Abstract
Objectives
The promotion of health and safety (H&S) awareness among hospital staff can be applied through various methods. The aim of this study was to assess the risk level of physical hazards in the hospital sector by combining workers' perception, experts' evaluation and objective measurements.
Methods
A cross-sectional study was designed using multiple triangulation. Hospital staff (n = 447) filled in an H&S questionnaire in a general hospital in Athens and an oncology one in Thessaloniki. Experts observed and filled in a checklist on H&S in the various departments of the two hospitals. Lighting, noise and microclimate measurements were performed.
Results
The staff's perception of risk was higher than that of the experts in many cases. The measured risk levels were low to medium. In cases of high-risk noise and lighting, staff and experts agreed. Staff's perception of risk was influenced by hospital's department, hospital's service, years of working experience and level of education. Therefore, these factors should be taken into account in future studies aimed at increasing the participation of hospital workers.
Conclusion
This study confirmed the usefulness of staff participation in the risk assessment process, despite the tendency for staff to overestimate the risk level of physical hazards. The combination of combining staff perception, experts' evaluation and objective measures in the risk assessment process increases the efficiency of risk management in the hospital environment and the enforcement of relevant legislation.
Keywords: Occupational safety, Health hazards, Attitude of health personnel, Risk assessment, Hospital legislation
Introduction
Risk assessment is a structured and systematic procedure that is dependent upon identification of the hazards and an appropriate estimation of risks in a workplace with a view to making inter-risk comparisons for purposes of their control or avoidance. In terms of occupational health, risk assessment aims to facilitate valid decision making in taking all necessary measures that will control the exposure to health hazards in any working environment. It permits employers to attest that all relative measures to work hazards are taken into account and that their evaluation is legitimate [1-3].
In recent years a qualitative occupational risk assessment strategy known as control banding has gained international attention in its goal to offer a complementary and simplified approach to reduce work-related injury and illness [4,5]. This approach clusters workplace hazards into stratified risk "bands" based on common hazards and control approaches that offer long-sought unification across Occupational Health and Safety (OHS) professionals [6]. The term has an industrial hygiene focus and represents a qualitative instrument to assess risks for chemical substances, generating solutions and implementing control measures [7]. In the 1980s this risk assessment approach was expanded to radiation, lasers, biosafety and eventually pharmaceuticals in the 1990s [5,8,9]. Control banding is supposed to provide assessment results of reasonable quality without expert involvement [10,11]. In essence, a risk matrix is developed that describes the likelihood and probable severity of the event under study. The risk matrix is generally described as a function of two variables: the severity of the hazard presented by any facility or operation (and which is often a function of the intrinsic safety or health hazard of the material handled at that facility), and the likelihood of a major incident occurring, e.g., an explosion or a release of toxic material. These two variables (or minor variations of them) serve as the basis for most risk matrices. Such matrices can have the desirable characteristics that provide a benchmark against which to evaluate other approaches [12,13].
Occupational hazards refer to workplace factors with a potential for harm in terms of injury or ill health. Hazards are classified in four categories: physical (noise, vibration, radiation, extremes of temperature, ergonomic), chemical (solid, liquid, vapour), biological (bacteria, fungi, viruses), and psychosocial (psychological and social stressful factors). Exposure to these hazards can cause occupational diseases and work accidents [14].
Hospital workers are exposed to various occupational hazards that may threaten their health and safety (H&S) [3]. Physical hazards in the general working environment that are also encountered in the hospital sector include temperature, illumination, noise, vibration, changes in atmospheric pressure, and ionizing and non-ionizing radiation [14-18]. A review of the international and Greek literature revealed the following physical hazards in the hospital working area: lighting, microclimate, noise, ionizing, and non ionizing radiation [19-22]. Lighting is a hazard that concerns all workers, especially during the night shift, in all hospital departments. Bad lighting can cause eye fatigue, whose local symptoms are pain, dacryorrhea, redness, and general symptoms, such as headache, sleepiness and irritation, as well as increased likelihood of accidents and decreased work productivity [15,23]. Sources that transmit heat in a hospital setting are numerous and this makes them important. Boilers, sterilization units, or even intense lighting in operation theatres are sources of heat, which (especially over 30℃) can cause rash, heat cramps, nausea, headaches, dizziness or just fatigue, and which can lead to impaired performance and work accidents [24,25]. Heat can also have negative consequences in persons with heart or liver diseases, and pregnant women [14]. Workers in hospital kitchens, laundry rooms and sterilization units are the main groups that are exposed to this hazard. Personnel that are occupied in boiler rooms, drive cars, or work outdoors, especially during summer in warm climates, are also exposed to heat [14]. Noise can influence workers' ability to work efficiently and safely [26]. Hospitals are not quiet workplaces. Many hospital departments offer exposure to high noise level that can cause hearing problems and influence workers' ability of concentration. For example, a noise level of 89 dB (A) was measured in the kitchen of a large hospital [22,27 30].
In Greece, hazard identification and assessment, although mandatory by law in the hospital sector since 1986, does not take place systematically. In this study, risk assessment of physical hazards (noise, temperature, relative humidity [RH], and lighting) was performed in two Greek hospitals, through inspection of departments by experts combined with subjective staff's perception of risk level and the results of objective measurements. One quantitative (objective measurements) and two qualitative (occupational safety professionals filled in a checklist through observation and workers filled in a questionnaire) risk assessment techniques were used. The use of multiple methods and sources (triangulation) was chosen since the application of only one method or sample - especially when it is not tested before, as it happens in the present study- may disclose only one part of reality. A combination of different methods and/or data sources in a study promotes the possibility of disclosure of multiple dimensions of empirical reality and contributes to improving the reliability and validity of data [31-36]. The proposed methodology (triangulation of different methods and data sources) can be a useful tool in any hospital areas in order to find out which hazards are of high, medium or low risk and which factors (demographic-working) are related to the staff's perception of risk level. It can also contribute to the enforcement of relevant legislation, and to the existence of a safer, more efficient and effective working place, such as the hospital.
Materials and Methods
This study was conducted by combining quantitative and qualitative risk assessment of physical hazards in two hospital working environments. Risk assessment is complete when all relative parameters are taken into account, when its application does not lead to serious oversights and inaccuracy, and when instability is reduced by good information. Models, hypotheses and estimates used in risk assessment must be kept on file so as to be repeatable in the future [37].
The definition of risk level necessitates the development of risk standards, which may represent the opinions of those who set the rules and the range of acceptance or tolerance for each risk. Such an example is occupational exposure limits (OELs) [15]. Risk may be defined with qualitative, semi-quantitative (with decreased quantitative accuracy) and quantitative methods [38]. Qualitative methods can use expert opinions by using a checklist. Semi-quantitative methods arrange hazards into a comparative scale or use a risk assessment matrix (RAM) [2]. Quantitative risk assessment is better shown through industrial hygiene measurements taken for comparison to OELs or noise level measurements. Risk level will define the need for corrective or preventive measures.
