Abstract
Conservative estimates indicate that 18–25% of women in the United States will be exposed to some form of sexual assault in their lifetime. A great number of these women will develop post-traumatic stress disorder (PTSD). The current study explores the relationship between emergency contraception (EC) administration and subsequent post-traumatic stress symptoms in female sexual assault (SA) survivors. In a study population of 111 participants, post traumatic stress symptoms were assessed approximately six months after the SA. Women who were already taking hormonal contraception (HC) at the time of the SA and those who declined EC were compared to women who took either Ogestrel or Plan B following the SA. While the administration of traditional HC and both types of EC were associated with fewer intrusive symptoms, women who took Ogestrel reported significantly lower post traumatic stress total symptom levels than did those who took Plan B or those who declined EC. The results suggest that the manipulation of sex hormone levels with HC and EC in the immediate aftermath of trauma may influence subsequent post-traumatic stress symptoms. The current results may be useful in guiding the choice of EC.
INTRODUCTION
Although figures vary considerably based on the studied population, conservative estimates suggest that between one in four and one in six women in the United States experience sexual assault at some point during their lives (Campbell & Wasco, 2005; Tjaden & Thoenes, 2006). Victims of sexual assault appear to be particularly vulnerable to developing post-traumatic stress disorder (PTSD), an anxiety disorder characterized by reexperiencing, avoidance, and hyperarousal symptoms which significantly impair normal functioning. Reexperiencing symptoms include intrusive and recurrent recollections of the traumatic event, reliving the event, and distress upon exposure to cues associated with the trauma. Avoidance symptoms include efforts to avoid any thoughts, feelings, or activities associated with the trauma, as well as a feeling of detachment from others. Hyperarousal symptoms include difficulty sleeping, irritability, increased startle response, and difficulty concentrating (American Psychiatric Association, 2000).
Some studies indicate that 34–52% of rape victims subsequently develop PTSD (Zinzow et al., 2011), and others report the highest rates of PTSD in response to rape, especially among women (Sundin & Horowitz, 2003; Campbell & Wasco, 2005; Frans et al., 2005). Sexual assault victims report higher levels of intrusion and avoidance symptoms than do survivors of other trauma types (Sundin & Horowiz, 2003). Although many of these symptoms largely subside within three months of trauma, many trauma survivors report fear and anxiety symptoms impairing everyday functioning persisting for longer periods of time (Breslau, 2001).
Despite the fact that women are exposed to either similar or significantly lower rates of trauma than are men (Kessler et al., 1995; Breslau et al., 1998; Frans et al., 2005), women are at least twice as likely to develop PTSD as are men (Kessler et al., 1995; Frans et al., 2005; Tolin & Foa, 2006). Additionally, PTSD may persist up to four times longer in women (Breslau et al., 1998). These sex differences in PTSD prevalence are observed cross-culturally and across many geographical locations (Altemus, 2006). Although men and women differ somewhat in the types of trauma they are exposed to throughout their lifetimes, the pronounced sex disparity in PTSD prevalence remains evident when analyses control for trauma type (Tolin & Foa, 2006). While these sex differences in PTSD are widely observed and agreed upon, surprisingly little research has investigated factors contributing to PTSD development in women.
Little is known about the impact of fluctuating sex hormone levels during the menstrual cycle on PTSD development or symptoms. Several authors have suggested that women may be more vulnerable to developing PTSD during certain phases of the menstrual cycle because acute stress responses are potently affected by menstrual cycle position and alterations of stress hormone responses have been implicated in PTSD (Saxe & Wolfe 1999; Rasmusson & Friedman, 2002). Other authors have argued for the investigation of menstrual cycle position on PTSD development on the grounds that menstrual cycle effects have been noted in fear conditioning, which may predict responses to exposure-based PTSD treatment (Milad et al., 2006). Studies in our laboratory have shown that women in the luteal phase of the menstrual cycle report more intrusions following exposure to emotional stimuli than do women in the follicular phase or men (Ferree & Cahill, 2009; Ferree, Kamat, & Cahill, 2011). A recent clinical study found that women in the mid-luteal phase of the menstrual cycle at the time of a trauma are significantly more likely to experience intrusive flashback memories than are women not in the luteal phase (Bryant et al., 2010). These findings suggest that menstrual cycle position or sex hormone levels at the time of trauma may influence subsequent PTSD susceptibility, but more work needs to be done exploring this possibility.
While exploring the potential effects of endogenous levels of estradiol and progesterone on post-traumatic stress symptoms is an important area of research calling out for further investigation, the effects of exogenously applied hormones may also be important to consider. In the aftermath of sexual assault, women are offered emergency hormonal contraception (EC). In order to prevent pregnancy, EC works in a similar manner to standard hormonal contraception (HC) by inhibiting ovulation, fertilization, and implantation of the egg (Frye, 2006). The difference between EC and normal HC is that EC is administered either in a single dose or two doses of synthetic estrogens and/or progestins rather than a distributed lower dosage administered over the course of a month.
