Abstract
Objectives
The effects of sleep-disordered breathing, sleep restriction, dyssomnias, and parasomnias on daytime behavior in children have been previously assessed. However, the potential relationship(s) between sleep hygiene and children’s daytime behavior remain to be explored. The primary goal of this study was to investigate the relationship between sleep hygiene and problematic behaviors in non-snoring and habitually snoring children.
Methods
Parents of 100 5- to 8-year-old children who were reported to snore “frequently” to “almost always,” and of 71 age-, gender-, and ethnicity-matched children who were reported to never snore participated in this study. As part of a larger, ongoing study, children underwent nocturnal polysomnography and parents were asked to complete the Children’s Sleep Hygiene Scale (CSHS) and the Conners’ Parent Rating Scales-Revised (CPRS-R:L).
Results
In the snoring group, strong negative correlations (r = −.39, p <.001) between the CSHS overall sleep hygiene score and the CPRS-R:L DSM-IV total scores emerged. Additionally, several subscales of the CSHS and CPRS-R:L were significantly correlated (p-values from <.000 to .004) in snoring children. No significant correlations were observed between the CSHS and the CPRS-R:L in the non-snoring children.
Conclusions
Parental reports of behavioral patterns in snoring children indicate that poorer sleep hygiene is more likely to be associated with behavior problems, including hyperactivity, impulsivity, and oppositional behavior. In contrast, no significant relationships between sleep hygiene and problem behaviors emerged among non-snoring children. These results indicate that children at risk for sleep disordered breathing are susceptible to daytime behavior impairments when concurrently coupled with poor sleep hygiene practices.
Keywords: sleep hygiene, behavior problems, children, snoring
Introduction
Impact of Sleep Loss
Sleep disorders have been shown to be related to daytime behavioral consequences in children. Children who were sleep restricted and those with sleep-disordered breathing (SDB), dysomnias, and parasomnias have been shown to experience substantial impact on daily functioning in health, mood, behavior regulation, academic performance, and quality of life [1–3]. Furthermore, sleep disturbances in pre-adolescent children are strongly related to psychological and medical problems, including respiratory illnesses, epilepsy, and otitis media [4], and parental reports suggest a relationship between sleep disorders and common child psychiatric disorders, such as Attention-Deficit/Hyperactivity Disorder (ADHD) [5,6] and childhood depression and anxiety [7]
The negative consequences of sleep-disordered breathing (SDB) on daytime and general cognitive functioning have been the focus of much research [8–12]. Researchers have noted that children who have SDB often present with clinical sequelae, such as cardiopulmonary complications in those with severe cardiovascular (?) disease [13] to more subtle daytime symptoms, including affect changes, attention and memory deficits, impairments in academic performance, and behavioral issues, such as hyperactivity and poor impulse control [8,10–12,14–16]. Owens and colleagues [17] reviewed medical records of children aged three to 18 to assess which risk factors were most strongly associated with adverse neurobehavioral outcomes in children referred for suspected SDB. Children who had SDB with a co-morbid sleep disorder were significantly more likely to have a history of behavioral, emotional, or academic problems, an ADHD diagnosis, and significantly higher externalizing (e.g., overtly manifested behaviors such as hyperactivity and oppositionality) and internalizing (e.g., unobservable feelings such as depression and anxiety) scores on various measures. They also found that insufficient sleep or sleep disruption associated with co-morbid sleep problems may lead to increased behavioral morbidity. A number of studies have indicated that children with insufficient, fragmented, or poor-quality sleep have increased impulsivity, hyperactivity, and aggression, as well as problems with mood, academic performance, and neurocognitive functioning [18–21].
Sleep Hygiene
Sleep hygiene is defined by the International Classification of Sleep Disorders [22] as the conditions and practices that promote circadian rhythm-appropriate, continuous, and effective sleep. This includes the establishment of a regular bedtime and wake time; adequate time in bed for sustained and adequate sleep; restriction of alcohol and caffeinated beverages before bedtime; and proper use of exercise, nutrition, and environmental factors that enhance restful sleep [22]. Two categories of behaviors contribute to inadequate sleep hygiene: (a) behaviors that lead to increased arousal, such as drinking caffeinated beverages and exercising late in the evening, and (b) behaviors that disrupt patterns of sleep, such as having the television on in the bedroom during sleep time. Inadequate sleep hygiene may be an important underlying contributor to sleep disorders and poor sleep [23].
Poor sleep hygiene practices can substantially affect daily functioning in many areas, including health, mood, behavior regulation, academic performance, and overall quality of life [24]. Those with inadequate sleep hygiene may present with insomnia, delayed sleep onset, nighttime awakenings, and early morning awakenings. As with other sleep problems, inadequate sleep hygiene can interfere with daily functioning, resulting in secondary mood and behavior changes, excessive daytime sleepiness, fatigue, cognitive impairment, poor concentration and attention, and caffeine use [24].
Purpose of the Present Study
Unfortunately, research on sleep hygiene has focused primarily on adolescents and adults [25,26]. Few studies have focused on sleep hygiene and behavior problems in younger children. Because children who experience inadequate sleep may present with excessive daytime sleepiness and attention problems and may be at risk for learning difficulties and affective regulation/behavior problems, this study investigated the potential relationship between poor sleep hygiene and problematic daytime behavior in young children [10,27–29]. Children with SDB or snoring are at a greater risk for behavioral and neurocognitive problems than children who do not snore [9,19]. Poor sleep hygiene is an additional factor that could contribute to similar difficulties in learning and behavior. Consequently, children who snore and have inadequate sleep hygiene may experience increased susceptibility to daytime problems in attention, as well as in behavioral and affective regulation in comparison to non-snoring children.