Study design
Hazards in hospital working environments vary. Hospital workers are exposed to a variety of hazards that differ according to education or tasks applied. The present study proposes a method of risk assessment including measurement of physical hazards, compares its results to expert evaluation and conducts subjective risk evaluation of hospital staff. It was designed as a cross-sectional survey by using triangulation of methods and sources (objective measurement, observation, questionnaire) for data collection. It was conducted in a general hospital in Athens and an oncology hospital in Thessaloniki. Necessary permissions were requested and granted from the scientific committees of the two hospitals. Both hospitals applied a preventive policy according to the law and occupational safety professionals were employed according to Greek regulations.
The study process comprised three phases [39]:
1. Detection of hazards, during the development of tools (focusing on physical hazards) including the RAM used;
2. Analysis and identification of hazard exposure (during observation, filling in checklists by occupational safety professionals and questionnaires by staff); and
3. Evaluation of hazard exposure (during measurement of hazards and of risk level according to RAM used).
A risk assessment report, including written instructions for safe working tasks, was completed according to Greek law and submitted to the employers [40].
Tools and risk calculation
Tools developed and used are:
1. An OHS Staff questionnaire (one general and two specific, one for operation theatres and one for clinical laboratories) was developed based on the available literature [2,41-44] and was filled in by hospital staff in their work places. A pilot study was performed in order to check the validity and reliability of the newly developed tool of this study. Questionnaires were tested for internal consistency and were found acceptable with a very high Cronbach's α of 0.90 [45]. The first part of the questionnaire included a brief description of the groups of hazards, directions for filling in the answers and questions on demographic information. The second part included closed and positive questions of H&S referring to the following nine groups of hazards: Work environment-working equipment, Physical hazards (in this study ergonomics were excluded from this group and were included in the group of work organization hazards), Electrical, Chemical, Biological, Fire safety, Work organization-working relations-ergonomics, Working with visual display units, and Waste management. These questions were answered by choosing one of the five possible answers: "Always", "Often", "Rarely", "Never" and "Do not know" for the cases with no hazard in their perception. Answers followed a Likert Scale (from 0= Always to 3=never), and corresponded, according to RAM, to three risk levels: "Always" and "Often"=0-1, equal to low level (A), "Rarely"=2 equal to medium level (B), and "Never"=3 equal to high level (C). In addition, there was a sixth choice of answer, "No application", if a hazard is irrelevant to a hospital department and is not included in the Scale. Based on the answers given to the group of questions on physical hazards only, of the second part of three questionnaires, the staff's perception of risk level was evaluated as low, medium, or high according to the score that results from the median value of the answers.
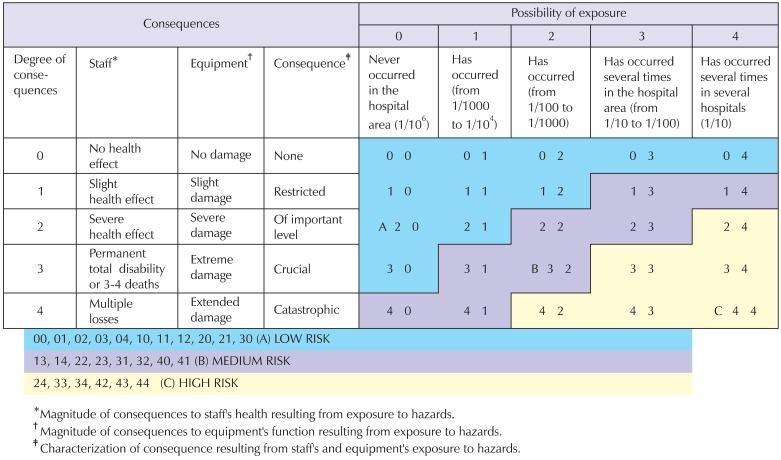
2. General Inspection Checklist on H&S Hazards, to be filled in by occupational safety professionals by Greek law on H&S issues. This is a record of quantification of evaluated hazards in the hospital working area and is filled in according to a developed guide/brochure. It is based on the theoretical models of risk evaluation and on educational instructions on hazards identification referring to safe and healthy conditions of working with physical hazards. The guide includes the RAM (Fig. 1), which was based on existing literature and further developed for this study, and from which the risk level of each hazard results were taken [2]. The checklist is formed with five columns with the following contents: the hazards (the same as those referred to the nine groups of the staff's questionnaire), a brief description of activity or situation in which the hazards exist, the possibility of exposure to the hazard is written down, the risk consequences (0-4) due exposure to the hazard, and the corresponding risk level (A, B, C). There are also two special checklists with the same formulation, one for operation theatres and one for clinical laboratories.
Fig. 1.
Risk assessment matrix.
3. Quantitative measurements for noise, temperature, humidity, and lighting were measured instantly (referring to limits of legal Greek and European standards) in the following departments: offices of administrative service, laboratories and desks of technical service, desks of nursing and medical services in all clinical departments, clinical laboratories in both hospitals, and in the operation theatre only in the special hospital. Temperature and RH in indoor hospital workplaces environments were measured by a digital humidity and temperature meter (HT-3003 by LUTRON). Illumination, referring to the work position in front of a desk, was measured by an electronic Luxmeter (DIGITAL LUX METER by INS). Noise level was measured by a type II sound level meter having a dB (A) weighting capability (CASTLE GA 205). According to this study's RAM, the classification of risk levels according to measured values followed three levels: low risk (A risk: Noise below 45 dB (A), Temperature 18-22℃, RH (percentage saturation) 40-60%, Lighting (referring to medium office work with medium visual demands) 500-700 Lux), medium risk (B level: between 45-80 dB (A), 23-26℃, 60-75%, 200-350 Lux) and high risk (C level: exceeding 85 dB (A), above 26℃ or below 18℃, below 40% or above 75%, 200 Lux). However, in work positions where accuracy plays an important role, for example operation theatres, the recommendable luminance is above 2000 Lux, resulting in an adjusted classification of risk level.
Sample
a) Hospital personnel (nurses, physicians, administrative and technical staff), filled in the OHS Staff questionnaire. The sample was randomly selected by strata defined by hospital service (administrative, technical, nursing and medical) and a third of the staff was included. The total sample in the general hospital included 360 subjects and 250 in oncology. The response rate was 68.9% in the general hospital (81.9% filled in the general questionnaire, 36% filled in the special questionnaire for operation room and 80% filled in the special questionnaire for clinical laboratory). In the oncology hospital, 199 workers participated (79.6%), from whom 104 filled in the general questionnaire (80%), 43 the special questionnaire for operation room (86%) and 52 (74.3%) the special questionnaire for clinical laboratory.
b) Occupational safety professionals (the researcher and the safety engineer) filled in, through observation, the Inspection Checklist on H&S Hazards in the different hospital departments
c) Measurements of physical hazards (noise, temperature, humidity and lighting) were performed in the hospital departments.