Two of the most commonly used forms of EC in the United States are Ogestrel and Plan B, and these differ in at least one critical way. Ogestrel consists of two doses of a combination of the synthetic estrogen ethinyl estradiol and the synthetic progestin levonorgestrel, while Plan B is a single higher dose of levonorgestrel alone (Leung, Levine & Soon, 2010).
In order to investigate the effects of EC on subsequent post-traumatic stress symptoms, we contacted women six months after sexual assault and assessed PTSD symptom profiles at that time during a phone interview. We compared intrusive and avoidance symptoms in women who took Plan B, Ogestrel, and those who declined to take EC.
METHODS
Collaboration
This project was conducted by Forensic Nurse Specialists, Inc. (FNS) in partnership with researchers at the University of California, Irvine. FNS is a private organization that provides forensic examinations 24 hours per day to law enforcement for victims of domestic violence and sexual assault. FNS operates six SART (Sexual Assault Response Team) centers in the Southern California area and maintains a central database of sexual assault victims coming into their centers in Los Angeles and Orange counties.
TACT Database
FNS maintains a database of sexual assault victims coming into their SART centers throughout Southern California. The TACT database includes a variety of information collected from each victim, such as age, race, post-coital interval, emergency contraception information, start date of the most recent menstrual period, use of alcohol or drugs at the time of assault, relationship to attacker, type of contraception, and other information. A population of 655 female sexual assault victims between the ages of 18 and 40 whose assaults occurred 5–7 months prior to the date of phone calls were identified from this database.
Exclusion Criteria
Only female sexual assault victims between the ages of 18 and 40 were identified in the database. Women were excluded from the sample if they were pregnant at the time of the assault, could not provide a date for the start of their last menstrual period, if they were developmentally disabled, if they had a history of severe mental illness, did not speak English, were victims of domestic violence, did not provide a valid phone number, had an exam in a SART center more than 48 hours after the time of assault, or if there was no record of which form of emergency contraception was administered.
Participants
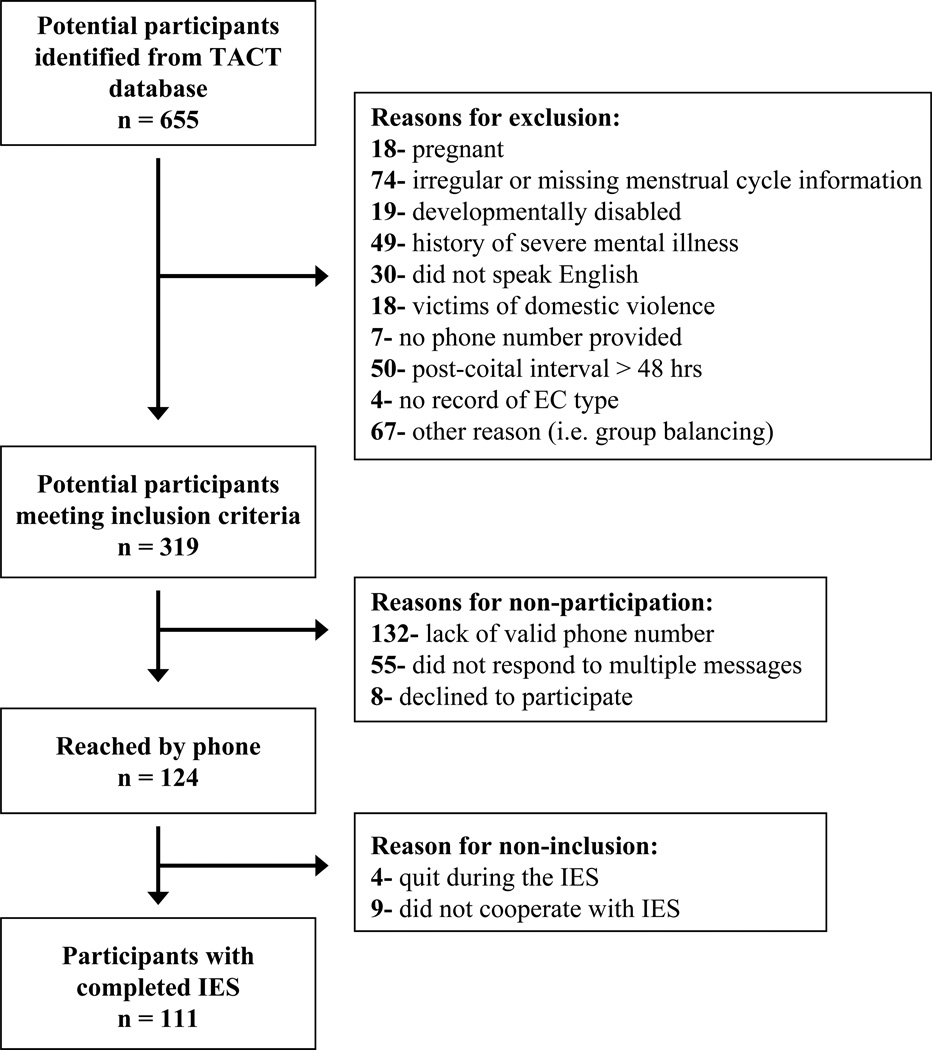
655 potential participants were identified in the TACT database, and 336 were excluded based on the criteria mentioned above. Following subsequent exclusions for a variety of reasons detailed in Figure 1, the final sample used in statistical analyses was comprised of 111 female sexual assault victims who provided informed consent and completed a phone interview for this study, which was approved by the University of California, Irvine Institutional Review Board. The study population was 6.3% Asian, 13.5% African-American, 31.5% Hispanic, 45.0% Caucasian, and 3.6% of other ethnicity. Participants were classified by self-reported start of most recent menstrual period into follicular (days 1–14, n = 51) and luteal (days 15–34, n = 60) phases of the menstrual cycle.