Based on aforementioned considerations and assumptions, our hypothesis was that snoring children who have poor sleep hygiene, as measured by the Children’s Sleep Hygiene Scale (CSHS)30, would exhibit more externalizing and internalizing behavior problems, as measured by the Conners’ Parent Rating Scale, Revised: Long Version (CPRS-R:L)314, than snoring children who do not have poor sleep hygiene. The comparison group of non-snoring children allowed for a more thorough analysis of problematic behaviors and sleep hygiene in children with no reported sleep difficulties.
Methods
Participants
Data collection was completed in100 snoring children and 71 non-snoring children, ages four to eight years, who were recruited for larger ongoing research studies at Kosair Children’s Hospital Sleep Medicine Center, and were matched for age, gender, and ethnicity. Recruitment for these larger studies was completed through a previously validated sleep questionnaire [8,32] mailed to participants through three Kentucky public school districts. The child’s guardian completed the questionnaire and returned it by mail to Kosair Children’s Sleep Medicine Research Center. The questionnaires were then examined for inclusion and exclusion criteria.
To qualify for the larger study examining snoring, children were rated as snoring “frequently” to “almost always” by their guardians and did not have any medical or psychiatric diagnoses. Children in the comparison group were rated to snore “never” and were excluded if they had any chronic medical conditions, craniofacial disorders, or if they were obese. The habitually snoring group composition was as follows: 49 females and 51 males, 50% of whom were White Non-Hispanic and 42% were African-American, and with a mean age of 6.85 (± 0.7) years. In the control group there were 37 males and 34 females. The mean age was 6.92 (± 1.15) years, 90.1% were White Non Hispanic, 7.1% were African American, and 2.8% were of “other” ethnicity.
Procedure
The children who were recruited as part of the larger study underwent a nocturnal polysomnography study (NPSG) at Kosair Children’s Hospital Sleep Medicine Center for evaluation of suspected SDB. Upon arrival to the Sleep Medicine Center, informed consent, subject assent, and HIPAA authorization forms were signed. After completion of the NPSG, the parent/guardian was asked to complete the CPRS-R: L [31] and the CSHS [30]. This study was approved by the University of Louisville Institutional Review Board and the Norton Healthcare Research Office.
Measures
The CPRS-R: L [31], is an 80-item comprehensive checklist for acquiring parental reports of behavior over the past month for children three through17 years. The items are rated on a scale of zero to three, indicating never, sometimes, almost always, or always. Scoring of the CPRS-R:L provides a total of 14 subscales, which are outlined in Table 1 [34]. Scores are represented as T-scores (Mean = 50; SD = 10) with higher scores indicating more problematic behaviors.
Table 1.
Mean Scores for both groups on the CPRS-R:L
| CPRS-R:L Scales | Mean T- Scores ± Standard Deviation Snoring Children* | Mean T- Scores ± Standard Deviation Non-Snoring Children |
|---|---|---|
| Oppositional | 55.4 ± 12.0 | 47.4 ± 8.1 |
| Cognitive Problems/Inattention | 58.0 ± 11.5 | 48.0 ± 6.4 |
| Hyperactivity | 58.1 ± 11.6 | 48.7 ± 6.1 |
| Anxious-Shy | 55.7 ± 12.0 | 45.5 ± 7.2 |
| Perfectionism | 51.0 ± 9.8 | 46.5 ± 7. 1 |
| Social Problems | 52.3 ± 10.8 | 47.1 ± 3.5 |
| Psychosomatic Symptoms | 57.2 ± 13.1 | 48.8 ± 7.0 |
| ADHD Index | 58.2 ± 11.9 | 47.1 ± 7.1 |
| CGI: Restless-Impulsive | 59.2 ± 12.9 | 46.9 ± 7.8 |
| CGI: Emotional Lability | 54.0 ± 12.8 | 44.9 ± 7.6 |
| Global Score | 57.3 ± 11.8 | 45.8 ± 7.6 |
| DSM-IV Inattentive | 56.5 ± 12.0 | 47.3 ± 7.1 |
| DSM-IV Hyperactive-Impulsive | 59.3 ± 12.4 | 49.5 ± 6.5 |
| DSM-IV Total | 59.3 ± 12.5 | 48.2 ± 7.4 |
All t-scores, p<.003
The CSHS [30] is a 22-item parent-report measure assessing sleep-facilitating and sleep-inhibiting practices of children ages two to 12 years. Parents report how often sleep-related behaviors have occurred during the past month along a six point scale (“always,” “frequently-if not always,” “quite often,” “sometimes,” “once in a while,” and “never”). The CSHS provides scores in six domains that include Physiological (e.g., consumption of food/beverage; roughhousing play before bed), Emotional (e.g., worried/upset), Cognitive (e.g., stimulating activities prior to/in bed), Environmental (e.g., light, temperature, and noise in bedroom), Bedtime Routine (e.g., relaxing and consistent schedule), and Sleep Stability (e.g., using the bed for sleep); and one total scale score, with higher scores indicating better sleep hygiene. While higher scores indicate better sleep hygiene, no clinical cut-off scores have been established to indicate clinically significant poor sleep hygiene. Initial computation of reliability (Cronbach’s alpha) yielded a value of α = 0.74 – 0.76 for all items [33]. Although this scale requires further studies to establish reliability and validity, it provided for the needs of this study through appropriate age norms and item selection.
