Abstract
Despite the known deficits in sleep that occur during adolescence and the high prevalence of substance use behaviors among this group, relatively little research has explored how sleep and substance use may be causally related. The purpose of this study was to explore the longitudinal bi-directional relationships between sleep duration, sleep patterns and youth substance use behaviors. Participants included 704 mostly white (86.4 %) youth, 51 % female, with a baseline mean age of 14.7 years. Self-reported substance use behaviors included past month alcohol, cigarette, and marijuana use. Sleep measures included sleep duration on weekends and weekdays, total sleep, weekend oversleep, and weekend sleep delay. Cross-lagged structural equation models, accounting for clustering at the school level, were run to determine the longitudinal association between sleep and substance use adjusting for socio-demographic characteristics, pubertal status, body mass index z-score, and depressive symptoms. Cigarette use and weekend sleep were bi-directionally related as were marijuana use and total sleep. No other bidirectional associations were identified. However, alcohol use predicted shorter weekend oversleep and marijuana use predicted increased weekend sleep and weekend oversleep. Sleep patterns and duration also predicted adolescents’ cigarette, alcohol, and marijuana use. Sleep, both patterns and duration, and substance use among youth are intertwined. Future research is needed to explore these bidirectional relationships, as well as other important contextual factors that may moderate these associations.
Keywords: Substance use, Sleep, Adolescents, Youth, Cross-lagged models
Introduction
Substance use rates remain high among youth. Recent national data from the Youth Risk Behavior Survey suggest that 39 % of 9–12th grade students have used alcohol, 18 % have smoked cigarettes, and 23 % of students have used marijuana at least once during the past month (Centers for Disease Control and Prevention 2012). Given these high prevalence rates of youth substance use, it is important to determine what factors continue to put youth at increased risk for engaging in these behaviors. One understudied factor that may be related to substance use is sleep. Sleep patterns and sleep duration change throughout adolescence, likely to the detriment of positive adolescent functioning. Previous research suggests correlations between late bed times and lower grades in school (Carskadon et al. 1998), reduced sleep and higher levels of depressive symptoms, lower levels of self-esteem (Fredriksen et al. 2004), as well as higher levels of substance use (O’Brien and Mindell 2005; Pasch et al. 2010). However, the research on sleep and substance use in adolescence has been limited primarily to studies of the impact of sleep problems, which overlooks the multidimensionality of sleep and is limited to only the highest risk adolescents. Furthermore, much of the research on sleep and substance use in adolescence has been cross-sectional, which prevents an understanding of the causal mechanisms and the temporal associations between sleep and substance use. Our purpose in this study is to examine the bi-directional longitudinal relationships between sleep duration, sleep patterns, and substance use in adolescence.
Sleep in adolescence is an important public health issue, as sleep has been cited to be particularly important during periods of brain maturation, such as the period of adolescence (Dahl and Lewin 2002). Only 20 % of teens sleep the recommended nine hours on school nights and 45 % sleep less than eight hours on weeknights (National Sleep Foundation 2006). While research suggests that youth may make up for lost sleep during the week on the weekends (Szymczak et al. 1993; Strauch and Meier 1988), this weekend sleep compensation may not be enough. Longitudinal data have shown that, as youth mature, they tend to have later bedtimes, earlier waking times, and increased variation in weeknight and weekend sleep schedules, likely due to social and biological changes (Strauch and Meier 1988; Wolfson and Carskadon 1998). As sleep is necessary for optimal physical and mental functioning, and given that teens are especially vulnerable to decreased amounts of sleep, this sleep deficit may be especially problematic due to crucial development processes that take place during this life stage.
Sleep, however, is multifaceted and includes sleep problems, sleep patterns and sleep duration. Sleep problems refer to having trouble falling or staying asleep and may also include sleep quality and day time tiredness. Sleep patterns refer to the times youth go to sleep and wake up and the consistency of those patterns across weekdays and weekends. Sleep patterns may be particularly important for adolescents as they frequently cycle between earlier wake/bed times (on school days) and later wake/bed times (on weekends). However, the circadian system does not adapt quickly to these frequent changes, which may result in increased risk for negative outcomes as these rapid pattern changes may lead to sleep deprivation and impaired functioning (Dahl and Lewin 2002). One possible outcome of sleep deprivation is deficits in the ability to self-regulate emotions and behaviors (Dahl and Lewin 2002). Finally, sleep duration refers to the length of sleep which, for many adolescents, varies between weekdays and weekends. Adolescents who are sleep deprived, or have a limited sleep duration, are more likely to have impairments on memory tasks (Carskadon et al. 1981), cognitive and emotional processing (Dahl and Lewin 2002; Wong et al. 2004), and neurobehavioral functioning (Sadeh et al. 2002). Because short sleep duration is common among adolescents during the weekday, sleep deprivation may develop, leading to further problems with sleep and mood regulation (Dahl and Lewin 2002). Therefore, it is important that an understanding of the associations between sleep and well-being in adolescence incorporate the multiple dimensions of sleep.
Most research on the relationships between sleep and substance use among youth has been primarily cross-sectional and has examined sleep problems (Johnson and Breslau 2001; Vignau et al. 1997; Phillips and Danner 1995; Tynjala et al. 1997), although there have been a few studies to examine sleep duration or sleep patterns and risk-taking behavior. An examination of sleep duration and risk-taking behavior among high school students revealed that students who reported the least amount of sleep on school nights and those with the largest difference between weekday and weekend bedtimes had higher levels of risk-taking behavior (O’Brien and Mindell 2005). In another cross-sectional study, youth who had lower amounts of weekday sleep had higher rates of past month alcohol use and drunkenness (Pasch et al. 2010). Additionally, youth with greater weekend delays (later bed time on the weekend than weekday) and weekend oversleeps (later wake time on the weekend than weekday) were more likely to engage in a range of risk behaviors including substance use (Pasch et al. 2010). Significant associations have been found between increased alcohol consumption and a lower weekday sleep duration, as well as increased smoking and lower weekend sleep duration among a sample of Brazilian young adults (Fischer et al. 2008). Similarly, in another study, adolescent smokers were found to sleep significantly less than non-smokers (Townsend et al. 1991). Cross-sectional research has demonstrated that multiple facets of sleep, including sleep problems, patterns, and duration, are associated with substance use in adolescence.
In order to establish the temporality of the association between sleep and substance use, longitudinal studies are needed. In fact, Sadeh et al. (2009) cite the “dearth of longitudinal studies” among adolescents (p. 1602). The longitudinal, causal relationships between these two factors are important to establish as practitioners who work with adolescents, as well as parents, may benefit from understanding the early warning signs of those factors that may lead to substance use (i.e., sleep duration and patterns) or to reductions in sleep duration or changes in the sleep patterns (i.e., substance use). Most longitudinal studies that have examined sleep and risk behaviors in children and adolescents primarily have examined sleep disturbance (Wetter and Young 1994), sleep difficulty (Wong et al. 2004; Wong et al. 2010; Wong et al. 2009), insomnia (Roberts et al. 2002; Roberts et al. 2009), and overtiredness (Wong et al. 2010). Sleep disturbances and sleep problems are important aspects of sleep; however, data from a national survey found that only approximately 6 % of adolescents surveyed experienced sleep problems (Johnson and Breslau 2001). Therefore, it is important to understand better the relationships between sleep and substance use, to explore how sleep patterns and sleep duration, two exposures experienced by all youth, may be related longitudinally to substance use. However, little research has explored the longitudinal relationships between sleep duration or sleep patterns and substance use, and, to our knowledge, no studies have explored the bi-directional associations between substance use and sleep in youth.