Figure 1.
Participant population, including explanations for exclusion from statistical analysis.
Experimental Procedure
Participants identified in the database were contacted 5 to 7 months following sexual assault. The Director of FNS (author Wheeler) called and asked each woman to complete the standard FNS follow-up questionnaire regarding medication compliance, counseling referrals, mental well-being, and patient satisfaction. After all of the standard follow-up questions were asked, Wheeler briefly told each participant about a study being conducted by FNS in partnership with UC Irvine and asked if she would be willing to talk to the lead researcher about participation. If she answered yes, the phone was passed to author Ferree, at which time Ferree described the basics of the experiment, the risks associated with participation, the confidentiality of all research materials, the right to discontinue participation at any time, and finally asked the participant to verbally provide informed consent. Once informed consent was granted, the PTSD symptom inventory was administered. This process took approximately 5 to 15 minutes for each participant.
PTSD Symptom Inventory
The Impact of Events Scale (IES) has been used in hundreds of studies since it was initially developed (Horowitz, Wilner, & Alvarez, 1979), has been found to perform consistently well, and is predictive of PTSD diagnoses as assessed by the gold-standard clinical interviews (Brewin, 2005). The IES requires participants to indicate the frequency with which 15 PTSD symptoms associated with a single traumatic event have occurred within the last week. Answers range from “not at all” (score of 0) to “often” (score of 5), and the scale includes seven questions addressing intrusion symptoms and eight questions addressing avoidance symptoms. It has been determined that optimal diagnostic performance most closely predicting PTSD diagnosis by Clinician-Administered PTSD Scale (CAPS) is a cutoff score of 35 (Neal et al., 1994).
Emergency Contraception
Following the standard forensic exam for sexual assault, victims were offered emergency hormonal contraception (EC) to prevent pregnancy. The two forms of EC used by FNS are Ogestrel and Plan B, and the choice of medication is determined by availability and hospital formulary. Ogestrel consists of two doses (12 hours apart) each containing 0.1 mg ethinyl estradiol and 0.5 mg levonorgestrel, and Plan B consists of a single dose of 1.5 mg levonorgestrel alone. Of the participants with complete survey data, 34 took Ogestrel, 49 took Plan B, and 28 declined EC. Of the women refusing EC, 17 were already using hormonal contraception at the time of the assault (HC) and 11 declined to take EC for unspecified reasons but were not taking any form of hormonal contraception at the time of the assault (No HC).
Statistical Analysis
IES total, intrusion, and avoidance scores were compared between emergency contraception methods (No HC, HC, Ogestrel, Plan B) and menstrual cycle phase (follicular and luteal) by ANOVA. Chi square tests of independence were performed to examine relationships between EC method and several features of the SA, and the relationship between features of the SA and IES total scores were tested by ANOVA.
RESULTS
Emergency Contraception Effects
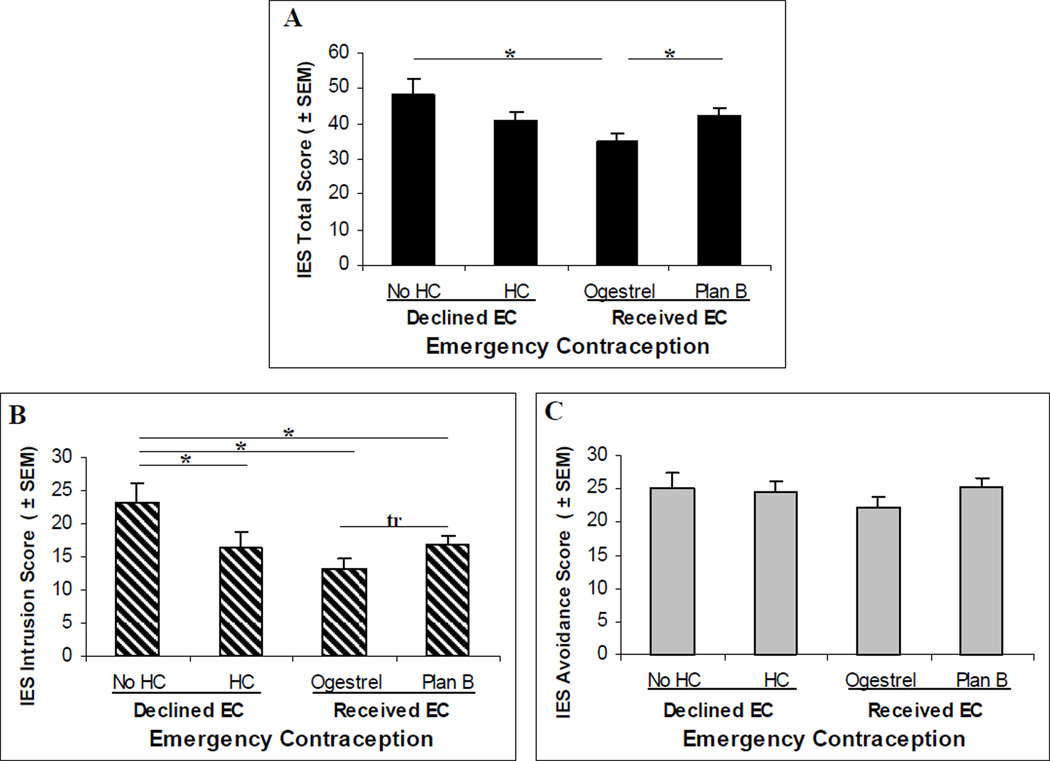