Validity
The questionnaires were tested for internal consistency and demonstrated very high Cronbach's α, ranging from 0.85 to 0.92 [46].
Ethical issues
The questionnaires were anonymous and the participants were informed in writing about the study purposes and their voluntary participation.
Data analysis
Quantitative variables are presented with mean and standard deviation. Qualitative variables are presented with absolute and relative frequencies. In order to determine the independent factors associated with H&S scores, multiple linear regression analyses in a stepwise method (p for entry <0.05 and p for removal <0.10) were performed. Regression coefficients (β) with their standard errors were produced from the results of regression analyses. All p-values reported are two-tailed. Statistical significance was set at 0.05 and analyses were conducted using SPSS version 17.0 (SPSS Inc., Chicago, IL, USA).
Results
Sample characteristics
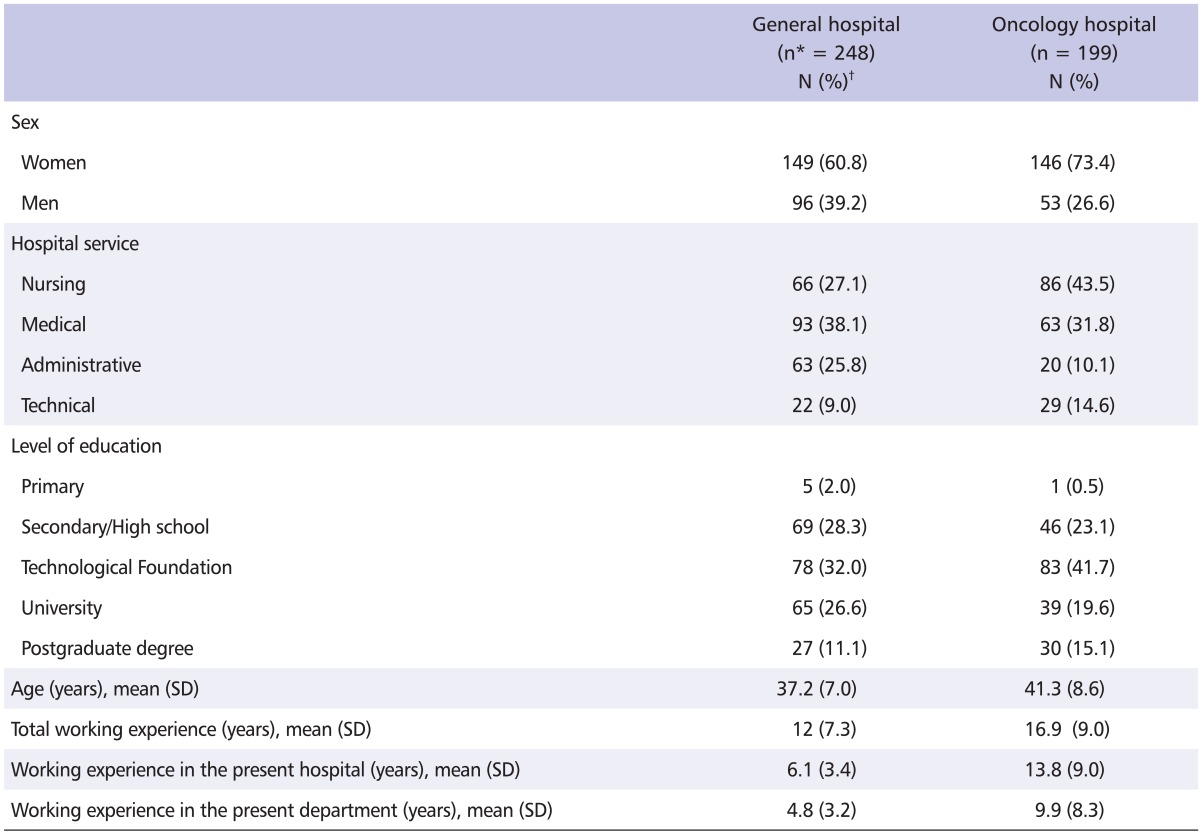
Table 1 presents the demographic data and work characteristics of the hospital staff that participated in the study. In both hospitals, the percentage of female workers was almost double than that of male workers. Most workers were in nursing and medical service and graduated from technological foundation, with a mean age of 40 years old, having 12 years of working experience for the general hospital and 17 years for oncology.
Table 1.
Characteristics of hospital staff for general and oncology hospitals
SD: standard deviation.
*n: total number of workers completed the study's questionnaire.
†N (%): number of workers (percentage) of total number of workers completed the study's questionnaire.