Hypotheses
Sleep and substance use among youth may be related through two mechanisms. First, those who have short sleep durations may chronically be functioning with a level of sleep deprivation. As such, their capacity to regulate emotions and manage day to day tasks may be diminished (Dahl 1996; Dahl and Lewin 2002). This is problematic as difficulties with emotion regulation may contribute to substance use (Wills et al. 2001). Additionally, over the long term, youth with shortened sleep duration, due to limited sleep on weekdays, and possibly frequent pattern changes leading to problems with circadian rhythms, may have difficulties with executive functioning tasks such as response inhibition and problem solving (Wong et al. 2010), that also have been found to increase the likelihood of substance use. Consequently, sleep may contribute to substance use through the dysregulation of executive functioning mechanisms. However, the use of substances, such as cigarettes, alcohol or marijuana, may lead to reduced sleep duration, particularly on weekdays, as well as larger sleep pattern differences between weekdays and weekends. These sleep duration reductions and pattern changes may be due to the effects of the substances on development. Among adolescents, an additive effect has been found for alcohol use and sleep deprivation particularly on motor coordination and cognitive functioning (Dahl and Lewin 2002). This additive effect may then perpetuate the alcohol use to sleep causal relationship. Similar mechanisms also may be at play for cigarette or marijuana use. Additionally, substance use has been found to affect sleep negatively (Hasler et al. 2012). As such, substance use may contribute to sleep changes through biological mechanisms.
Given the lack of longitudinal studies exploring the associations between sleep duration, sleep patterns and substance use among youth, the purpose of the present study was to examine the longitudinal bi-directional associations between youth sleep, including both sleep patterns and duration, and substance use across a 2-year period. Cross-lagged models, or bi-directional models, allow for the simultaneous exploration of cross-sectional and longitudinal pathways between variables. It has been suggested that longitudinal, bi-directional models are needed to understand better the sleep and substance use relationship (Hasler et al. 2012). In the current study, cross-lagged models will help us to understand better both the clustering of these two key behaviors in adolescence as well as further our knowledge about the longitudinal impacts each of these variables has on the other. It is hypothesized that sleep and substance use are related; however, given the limited longitudinal research that explores the bi-directional pathways, the directionality of the associations is not hypothesized.
Methods
Participants in this study are from two independent longitudinal samples of adolescents and one parent who took part in either the IDEA (Identifying the Determinants of Eating and Activity) or ECHO (Etiology of Childhood Obesity) cohort studies, both of which were conducted in the Twin Cities Metropolitan Area of Minnesota. IDEA and ECHO were both 2-year longitudinal studies whose purpose was to understand the social and environmental influences on unhealthy weight gain during adolescence (Lytle 2009). Baseline data for the present study were collected in 2006–2007 (IDEA) and 2007–2008 (ECHO) and follow-up data collected in 2008–2009 (IDEA) and 2009–2010 (ECHO). For both studies, parent/adolescent pairs were excluded from participating in either study if they planned to move from the area in the next 3 years, had a medical condition that affected their growth (e.g., hypo/hyperthyroidism), were non-English speaking, and/or had any other physical or emotional condition that would affect their diet/activity levels or make it difficult to complete surveys or measurements. All study protocols were approved by the University of Minnesota Institutional Review Board.
IDEA participants (n = 349, age range 10.8–17.7) were recruited from (1) an existing cohort of youth participating in the Minnesota Adolescent Community Cohort (MACC) Tobacco Study (Widome et al. 2007), (2) a Minnesota Department of Motor Vehicle (DMV) list restricted to the 7-county metro area, and (3) a convenience sample drawn from local communities. A total of 26 % of the youth were recruited from the MACC cohort, 49 % were recruited from the DMV sample, and 25 % were recruited from the convenience sample. Recruitment for MACC was carried out from a random sample of 60 geographical and political units (GPU) (out of a total of 129), which were created to provide a sample of the local tobacco control environments in Minnesota. A total of 3,637 teens divided into five age-based cohorts (i.e., 12, 13, 14, 15, 16), with approximately 725 youth in each were recruited and followed over time. Recruitment letters for the IDEA study, a total of 506, were mailed to the MACC cohort and their age-eligible siblings beginning in August 2006 and continuing through March 2007. A total of 328 youth completed both baseline and 2-year follow-up survey resulting in a 94 % response rate.
The ECHO study (n = 374) also included youth (ages 11.0–17.6) and one parent/guardian, and these participants were recruited from the membership of HealthPartners® (HP) health plan. The recruitment strategy was designed to recruit a racially-diverse sample of adolescents that represented both healthy weight and overweight individuals in the seven-county metropolitan area of Minneapolis/St. Paul, Minnesota. To be eligible, youth had to be current HP members, in grades 6th through 11th in the fall of 2007, living in one of the randomly selected middle or high-school districts included in the sample, have a parent willing to participate and be willing to allow their names and contact information to be sent from HP to the study team at the University of Minnesota for further eligibility screening, consent and measurement. A total of 320 youth completed both baseline and 2-year follow-up survey resulting in an 85.6 % response rate. Additional details about recruitment have been published elsewhere (Pasch et al. 2012).
The measures collected in both the IDEA and ECHO studies were identical for all participants. Using identical measures was done for the purpose of combining data from the two studies in order to provide a larger, more racially and economically diverse sample. The combined sample included 723 adolescents. Adolescent participants were 14.7 years of age on average at baseline (range 10–17), approximately 49 % were male, 86 % were White, 5.3 % African-American, 1 % Asian, 0.1 % Native Hawaiian/Pacific Islander, 0.4 % American Indian, 6.3 % other race/ethnicity and 12 % received free or reduced cost lunch. Approximately 5 % of the sample indicated they were of Latino or Hispanic or Mexican-American or Spanish origin in a separate question similar to the question used in the US Census. Table 1 includes demographic data for each sample at baseline and 2-year follow-up, as well as for the combined sample. The present study uses cohort data from baseline and the 2-year follow-up.
Table 1.
Descriptive data on sleep, substance use, and covariates, by sample and data collection wave (N = 704)
| Combined sample | IDEA sample | ECHO sample | ||||
|---|---|---|---|---|---|---|
| Baseline | Follow-up | Baseline | Follow-up | Baseline | Follow-up | |
| Sleep variables, M (SD) | ||||||
| Weekday sleep | 8.26 (1.12) | 8.08 (1.20) | 8.05 (1.04)a | 8.11 (1.26) | 8.45 (1.16)a | 8.04 (1.47) |
| Weekend sleep | 9.62 (1.42) | 9.34 (1.39) | 9.49 (1.43)b | 9.22 (1.39)b | 9.74 (1.40)b | 9.47 (1.39)b |
| Total sleep | 60.50 (7.09) | 59.06 (7.38) | 59.25 (6.66)a | 58.97 (7.69) | 61.70 (7.29)a | 59.14 (7.04) |
| Weekend delay | 1.52 (1.08) | 1.55 (1.09) | 1.57 (1.01) | 1.60 (1.03) | 1.46 (1.14) | 1.49 (1.16) |
| Weekend oversleep | 2.89 (1.54) | 2.79 (1.63) | 3.01 (1.53)b | 2.68 (1.64) | 2.76 (1.55)b | 2.90 (1.63) |
| Substance use (proportion) | ||||||
| Cigarette use | 5.1 % | 15.0 % | 7.0 %b | 17.9 %b | 3.3 %b | 12.0 %b |
| Alcohol use | 11.7 % | 36.8 % | 18.6 %a | 44.8 %a | 5.0 %a | 29.3 %a |
| Marijuana use | 3.1 % | 13.1 % | 4.1 % | 16.0 %b | 2.2 % | 10.1 %b |
| Covariates | ||||||
| Age, M (SD) | 14.68 (1.83) | 16.65 (1.85) | 15.40 (1.70)a | 17.38 (1.73)a | 13.99 (1.67)a | 15.91 (1.68)a |
| Female | 51.1 % | 50.7 % | 51.5 % | |||
| White | 86.4 % | 93.6 %a | 79.4 %a | |||
| Pubertal status, M (SD) | 2.90 (.73) | 3.04 (.67)a | 2.77 (0.76)a | |||
| Parent education, M (SD) | 4.96 (1.14) | 4.99 (1.12) | 4.92 (1.00) | |||
Comparison of studies differed significantly p < 0.001
Comparison of studies differed significantly p ≤ 0.05
Measures
Youth and one parent completed self-reported surveys and had their height and weight objectively measured by trained clinic staff. At the start of the visit, parents and youth were both given informed consent/assent forms to read and sign. Youth completed a self-report survey, in a separate room from their parents, which included questions on substance use and sleep as part of a larger survey to assess a broad range of adolescent health behaviors as well as the etiology of child/adolescent obesity. Parents also completed a self-report survey; however, only a measure of parental education from this survey was used for the present study.