An ANOVA comparing IES total scores among the different EC groups revealed a main effect of EC [F(3, 107) = 3.21, p < .05, η p2 = 0.083]. Fisher’s PLSD follow-up tests indicated that the Ogestrel group had lower scores than did both the Plan B group, and the No HC group (both p < .05). No other differences emerged (all p > .15). An ANOVA comparing IES Intrusion subscale scores also revealed a main effect of EC [F(3, 107) = 3.68, p < .05, ηp2 = 0.094]. Fisher’s PLSD follow-up tests revealed that the group who declined EC had higher scores than did all three of the other groups (all p < .05), and there was a trend (p = .06) toward the Ogestrel group having lower scores than the Plan B group. Finally, an ANOVA comparing IES avoidance subscale scores revealed that there was no main effect of EC [F(3, 107) = 1.10, p > .35, ηp2 = 0.030], and Fisher’s PLSD follow-up tests revealed no group differences (all p > .05). See Figure 2. Table 1 contains effect sizes (Cohen’s d) for the group comparisons.
Figure 2.
Impact of Events Scale scores in each group. (A) IES Total scores, with the clinical cutoff of 35 marked by dashed line. (B) Scores on the IES Intrusion subscale. (C) Scores on the IES Avoidance subscale. *p < .05; tr indicates p = .06
Table 1.
Effect sizes (Cohen’s d) for group comparisons of IES Total, Intrusion, and Avoidance scores.
| Cohen's d | |||
|---|---|---|---|
| IES Total | IES Intrusion | IES Avoidance | |
| No HC vs. HC | 0.56 | 0.71* | 0.07 |
| No HC vs. Ogestrel | 0.86* | 1.067* | 0.33 |
| No HC vs. Plan B | 0.40 | 0.68* | −0.05 |
| HC vs. Ogestrel | 0.43 | 0.34 | 0.29 |
| HC vs. Plan B | −0.13 | −0.08 | −0.13 |
| Ogestrel vs. Plan B | −0.51* | −0.44 (tr) | −0.37 |
indicates significant differences between groups as detected by Fisher’s PLSD follow-up tests.
Menstrual Phase Effects
Analyses were conducted exploring the effects of both EC and self-reported menstrual phase to determine whether menstrual phase was an important factor. A two-way ANOVA of IES total scores revealed a main effect of EC [F(3, 103) = 3.35, p < .05, ηp2 = 0.089], and no main effect of Menstrual Phase or an Menstrual Phase × EC interaction were observed (both p > .30). A two-way ANOVA of IES Intrusion scores only revealed a main effect of EC [F(3, 103) = 3.24, p < .05, ηp2 = 0.086], and no main effect of Menstrual Phase or an Menstrual Phase × EC interaction were observed (both p > .50). A two-way ANOVA of IES Avoidance scores revealed no main effects of EC or Menstrual Phase, nor a Menstrual Phase × EC interaction (all p > .15).
Features of the Assault
Chi-square tests of independence were performed to examine the relationships between EC group and the following features of the SA: weapon use, drug use, alcohol use, loss of consciousness (LOC), more than one assailant, stranger vs. acquaintance, use of physical violence, use of threats, previous history of SA, and post-SA therapy (Table 2). The relationship between the variables EC and alcohol use was significant, χ2 (3, N = 111) = 12.04, p < .01. Women in the No HC group were less likely to have consumed alcohol at the time of SA, and women who in the HC group were more likely to have consumed alcohol. The relationship between the variables EC and post-SA therapy failed to reach significance χ2 (3, N = 111) = 7.61, p = .06. Women in the HC group were somewhat more likely to seek therapy, and women who took Plan B were somewhat less likely to seek therapy. No other relationships were detected between EC and other features of the assault (all p > .35).
Table 2.
