [PubMed] [Google Scholar]
- [10].Pelletier KR, Marie A, Krasner M, Haskell WL. Current trends in the integration and reimbursement of complementary and alternative medicine by manage care, insurance carriers, and hospital providers. Am J Health Promot. 1997;12:112–22. doi: 10.4278/0890-1171-12.2.112. [DOI] [PubMed] [Google Scholar]
- [11].Carrick FR. The treatment of cervical dystonia by manipulation of the cervical spine: A study of brain hemisphericity, patient attributes and dystonia characteristics. Int J Appl Kinesiology Kinesiological Med. 2001;10:20–36. [Google Scholar]
- [12].Frenkel MA, Borkan JM. An approach for integrating complementary-alternative medicine into primary care. Fam Pract. 2003;20:324–32. doi: 10.1093/fampra/cmg315. [DOI] [PubMed] [Google Scholar]
- [13].Delnooz CC, Horstink MW, Tijssen MA, van de Warrenburg BP. Paramedical treatment in primary dystonia: a systematic review. Mov Disord. 2009;24:2187–98. doi: 10.1002/mds.22608. [DOI] [PubMed] [Google Scholar]
- [14].Gray CM, Tam AW, Pronk NP, O’ Connor PJ. Complementary and alternative medicine use among health plan members. A cross-sectional survey. Eff Clin Pract. 2002;5:17–22. [PubMed] [Google Scholar]
- [15].Elder WG, Hustedde C, Rakel D, Joyce J. CAM curriculum activities to enhance professionalism training in medical schools. Complement Health Pract Rev. 2008;13:127–133. doi: 10.1177/1533210107313917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Tindle HA, Davis RB, Phillips RS, Eisenberg DM. Trends in use of complementary and alternative medicine by US adults: 1997-2002. Altern Ther Health Med. 2005;11:42–9. [PubMed] [Google Scholar]
- [17].Defazio G, Berardelli A, Hallet M. Do primary adult-onset focal dystonias share aetiological factors? Brain. 2007;130:1183–93. doi: 10.1093/brain/awl355. [DOI] [PubMed] [Google Scholar]
- [18].Kartha N. Therapeutic challenges in dystonia. Neurol Clin. 2010;28:927–40. doi: 10.1016/j.ncl.2010.03.020. [DOI] [PubMed] [Google Scholar]
- [19].LeDoux MS. Meige syndrome: what’ s in a name? Parkinsonism Relat Disord. 2009;15:483–9. doi: 10.1016/j.parkreldis.2009.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Tisch SH, Brake HM, Law M, Cole IE, Darveniza P. Spasmodic dysphonia: clinical features and effects of botulinum toxin therapy in 169 patients-an Australian experience. J Clin Neurosci. 2003;10:434–8. doi: 10.1016/s0967-5868(03)00020-1. [DOI] [PubMed] [Google Scholar]
- [21].Adam OR, Jankovic J. Treatment of dystonia. Parkinsonism Relat Disord. 2007;13(Suppl 3):S362–8. doi: 10.1016/S1353-8020(08)70031-2. [DOI] [PubMed] [Google Scholar]