Sleep Duration
Sleep duration was assessed by the time students usually went to bed (turned out the lights in order to go to sleep) and usually got out of bed in the morning on a typical weekday and weekend. These items, adapted from the Night Eating Diagnostic Scale (Gluck et al. 2001), were then used to compute weekday and weekend sleep duration. To measure total week sleep, a summary score of weekday sleep (multiplied by five) and weekend sleep (multiplied by two) was calculated. Similar questions have been used successfully with adolescents in previous studies (Laberge et al. 2001; Lee et al. 1999; Wolfson 1996) and have been significantly correlated with measures of sleep using both diary and sleep actigraphy measures (Wolfson et al. 2003).
Sleep Patterns
Weekend sleep delay was calculated by subtracting when youth went to sleep on weekdays from when s/he went to sleep on weekends. A larger value for weekend sleep delay indicates a later weekend bedtime. Weekend oversleep was calculated by subtracting when the youth woke up on weekdays from when s/he woke up on weekends. A larger value for weekend oversleep indicates a later weekend wake-time.
Tobacco Use
Tobacco use was assessed with one question that asked how much the student currently smoked with 10 response options ranging from “I don’t smoke” to “a pack or more each day.” The response options were recoded so that those who indicated any use of cigarettes in the past month were coded as “1” and all others were coded as “0.” This item has been used previously with youth (Johnston et al. 1998).
Alcohol Use
Alcohol use was assessed with one question that asked how many times in the past month they had alcohol to drink, including beer, wine, and liquor, but not including sips, with response options ranging from 0 to 40 or more times. The response options were recoded so that those who indicated any use of alcohol in the past month were coded as “1” and all others were coded as “0.” This item has been used previously with youth (Johnston et al. 1998).
Marijuana Use
Marijuana use was assessed by asking students to report the number of times they used marijuana in the past month with response options ranging from 0 to 40 or more times. The response options were recoded so that those who indicated any use of marijuana in the past month were coded as “1” and all others were coded as “0.” This item has been used previously with youth (Johnston et al. 1998).
Socio-Economic Status
A proxy measure of socio-economic status was included using parent’s highest level of education and was assessed on the parent survey. This one item question asked “Among all of the adults in your home, what is the highest level of education completed?” Response options included “Did not finish high school,” “Finished high school (or got a GED),” “Went to vocational school (computer/electrician/mechanic/healthcare/beauty school),” “Took some college (but did not graduate),” “Graduated from college or a university,” “Professional training beyond a 4-year college degree.” Socio-economic status was used as a continuous covariate (values 1–6) due to previously documented associations with substance use (Goodman and Huang 2002).
Race/Ethnicity
Race/ethnicity was measured with one item asking “Do you think of yourself as…? (Check ALL that apply).” Response options included “White,” “Black or African-American,” “Asian,” “Native Hawaiian or other Pacific Islander,” American Indian or Alaskan Native,” “Other,” and “I don’t know.” Race was dichotomized into White/Non-White. Race was included as a covariate as there are racial/ethnic differences in the prevalence of substance use (Shih et al. 2010).
Gender
Gender was assessed with one question where the youth indicated if s/he male or female and was coded with female = 1 and male = 0. Gender differences have been found for both substance use (Eaton et al. 2010) and sleep (Fredriksen et al. 2004; Laberge et al. 2001; Lee et al. 1999).
Age
Youth completed a question that asked them to indicate their birthdates including day, month, and year. Age at the time of survey completion was then calculated by subtracting the birthdate from the date of the survey and used as a continuous covariate due to differences in age for both substance use (Eaton et al. 2010) and sleep (Carskadon et al. 1993; Wolfson 1996).
Pubertal Development
Pubertal development was measured with the 5-item self-report Pubertal Development Scale (Petersen et al. 1988) and was included as a continuous covariate. Puberty was included as a covariate as previous research has found that those who develop early are more likely to be substance users (Patton and Viner 2007) and that pubertal development is associated with sleep (i.e., those who are more developed are more likely to have later bedtimes) (Dahl and Lewin 2002; Carskadon et al. 1993; Sadeh et al. 2009). Additionally, those adolescents going through puberty may require increased sleep as they go through this developmental change (Dahl and Lewin 2002). As this variable may be related to both sleep and substance use, it was included as a covariate to remove possible confounding effects in the relationship between sleep and substance use.
Body Mass Index z-Score
Trained staff also measured each participant’s height using a Shorr height board (Irwin Shorr, Olney, MD, USA), and weight using a Tanita scale, a bioelectrical impedance device that assesses body weight, lean and fat mass (TanitaTBF-300A Body Composition Analyzer, Arlington Heights, IL, USA). The objectively measured height and weight values were transformed into body mass index for age z-scores (BMI z-score) using national reference data (Kuczmarski et al. 2002). A BMI z-score represents body measurements in standard deviation units, or deviations from the mean. BMI z-score allows for the comparison across ages as well as the relative weight status of youth at the distribution extremes (Kuczmarski et al. 2002). BMI z-score was included as a continuous covariate as it has been associated with both substance use such that greater alcohol, tobacco, and other drug use has predicted a greater BMI z-score (Pasch et al. 2008; Pasch et al. 2012) and greater alcohol use has predicted a decreased BMI z-score (Pasch et al. 2012). Additionally, sleep has been associated with a greater body mass index or overweight status (Cappuccio et al. 2008; Patel and Hu 2008; Patel et al. 2006; Lytle et al. 2011). Given the associations between sleep, substance use, and BMI, BMI z-score was included as a covariate to rule out possible extraneous associations in the relationship between sleep and substance use.
Depressive Symptoms
Depressive symptoms were measured using the 6-item Kandel-Davies scale (Kandel and Davies 1982). Depressive symptoms have previously documented associations with both substance use, as increased substance use has been associated with an increased risk for depressive symptoms (Hallfors et al. 2005) and sleep, as increased depressive symptoms have been associated with shorter sleep duration and greater sleep pattern differences (Pasch et al. 2010). To control for the effects of depressive symptoms on both sleep and substance use, this variable was included as a continuous covariate.