Features of the SA. (Left) Percentages of survivors in each group for each SA feature. (Right) IES scores associated with each SA feature.
| % Survivors per Group | IES Total Score | ||||||
|---|---|---|---|---|---|---|---|
| Declined EC | Received EC | ||||||
| SA involved: | No HC | HC | Ogestrel | Plan B | Yes | No | Unknown |
| a weapon | 0.0 | 0.0 | 2.9 | 6.1 | 47.5 | 43.3 | |
| drugs | 18.2 | 0.0 | 14.7 | 20.4 | 44.5 | 41.0 | 34.1 |
| alcohol | 36.4 | 94.1 | 76.5 | 75.5 | 40.2 | 40.9 | |
| LOC | 18.2 | 52.9 | 38.2 | 42.9 | 38.9 | 41.4 | |
| > 1 assailant | 9.1 | 5.9 | 11.8 | 18.4 | 32.8 | 42.6 | 34.4 |
| a stranger | 18.2 | 17.7 | 14.7 | 22.5 | 42.8 | 39.8 | |
| physical violence | 18.2 | 17.7 | 14.7 | 12.2 | 41.5 | 43.4 | 35.6 |
| threats | 18.2 | 5.9 | 17.7 | 20.4 | 43.0 | 43.8 | 36.2 |
| history of previous SA | 27.3 | 11.8 | 20.6 | 28.6 | 42.2 | 39.8 | |
| post-SA therapy | 36.4 | 52.9 | 41.2 | 18.4 | 41.2 | 40.0 | |
Participants who were unsure whether drugs were involved in the SA showed a non-significant trend toward lower IES total scores [F(2, 108) = 2.55, p = .08, ηp2 = 0.045]. Significantly lower IES total scores were observed among participants who were unsure whether the SA involved physical violence [F(2, 108) = 3.48, p < .05, ηp2 = 0.060] or threats[F(2, 108) = 3.67, p < .05, ηp2 = 0.064]. Participants whose SA involved only one perpetrator had higher IES total scores than participants whose SA involved more than one perpetrator [F(2, 108) = 4.30, p < .05, ηp2 = 0.074]. No differences in IES total scores were observed based on whether or not the SA involved a weapon, alcohol use, loss of consciousness, attack by a stranger vs. acquaintance, a history of prior SA, or whether post-SA therapy was sought (all p ≥ .35, Table 1).
DISCUSSION
The main finding of this experiment was a significant influence of EC administration on IES total scores, such that women who took Ogestrel reported lower levels of post-traumatic stress symptoms than did either women in the No HC group or those who took Plan B. Further analyses revealed that this effect was driven by decreases in intrusion symptoms, as we did not observe effects of EC on avoidance symptoms. Additionally, we did not observe any effects of menstrual cycle position at the time of trauma on subsequent post-traumatic stress symptoms. The observed effects of EC mostly fell into the medium to large range of effect sizes. The findings of this experiment suggest that peri-traumatic exogenous sex hormone administration can affect subsequent post-traumatic stress symptoms.
Influence of EC
Unfortunately, relatively little is known about the effects of EC on endogenous sex hormone levels both immediately and in the days following administration, so it is difficult to speculate about how the different forms of EC affected symptoms. Not much research has been done investigating the effects of EC on estradiol and progesterone levels, and the research that has been done suggests that different effects on the subsequent menstrual cycle are observed depending on whether EC is administered prior to or after ovulation (Leung, Levine & Soon, 2010). It appears that Plan B may eliminate normally observed hormone elevations during the luteal phase if administered prior to ovulation (Tirelli, Cagnacci & Volpe, 2008), but administration before ovulation fail to affect hormone levels (Durand et al., 2001). No studies of which we are aware report the effects of the Ogestrel regimen on hormone levels in the subsequent menstrual cycle, nor are there studies examining the acute effects of Plan B or Ogestrel peri-traumatically.
Because intrusion symptoms were similar in women in the HC group and women who took Ogestrel, these results may be attributable to a common mechanism of action which results in persistently reduced levels of endogenous sex hormones (Frye, 2006). However, it is not clear why an acutely administered combination of synthetic estrogen and progestin should be more beneficial than a higher dose of synthetic progestin alone, since both forms of EC are thought to have the same effect on endogenous sex hormone levels. While both forms of EC appear to be associated with fewer post-traumatic stress symptoms than is a refusal to take EC (in the No HC group), it remains possible that the combination of synthetic estradiol and progestin confers some protective interactive effect which is greater than that of a synthetic progestin alone. Because we observed differences between two forms of EC that are theorized to have similar effects on endogenous sex hormone levels, it remains possible that the differential effects are due to some direct action of the exogenous hormones themselves rather than an indirect influence upon endogenous sex hormone levels. Any explanations of the observed results that include arguments about the acute or prolonged effects of EC on sex hormone levels will remain speculative until more is known about the specific effects of Ogestrel.