Data Analysis
Bivariate correlations were computed using SPSS software to determine associations between the behavioral scales and the sleep hygiene measure. Each of the subscales of the CPRS-R:L were independently compared to each subscale on the CSHS. Due to the large number of correlations, the determination of statistical significance was set at p < 0.01. Additionally, group differences between genders and between ethnicity (Caucasian vs. non-Caucasian) in sleep hygiene total scores were examined using t-tests. Independent samples t-tests were used to examine differences in overall sleep hygiene, as measured by the CSHS, based on gender, ethnicity (Caucasian vs. non-Caucasian), and diagnosis (snoring vs. non-snoring). A Bonferroni Correction [34] was employed because of the number of t-tests involved and the adjusted significance level was set at p < 0.003. In addition to the underlying hypothesis positing a direct relationship between sleep hygiene and behavioral ratings, the mediating effect of snoring was analyzed via a mediation model [35]. Structural Equation Modeling was conducted using Amos 18 (Amos Development Corporation, FL). All models were fitted through Maximum Likelihood Estimation, bootstrapping, and 95% bias-corrected confidence intervals. This analysis aimed to further clarify the potential relationships between sleep hygiene and behavioral ratings.
Results
Between-Group Differences
No significant differences in sleep hygiene scores were noted for gender, ethnicity, or diagnostic groups. An independent samples t-test (p < .003) was also used to examine the difference in behavior problems on the (CPRS-R:L) between snoring and non-snoring children. The children in the snoring group generated significantly higher scores on all scales than the non-snoring children (see Table 1). Several subscales on the CPRS-R indicated mean scores in the nearly clinically significant range for the snoring group. In particular, CGI Restless-Impulsive, DSM-IV Hyperactive-Impulsive, and DSM-IV Total all had mean T-scores of 59, representing nearly one standard deviation above the population mean scores.
Snoring Children: Externalizing Symptoms
In snoring children, strong negative correlations occurred between the CSHS overall Sleep Hygiene score and CPRS-R:L DSM-IV total scores (r = −.39, p < .001) indicating that as sleep hygiene declined, problematic behaviors increased (see Table 2). The CSHS Total scale was also negatively correlated with the CPRS-R:L Global Index, Hyperactivity, DSM-IV Hyperactivity-Impulsivity, Oppositional Problems, and ADHD Index. Significant correlations were found between the CSHS Physiological scale and the CPRS-R:L Global Index, Hyperactivity, Restlessness-Impulsive, DSM-IV Hyperactivity-Impulsivity, DSM-IV total, and Oppositional Problems scales. Furthermore, the CSHS Cognitive scale was negatively correlated with the CPRS-R:L DSM-IV Hyperactivity-Impulsivity, DSM-IV Total, Global Index, Hyperactivity, Restlessness-Impulsive, and the ADHD Index scales. The CSHS Emotional scale significantly negatively correlated with the CPRS-R:L Global Index, Oppositional problems, and DSM-IV total scales. The CSHS Bedtime Routine scale also negatively correlated with the CPRS-R:L Hyperactivity, DSM-IV Hyperactivity, and the DSM-IV Total scales. These results indicate that children who snore and have poor sleep hygiene experience multiple internalizing and externalizing behavioral problems that mimic symptoms of ADHD when rated on the CPRS-R:L.
Table 2.