Data Analyses
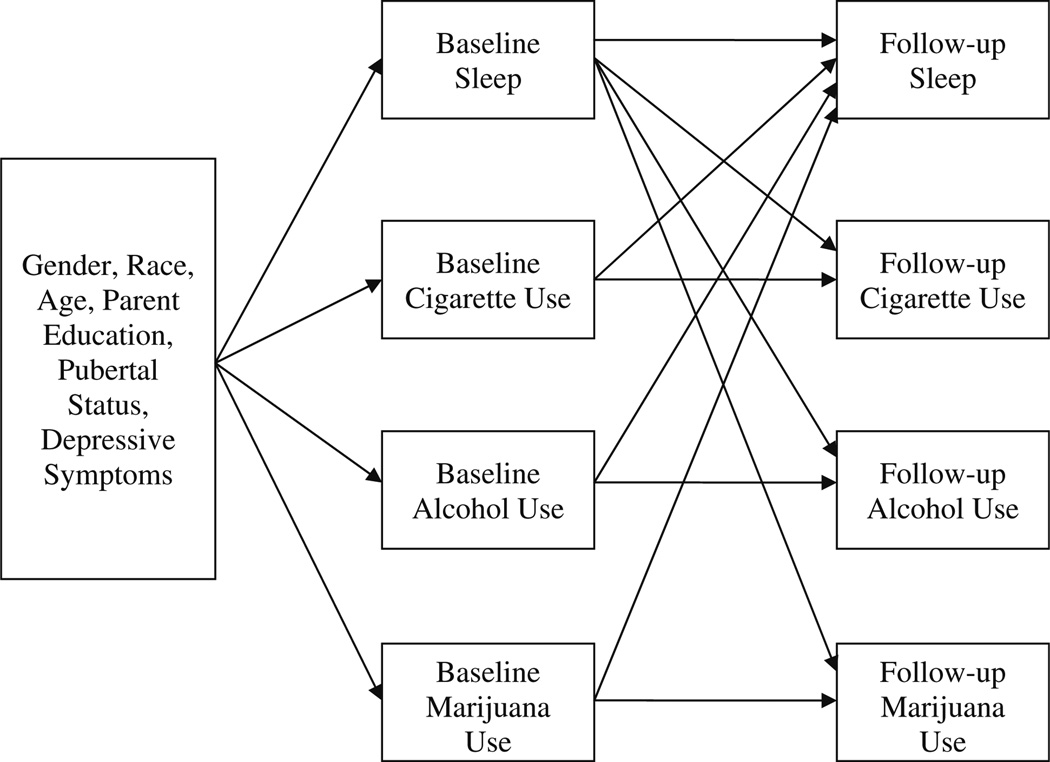
An autoregressive cross-lagged (ARCL) model was tested using MPlus 6.1 (Muthén & Muthén 1998–2010) to determine the bi-directional relationships between sleep and substance use (Bollen and Curran 2006) across a 2-year time period. This type of structural equation model tests the significance of the cross-lagged paths (i.e., baseline substance use to follow-up sleep and baseline sleep to follow-up substance use) while controlling for across-time stability of the variables of interest as well as covariates. MPlus also can account for potential clustering; school was used as the clustering variable. Six models were fit, one for each sleep variable of interest (Fig. 1). The decision was made to look at each sleep variable separately rather than in one model because of the interdependence between the variables (i.e., the sleep pattern variables were based on the sleep duration variables). Cross-lagged paths were tested by estimating three paths from baseline sleep to the three follow-up substance use variables (cigarettes, alcohol, and marijuana) and by estimating three paths from the three baseline substance use variables to follow-up sleep. Cross-stability paths were tested by estimating four paths from the baseline sleep and substance use variables to the equivalent follow-up variables. The interpretation of the cross-lagged paths is thus the influence of the baseline measure “above and beyond the influence” of the cross-stability path (Bollen and Curran 2006). The covariates of interest were controlled for by adding paths to the baseline sleep and substance use measures. The sleep and substance use measures were allowed to co-vary at both baseline and follow-up to account for potential cross-sectional relationships between the variables.
Fig. 1.
Conceptual model showing the cross-lagged relationship between sleep and substance use. Figure does not present covariance paths between the sleep variable and the three substance use variables at both time points
MPlus is able to include both dichotomous (substance use) and continuous (sleep) variables as outcomes, but to accommodate for the dichotomous outcomes the weighted least-squares with mean and variance adjustment (WLSMV) estimator was used (Muthén & Muthén 1998–2010). Participants missing information on the exogenous covariates (age, gender, race, parent education, pubertal status, or depressive symptoms) were excluded from analyses (N = 19), leaving a final sample size of 704. Several criteria were used to assess the fit of the two models: the χ2 statistic; the Tucker-Lewis Index (TLI) and the Comparative Fit Index (CFI), both of which are recommended to be .95 or higher; and the Root Mean Squared Error of Approximation (RMSEA), which is recommended to be .06 or lower (Hu and Bentler 1999).
Results
Relationships Between Demographic Variables and Substance Use at Baseline
Older youth and those with higher levels of depressive symptoms were more likely to be using cigarettes, alcohol, and marijuana at baseline, while females were less likely to be using any of the three substances at baseline (see Table 2). Youth who were more advanced in their pubertal development at baseline were more likely to be using cigarettes.
Table 2.
Standardized path coefficients, by sleep variable (N = 704)
| Weekday sleep |
Weekend sleep |
Total sleep |
Weekend sleep delay |
Weekend oversleep |
|
|---|---|---|---|---|---|
| Control paths | |||||
| Gender (0 = male, 1 = female) → sleep | .04 | .08 | .06 | −.10* | −.02 |
| Race (0 = white, 1 = non-white) → sleep | −.02 | −.07 | −.04 | .18*** | .09** |
| Age → Sleep | −.45*** | −.20*** | −.44*** | .22*** | .31*** |
| Depressive symptoms → sleep | −.18*** | −.09** | −.17*** | .04 | .06 |
| Pubertal status → sleep | −.11* | −.02 | −.10 | .03 | .07 |
| Parent education → sleep | −.03 | .01 | −.02 | −.13*** | −.08* |
| BMIZ → sleep | −.08* | −.11** | −.11*** | .11** | .03 |
| Gender (0 = male, 1 = female) → cigarette use | −.40*** | −.38*** | −.41*** | −.35*** | −.34*** |
| Race (0 = white, 1 = non-white) → cigarette use | −.05 | −.07 | −.06 | −.08 | −.08 |
| Age → cigarette use | .22* | .27** | .22* | .25** | .28** |
| Depressive symptoms → cigarette use | .28*** | .27*** | .28*** | .26*** | .26*** |
| Pubertal status → cigarette use | .29* | .29* | .29* | .28* | .29* |
| Parent education → cigarette use | −.05 | −.03 | −.05 | −.13 | −.02 |
| BMIZ → cigarette use | .04 | .06 | .04 | .03 | .06 |
| Gender (0 = male, 1 = female) → alcohol use | −.11 | −.13* | −.12* | −.11 | −.12* |
| Race (0 = white, 1 = non-white) → alcohol use | .02 | .03 | .03 | .01 | .01 |
| Age → alcohol use | .57*** | .58*** | .57*** | .57*** | .58*** |
| Depressive symptoms → alcohol use | .14** | .16*** | .15** | .15** | .15*** |
| Pubertal status → alcohol use | .12 | .12 | .12 | .12 | .12 |
| Parent education → alcohol use | −.08 | −.08 | −.08* | −.07 | −.06 |
| BMIZ → alcohol use | −.02 | −.02 | −.02 | −.03 | −.02 |
| Gender (0 = male, 1 = female) → marijuana use | −.34*** | −.32*** | −.32*** | −.37*** | −.38*** |
| Race (0 = white, 1 = non-white) → marijuana use | −.05 | −.03 | −.06 | −.00 | .01 |
| Age → marijuana use | .30** | .30*** | .30** | .35*** | .30** |
| Depressive symptoms → marijuana use | .18*** | .19*** | .18*** | .22*** | .22*** |
| Pubertal status → marijuana use | .13 | .15 | .14 | .16 | .14 |
| Parent education → marijuana use | −.03 | −.05 | −.03 | −.05 | −.06 |
| BMIZ → marijuana use | .01 | −.02 | .00 | .05 | .01 |
| Covariance paths | |||||
| Cigarette use baseline ↔ alcohol use baseline | .61*** | .57*** | .60*** | .59*** | .59*** |
| Cigarette use baseline ↔ marijuana use baseline | .76*** | .80*** | .78*** | .72*** | .72*** |
| Alcohol use baseline ↔ marijuana use baseline | .61*** | .66*** | .61*** | .62*** | .64*** |
| Sleep baseline ↔ cigarette use baseline | −.05 | .04 | −.02 | .30*** | .31*** |
| Sleep baseline ↔ alcohol use baseline | −.14* | −.04 | −.14* | .16* | .14* |
| Sleep baseline ↔marijuana use baseline | −.02 | −.04 | −.05 | .34*** | .23*** |
| Cigarette use follow-up ↔ alcohol use follow-up | .58*** | .62*** | .58*** | .59*** | .61*** |
| Cigarette use follow-up ↔ marijuana use follow-up | .78*** | .72*** | .75*** | .87*** | .86*** |
| Alcohol use follow-up ↔Marijuana use follow-up | .81*** | .76*** | .81*** | .78*** | .76*** |
| Sleep follow-up ↔ cigarette use follow-up | −.02 | .18 | .04 | .23 | .35** |
| Sleep follow-up ↔ alcohol use follow-up | .09 | −.08 | .05 | .32*** | .13* |
| Sleep follow-up ↔ marijuana use follow-up | −.16 | −.39* | −.25 | .10 | .07 |
| Stability paths (baseline → follow-up) | |||||
| Sleep | .38*** | .34*** | .45*** | .38*** | .27*** |
| Cigarette use | .79*** | .83*** | .78*** | .85*** | .69*** |
| Alcohol use | .71*** | .72*** | .71*** | .67*** | .88*** |
| Marijuana use | .81*** | .85*** | .81*** | .89*** | .85*** |
| Cross-lagged paths (baseline → follow-up) | |||||
| Sleep → cigarette use | −.14* | −.13* | −.17** | −.01 | −.08 |
| Sleep → alcohol use | −.03 | −.03 | −.04 | .12* | .08 |
| Sleep → marijuana use | −.19* | −.04 | −.17* | −.04 | .06 |
| Cigarette use → sleep | −.37 | −.58* | −.47* | −.31 | −.13 |
| Alcohol use → sleep | .13 | −.46* | .01 | −.09 | −.37* |
| Marijuana use → sleep | .45 | .98*** | .65** | .39 | .37* |
| Model information | |||||
| χ2 (df = 34, p value) | 47.73 (.06) | 49.86 (.04) | 47.79 (.06) | 42.50 (.15) | 43.35 (.13) |
| CFI | .99 | .98 | .99 | .99 | .99 |
| TLI | .97 | .96 | .97 | .98 | .98 |
| RMSEA | .02 | .03 | .02 | .02 | .02 |
p < .05;
p < .01;
p < .001
Relationships Between Demographic Variables and Sleep at Baseline
Females had lower baseline weekend sleep delays, indicating that males had a greater difference in their weekend and weekday bedtimes compared with females (see Table 2). Non-White youth had higher baseline weekend sleep delays and higher weekend oversleeps (larger difference between weekend and weekday wake time). Older youth had greater weekend sleep delays and weekend oversleeps, but lower levels of weekday sleep, weekend sleep, and total sleep at baseline than younger youth. Parent education was associated negatively with weekend sleep delay, such that youth whose parents had higher levels of education had a smaller difference between their weekday and weekend bedtimes.