Menstrual Phase
Analyses using menstrual cycle position should be cautiously interpreted for several reasons. Due to the nature of the study’s recruitment, at the time the study began, 6 months had passed between our initial participants’ arrival at the SART centers and symptom assessment interviews. As SART procedures were not guided by the requirements of our study, women were not told that accuracy was important and were not pressed to provide an exact date of the start of their most recent period. As the study progressed, the SART teams were more careful about collecting this information. Menstrual cycle position was of secondary importance to the current study, which focused on the effects of EC, and careful records were kept concerning EC administration. For these reasons, caution must be exercised in interpreting the results of our analyses of menstrual cycle. Because other authors have reported that women in the mid-luteal phase of the menstrual cycle show a greater likelihood of experiencing traumatic flashback memories (Bryant et al., 2010), it remains possible that more accuracy in determining cycle position would have yielded observable effects on symptoms. As self-report is not always accurate, future studies specifically interested in the potential effects of menstrual cycle position on PTSD symptoms should incorporate salivary hormone samples to verify cycle position.
Features of the Assault
Few significant differences were revealed between EC groups and features of the SA. Women who refused EC were less likely to have consumed alcohol, and women who were on HC were more likely to have consumed alcohol. Although the relationship between EC and post-SA therapy failed to reach significance, women on HC were more likely to seek post-SA therapy than women who took Plan B. Despite these differences, it appears unlikely that the differences in IES scores are due to differences in features of the SA within these groups. Several of our findings regarding effects of SA features on IES scores are counterintuitive. For instance, it is surprising that we observed lower IES scores in women with multiple assailants compared to those with one assailant. This may in part be due to the very small number of women in each group with multiple assailants. We are aware that there is a chance that some of these results may be spurious, but they were not our primary concern and we are hesitant to make broad conclusions based on these findings. The goal of these analyses was to show that the observed group differences in IES scores were not due to specific features of the SA being over- or underrepresented in any EC group. Although the EC groups did show slightly different profiles of SA features, as neither of the features for which there were group differences (alcohol use and post-SA therapy) were also associated with corresponding changes in IES total scores, we feel confident that such features do not account for our effects.
Use of Inventories to Assess PTSD
Given the highly sensitive nature of our subject population, we decided to use a very brief, easy-to-understand and relatively unobtrusive assessment tool. Fortunately, there are several well respected brief post-traumatic stress symptom inventories that, despite not allowing one to assign a clinical diagnosis outright, are tightly related to PTSD diagnosis based on gold-standard assessment tools such as the Structured Clinical Interview for DSM Disorders (SCID) and the CAPS. One of the most widely respected of these short assessment tools is the IES, which has been extensively validated and implemented in dozens, if not hundreds, of studies (for review of many of these inventories, see Brewin, 2005). Although the diagnostic value of the IES is very tightly related to diagnoses made by CAPS and SCID, it should be noted that in the present study we did not actually measure PTSD proper—which must be determined by clinical interview—but rather post-traumatic stress symptoms. Ideally, future studies of PTSD symptoms will include assessment by trained clinicians using the CAPS or SCID. Anecdotally, in many cases during the present experiment, women were hesitant to complete our interviews despite having been told they would only take five minutes of their time and would not involve any questions about the trauma itself. This fact, in combination with the expertise of author Wheeler drawn from decades of working with sexual assault victims from a variety of backgrounds, suggests that the feasibility of a study utilizing the CAPS or SCID in a population of sexual assault survivors may be questionable.
Concluding Remarks and Implications for Clinical Practice
It is important to note that although decreased post traumatic stress symptoms were observed in the Ogestrel group, the IES scores still remained relatively high in all groups. To place the current results in a broader context with reference to normative samples, mean (± SD) IES scores in trauma victims without reference to a specific time elapsed since the trauma were 16.7 ± 17.9, compared to a mean of 8.1 ± 12.3 in people without a history of trauma (Briere & Elliott, 1998). It may be more valuable to compare the IES scores in the current study to those of other trauma survivors six months after trauma. In a sample of burn victims, participants without a PTSD diagnosis had a mean total IES score of 12.0 ± 12.0, and those with PTSD had a mean of 36.3 ± 20.9 six months after the trauma (Perry et al., 1992). In a sample of people who experienced physical injury as a result of traumatic events, those without PTSD had mean total IES scores of 12.9 ± 7.9, and those with PTSD had a mean of 48.0 ± 13.5 six months after the precipitating traumatic events (Shalev et al., 1996). The IES scores of our sample, therefore, were relatively high in all four of our groups, perhaps due to the specific nature of sexual assault and the additional vulnerability to PTSD this trauma confers (Sundin & Horowitz, 2003; Zinzow et al., 2001). Our findings of symptom reduction were statistically significant and our effect sizes fell into the medium to large range, suggesting potential clinical relevance. However, while the use of EC may reduce symptom frequency and severity, particularly for intrusive symptoms, it does not appear to lead to a complete abatement of symptoms. It is also noteworthy that the group differences in Intrusion subscale scores accounted for the observed differences in IES total scores. As all of our previous laboratory work upon which this study was based focused on intrusive memories, this was consistent with our hypotheses. We had no predictions based on avoidance symptoms, and it is unclear why use of EC was not associated with a reduction in avoidance symptoms as well.