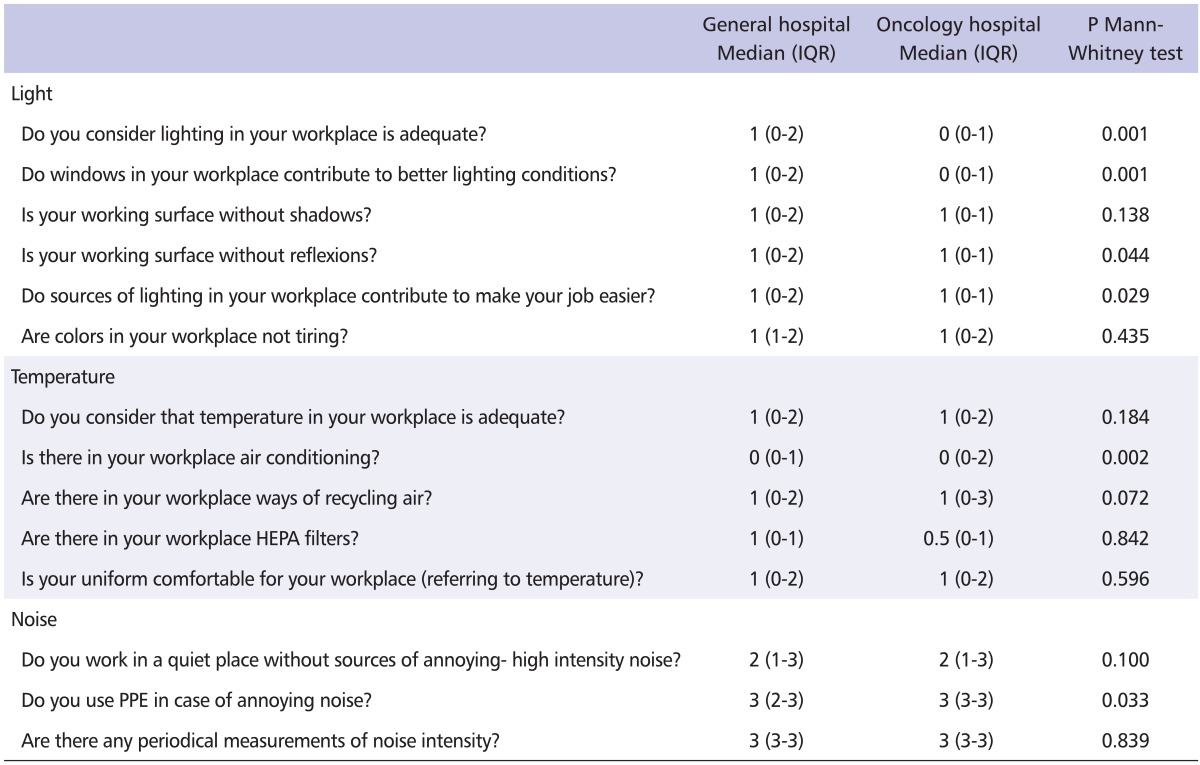
Qualitative risk assessment by hospital staff
The combined median values of the answers concerning the physical hazards for both the general and oncology hospitals are shown in Table 2. The participants of both hospitals declared high levels of risk concerning noise. Participants from the general hospital perceived greater risk level for factors referring to adequate lighting, workplaces with windows and existence of better natural light, no existing reflex working surface, and appropriate light sources that make it easy to work, compared to the participants from the oncology hospital. Lighting was measured in office work positions in all hospital departments in both hospitals. Workers occupying the various hospital workplaces assessed the risk level through their subjective feelings about the lighting or noise levels and whether any discomfort was experienced. In the general hospital, the majority of administration offices was placed in underground rooms where windows and natural light were limited and, as a result, workers evaluated the level of lighting as of high risk. In contrast, participants from the oncology hospital perceived greater risk level for factors referring to existence of air conditioning in the workplace and existence of personal protective equipment compared to the participants from the general hospital. The oncology hospital is an older building than the general one, with minimal possibilities for modern ergonomic design and facilities, including appropriate adjustment of microclimate conditions. In addition, the common tasks performed by participants in the oncology hospital have to do with treatment of cancer patients only, which means the continuous handling of hazardous equipment and tasks such as chemotherapy and radiotherapy. These parameters may have strongly influenced subjective evaluation of risk level in the hospital working area.
Table 2.
Risk assessment according to workers' answers to the study questionnaire
IQR: interquartile range, HEPA: high efficiency particulate air, PPE: personal protective equipment.
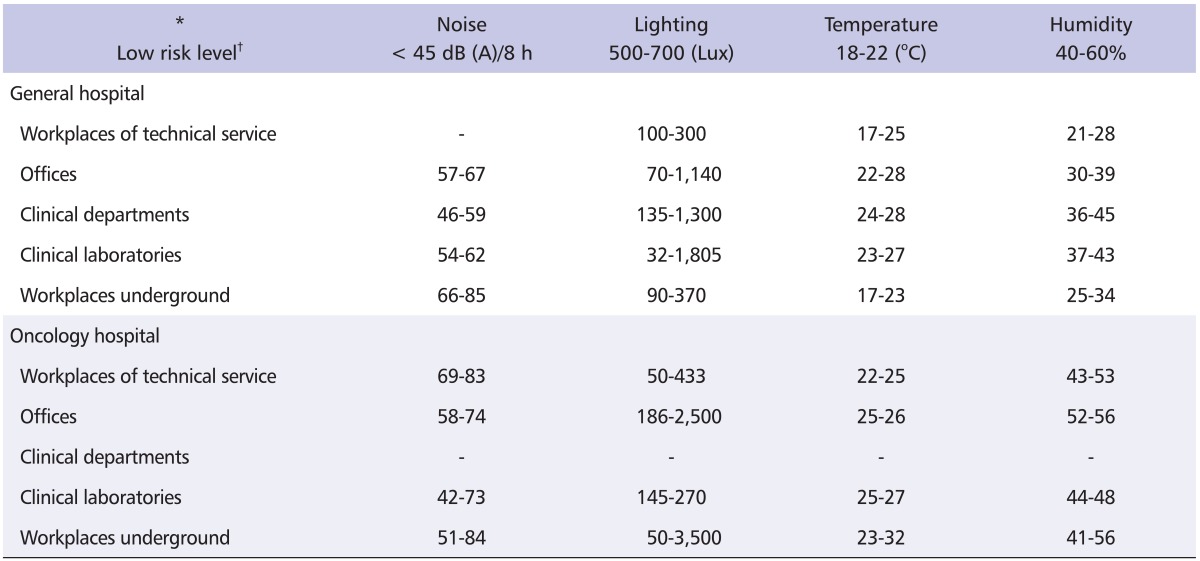
Quantitative risk assessment of physical hazards
In the general hospital (Table 3), noise level was measured high in the boiler room, laundry, emergency department, biochemical laboratory and blood donation unit. The level of lighting was between 32/50 and 395 Lux with the lowest in the X-rays diagnostic room, in offices without natural light and low artificial and local lighting and in the departments housed in the basement of the hospital. Levels of temperature were between 16-27℃, with the minimum measured in the departments housed in the basement. Levels of humidity were between 22-45%.
Table 3.
Minimum and maximum results of measurements of physical hazards
*Noise: value below 45 dB (A) refers to A, between 45-80 dB (A) refers to B, exceeded the 85 dB (A) refers to C, Lighting: value between 500-700 Lux refers to A, between 200-350 Lux refers to B, below 200 Lux refers to C Temperature: range of 18-22℃ refers to A, 23-26℃ refers to B, above 26℃ or below18℃ refers to C, Humidity: range of 40-60% refers to A, 60-75% refers to B, below 40% or above 75% refers to C.
†According to study's risk assessment matrix: A = low risk level, B = medium risk level, C = high risk level.
In the oncology hospital (Table 3), the following departments had the highest levels of noise: the boiler unit, ironing room, sterilization unit located next to the boiler, biochemical laboratory, emergency department and waiting room of the X-rays diagnostic unit. The lowest levels of lighting were found in the X-rays diagnostic room, offices away from windows with low artificial and local lighting and in departments housed in the basement, such as the central boiler, central sterilization unit, kitchen, radiotherapy unit, nuclear medicine unit and blood donation unit. The coldest place was the corridor of the emergency unit. The warmest workplaces were the sterilization room, boiler unit and kitchen, combined with the highest level of humidity as well.