Pearson Correlations of CSHS Scale
| Totals and CPRS-R:L Scale Scores | |||||||
|---|---|---|---|---|---|---|---|
| Physiological | Cognitive | Emotional | Environmental | Bedtime Routine | Sleep Stability | Sleep Hygiene Total | |
| Oppositional Problems |
−0.25 0.001 |
−0.20 0.04 |
−0.32 0.00 |
−0.05 0.63 |
−0.18 0.07 |
−0.17 0.10 |
−0.33 0.00 |
| Cognitive Problems/Inattention |
−0.28 0.001 |
−0.25 0.01 |
−0.18 0.07 |
−0.07 0.50 |
−0.14 0.18 |
−0.14 0.18 |
−0.31 0.002 |
| Hyperactivity |
−0.27 0.006 |
−0.31 0.002 |
−0.16 0.11 |
−0.01 0.93 |
−0.29 0.003 |
−0.18 0.07 |
−0.38 0.00 |
| Anxious-Shy |
−0.26 0.01 |
−0.19 0.06 |
−0.24 0.02 |
−0.16 0.12 |
0.00 0.99 |
−0.27 0.01 |
−0.34 0.00 |
| Perfectionism |
−0.27 0.007 |
−0.20 0.05 |
−0.26 0.009 |
−0.17 0.10 |
0.06 0.52 |
−0.26 0.01 |
−0.35 0.00 |
| Social Problems | −0.17 0.09 |
−0.06 0.59 |
−0.19 0.06 |
−0.10 0.34 |
−0.09 0.40 |
−0.24 0.02 |
−0.27 0.007 |
| Psychosomatic Symptoms |
−0.33 0.00 |
−0.17 0.09 |
−0.18 0.07 |
−0.17 0.10 |
−0.02 0.84 |
−0.16 0.11 |
−0.34 0.00 |
| ADHD Index | −0.21 0.04 |
−0.27 0.008 |
−0.23 0.02 |
−0.06 0.58 |
−0.16 0.11 |
−0.08 0.46 |
−0.29 0.003 |
| CGI: Restlessness-Impulsive |
−0.27 0.01 |
−0.30 0.00 |
−0.26 0.01 |
−0.02 0.87 |
−0.20 0.05 |
−0.11 0.29 |
−0.34 0.00 |
| CGI: Emotional Lability |
−0.26 0.009 |
−0.09 0.39 |
−0.34 0.00 |
−0.14 0.17 |
−0.04 0.72 |
−0.04 0.68 |
−0.25 0.01 |
| Global Index |
−0.36 0.00 |
−0.32 0.00 |
−0.33 0.00 |
−0.03 0.78 |
−0.18 0.08 |
−0.12 0.24 |
−0.39 0.00 |
| DSM-IV Inattentive | −0.09 0.35 |
−0.14 0.16 |
−0.13 0.21 |
−0.09 0.35 |
−0.11 0.28 |
−0.05 0.60 |
−0.18 0.07 |
| DSM-IV Hyperactivity-Impulsivity |
−0.26 0.009 |
−0.35 0.00 |
−0.20 0.04 |
0.05 0.65 |
−0.30 0.00 |
−0.18 0.07 |
−0.38 0.00 |
| DSM-IV Total |
−0.26 0.01 |
−0.34 0.00 |
−0.29 0.003 |
0.01 0.95 |
−0.28 0.005 |
−0.17 0.09 |
−0.39 0.00 |
Snoring Children: Internalizing Symptoms
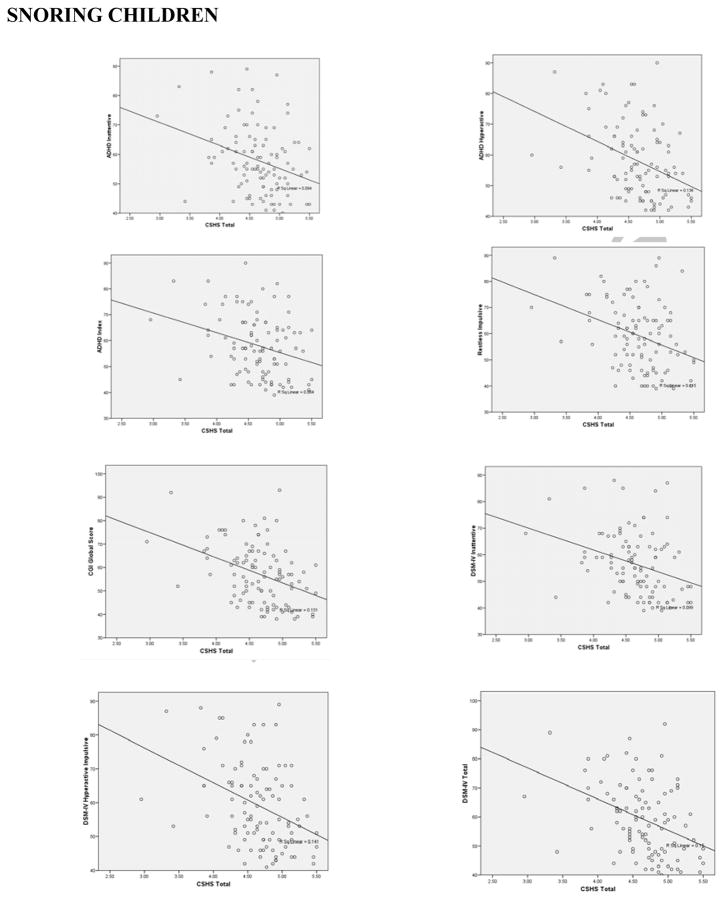
In snoring children, the CSHS total scale was negatively correlated with the subscales of Perfectionism, Psychosomatic Symptoms, Anxious-Shy, Restlessness-Impulsive, Cognitive/Inattention Problems, and Social Problems. Thus, those with better sleep hygiene were less likely to exhibit symptoms of perfectionism, psychosomaticism, anxiety, impulsivity, inattention, and social difficulties (Figure 1).
Figure 1.
Scatterplots of various Children’s Sleep Hygiene Scale (CSHS) and the Conners’ Parent Rating Scales-Revised (CPRS-R:L) measures against sleep hygiene in habitually snoring and non snoring children
The CSHS Physiological scale was negatively correlated with the Psychosomatic Symptoms, Cognitive/Inattention Problems, Perfectionism, Emotional Lability, and Anxious-Shy subscales. These results indicate that children with better sleep hygiene, particularly those who drink less caffeine and are less likely to go to bed hungry, were less likely to exhibit physiological symptoms that manifest as psychosomatic complaints, inattention, mood dysregulation, perfectionism, or anxiety.
Negative correlations were found between the CSHS Emotional scale and the CPRS-R:L Emotional Lability and Perfectionism subscales. Therefore, emotional regulation problems and perfectionistic tendencies were not as strongly demonstrated in children with better sleep hygiene.
The Sleep Stability scale on the CSHS was negatively correlated with the Anxious Shy and the Perfectionism subscales on the CPRS-R:L. Children with better sleep schedules and hygiene practices did not exhibit anxiety symptoms or perfectionism.