Despite the hurdles inherent in conducting this type of study, studies of factors contributing to PTSD are critically important. PTSD is a crippling disorder affecting approximately 8% of individuals in the United States during their lifetimes (Kessler et al., 1995) and one that is extremely difficult to treat. Although some evidence indicates that symptoms do naturally diminish over time (Resnick et al., 2007), systematic reviews of studies concerning the efficacy of treatment with drugs or therapy are quite bleak, suggesting that treatment is marginally effective in many people and may even make symptoms worse in some individuals (Berger et al., 2009; Roberts, Kitchiner, Kenardy & Bisson, 2009). Many theories of PTSD have been developed based on studies using primarily male populations of combat veterans, and considering the heightened rates of PTSD in women, studies specifically investigating responses to trauma in women are needed.
Furthermore, although sexual assault survivors may be difficult to recruit for participation in research, sexual assault is rather prevalent and appears to confer a particularly high risk of PTSD among survivors (Sundin & Horowitz, 2003; Zinzow et al., 2001). Therefore, examinations of the factors contributing to psychological response to trauma appear to be especially important in this group. Some research suggests that menstrual cycle position at the time of trauma, and thus the endogenous ovarian hormonal milieu, influences the likelihood of experiencing traumatic flashback memories characteristic of PTSD (Bryant et al., 2010). The relationship between exogenous hormone administration and the psychological response to trauma seems warranted as well, as EC is routinely administered in the aftermath of sexual assault. While both Plan B and Ogestrel appear to be equally effective at preventing pregnancy, if one form of EC is associated with better subsequent psychological outcomes, it would appear that this form of EC may be preferential. While the present results suggest that Ogestrel is associated with lower levels of distressing intrusive symptoms than is Plan B, it is important that studies be done in efforts to confirm or refute the present results in order to best guide standardized procedures in the treatment of sexual assault survivors.
ACKNOWLEDGMENTS
This study was supported by National Institute of Mental Health Grant RO1-57508 to L.C. The authors wish to acknowledge the fantastic office staff of Forensic Nurse Specialists, Inc.—Diane Havron, Jennifer Hastings, and Elaine Pantano—for their extensive help. Without them this study would not have been possible.
Contributor Information
Nikole Kirin Ferree, Department of Neurobiology and Behavior, University of California, Irvine, 949-824-3813, nferree@uci.edu
Malinda Wheeler, Director- Forensic Nurse Specialists, Inc., Los Alamitos, Ca., 562-430-6220, Fax- 562-431-3947, malinda@fnsinc.org.
Larry Cahill, Department of Neurobiology and Behavior, Center for the Neurobiology of Learning and Memory, University of California, Irvine, 949-824-1937, lfcahill@uci.edu
REFERENCES
- Altemus M. Sex differences in depression and anxiety disorders: Potential biological determinants. Hormones and Behavior. 2006;50:534–538. doi: 10.1016/j.yhbeh.2006.06.031. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-IV-TR. Washington, D.C: Author; 2000. [Google Scholar]
- Berger W, Mendlowicz MV, Marques-Portella C, Kinrys G, Fontanelle LF, Marmar CR, Figueira I. Pharmacologic alternatives to antidepressants in posttraumatic stress disorder: a systematic review. Progress in Neuropsychopharmacology and Biological Psychiatry. 2009;33(2):169–180. doi: 10.1016/j.pnpbp.2008.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and Posttraumatic Stress Disorder in the community: The 1996 Detroit area survey of trauma. Archives of General Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Breslau N. Outcomes of posttraumatic stress disorder. Journal of Clinical Psychiatry. 2001;62(Suppl. 17):55–59. [PubMed] [Google Scholar]
- Brewin CR. Systematic review of screening instruments for adults at risk of PTSD. Journal of Traumatic Stress. 2005;18(1):53–62. doi: 10.1002/jts.20007. [DOI] [PubMed] [Google Scholar]
- Briere J, Elliott DM. Clinical utility of the Impact of Event Scale: Psychometrics in the general population. Assessment. 1998;5:171–180. doi: 10.1177/107319119800500207. [DOI] [PubMed] [Google Scholar]
- Bryant RA, Felmingham KL, Silove D, Creamer M, O’Donnell M, McFarlane AC. The association between menstrual cycle and traumatic memories. Journal of Affective Disorders. 2010;131:398–401. doi: 10.1016/j.jad.2010.10.049. [DOI] [PubMed] [Google Scholar]
- Campbell R, Wasco SM. Understanding rape and sexual assault: 20 years of progress and future directions. Journal of Interpersonal Violence. 2005;20(1):127–131. doi: 10.1177/0886260504268604. [DOI] [PubMed] [Google Scholar]