Youth with higher baseline levels of depressive symptoms had lower baseline weekday sleep, weekend sleep, and total sleep at baseline. Additionally, youth who were more advanced in their pubertal development at baseline had less baseline weekday sleep. Finally, BMIZ was associated positively with weekend sleep delay, such that youth with a higher baseline BMIZ had a greater difference between their weekday and weekend bedtimes, but BMIZ was associated negatively with weekday sleep, weekend sleep, and total sleep.
Covariance Paths: Cross-Sectional Associations Between Variables
At both baseline and 2-year follow-up, cigarette, alcohol, and marijuana use were highly correlated (see Table 2). At baseline, use of each of the three substances was associated positively with weekend sleep delay and weekend oversleep, indicating that youth who were using cigarettes, alcohol, or marijuana had a larger discrepancy between their weekend and weekday bedtime and a later wake-up time on weekends than weekdays compared with youth who were not using these substances. Alcohol use at baseline was associated negatively with baseline weekday sleep and total sleep.
At 2-year follow-up there were fewer associations between sleep and substance use. Alcohol use was still associated positively with weekend sleep delay, and both alcohol and cigarette use were associated positively with weekend oversleep. Marijuana use was associated negatively with weekend sleep, indicating that, at follow-up, youth who were using marijuana slept less on the weekend than their non-using counterparts.
Stability Paths: Relationships Among the Same Variables Over Time
All of the stability paths were significant, indicating that baseline levels of the sleep and substance use variables were predictive of the same variables at follow-up (see Table 2). The stability paths for cigarette, alcohol, and marijuana use were extremely high, ranging from .67 to .89. The stability paths for the sleep variables were less pronounced, ranging from .27 for weekend oversleep to .45 for total sleep.
Cross-Lagged Paths: Bi-Directional Longitudinal Relationships Between Sleep and Substance Use
Higher levels of weekday and total sleep at baseline predicted a lower likelihood of cigarette and marijuana use at follow-up (see Table 2). Higher levels of baseline weekend sleep predicted a lower likelihood of follow-up cigarette use. However, weekend sleep delay (a later bedtime on the weekends than during the week) at baseline predicted a higher likelihood of alcohol use at follow-up.
Cigarette use at baseline predicted less weekend and total sleep at follow-up. Alcohol use at baseline predicted less weekend sleep but also less weekend oversleep at follow-up. Marijuana use at baseline predicted more weekend sleep, greater weekend oversleep, and higher total sleep at follow-up.
Discussion
Despite the known deficits in sleep that occur during adolescence and the high prevalence of substance use behaviors among this group, little is known about how the multiple dimensions of sleep and substance use may be interrelated. The present study is one of the first to examine longitudinal bi-directional associations between sleep patterns, sleep duration, and substance use behaviors among youth, while simultaneously controlling for different forms of substance use and important covariates. By controlling for these covariates, such as pubertal development, body mass index, and depressive symptoms, which have been linked to both substance use and sleep, we have removed the possibility of a confounding effect in the relationship between sleep and substance by these variables. Additionally, the analyses conducted in this study allowed for the exploration of both cross-sectional (covariance) and longitudinal (2-year cross-lagged) associations, which allows for a better understanding of the possible causal mechanisms at play in this relationship.
Similar to previous cross-sectional studies (Pasch et al. 2010; O’Brien and Mindell 2005), lower levels of weekday sleep were associated with an increased likelihood of alcohol use at baseline and larger differences in sleep patterns (bed times and wake times) were associated with an increased likelihood of all substance use. It has been suggested that reduced levels of sleep may lead to lowered inhibition and/or poor emotional regulation, which may put youth at increased risk of substance use (Wong et al. 2010). Given that most youth do not get enough sleep on weekdays (National Sleep Foundation 2006), these even lower levels of weekday sleep may result in a reduced capacity to refuse substances from peers.
Cross-sectionally at 2-year follow-up, a greater weekend sleep delay (time to bed on the weekends as compared to weekdays) was associated with alcohol use and a greater weekend oversleep (wake time on the weekends as compared to weekdays) was associated with cigarette smoking and alcohol use. These findings suggest that youth who engage in substance use are more likely to stay out later and to sleep in longer on the weekends. As a lack of parental monitoring has been associated with an increased risk for substance use (Guo et al. 2001), these youth may lack parental monitoring, allowing them to stay out and go to sleep later on the weekends and, in turn, sleep later in the morning.
Longitudinally, several relationships emerged between sleep and substance use. First, increased levels of weekday and total sleep at baseline predicted a lower likelihood of past month cigarette and marijuana use at 2-year follow-up. Similarly, increased weekend sleep at baseline predicted a lower likelihood of past month smoking. These findings suggest that developing good sleep habits earlier in adolescence may help to keep youth from engaging in substance use and have important implications for parents and practitioners who work with youth. As substance use is a major public health problem, early intervention points, such as helping youth to develop good sleep hygiene practices, may be effective, particularly in reducing substance use among youth. Practitioners working with youth should consider probing more deeply about sleep when talking with youth, as more detailed information on sleep behavior may serve as a screening tool for substance use among youth. Further studies are needed to replicate these findings in larger, more diverse samples.