The Environmental scale on the CSHS produced no significant relationships with any of the subscales on the CPRS-R:L.
Non-Snoring Children
No significant correlations were found between the CPRS-R:L and the CSHS Total, Physiological, Cognitive, Environmental, Bedtime Routine, or Sleep Stability scales in non-snoring children (Figure 1).
Significant positive correlations were found, however, between the CSHS Emotional scale and the CPRS-R:L Global Index, DSM-IV Inattentive, DSM-IV Hyperactivity-Impulsivity, Oppositional Problems, Restless-Impulsivity, and the DSM-IV total scales in non-snoring children. Thus, non-snoring children who felt anxious or worried at bedtime also demonstrated more inattention, hyperactivity, impulsivity, restlessness, and oppositional behavior during the day.
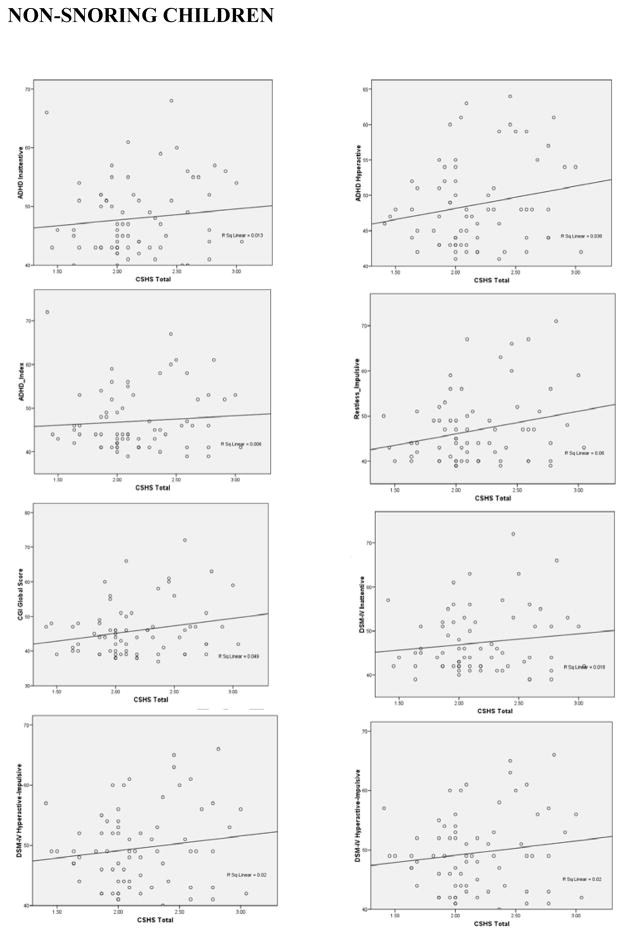
To further explore the potential mediation effects of snoring on the association between sleep hygiene and behavioral regulation we ascertained the presence of a highly robust mediation model in which snoring significantly mediates the association between sleep hygiene and behavioral ratings (Figure 2; Table 3). The pattern of behaviors ascribable to snoring and sleep hygiene can especially be characterized by restlessness-impulsiveness and symptoms of inattentiveness and hyperactivity. In other words, the presence of sleep hygiene-associated behavioral changes was revealed by mediation through snoring.
Figure 2.
Mediation model linking snoring to the association between global sleep hygiene (CSHS total score) and behavioral dysregulation.
Table 3.
Statistical analyses on the mediating effect of snoring in the association between sleep hygiene and behavior in children (see also Figure 2).
| direct effect* | mediating effect | Test-statistic | p-value | |
|---|---|---|---|---|
| 0.24 | Oppositional Problems | 0.33 | 4.8 | 0.000002 |
| 0.11 | Cognitive Problems/Inattention | 0.46 | 6.6 | 0.000000 |
| 0.20 | Hyperactivity | 0.40 | 6.0 | 0.000000 |
| 0.15 | Anxious-Shy | 0.42 | 6.3 | 0.000000 |
| −0.01 | Perfectionism | 0.23 | 3.3 | 0.001131 |
| 0.24 | Social Problems | 0.27 | 3.9 | 0.000121 |
| 0.25 | Psychosomatic Symptoms | 0.34 | 4.9 | 0.000001 |
| 0.08 | ADHD Index | 0.45 | 6.9 | 0.000000 |
| 0.25 | CGI: Restlessness-Impulsive | 0.46 | 7.0 | 0.000000 |
| 0.11 | CGI: Emotional Lability | 0.36 | 5.3 | 0.000000 |
| 0.22 | Global Index | 0.45 | 6.8 | 0.000000 |
| 0.13 | DSM-IV Inattentive | 0.39 | 5.8 | 0.000000 |
| 0.14 | DSM-IV Hyperactivity-Impulsivity | 0.40 | 6.0 | 0.000000 |
| 0.15 | DSM-IV Total | 0.44 | 6.6 | 0.000000 |
Discussion
In the present study, parental reports indicated that poorer sleep hygiene was associated with daytime behavior problems in snoring children. Children who experience inadequate sleep may exhibit excessive daytime sleepiness and attention problems, and they may be at risk for learning difficulties and affective regulation/behavior problems [10,27–29]. According to Gozal and colleagues [9], children who snore are likely to experience inadequate sleep, and may be at increased risk of experiencing difficulty with daytime functioning. Specifically, children who exhibit SDB or snoring are at greater risk for behavioral and neurocognitive problems [9,19]. Ali and colleagues [12] and O’Brien et al. [19] demonstrated that snoring disrupts sleep and has detrimental effects on the quality of sleep while increasing the risk for daytime learning problems, poor school performance, daytime sleepiness, and hyperactivity. Because both inadequate sleep and snoring may produce daytime impairments in attention, learning, and activity, children who snore and have poor sleep hygiene would be expected to have increased susceptibility to daytime problems in attention and regulation of behavior and affect.
