Abstract
To identify potential risk factors for hearing loss from the infant with high risk criteria as guided by the Joint Committee on Infant Hearing (JCIH, 2000). 490 infants with age range of 2 days to 6 months who had undergone detailed audiological evaluation during for the period of 3 years at Gauhati Medical College Hospital were taken for the study. The hearing screening was performed on each infant using Distortion Product Otoacoustic Emission (DPOAE) testing. The infants who failed DPOAEs screening were followed up and Auditory Brainstem Response testing. Out of 490 high risk infants who had undergone detailed audiological evaluation 145 infants were found to be having hearing loss. Out of 145 infants 73 infants were male and 72 infants were female. The risk factor for hearing loss with the highest incidence was hyperbilirubenemia, Apgar scores of 0–4 at 1 min or 0–6 at 5 min was the second most prevalent risk factor, followed by TORCH infections. This study suggests the need for review of high risk register that is used along with the physiological and electrophysiological hearing test to screen the infants. The high risk register remains helpful in determining follow up plans so that children who may develop late onset of hearing loss will not be missed. Being aware of which risk factors are more likely to cause hearing loss in infants would be helpful to plan for follow up these children.
Keywords: Infant hearing, High risk register, Potential risk factors, Hearing screening
Introduction
There are evidences that the human fetus responds to sounds as early as 22 weeks of gestation, Beata and Loana [1]. Although the development of the cochlea and inner ear active mechanisms are complete at birth, the central auditory pathway needs further maturation, a process which is related to and dependent upon auditory stimulation. Hearing loss is one of the most common congenital anomalies, occurring in approximately 1–3 infants per 1,000, Downs [2]. Hearing loss has no physical characteristics and the child with hearing loss looks normal and often achieve normal early milestones, including babbling.
There are serious negative consequences associated with undetected hearing loss, such as speech, language and cognitive delays, poor social adjustment, poor educational achievement, as well as subsequent economic disadvantage, Yoshinaga-Itano and Gravel [10]. Many studies revealed that children with hearing loss identified before 6 months of age, and provided early intervention services, achieved language scores at or near their cognitive scores. The Joint Committee on Infant Hearing, JCIH [3] recommends screening of hearing of all infants not later than 1 month of age. For those who fail screening, a comprehensive audiologic evaluation should take place within 3 months of age, and those with confirmed hearing loss should receive appropriate intervention not later than 6 months of age.
Meyer et al. [5] investigated actual incidence of and risk factors for hearing loss which revealed that the incidence of permanent congenital hearing loss in the Neonatal Intensive Care Unit (NICU) population is ten to twenty times higher than in the general population. The risk factors connected to pregnancy includes intrauterine infections, especially TORCH (toxoplasma, rubella, cytomegalovirus, and herpes), ototoxic medication (amino glycosides, loop diuretics, quinine derivatives, etc.), alcohol and/or drug intake. Perinatal and postnatal causes of hearing loss includes, prematurity (gestational age under 34 weeks, birth weight under 1500 g), severe perinatal hypoxia, infections (in specially Pneumococcus, Haemophilus influenzae meningitis, encephalitis), hyperbilirubinemia (blood bilirubin level >20 mg/dl), ototoxic drugs (amino glycosides and frusamide administration more than 5 days without serum level monitoring), neonatal pulmonary hypertension—mechanical ventilation for 5 days or longer, extracorporeal membrane oxygenation (ECMO), trauma during delivery, severe intracranial hemorrhage, neonatal convulsion, Beata and Loana [1].
Many studies designed to determine risk factors associated with hearing loss Meyer et al. [5], Yoshinaga-Itano [9], Yoshikawa et al. [8] have brief controversy among the results. Such results highlight the need to continue to investigate additional risk factors for hearing loss. It may be even argued that risk factors for hearing loss in developed countries are actually being decreased due to advanced medical care and proper counseling program. Infants in developed countries are not exposed to additional environmental factors present in many developing countries, which may increase the risk of hearing loss in infants.
Objective of the Study
The purpose of this study is to identify potential risk factors for infant hearing loss from the infant high risk criteria as guided by the Joint Committee on Infant Hearing JCIH, [4].
Method
Subjects
490 infants with age range of 2 days to 6 months who had undergone detailed audiological evaluation during 25th May 2006 to 2009 for the period of 3 years at Gauhati Medical College Hospital (GMCH) were taken for the study.
Equipments
Neurosoft-neuro-audio digital neurophysiologic system for EP and OAE were used for testing the infants hearing.