This study also found that youth with greater weekend sleep delays (time to bed) at baseline were more likely to use alcohol at the 2-year follow-up. Similar to the cross-sectional findings, youth who vary their weekday–weekend bedtimes may be those youth with less structure and a greater ability to stay out later on the weekends due to limited parental monitoring, and, thus, are at a greater risk for future engagement in alcohol use. Additionally, as youth age, they may be more likely to stay up later on the weekends either going out with friends or staying home, with parental permission, leading to greater variability in their weekday-weekend bedtimes. Youth with greater pattern differences also may be more likely to have trouble getting to sleep on weekdays when schedules are more restricted, leading to sleep deprivation and compromises in the adolescent’s ability to refuse substances, as well as reductions in the ability to self-regulate both behavior and emotions. While previous longitudinal work has found that sleep problems increase the likelihood of substance use (Wong et al. 2004; Wong et al. 2010; Wong et al. 2009), the present study extends this area of research into the areas of sleep duration and sleep patterns. This study found support for the hypothesis that sleep in early adolescence impacts subsequent substance use, but future work is needed to continue to explore these relationships and include variables such as parental monitoring, peer influence, and self- regulation.
This study expanded previous research by exploring how substance use predicted future sleep duration and patterns. While no relationships were found for substance use predicting weekday sleep, substance use at baseline did predict weekend sleep. Youth who used cigarettes or alcohol at baseline had reduced levels of weekend sleep at 2-year follow-up. Cigarette use at baseline also predicted reduced total sleep at follow-up, similar to previous cross-sectional research (Fischer et al. 2008; Townsend et al. 1991). Youth who engage in these behaviors at baseline may be more likely to continue these behaviors and, as such, later weekend sleep may be reduced because they are staying up to engage in substance use behaviors, likely with friends. Another possible mechanism for this association may be through the impacts of substance use on sleep (Hasler et al. 2012). As such, youth may develop problems sleeping for the appropriate amount of time needed during this developmental stage. Future research is needed that would include increased follow-up data points to understand more fully the trajectories of sleep and substance use across the adolescent period. Another possible reason for the effects of substance use on sleep is that youth who engage in substance use may be more likely to have greater levels of worry or stress, which may then lead to reduced sleep or sleep problems over time. Among adults, those who had disturbed sleep related to worry were two times more likely to become problem drinkers (Crum et al. 2004). It also may be possible that those adolescents who worry or have greater levels of stress turn to substance as a coping mechanism. This increased substance use may, then, have detrimental effects on sleep. Future studies should explore how worry and stress may be associated with the sleep and substance use relationship among youth.
While cigarette and alcohol use predicted reduced levels of sleep, marijuana use at baseline predicted increased weekend sleep. Additionally, those youth who engaged in marijuana use at baseline were also more likely to have increased total sleep at follow-up. While this may seem contrary to current study findings for cigarette and alcohol use, this may suggest that those youth who engage in marijuana use may, over time, sleep longer on the weekends. Youth who use marijuana may develop habits of sleeping more when sleep schedules are more able to vary (i.e., weekends) and, as such, increase sleep on the weekends.
While weekend sleep delay (time to bed) at baseline did not predict increased engagement in substance use, both alcohol and marijuana use predicted weekend oversleep (wake time); however, in opposite directions. Alcohol users had a smaller weekend oversleep at follow-up, while marijuana users had a larger oversleep. Alcohol has been found to have a negative effect on sleep, especially in acute high doses (Roehrs and Roth 2001). While we did not directly measure binge drinking in this study, the high doses of alcohol consumed when engaging in binge drinking may be particularly influential on youth’s sleep duration and patterns. Given that binge drinking is common among youth (Eaton et al. 2010), future research should incorporate a measure of binge drinking to understand more fully the alcohol-sleep relationship. Additionally, given that alcohol use at baseline also was associated with a reduced weekend sleep duration at follow-up, it may suggest that early alcohol use may have a particular effect on the “make-up” sleep that youth typically engage in on the weekends. Given the problems associated with changes in sleep patterns (Dahl and Lewin 2002), these effects of alcohol use may be particularly problematic. This study adds to the current literature regarding the negative effects of substance use by demonstrating how use in adolescence impacts future sleep duration and patterns.
Several mechanisms for the bi-directional associations between sleep and substance use have been proposed in this study; however, no one clear mechanism has emerged as the primary explanation. Overall, it appears that increased sleep duration on the weekdays is protective of later substance use, including cigarette, alcohol and marijuana use. Cigarette and alcohol use at baseline were detrimental for weekend sleep, but marijuana use predicted increases in weekend sleep. Both alcohol and marijuana use had effects on sleep patterns 2 years later. Although there are no definite mechanisms elucidated, this study supports the hypothesis that substance use and sleep patterns are related. One possibility for these inconclusive findings on mechanisms may be that in this study substance use was only measured by past month engagement in use in only three dimensions, cigarette, alcohol, and marijuana use. Further research is needed that uses more nuanced measures of substance use, including binge drinking and drunkenness, as well as measures that provide more variability in the levels of use, such as using continuous measures of substance use.
While this is one of the first studies to explore the longitudinal relationships between sleep duration, sleep patterns and substance use, it does have some limitations. It was conducted with primarily White, middle class, youth, which limits the generalizability of the findings. Another limitation is the self-report of sleep; however, similar sleep questions have been used successfully with youth in previous studies (Laberge et al. 2001; Lee et al. 1999; Wolfson 1996) and have been shown to be correlated significantly with measures of sleep using both diary and sleep actigraphy measures (Wolfson et al. 2003). While the sleep measures have been used previously, a limitation of these questions is that there was no time frame indicated in the stem of the question. However, the question did ask the youth to report the usual time s/he went to sleep and woke up so this would likely reflect overall sleep habits but does result in a different time frame assessed than the substance use questions. Additionally, due to the low prevalence of substance use in this population, we were unable to test for potential moderating effects. And while the current study is longitudinal, the results are based on only two time points, which is not sufficient to assess causality definitively. Further research is needed with more representative samples, additional time points, and the inclusion of additional explanatory variables, such as self-regulation or parenting, to continue to explore how sleep and substance use behaviors may co-vary and the possible mechanisms for their co-occurrence.
There are also several strengths of this study. In order to understand better the interrelationships of sleep and substance use, this study explored the bi-directional longitudinal relationships between these two domains while simultaneously controlling for baseline and 2-year follow-up associations between variables, as well as important covariates related to both sleep and substance use. By controlling for these variables, we were able to examine the relationship between sleep and substance use by removing some of the measurement error that exists when independent models of substance use behaviors are used. Additionally, having both the cross-lagged effects across waves and the covariance relationships within time periods is a strength of the modeling strategy used as it allowed for the determinations of how sleep and substance use were longitudinally related, beyond the cross-sectional associations. This study confirms the cross-sectional research that has been conducted previous to this study, but also demonstrates longitudinal relationships between substance use and sleep, which builds a case for a causal relationship. As sleep is such a crucial component to every-day functioning, continued work is needed to explore how its many facets are intertwined with youth substance use.
The findings of this study provide support for a bi-directional association between sleep and substance use among adolescent. Specifically, sleep patterns and duration are important precursors to adolescent substance use. Furthermore, adolescent substance use can impact future sleep patterns and duration, which could have a lasting impact on psychological and physical well-being. These relationships have significance for the optimal growth and development of adolescents. As it is likely that these relationships are mediated or moderated by other factors, such as peer and familial norms, further investigation into specific mechanisms is warranted. Outcomes from this and future studies may help to inform interventions to target substance use and sleep in youth in order to improve health outcomes related to these areas.
Acknowledgments
This research was funded through a grant from the National Cancer Institute as part of their Transdisciplinary Research in Energetics and Cancer (TREC) Initiative. Grant #1U54CA116849 and through a grant supported by the Etiology of Childhood Obesity (ECHO) with funding from the National Heart, Lung and Blood Institute, Grant #R01HL085978. The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute, National Heart, Lung and Blood Institute, or the National Institutes of Health.
Biographies
Keryn. E. Pasch is an Assistant Professor in the Department of Kinesiology and Health Education in the College of Education at the University of Texas, Austin. She received her M.P.H. in Health Behavior and Health Education from the University of North Carolina at Chapel Hill’s Gillings School of Global Public Health and her Ph.D. in Behavioral Epidemiology from the University of Minnesota School of Public Health. Her research interests include the co-occurrence of risk behaviors in adolescence and early adulthood and the influence of media on adolescent health behavior.