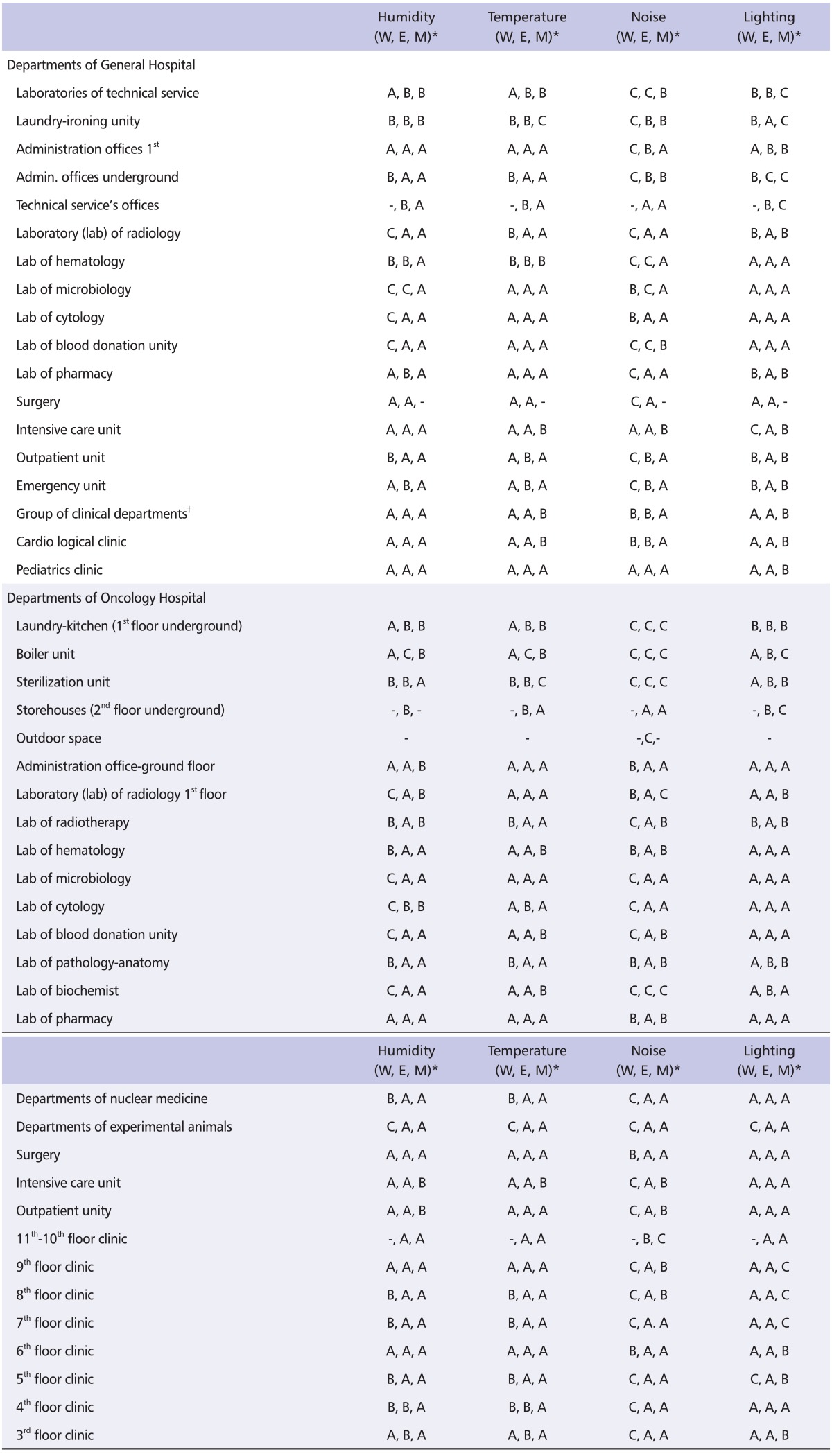
Description of risk level according to staff's perception, experts' evaluation and measurements of physical hazards
Table 4 presents the risk level of the four physical hazards (microclimate conditions: RH, temperature, noise and lighting) as perceived by staff (median of answers in the relevant part of the questionnaire), experts' evaluation (risk level according to RAM in the inspected hospital's departments) and the results of instant objective measurements in the two hospitals (according to normal range of limits).
Table 4.
Prescription of risk levels according to RAM as defined by workers, experts and objective measurements
Risk level of physical hazards (A: Low, B: Medium, C: High).
RAM: risk assessment matrix.
*Evaluated risk level by workers (W), experts (E), measurements (M).
†Orthopedics, psychiatric, 1st and 2nd pathological, neurological, gynecological.
In the general hospital, workers in the majority of departments perceived noise at a high risk level and humidity at a medium level. Experts in the same departments evaluated noise at a medium level and lighting at a low level. Regarding measurements, humidity was low level in all departments, temperature was low in almost half of the departments and was medium level in the rest. Lighting in the majority of departments was at medium level, but low level in the basement. Noise was low level in the majority of departments. Exceptions for noise were high level in the laundry and central boiler and medium level in the emergency department, in administrative offices and blood donation unit.
In the oncology hospital, workers in the majority of departments perceived a high risk of noise and a high and medium of risk of humidity. However, experts evaluated the risk level as low in the same departments. Regarding measurements, RH was mostly measured at a low level (40-60%), and at a medium level (60-75%) only in eight departments. Temperature values were at a low level (range of 18-22℃) in the majority of departments, with the exception of the central sterilization unit where it was at a high risk level (above 26℃). Lighting was measured at a high risk level (below 200 Lux) in five departments (underground workplaces and offices of clinical departments) while in the majority of the rest it was at a low risk level (500-700 Lux). Finally, noise, in the majority of departments was low (below 45 dB [A]), whereas in the following departments a high risk level (exceeded 85 dB [A]) was measured: laboratories of technical service, boiler room, laundry, central sterilization unit, radiology unit, biochemical laboratory and outdoor space.