Externalizing Behavior
Our hypothesis that snoring children with poorer sleep hygiene exhibit more externalizing daytime behaviors was supported. Significant negative relationships were found between parent-reported sleep hygiene and hyperactivity, impulsivity, and oppositionality. These results strongly support previous research indicating that inadequate sleep, problematic sleep behaviors, and SDB in children may also contribute to daytime conduct problems, hyperactivity, and inattention [36,37]. One could hypothesize that children whose self- regulatory abilities have been compromised by inadequate sleep have more difficulty planning and executing responses to complex or challenging social demands. It is possible that children with poorer self-regulating abilities are more likely than other children to express sleep-induced impairments of moment-by-moment self-regulation that affect their daytime functioning. It is also possible that sleep problems contribute to cumulative impairment in the development of self-regulatory skills.
These positive correlations may give more support to the finding that snoring children are more prone to daytime behavior problems if they do not get adequate and good quality sleep as promoted by appropriate sleep hygiene. Only one aspect of sleep hygiene (emotional distress at bedtime) was associated with daytime behavioral impairments in non-snoring children. Likely, those children who have had disrupted behavior regulation throughout the day tend to have ongoing dysregulation at bedtime whether or not they snore. It seems, however, because of the limited relationship between sleep hygiene and daytime behavior in non-snoring children, that a child who does not snore may not be as susceptible to the daytime effects of poor sleep hygiene as a child who snores and is already at risk for daytime behavior problems. In other words, the daytime manifestations of snoring children with poor sleep hygiene would represent a two-hit phenomenon that may more readily decompensate all of the compensatory mechanisms recruited to accommodate these cognitive and behavioral burdens. Thus, effective treatment of either snoring or poor sleep hygiene may be sufficient to allow for near normal adjustments in parent-reported behaviors.
Internalizing Behavior
The hypothesis that snoring children with poorer sleep hygiene are more likely to exhibit internalize behavior was also supported. Poorer sleep hygiene was associated with more perfectionism, psychosomatic symptoms, anxious-shy behavior, cognitive/inattention problems, emotional lability, and social problems in the snoring children. Again, our findings closely concur with previous reports indicating that symptoms of fatigue, cognitive impairment, and poor academic performance are some of the most common daytime symptoms associated with SDB in children [37].
Therefore, sleep disruption such as that elicited by habitual snoring will likely lead children to develop cumulative fatigue during the day, which would increase the probability that they will be more distractible and irritable if poor sleep routines are superimposed. Past research has demonstrated that children with sleep disturbances have difficulty with regulation of mood and behavior [27]. In addition, children who have primary snoring tend to have more problems with attention, anxiety, depressive symptoms, and social problems than non-snoring children [19,38]. This lack of self-regulation could cause children to become more emotionally labile and more reactive than their classmates, thereby leading to more social difficulties and problematic peer interactions. It is also possible that children who experience anxiety and depression have more difficulty initiating sleep and may delay going to bed or engage in stimulating pre-bedtime activities to distract from ongoing internal processes. Similarly, when children do not get sufficient sleep they become fatigued, irritable, and emotionally labile [26,39], which significantly impacts daytime functioning and has important implications for school performance and social adjustment. The present study supports all aforementioned findings but further sheds light into the potential interactions of sleep hygiene and disrupted sleep on emotional lability in children. Of importance to clinicians treating children with sleep-disordered breathing, all aspects of sleep hygiene with the exception of the comfort of the sleep environment were related to daytime behavioral disturbances. Thus, clinicians should query parents and children with respect to stability of sleep routines, emotional distress at bedtime, pre-bedtime worries, caffeine consumption, and relaxing pre-bedtime activities. If any of these areas are disrupted, they should be addressed in an effort to reduce the impact of sleep-disordered breathing on daytime behavioral functioning.
Limitations of the Study
Several limitations of the study deserve mention. First, while the findings of the study were significant, the sample size of 171 children was not evenly divided according to ethnicity, and a larger proportion of the snoring sample was African American in comparison to the validation studies of the CSHS. Future studies should use a stratified sample with more diversity to determine if ethnicity, race, or cultural practices mitigate the relationship between sleep hygiene and daytime behavior. Second, this study used only parental report to identify and measure both sleep hygiene practices and behavior problems. Because parents of children who snore may report generalized poor behavioral patterns in their children, future research could benefit from obtaining additional information such as a sleep diary or actigraphy or collateral information from teachers and the children themselves. Third, children were not matched for social economic status, which has previously been shown to have an impact on sleep hygiene. Fourth, the restricted age range of children is an advantage for consistency of the data but could also be perceived as a limitation. It may be beneficial to investigate the relationship between sleep hygiene and problem behaviors across the pediatric age spectrum. Finally, the use of correlational analyses precludes determination of causality. It is impossible to conclude whether poor sleep hygiene is the cause of behavior problems, if problematic behaviors elicit poor sleep hygiene, or if a third factor is influencing both. Interventional studies in which implementation of a sleep hygiene protocol and measurement of its effect on behavior would be necessary.