Lara A. Latimer is a Doctoral Candidate in Health Education in the Department of Kinesiology and Health Education in the College of Education at the University of Texas at Austin. She received her MA in Health Education from The University of Texas at Austin and has a BS in Exercise and Sport Science from Texas Tech University in Lubbock, Texas. Her research interests include nutrition- and activity-related aspects of child and adolescent health, obesity, in-school food and beverage promotion, and college health behaviors.
Jessica Duncan Cance is an Assistant Professor in the Department of Kinesiology and Health Education in the College of Education at the University of Texas at Austin. She received her M.P.H. in Behavioral Sciences and Health Education from the Rollins School of Public Health at Emory University and her Ph.D. in Health Behavior and Health Education from the University of North Carolina at Chapel Hill’s Gillings School of Global Public Health. Her research interests are in the prevention and etiology of adolescent health risk behaviors. She is specifically interested in how longitudinal interactions of biological, psychological, and social factors impact substance use.
Stacey G. Moe is a Project Coordinator in the Division of Epidemiology and Community Health in the School of Public Health at the University of Minnesota. She received her M.P.H. in Community Health Education from the University of Minnesota School of Public Health. Her research interests include school- and community-based programs to study primary prevention of childhood obesity and youth health promotion.
Leslie A. Lytle is a Professor in the Division of Epidemiology and Community Health in the School of Public Health at the University of Minnesota. She received her Ph.D. in Health Behavior and Health Education from the University of Michigan School of Public Health. She is also a Registered Dietician. Her research interests include youth health promotion and the prevention of childhood obesity using an ecological framework.
Contributor Information
Keryn E. Pasch, Email: kpasch@austin.utexas.edu, Department of Kinesiology and Health Education, University of Texas, 1 University Station, D3700, Austin, TX 78712, USA.
Lara A. Latimer, Department of Kinesiology and Health Education, University of Texas, 1 University Station, D3700, Austin, TX 78712, USA
Jessica Duncan Cance, Department of Kinesiology and Health Education, University of Texas, 1 University Station, D3700, Austin, TX 78712, USA.
Stacey G. Moe, Division of Epidemiology and Community Health, School of Public Health, University of Minnesota, Minneapolis, MN 55454, USA
Leslie A. Lytle, Division of Epidemiology and Community Health, School of Public Health, University of Minnesota, Minneapolis, MN 55454, USA
References
- Bollen KA, Curran PJ. Latent curve models : a structural equation perspective (Wiley series in probability and statistics) Hoboken, N.J.: Wiley-Interscience; 2006. [Google Scholar]
- Cappuccio FP, Taggart FM, Kandala NB, Currie A, Peile E, Stranges S, et al. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31(5):619–626. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carskadon MA, Harvey K, Dement WC. Acute restriction of nocturnal sleep in children. Perception and Motor Skills. 1981;53:103–112. [Google Scholar]
- Carskadon MA, Vieira C, Acebo C. Association between puberty and delayed phase preference. Sleep. 1993;16(3):258–262. doi: 10.1093/sleep/16.3.258. [DOI] [PubMed] [Google Scholar]
- Carskadon MA, Wolfson AR, Acebo C, Tzischinsky O, Seifer R. Adolescent sleep patterns, circadian timing, and sleepiness at a transition to early school days. Sleep. 1998;21(8):871–881. doi: 10.1093/sleep/21.8.871. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Youth risk behavior surveillance—United States, 2011. Morbidity and Mortality Weekly Report. 2012;61(4):1–166. [PubMed] [Google Scholar]
- Crum RM, Storr CL, Chan YF, Ford DE. Sleep disturbance and risk for alcohol-related problems. The American Journal of Psychiatry. 2004;161(7):1197–1203. doi: 10.1176/appi.ajp.161.7.1197. [DOI] [PubMed] [Google Scholar]
- Dahl RE. The impact of inadequate sleep on children’s daytime cognitive function. Seminars in Pediatric Neurology. 1996;3(1):44–50. doi: 10.1016/s1071-9091(96)80028-3. [DOI] [PubMed] [Google Scholar]
- Dahl RE, Lewin DS. Pathways to adolescent health: Sleep regulation and behavior. Journal of Adolescent Health. 2002;31:175–184. doi: 10.1016/s1054-139x(02)00506-2. [DOI] [PubMed] [Google Scholar]
- Eaton DK, Kann L, Kinchen S, Shanklin S, Ross J, Hawkins J, et al. Youth risk behavior surveillance—United States, 2009. MMWR. Surveillance summaries: Morbidity and mortality weekly report. Surveillance summaries/CDC. 2010;59(5):1–142. [PubMed] [Google Scholar]
- Fischer FM, Nagai R, Teixeira LR. Explaining sleep duration in adolescents: the impact of socio-demographic and lifestyle factors and working status. Chronobiology International. 2008;25(2):359–372. doi: 10.1080/07420520802110639. [DOI] [PubMed] [Google Scholar]
- Fredriksen K, Rhodes J, Reddy R, Way N. Sleepless in Chicago: Tracking the effects of adolescent sleep loss during the middle school years. Child Development. 2004;75(1):84–95. doi: 10.1111/j.1467-8624.2004.00655.x. [DOI] [PubMed] [Google Scholar]
- Gluck M, Geliebter A, Satov T. Night eating syndrome is associated with depression, low self-esteem, reduced daytime hunger, and less weight loss in obese outpatients. Obesity Research. 2001;9:264–267. doi: 10.1038/oby.2001.31. [DOI] [PubMed] [Google Scholar]
- Goodman E, Huang B. Socioeconomic status, depressive symptoms, and adolescent substance use. Archives of Pediatrics and Adolescent Medicine. 2002;156(5):448–453. doi: 10.1001/archpedi.156.5.448. [DOI] [PubMed] [Google Scholar]
- Guo J, Hawkins JD, Hill KG, Abbott RD. Childhood and adolescent predictors of alcohol abuse and dependence in young adulthood. Journal of Studies on Alcohol. 2001;62(6):754–762. doi: 10.15288/jsa.2001.62.754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hallfors DD, Waller MW, Bauer D, Ford CA, Halpern CT. Which comes first in adolescence—Sex and drugs or depression? American Journal of Preventive Medicine. 2005;29(3):163–170. doi: 10.1016/j.amepre.2005.06.002. [DOI] [PubMed] [Google Scholar]
- Hasler BP, Smith LJ, Cousins JC, Bootzin RR. Circadian rhythms, sleep, and substance abuse. Sleep Medicine Reviews. 2012;16(1):67–81. doi: 10.1016/j.smrv.2011.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu LT, Bentler PM. Cutoff criteria for fit indices in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Johnson EO, Breslau N. Sleep problems and substance use in adolescence. Drug and Alcohol Dependence. 2001;64(1):1–7. doi: 10.1016/s0376-8716(00)00222-2. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O’Malley PM, Bachman JG. National survey results on drug use from the monitoring the future study, 1975–1997. 1998 [Google Scholar]
- Kandel D, Davies M. Epidemiology of depressive mood in adolescents. Archives of General Psychiatry. 1982;39:1205–1212. doi: 10.1001/archpsyc.1982.04290100065011. [DOI] [PubMed] [Google Scholar]
- Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 CDC growth charts for the United States: Methods and development. Vital and Health Statistics. 2002;11(246):1–203. [PubMed] [Google Scholar]
- Laberge L, Petit D, Simard C, Vitaro F, Tremblay RE. Development of sleep patterns in early adolescence. Journal of Sleep Research. 2001;10:59–67. doi: 10.1046/j.1365-2869.2001.00242.x. [DOI] [PubMed] [Google Scholar]