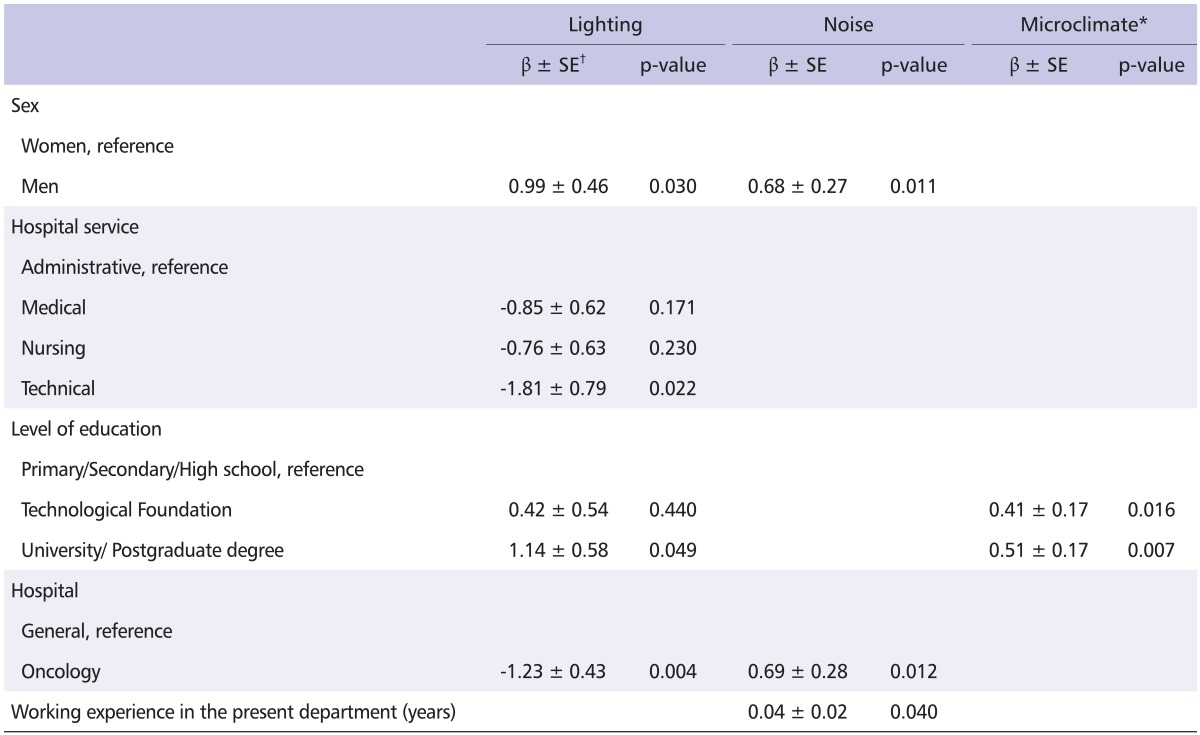
Factors influencing the staff's perception of risk level of physical hazards
From the multiple linear regression analysis conducted in a stepwise method (Table 5), men and those with higher educational level perceived a higher risk level of lighting. In contrast, staff of the oncology hospital, compared to those in the general one, and technical personnel, compared to administrative personnel, perceived a lower risk level of lighting (in the general hospital administration offices were mostly underground). Men and staff of the oncology hospital perceived a higher risk level of noise than those of the general hospital. Technical service staff in the oncology hospital were men only, who worked in an old building with three levels underground, longer than the ones in the general hospital. Furthermore, the years of working experience were positively correlated with higher risk level perceptions for noise in the multiple linear regression analysis. Higher educational level was also associated with higher risk level perceptions concerning temperature.
Table 5.
Results from stepwise regression analysis concerning staff's perception scores about appropriate lighting, noise and microclimate conditions
SE: standard error.
*Temperature & humidity.
†Regression coefficient ± SE.
Discussion
In both hospitals, the risk level for lighting as estimated from the RAM was underestimated by staff and experts since the measurements showed appropriate conditions, with the exception of some departments of the oncology hospital that are located underground and are deprived of natural light. Participants may have perceived that lighting was low in their workplaces in terms of their various tasks inside different parts of their hospitals, some tasks that do not always take place in front of an office or a position where extra sources of lighting are available to help them work with greater resolution and accuracy. Referring to microclimate conditions, workers underestimated the risk level compared to experts, whose evaluation was similar to measurement results in the majority of hospital departments. Temperature and RH may have been perceived by participants as lower than the results of instant objective measurements, as they work constantly during their shift, wearing their work uniforms in the hospital areas and being used to these conditions. However, experts evaluated the risk level as outside observers just once, during the completion of the checklist. Noise was overestimated by workers in both hospitals relative to the objective measurements, except some underground units with a high measured risk. Wherever noise was perceived by the participants as hazardous (i.e., high level), although the objective measurements showed that it was under the regulatory limits, the density 40-60 dB(A) may have caused a distraction during periods of concentration in preparing reports and analytical reports or when trying to focus on patient needs.
It could be claimed that both hospitals are workplaces with a medium level of risk referring to physical hazards, with the oncology one having a higher level of risk in microclimate conditions as it is located in Northern Greece with a wetter climate in general. This finding is also in agreement with the ranking of hospitals, according to the Greek law, as a workplace with medium risk level.
Independent variables that correlate to staff's perception of risk
In both hospitals, variables that were studied were level of education, sex, total years of work, years of work in the present hospital and in the present department, and professional specialty. Level of education, professional specialty and working experience influenced the staff's perception of risk level at a statistically significant level. It could be argued that the level of education influences the level of knowledge in H&S issues. Therefore, the perception of risk level or the tasks done by highly educated hospital workers (e.g., physicians) demand better conditions of lighting or quieter workplaces to concentrate. The finding that men and those with higher educational level perceived a higher risk level of lighting may have been due to the fact that hospital personnel (physicians or nurses) consider proper lighting with high intensity to be necessary for appropriate care of the patients or in the preparation of reports or analysis samples. In addition, the workers' experience and the object of their work (technicians or administrators, that work for many years, in underground workplaces, close to noisy machines or without windows and natural sources of lighting) play important roles in their perception of the risk level for noise.
Comparison of hospitals
A comparison of the findings in the two hospitals revealed several differences between the staff's risk perception and the experts' evaluation, possibly due to the workers' lack of the same work experience in the two hospitals, which partially influenced their perception of risk level. These two hospitals are different in terms of specialization. One offers all general health services (prevention, therapy, rehabilitation) to the general population in one geographical area in greater Athens. The other is an oncology one, in a city with increased humidity, receiving cancer patients from the whole Northern Greece, and offering specialized services to them and, as a result, having different working conditions and work-related stressors. Another parameter is the age of the buildings, with the general hospital being three decades younger. The oncology staff therefore finds it more difficult to ensure proper maintenance of equipment or adoption of modern working conditions.
Utility of tools for different hospitals
The tools used in this study were considered usefully adequate because it was possible to find existing differences that could be associated with the specific characteristics of the two hospitals, as described above. They are also prototype means of risk assessment in the hospital working area. On one hand, they facilitate experts (occupational physicians and safety professionals) in locating hazards, in the application of what they are obliged to do by Greek law. On the hand, workers themselves participate actively in the risk evaluation process in their work place. This may assist them in realizing the perceptual risks rather than the regulatory issues and they are able to observe, to be informed of and to adopt their work behavior and expectations.