Conclusions
Although intervention studies are needed, clinicians working with children who present with behavior problems should be aware of the potential role that sleep hygiene may play in the severity of daytime behavior problems, particularly in the presence of snoring. Additionally, parents should be fully apprised of unhealthy sleep practices to better understand the impact that a poor sleep routine may impose on their children’s behavior. Furthermore, they should be guided on interventions that may improve sleep hygiene and potentially improve quality of life.
Acknowledgments
This study was supported by NIH grant HL-65270, The Children’s Foundation Endowment for Sleep Research, and by the Commonwealth of Kentucky Challenge for Excellence Trust Fund.
Abbreviations
- SDB
Sleep-disordered breathing
- ADHD
Attention-Deficit/Hyperactivity Disorder
- CSHS
Children’s Sleep Hygiene Scale
- CPRS-R
L, Conners’ Parent Rating Scale, Revised: Long Version
- NPSG
Nocturnal polysomnography
Footnotes
No off label use of products is described, and the authors have no conflict of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Ferber R. The sleepless child. In: Guilleminault C, editor. Sleep and its disorders in children. New York: Raven Press; 1987. pp. 141–163. [Google Scholar]
- 2.Mindell JA, Kuhn B, Lewin DS, Meltzer LJ, Sadeh A. Behavioral treatment of bedtime problems and night wakings in infants and young children. Sleep. 2006;29:1263–1276. [PubMed] [Google Scholar]
- 3.Donaldson DL, Owens JA. Sleep and sleep problems. In: Bear GG, Minke KM, editors. Children’s needs III: Development, prevention, and intervention. Washington DC: National Association of School Psychologists; 2006. pp. 1025–1039. [Google Scholar]
- 4.Stein MA, Mendelsohn J, Obermeyer WH, Amromin J, Benca R. Sleep and behavior problems in school-aged children. Pediatrics. 2001;107:60–69. doi: 10.1542/peds.107.4.e60. [DOI] [PubMed] [Google Scholar]
- 5.Corkum P, Tannock R, Moldofsky H. Sleep disturbance in children with attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychaitry. 1991;37:637–646. doi: 10.1097/00004583-199806000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Stein MA. Unraveling sleep problems in treated and untreated children with ADHD. J Adolesc Psychopharm. 1999;9:157–168. doi: 10.1089/cap.1999.9.157. [DOI] [PubMed] [Google Scholar]
- 7.Gregory AM, Rijsdijk FV, Dahl RE, McGuffin P, Eley TC. Associations between sleep problems, anxiety, and depression in twins at 8 years of age. Pediatrics. 2006;118:1124–1132. doi: 10.1542/peds.2005-3118. [DOI] [PubMed] [Google Scholar]
- 8.Gozal D. Sleep-disordered breathing and school performance in children. Pediatrics. 1998;102:616–620. doi: 10.1542/peds.102.3.616. [DOI] [PubMed] [Google Scholar]
- 9.Gozal D, O’Brien L, Row BW. Consequences of snoring and sleep disordered breathing in children. Pediatr Pulmonol Suppl. 2004;26:166–168. doi: 10.1002/ppul.70094. [DOI] [PubMed] [Google Scholar]
- 10.Beebe DW. Neurobehavioral morbidity associated with disordered breathing during sleep in children: a comprehensive review. Sleep. 2006;29:1115–1134. doi: 10.1093/sleep/29.9.1115. [DOI] [PubMed] [Google Scholar]
- 11.Rosen CL, Storfer-Isser A, Taylor HG, Kirchner HL, Emancipator JL, Redline S. Increased behavioral morbidity in school-aged children with sleep-disordered breathing. Pediatrics. 2004;114:1640–1648. doi: 10.1542/peds.2004-0103. [DOI] [PubMed] [Google Scholar]
- 12.Ali NJ, Pitson DJ, Stradling JR. Snoring, sleep disturbance, and behaviour in 4–5 year olds. Arch Dis Child. 1993;68:360–366. doi: 10.1136/adc.68.3.360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guilleminault C, Eldridge FL, Simmons FB, Dement WC. Sleep apnea in eight children. Pediatrics. 1976;58:23–30. [PubMed] [Google Scholar]
- 14.Chervin RD, Dillon JE, Archbold KH, Ruzicka DL. Conduct problems and symptoms of sleep disorders in children. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42:201–208. doi: 10.1097/00004583-200302000-00014. [DOI] [PubMed] [Google Scholar]
- 15.Owens J, Spirito A, Marcotte A, McGuinn M, Berkelhammer L. Neuropsychological and behavioral correlates of obstructive sleep apnea syndrome in children: A preliminary study. Sleep and Breathing. 2000;4:67–78. doi: 10.1007/BF03045026. [DOI] [PubMed] [Google Scholar]
- 16.Blunden S, Lushington K, Lorenzen B, Martin J, Kennedy D. Neuropsychological and psychosocial function in children with a history of snoring or behavioral sleep problems. Journal of Pediatrics. 2005;146:780–786. doi: 10.1016/j.jpeds.2005.01.043. [DOI] [PubMed] [Google Scholar]