- Lee KA, McEnany G, Weekes D. Gender differences in sleep patterns for early adolescents. Journal of Adolescent Health. 1999;24:16–20. doi: 10.1016/s1054-139x(98)00074-3. [DOI] [PubMed] [Google Scholar]
- Lytle LA. Examining the etiology of childhood obesity: The IDEA study. American Journal of Community Psychology. 2009;44(3–4):338–349. doi: 10.1007/s10464-009-9269-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lytle LA, Pasch KE, Farbakhsh K. The relationship between sleep and weight in a sample of adolescents. Obesity. 2011;19(2):324–331. doi: 10.1038/oby.2010.242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus User’s Guide. 6th Ed. Los Angeles, CA: Muthén & Muthén; 1998–2010. [Google Scholar]
- National Sleep Foundation. Washington, D.C.: National Sleep Foundation; 2006. Sleep in America Poll. [Google Scholar]
- O’Brien EM, Mindell JA. Sleep and risk-taking behavior in adolescents. Behavioral Sleep Medicine. 2005;3(3):113–133. doi: 10.1207/s15402010bsm0303_1. [DOI] [PubMed] [Google Scholar]
- Pasch KE, Laska MN, Lytle LA, Moe SG. Adolescent sleep, risk behaviors, and depressive symptoms: Are they linked? American Journal of Health Behavior. 2010;34(2):237–248. doi: 10.5993/ajhb.34.2.11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasch KE, Nelson MC, Lytle LA, Moe SG, Perry CL. Adoption of risk-related factors through early adolescence: Associations with weight status and implications for causal mechanisms. The Journal of Adolescent Health. 2008;43(4):387–393. doi: 10.1016/j.jadohealth.2008.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pasch KE, Velazquez CE, Cance JD, Moe SG, Lytle LA. Youth substance use and body composition: Does risk in one area predict risk in the other? Journal of Youth and Adolescence. 2012;41(1):14–26. doi: 10.1007/s10964-011-9706-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel SR, Hu FB. Short sleep duration and weight gain: A systematic review. Obesity (Silver Spring) 2008;16(3):643–653. doi: 10.1038/oby.2007.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel SR, Malhotra A, White DP, Gottlieb DJ, Hu FB. Association between reduced sleep and weight gain in women. American Journal of Epidemiology. 2006;164(10):947–954. doi: 10.1093/aje/kwj280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patton GC, Viner R. Pubertal transitions in health. Lancet. 2007;369(9567):1130–1139. doi: 10.1016/S0140-6736(07)60366-3. [DOI] [PubMed] [Google Scholar]
- Petersen AC, Crockett LJ, Richards M, Boxer A. A self-report measure of pubertal status: Reliability, validity and initial norms. Journal of Youth and Adolescence. 1988;17(2):117. doi: 10.1007/BF01537962. [DOI] [PubMed] [Google Scholar]
- Phillips BA, Danner FJ. Cigarette smoking and sleep disturbance. Archives of Internal Medicine. 1995;155(7):734–737. [PubMed] [Google Scholar]
- Roberts RE, Roberts CR, Chen IG. Impact of insomnia on future functioning of adolescents. Journal of Psychosomatic Research. 2002;53(1):561–569. doi: 10.1016/s0022-3999(02)00446-4. [DOI] [PubMed] [Google Scholar]
- Roberts RE, Roberts CR, Duong HT. Sleepless in adolescence: Prospective data on sleep deprivation, health and functioning. Journal of Adolescence. 2009;32(5):1045–1057. doi: 10.1016/j.adolescence.2009.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roehrs T, Roth T. Sleep, sleepiness, and alcohol use. Alcohol Research & Health. 2001;25(2):101–109. [PMC free article] [PubMed] [Google Scholar]
- Sadeh A, Dahl RE, Shahar G, Rosenblat-Stein S. Sleep and the transition to adolescence: A longitudinal study. Sleep. 2009;32(12):1602–1609. doi: 10.1093/sleep/32.12.1602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadeh A, Gruber R, Raviv A. Sleep, neurobehavioral functioning, and behavior problems in school-age children. Child Development. 2002;73(2):405–417. doi: 10.1111/1467-8624.00414. [DOI] [PubMed] [Google Scholar]
- Shih RA, Miles JN, Tucker JS, Zhou AJ, D’Amico EJ. Racial/ethnic differences in adolescent substance use: mediation by individual, family, and school factors. Journal of Studies on Alcohol and Drugs. 2010;71(5):640–651. doi: 10.15288/jsad.2010.71.640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strauch I, Meier B. Sleep need in adolescents: A longitudinal approach. Sleep. 1988;11(4):378–386. doi: 10.1093/sleep/11.4.378. [DOI] [PubMed] [Google Scholar]
- Szymczak JT, Jasinska M, Pawlak E, Zwierzykowska M. Annual and weekly changes in the sleep-wake rhythm of school children. Sleep. 1993;16(5):433–435. doi: 10.1093/sleep/16.5.433. [DOI] [PubMed] [Google Scholar]
- Townsend J, Wilkes H, Haines A, Jarvis M. Adolescent smokers seen in general practice: health, lifestyle, physical measurements, and response to antismoking advice. British Medical Journal. 1991;303(6808):947–950. doi: 10.1136/bmj.303.6808.947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tynjala J, Kannas L, Levalahti E. Perceived tiredness among adolescents and its association with sleep habits and use of psychoactive substances. Journal of Sleep Research. 1997;6(3):189–198. doi: 10.1046/j.1365-2869.1997.00048.x. [DOI] [PubMed] [Google Scholar]
- Vignau J, Bailly D, Duhamel A, Vervaecke P, Beuscart R, Collinet C. Epidemiologic study of sleep quality and troubles in French secondary school adolescents. Journal of Adolescent Health. 1997;21(5):343–350. doi: 10.1016/S1054-139X(97)00109-2. [DOI] [PubMed] [Google Scholar]
- Wetter DW, Young TB. The relation between cigarette-smoking and sleep disturbance. Preventive Medicine. 1994;23(3):328–334. doi: 10.1006/pmed.1994.1046. [DOI] [PubMed] [Google Scholar]
- Widome R, Forster JL, Hannan PJ, Perry CL. Longitudinal patterns of youth access to cigarettes and smoking progression: Minnesota Adolescent Community Cohort (MACC) study (2000–2003) Preventive Medicine. 2007;45(6):442–446. doi: 10.1016/j.ypmed.2007.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wills TA, Cleary S, Filer M, Shinar O, Mariani J, Spera K. Temperament related to early-onset substance use: test of a developmental model. Prevention Science. 2001;2(3):145–163. doi: 10.1023/a:1011558807062. [DOI] [PubMed] [Google Scholar]
- Wolfson AR. Sleeping patterns of children and adolescents: Developmental trends, disruptions, and adaptations. Child and Adolescent Psychiatric Clinics of North America. 1996;5(3):549–568. [Google Scholar]
- Wolfson AR, Carskadon MA. Sleep schedules and daytime functioning in adolescents. Child Development. 1998;69(4):875–887. [PubMed] [Google Scholar]
- Wolfson AR, Carskadon MA, Acebo C, Seifer R, Fallone G, Labyak SE, et al. Evidence for the validity of a sleep habits survey for adolescents. Sleep. 2003;26(2):213–216. doi: 10.1093/sleep/26.2.213. [DOI] [PubMed] [Google Scholar]
- Wong MM, Brower KJ, Fitzgerald HE, Zucker RA. Sleep problems in early childhood and early onset of alcohol and other drug use in adolescence. Alcoholism, Clinical and Experimental Research. 2004;28(4):578–587. doi: 10.1097/01.alc.0000121651.75952.39. [DOI] [PubMed] [Google Scholar]
- Wong MM, Brower KJ, Nigg JT, Zucker RA. Childhood sleep problems, response inhibition, and alcohol and drug outcomes in adolescence and young adulthood. Alcoholism, Clinical and Experimental Research. 2010;34(6):1033–1044. doi: 10.1111/j.1530-0277.2010.01178.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong MM, Brower KJ, Zucker RA. Childhood sleep problems, early onset of substance use and behavioral problems in adolescence. Sleep Medicine. 2009;10(7):787–796. doi: 10.1016/j.sleep.2008.06.015. [DOI] [PMC free article] [PubMed] [Google Scholar]