Test Protocol
Otoacoustic emission testing DPOAE was used to screen the neonates which were analyzed in the frequency range of 1 to 8 kHz. Meyer et al. [5] recommended that signal to noise ratio (SNR) for an infant to be passed is 3 dB and above. SNR of less than 3 dB is considered as failed in screening. The infants who failed in OAEs screening was followed up and auditory brainstem response (ABR) testing was done. The parameters used for recording ABR test were the intensity range of testing was from 130 dB SPL (85 dB HL) to 70 dB SPL (25 dB HL) at a repetition rate of 27.7. The number of samples used for averaging while recording was 2,000. The polarity used was rarefaction. The absence of Vth peak at 70 dB SPL was used as the failing criteria.
Procedure
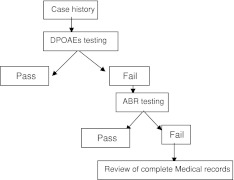
Testing was done in a sound treated room at speech and hearing unit of ENT department of GMCH. The data obtained from each child was maintained in two register (main register and follow-up register). The medical records of the children who had undergone detailed audiological evaluation during May 2007 to 2010 for the period of 3 years at GMCH were examined. The medical reports included evaluations at various departments of the hospital including pediatric unit, ENT (speech and language and hearing evaluation), neurological unit of the neonates along with the discharge report were examined. The data was analyzed accordingly to identify the most prevalent cause for the hearing loss among these infants (Chart 1).
Chart 1.
Procedure followed during hearing screening of the infants
Results
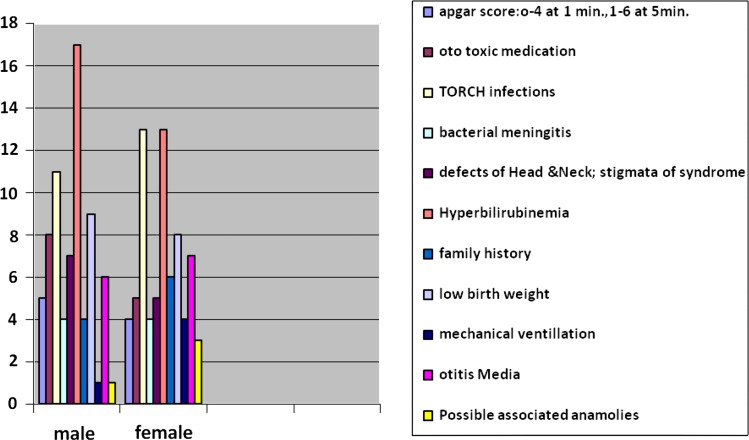
In the present study out of 490 high risk infants who had undergone detailed audiological evaluation 145 infants were found to be having hearing loss. Out of 145 infants 73 infants were male and 72 infants were female Graph 1.
Graph 1.
Comparison of respective risk factors responsible for hearing loss among male and female infants
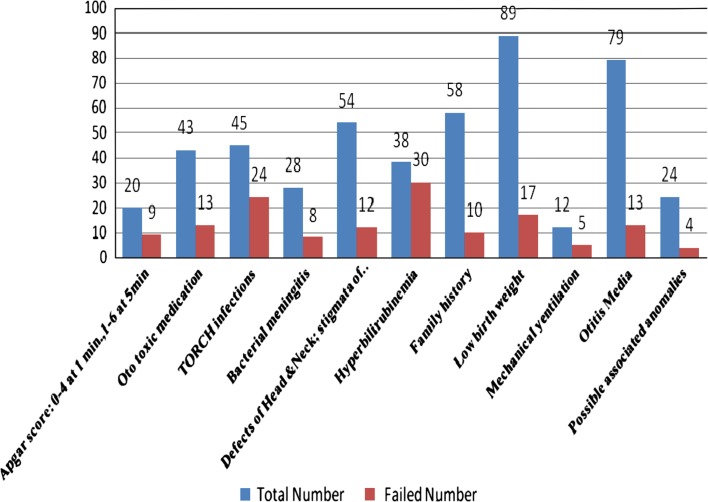
The Graph 2 shows the risk factor for hearing loss with the highest incidence was hyperbilirubinemia, Apgar scores of 0–4 at 1 min or 0–6 at 5 min was the second most prevalent risk factor, followed by TORCH infections, ototoxic medication, bacterial meningitis, mechanical ventilation lasting for more than 5 days, low birth weight, defects of head and neck; stigmata of syndrome, family history, otitis media and possible associated anomalies. Table 1.
Graph 2.
Comparison of frequency of occurrence of hearing loss in each risk factor group
Table 1.