In addition, because expert evaluation is mostly performed by external specialists, the comparison of their evaluation with that of the staff could help better describe the different situations at different times. The tools developed and used in this study could be useful and appropriate for any hospital, since their reliability and validity were satisfactory in the study sample. In any case, their use is a dynamic and complex process, and further examination will be necessary in order to establish them as standard risk assessment tools.
Study limitations and future research
The present study was designed and implemented as a cross-sectional survey, due to time restrictions that limited the proof of repetition.
The development and testing of new questionnaires and checklists are both a strength and a limitation. Validity was ensured through the triangulation of methods and data sources and the measured reliability was high. The results may therefore contribute significantly to the hospital staff awareness of H&S, to the facilitation of OHS professionals and to the enforcement of Greek labor law. However, the study results cannot be generalized to the entire hospital sector. Therefore, more research is required in other hospitals and with repetitive application of the same risk assessment methods. Only four physical hazards were measured: noise, lighting, temperature and humidity. The possibility of also measuring others, such as radiation, would have provided a more complete picture of the hospital risk level but it was not feasible in the present study due to the cost of performing such measurements. Ergonomics were also excluded from this group of hazards due to the need for more disciplines, including anthropometry, biomechanics, mechanical engineering, industrial engineering, industrial design, kinesiology, physiology, psychology and further experimental design suitable for the study of workers and their environments. Future investigation should therefore include all physical hazards and other groups of hazards. The lack of familiarity with the utility of risk assessment in the Greek hospital sector could also be improved by periodical risk assessment studies.
The differences observed in the perceived risk level of physical hazards, between the subjective evaluations by staff and the quantitative measurements, demonstrate the need for training in H&S issues. Such training would also assist in aligning the results between qualitative and quantitative assessment and would determine the superior assessment for each workplace and task in the hospital. The training could possibly be tailored to also address the staff's perception of risk and offer them input to improve their working environment. This participatory approach to a work-related intervention might improve worker satisfaction and lead to a synergistic increase in work-related safety.
In conclusion, the proposed triangulation methodology could be a useful tool for any hospital area. The respondent answers, measurements and observations revealed the complexity in the application of risk assessment, and helped to confront the hazards, both real and perceived, in the workplace. The lack of staff awareness on H&S issues contributed to both over- and under-estimation of the risk level. Experts, as external evaluators in a cross-sectional study, may also have under- or overestimated the existing risk level. These two facts underline the need for the risk assessment process to be repeated occasionally. Despite the absence of any investigation aimed at understanding the complexities of hospital working conditions, the study results showed that appropriate information and education of health care staff on H&S issues are necessary in order to implement adequate preventive policies. Additionally, the contribution of workers in the risk assessment process is valuable and ways must be found of including their perception of risk- given the appropriate education - as this will provide a more complete picture of the workplace situation.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Paustenbach DJ. The practice of health risk assessment in the United States (1975-1995): how the US and other countries can benefit from that experience. Hum Ecol Risk Assess. 1995;1:29–62. [Google Scholar]
- 2.Sadhra SS, Rampal KG. Basic concepts and developments in health: risk assessment and management. In: Sadhra SS, Rampal KG, editors. Occupational health risk assessment and management. 4th ed. Oxford (UK): Blackwell Science Ltd; 1999. pp. 3–187. [Google Scholar]
- 3.Harrington JM, Gill FS, Aw TC, Applebey G, Atwell CP. Occupational health. 4th ed. Oxford (UK): Blackwell Pup.; 2000. pp. 3–347. [Google Scholar]
- 4.Zalk DM, Kamerzell R, Paik S, Kapp J, Harrington D, Swuste P. Risk level based management system: a control banding model for occupational health and safety risk management in a highly regulated environment. Ind Health. 2010;48:18–28. doi: 10.2486/indhealth.48.18. [DOI] [PubMed] [Google Scholar]
- 5.Zalk DM, Nelson DI. History and evolution of control banding: a review. J Occup Environ Hyg. 2008;5:330–346. doi: 10.1080/15459620801997916. [DOI] [PubMed] [Google Scholar]
- 6.Fingerhut M. Global qualitative risk management (control banding) activities. Ind Health. 2008;46:305–307. doi: 10.2486/indhealth.46.305. [DOI] [PubMed] [Google Scholar]
- 7.Russell RM, Maidment SC, Brooke I, Topping MD. An introduction to a UK scheme to help small firms control health risks from chemicals. Ann Occup Hyg. 1998;42:367–376. doi: 10.1016/s0003-4878(98)00056-8. [DOI] [PubMed] [Google Scholar]
- 8.Naumann BD, Sargent EV, Starkman BS, Fraser WJ, Becker GT, Kirk GD. Performance-based exposure control limits for pharmaceutical active ingredients. Am Ind Hyg Assoc J. 1996;57:33–42. doi: 10.1080/15428119691015197. [DOI] [PubMed] [Google Scholar]
- 9.Sargent EV, Kirk GD. Establishing airborne exposure control limits in the pharmaceutical industry. Am Ind Hyg Assoc J. 1988;49:309–313. doi: 10.1080/15298668891379792. [DOI] [PubMed] [Google Scholar]
- 10.Hashimoto H, Goto T, Nakachi N, Suzuki H, Takebayashi T, Kajiki S, Mori K. Evaluation of the control banding method--comparison with measurement-based comprehensive risk assessment. J Occup Health. 2007;49:482–492. doi: 10.1539/joh.49.482. [DOI] [PubMed] [Google Scholar]
- 11.Oldershaw PJ. Control banding workshop, 4-5 November 2002, London. Ann Occup Hyg. 2003;47:531–532. doi: 10.1093/annhyg/meg087. [DOI] [PubMed] [Google Scholar]