- 17.Owens JA, Mehlenbeck R, Lee J, King MM. Effect of weight, sleep duration, and comorbid sleep disorders on behavioral outcomes in children with sleep-disordered breathing. Archives of Pediatric and Adolescent Medicine. 2008;162:313–321. doi: 10.1001/archpedi.162.4.313. [DOI] [PubMed] [Google Scholar]
- 18.Paavonen EJ, Almqvist F, Tamminen T, Piha J, Moilanen I, Räsänen E, et al. Poor sleep and psychiatric symptoms at school: An epidemiological study. European Child and Adolescent Psychiatry. 2002;11:10–17. doi: 10.1007/s007870200002. [DOI] [PubMed] [Google Scholar]
- 19.O’Brien LM, Mervis CB, Holbrook CR, et al. Neurobehavioral implications of habitual snoring in children. Pediatrics. 2004;114:44–49. doi: 10.1542/peds.114.1.44. [DOI] [PubMed] [Google Scholar]
- 20.Randazzo AC, Muehlbach MJ, Schweitzer PK, Walsh JK. Cognitive function following acute sleep restriction in children ages 10–14. Sleep. 1998;21:861–868. [PubMed] [Google Scholar]
- 21.Fallone G, Owens JA, Deane J. Sleepiness in children and adolescents: Clinical implications. Sleep Medicine Reviews. 2002;6:287–306. doi: 10.1053/smrv.2001.0192. [DOI] [PubMed] [Google Scholar]
- 22.American Academy of Sleep Medicine (AASM) International classification of sleep disorders. 2. Westchester, IL: Author; 2001. [Google Scholar]
- 23.Doghramji P. Insomnia—a clinical perspective. In: Richardson G, editor. International Congress and Symposium Series 262: Update on the science, diagnosis, and management of insomnia. London, UK: Royal Society of Medicine Press, Ltd; 2006. pp. 21–43. [Google Scholar]
- 24.Mindell JA, Owens JA. Clinical guide to pediatric sleep: Diagnosis and management of sleep problems. Philadelphia: Lippincott, Williams, & Wilkins; 2003. [Google Scholar]
- 25.LeBourgeois MK, Giannotti F, Cortesi F, Wolfson AR, Harsh J. The relationship between reported sleep quality and sleep hygiene in Italian and American adolescents. Pediatrics. 2005;115:257–265. doi: 10.1542/peds.2004-0815H. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Morin CM, Culbert JP, Schwartz SM. Nonpharmacological interventions for insomnia: A meta-analysis of treatment efficacy. Am J Psychiatry. 1994;151:1172–1180. doi: 10.1176/ajp.151.8.1172. [DOI] [PubMed] [Google Scholar]
- 27.Dahl RE. The regulation of sleep and arousal: Development and psychopathology. Dev Psychopathology. 1996;8:3–27. [Google Scholar]
- 28.Kahn A, Van de Merck R, Rebuffat E. Sleep problems in healthy preadolescents. Pediatrics. 1989;84:542–546. [PubMed] [Google Scholar]
- 29.Moore M, Allison D, Rosen CL. A review of pediatric nonrespiratory sleep disorders. Chest. 2006;130:1252–1262. doi: 10.1378/chest.130.4.1252. [DOI] [PubMed] [Google Scholar]
- 30.LeBourgeois MK. Children’s sleep hygiene scale. Caretaker-report form for 2- to 12-year-old children. Hattiesburg, MS: University of Southern Mississippi: Sleep Research Laboratory; 2001. [Google Scholar]
- 31.Conners CK. Conners’ Rating Scales-Revised. North Tonawanda, NY: Multi-Health; 1997. [Google Scholar]
- 32.Montgomery-Downs HE, O’Brien LM, Holbrook CR, Gozal D. Snoring and sleep-disordered breathing in young children: Subjective and objective correlates. Sleep. 2004;27:87–94. doi: 10.1093/sleep/27.1.87. [DOI] [PubMed] [Google Scholar]
- 33.Harsh J, Easley A, LeBourgeois MK. An instrument to measure children’s sleep hygiene. Sleep. 2002;26:A316. [Google Scholar]
- 34.Abdi H. Bonferroni and Sidak corrections for multiple comparisons. In: Salkind N, editor. Encyclopedia of Measurement and Statistics. Thousand Oaks, CA: Sage; 2007. pp. 103–107. [Google Scholar]
- 35.Pearl J. Direct and indirect effects. Proceedings of the Seventeenth Conference on Uncertainty in Artificial Intelligence; Morgan Kaufmann; 2001. pp. 411–420. [Google Scholar]
- 36.Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Dev. 1998;69:875–887. [PubMed] [Google Scholar]
- 37.Carroll JL. Obstructive sleep-disordered breathing in children: New controversies, new directions. Clin Chest Med. 2003;24:261–282. doi: 10.1016/s0272-5231(03)00024-8. [DOI] [PubMed] [Google Scholar]
- 38.Cortese S, Lecendreux M. Sleep problems in children with ADHD, impact of treatment and comorbidities. In: Ivanenko A, editor. Sleep and psychiatric disorders in children and adolescents. New York, NY: Informa Healthcare; 2008. pp. 185–192. [Google Scholar]
- 39.Crabtree VM, Ivanenko A, Gozal D. Clinical and parental assessment of sleep in children with attention-deficit/hyperactivity disorder referred to a pediatric sleep medicine center. Clin Pediatr (Phila) 2003;42:807–813. doi: 10.1177/000992280304200906. [DOI] [PubMed] [Google Scholar]