- Durand M, del Carmen Cravioto M, Raymond EG, Duran-Sanchez O, De la Luz Cruz-Hinojosa M, Castell-Rodriguez A, Schiavon R, Larrea F. On the mechanism of action of short-term levonorgestrel administration in emergency contraception. Contraception. 2001;64:227–234. doi: 10.1016/s0010-7824(01)00250-5. [DOI] [PubMed] [Google Scholar]
- Ferree NK, Cahill L. Post-event spontaneous intrusive recollections and strength of memory for emotional events in men and women. Consciousness and Cognition. 2009;18:126–134. doi: 10.1016/j.concog.2008.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferree NK, Kamat R, Cahill L. Influences of menstrual cycle position and sex hormone levels on spontaneous intrusive recollections following emotional stimuli. Consciousness and Cognition. 2011;20:1154–1162. doi: 10.1016/j.concog.2011.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frans Ö, Rimmö P-A, Åberg L, Frederickson M. Trauma exposure and post-traumatic stress disorder in the general population. Acta Psychiatrica Scandinavica. 2005;111:291–299. doi: 10.1111/j.1600-0447.2004.00463.x. [DOI] [PubMed] [Google Scholar]
- Frye CA. An overview of oral contraceptives: Mechanism of action and clinical use. Neurology. 2006;66(Suppl 3):S29–S36. doi: 10.1212/wnl.66.66_suppl_3.s29. [DOI] [PubMed] [Google Scholar]
- Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: A measure of subjective stress. Psychosomatic Medicine. 1979;41(3):209–218. doi: 10.1097/00006842-197905000-00004. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic Stress Disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Leung VWY, Levine M, Soon JA. Mechanisms of action of hormonal emergency contraceptives. Pharmacotherapy. 2010;30(2):158–168. doi: 10.1592/phco.30.2.158. [DOI] [PubMed] [Google Scholar]
- Milad MR, Goldstein JM, Orr SP, Wedig MM, Klibanski A, Pitman RK, Rauch SL. Fear conditioning and extinction: Influence of sex and menstrual cycle in healthy humans. Behavioral Neuroscience. 2006;120(5):1196–1203. doi: 10.1037/0735-7044.120.5.1196. [DOI] [PubMed] [Google Scholar]
- Neal LA, Busuttil W, Rollins J, Herepath R, Strike P, Turbull G. Convergent validity of measures of post-traumatic stress disorder in a mixed military and civilian population. Journal of Traumatic Stress. 1994;7(3):447–455. doi: 10.1007/BF02102789. [DOI] [PubMed] [Google Scholar]
- Perry S, Difede J, Musngi G, Frances AJ, Jacobsberg L. Predictors of posttraumatic stress disorder after burn injury. American Journal of Psychiatry. 1992;149:931–935. doi: 10.1176/ajp.149.7.931. [DOI] [PubMed] [Google Scholar]
- Rasmusson AM, Friedman MJ. Gender issues in the neurobiology of PTSD. In: Kimmerling R, Oimette P, Wolfe J, editors. Gender and PTSD. New York: The Guilford Press; 2002. pp. 43–75. [Google Scholar]
- Resnick H, Acierno R, Waldrop AE, King L, King D, Danielson C, Ruggiero KJ, Kilpatrick D. Randomized controlled evaluation of an early intervention to prevent post-rape psychopathology. Behavior Research and Therapy. 2007;45:2432–2447. doi: 10.1016/j.brat.2007.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts N, Kitchiner N, Kenardy J, Bisson J. Multiple session early psychological interventions for the prevention of post-traumatic stress disorder. Cochrane Database of Systematic Reviews. 2009 Jul;8(3):CD006869. doi: 10.1002/14651858.CD006869.pub3. 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saxe G, Wolfe J. Gender and posttraumatic stress disorder. In: Saigh PA, Bremner JD, editors. Posttraumatic stress disorder: A comprehensive text. Boston: Allyn & Bacon; 1999. pp. 160–179. [Google Scholar]
- Shalev AY, Peri T, Canetti L, Schreiber S. Predictors of PTSD in injured trauma survivors: a prospective study. American Journal of Psychiatry. 1996;153:219–225. doi: 10.1176/ajp.153.2.219. [DOI] [PubMed] [Google Scholar]
- Sundin EC, Horowitz MJ. Horowitz’s Impact of Event Scale: Evaluation after 20 years of use. Psychosomatic Medicine. 2003;65:870–876. doi: 10.1097/01.psy.0000084835.46074.f0. [DOI] [PubMed] [Google Scholar]
- Tirelli A, Cagnacci A, Volpe A. Levonorgestrel administration in emergency contraception: bleeding pattern and pituitary-ovarian function. Contraception. 2008;77:328–332. doi: 10.1016/j.contraception.2008.01.013. [DOI] [PubMed] [Google Scholar]
- Tjaden P, Thoennes N. NCJ210346. Washington, DC: National Institute of Justice, US Department of Justice; 2006. Extent, nature, and consequences of rape victimization: Findings from the National Violence Against Women Survey. [Google Scholar]
- Tolin DF, Foa EB. Sex differences in trauma and Posttraumatic Stress Disorder: A quantitative review of 25 years of research. Psychological Bulletin. 2006;132(6):959–992. doi: 10.1037/0033-2909.132.6.959. [DOI] [PubMed] [Google Scholar]
- Zinzow HM, Resnick HS, Mccauley JL, Amstadter AB, Ruggiero KJ, Kilpatrick DG. Prevalence and risk of psychiatric disorders as a function of variant rape histories: Results from a national survey of women. Social Psychiatry and Psychiatric Epidemiology. 2011 doi: 10.1007/s00127-011-0397-1. [DOI] [PMC free article] [PubMed] [Google Scholar]