- 12.Anttonen H, Paakkonen R. Risk Assessment in Finland: Theory and Practice. Saf Health Work. 2010;1:1–10. doi: 10.5491/SHAW.2010.1.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Money CD. European experiences in the development of approaches for the successful control of workplace health risks. Ann Occup Hyg. 2003;47:533–540. doi: 10.1093/annhyg/meg061. [DOI] [PubMed] [Google Scholar]
- 14.Hasselhorn HM, Toomingas A, Lagerstrom M. Occupational health for health care workers. A practical guide. Amsterdam (Netherlands): Elsevier Science B.V.; 1999. pp. 1–113. [Google Scholar]
- 15.Ashton I, Gill SF. Monitoring for health hazards at work. 3rd ed. Oxford (UK): Blackwell Science; 2000. pp. 33–185. [Google Scholar]
- 16.Gehanno JF, Ledosseur P. In occupational health for health care workers. A practical guide. Amsterdam (Netherlands): Elsevier Science B.V.; 1999. Radiation problems in the health care professions; pp. 144–151. [Google Scholar]
- 17.Lawson IJ. Vibration. In: Sadhra SS, Rampal KG, editors. Occupational health: risk assessment and management. 4th ed. Oxford (UK): Blackwell Science Ltd; 1999. p. 379. [Google Scholar]
- 18.Hipkin J, Spence E, Sutherland A. Risk assessment for workers exposed to ionizing radiation. In: Sadhra SS, Rampal KG, editors. Occupational health: risk assessment and management. 4th ed. Oxford (UK): Blackwell Science Ltd; 1999. pp. 428–430. [Google Scholar]
- 19.Jefferies P, Clemett RS, Turner JR. Radiation hazards during cobalt 60 plaque therapy for choroidal melanoma. Aust N Z J Ophthalmol. 1993;21:37–41. doi: 10.1111/j.1442-9071.1993.tb00128.x. [DOI] [PubMed] [Google Scholar]
- 20.Christensen M. Noise levels in a general intensive care unit: a descriptive study. Nurs Crit Care. 2007;12:188–197. doi: 10.1111/j.1478-5153.2007.00229.x. [DOI] [PubMed] [Google Scholar]
- 21.Ryherd EE, Waye KP, Ljungkvist L. Characterizing noise and perceived work environment in a neurological intensive care unit. J Acoust Soc Am. 2008;123:747–756. doi: 10.1121/1.2822661. [DOI] [PubMed] [Google Scholar]
- 22.Tsiou C, Efthymiatos G, Katostaras T. Noise in the operating rooms of Greek hospitals. J Acoust Soc Am. 2008;123:757–765. doi: 10.1121/1.2821972. [DOI] [PubMed] [Google Scholar]
- 23.Velonakis E, Sourtzi P. Health and work. Athens (Greece): BETA Medical Edition; 2009. Greek. [Google Scholar]
- 24.Scott E, Beswick A, Wakefield K. The hazards of diathermy plume. Part 1. The literature search. Br J Perioper Nurs. 2004;14:409–414. doi: 10.1177/175045890401400904. [DOI] [PubMed] [Google Scholar]
- 25.Hammer DL. Hot refueling hazards. Mil Med. 1989;154:150–153. [PubMed] [Google Scholar]
- 26.Melamed S, Luz J, Green MS. Noise exposure, noise annoyance and their relation to psychological distress, accident and sickness absence among blue-collar workers--the Cordis Study. Isr J Med Sci. 1992;28:629–635. [PubMed] [Google Scholar]
- 27.Tsiou C. Noise in hospital area. [dissertation] Athens (Greece): University of Athens Faculty of Nursing; 2000. Greek. [Google Scholar]
- 28.Topf M. Hospital noise pollution: an environmental stress model to guide research and clinical interventions. J Adv Nurs. 2000;31:520–528. doi: 10.1046/j.1365-2648.2000.01307.x. [DOI] [PubMed] [Google Scholar]
- 29.Tran N, McLean D, Yassi A. Noise problems in health care facilities. In: Hasselhorn H.M, Toomingas A, Lagerstrom M, editors. Occupational health for health care workers. A practical guide. Stockholm (Sweden): Elsevier; 1999. pp. 152–157. [Google Scholar]
- 30.Yassi A, Gaborieau D, Gillespie I, Elias J. The noise hazard in a large health care facility. J Occup Med. 1991;33:1067–1070. [PubMed] [Google Scholar]
- 31.Tziaferi S, Sourtzi P. Triangulation: A methodological approach in health care research. Nursing. 2002;3:258–265. Greek. [Google Scholar]
- 32.Redfern SJ, Norman IJ. Validity through triangulation. Nurse Researcher. 1994;2:41–56. [Google Scholar]
- 33.Hammersley M, Atkinson P. Ethnography: principles in practice. London (UK): Tavistock; 1992. pp. 198–199. [Google Scholar]
- 34.Denzin N. The research act in Sociology, a theoretical introduction to sociological methods. 3rd ed. New York (NY): McGraw-Hill; 1989. [Google Scholar]
- 35.Hinds PS, Young KJ. A triangulation of methods and paradigms to study nurse-given wellness care. Nurs Res. 1987;36:195–198. [PubMed] [Google Scholar]
- 36.Woods NF, Mitchell PH. Designing studies to explore association and difference. In: Woods NF, Catanzaro, editors. Nurs Res: theory and practice. St Lewis (MI): MOSBY; 1988. p. 151. [Google Scholar]
- 37.Presidential Degree 17/96 "Measures on the improvement of health and safety of workers in compliance with directives 89/391/EU and 91/383/EU" Paper of the Goverment of Hellenic Democracy. Athens (Greece): Ed. National Print Office; 1996. pp. 1–12. Greek. [Google Scholar]
- 38.Raafat H, Sadhra SS. Risk characterization. In: Sadhra SS, Rampal KG, editors. Occupational health: risk assessment and management. 4th ed. Oxford (UK): Blackwell Science Ltd; 1999. pp. 177–193. [Google Scholar]
- 39.Drivas S, Zorba K, Koukoulaki TH. Methodological guide in evaluating and preventing occupational risk. Athens (Greece): Greek Institute in Health & Safety; 2000. pp. 15pp. 25–36. Greek. [Google Scholar]
- 40.Velonakis MG, Tsalikoglou F. System of health and safety administration in hospital working area. Athens (Greece): Ed. Parisianou; 2005. pp. 9–192. Greek. [Google Scholar]
- 41.European year on safety, hygiene and health in workplace - A Guide on Working with hazardous products. Luxembourg: Ed. Service of Official Editions of European Communities; 1992. pp. 1–46. Greek. [Google Scholar]
- 42.Four indicatory guides on enforcement of Guideline "temporary or mobile building sites". Luxembourg: Ed. Service of Official Editions of European Communities; 1993. Europe on health and safety in workplace; pp. 1–72. Greek. [Google Scholar]
- 43.Sandford M. Checking your way to working safely. Aust Nurs J. 1997;5:15–24. [PubMed] [Google Scholar]
- 44.Groupement professionel de formation de l' hospitalisation privée du Sud-Est (GPFHP) La prévention des risques professionnels dans les établissements hospitaliers privés. Guide d' evaluation. Paris (France): Ed. Institut National de Recherche et de Sécurité (INRS); 1997. p. 68. French. [Google Scholar]
- 45.Tziaferi S. Risk assessment of occupational hazards in Hospital Area [dissertation] Athens (Greece): Department of Nursing, University of Athens; 2006. p. 153. Greek. [Google Scholar]
- 46.Tziaferi S, Sourtzi P, Velonakis Em. Pilot study Risk assessment in Hospital area. Nursing. 2006;45:380–390. Greek. [Google Scholar]