Number of infants tested in each risk factor group and number of infants failed in the hearing screening
| Risk factors | Total number | Number failed |
|---|---|---|
| Apgar score: 0–4 at 1 min, 1–6 at 5 min | 20 | 9 |
| Oto toxic medication | 43 | 13 |
| TORCH infections | 45 | 24 |
| Bacterial meningitis | 28 | 8 |
| Defects of head and neck; stigmata of syndrome | 54 | 12 |
| Hyperbilirubinemia | 38 | 30 |
| Family history | 58 | 10 |
| Low birth weight | 89 | 17 |
| Mechanical ventilation | 12 | 5 |
| Otitis media | 79 | 13 |
| Possible associated anomalies | 24 | 4 |
Discussion
Out of the ten indicators repeatedly stated by the Joint Committee on Infant Hearing, JCIH [4] as associated with the category of sensorineural or conductive hearing loss at birth through age 28 days, four specifically related to the children at NICU.
These include,
Hyperbilirubenemia at a serum level, requiring exchange transfusion; birth weight less than 1500 g.
Apgar scores of 0–4 at 1 min or 0–6 at 5 min.
TORCH infections.
Ototoxic medications including, but not limited to, the amino glycosides, used in multiple courses or in combination with loop diuretics.
In addition, two more indicators are related to risks frequently found
Bacterial meningitis. Also, children with intrauterine infections, such as CMV, rubella, herpes, syphilis, and toxoplasmosis; craniofacial anomalies, including those with morphologic abnormalities of the pinna and ear canal; or syndromes known to be associated with sensorineural or conductive hearing loss, such as children with Down syndrome, are frequently admitted to NICUs for associated health problem.
Mechanical ventilation lasting for more than 5 days.
The lower the birth weight, the more likely a child will have neurosequelae, hearing loss or visual impairment, asthma, and cognitive impairment.
The present study, however found the occurrence of hearing loss among the infants with the history of neonatal hyperbilirubenemia was most. Shimuzu et al. [6] found low birth weight to be the most common among their sample. Swigonski et al. [7] found ototoxic medications as the most frequent occurring risk factor. This difference may be due to testing habits of the hospitals. It may be also due to other factors such as socioeconomic status, education, or prenatal care of mothers involved.
Conclusion
This study suggests the need for review of high risk register that is used along with the physiological and electrophysiological hearing test to screen the infants. The high risk register remains helpful in determining follow up plans so that children who may develop late onset of hearing loss will not be missed. Being aware of which risk factors are more likely to cause hearing loss in infants would be helpful for doctors to plan for follow up these children.
References
- 1.Beata AS, Ioana AN. Etiopathogeny of congenital and early-onset hearing loss; detection and early intervention methods in infants and children. J Clin Med. 2008;3(1):45–51. [Google Scholar]
- 2.Downs M. The case for detection and intervention at birth. Semin Hearing. 2004;15:76–83. doi: 10.1055/s-0028-1083757. [DOI] [Google Scholar]
- 3.Joint committee on infant hearing. Position statement (1994) American Speech, Language and Hearing Association 36(12):38–41 [PubMed]
- 4.Joint committee on infant hearing (2000) Position statement: Principles and guidelines for early hearing detection and intervention programs. Cited from http://www.cdc.gov/ncbddd/ehdi/documents/jcihyr2000.pdf [PubMed]
- 5.Meyer C, Wittle J, Hiildmann A, Hennecke H, Schunck U, Maul K, et al. Neonatal screening for hearing disorder in infants at risk: incidence, risk factors, and follow-up. Pediatrics. 1999;104(4):900–904. doi: 10.1542/peds.104.4.900. [DOI] [PubMed] [Google Scholar]
- 6.Shimizu H, Walters RJ, Proctor LR, Kennedy DW, Allen MC, Markowitz RK. Identification of hearing impairment in the neonatal intensive care unit population: outcome of a five-year project at the Johns Hopkins hospital. Semin Hearing. 1990;11(2):150–160. doi: 10.1055/s-0028-1091343. [DOI] [Google Scholar]
- 7.Swigonski N, Shallop J, Bull MJ, Lemons A. Hearing screening of high risk newborns. Ear Hear. 1987;8(1):26–30. doi: 10.1097/00003446-198702000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Yoshikawa S, Ikeda K, Kudo T, Kobayashi T. The effects of hypoxia, premature birth, infection, ototoxic drugs, circulatory systems and congenital disease on neonatal hearing loss. Auris Nasus Larynx. 2004;31:361–368. doi: 10.1016/j.anl.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 9.Yoshinaga-Itano C. Levels of evidence: universal newborn hearing screening (UNHS) and early detection and intervention systems (EHDI) J Commun Disord. 2004;37:451–465. doi: 10.1016/j.jcomdis.2004.04.008. [DOI] [PubMed] [Google Scholar]
- 10.Yoshinaga-Itano C, Gravel JS. The evidence for universal newborn hearing screening. Am J Audiol. 2001;10:62–64. doi: 10.1044/1059-0889(2001/013). [DOI] [PubMed] [Google Scholar]