Summary
Burned patients are prone to develop severe intestinal complications because of decreased splanchnic circulation. We report three cases of sigmoid perforation in burn patients appearing late during hospitalization. The common aetiological factor was a state of septic shock treated with infusion of vasopressors. Two patients also received corticosteroids as treatment for acute respiratory distress syndrome. These cases underline the necessity to maintain adequate organ perfusion and to prevent intestinal ischaemia in severe burns.
Keywords: burns, sigmoid diverticulitis perforation, septic shock, vasopressor, corticosteroid, opioid drugs
Abstract
Les patients brûlés sont sujets à développer de graves complications intestinales en raison de la circulation splanchnique diminuée. Les Auteurs décrivent trois cas de perforation du sigmoïde chez les patients brûlés qui se sont manifestés tardivement après l'hospitalisation. Le facteur commun étiologique était un état de choc septique traité avec perfusion des vasopresseurs. Deux patients ont aussi reçu des corticostéroïdes pour le traitement du syndrome de détresse respiratoire aiguë. Ces cas soulignent la nécessité de maintenir la perfusion adéquate des organes et d'éviter l'ischémie intestinale dans les grands brûlés.
Introduction
A severe cutaneous thermal injury induces multiple organ hypoperfusion. Mesenteric circulation may be dramatically reduced during initial fluid resuscitation. The gut barrier may also suffer from low blood flow during frequent situations of septic shock and administration of catecholamines.
The following three cases illustrate severe intestinal complications in burn patients due to splanchnic hypoperfusion and gastrointestinal barrier fragility.
Case report 1
A 47-yr-old male with a history of chronic alcoholism and smoking was admitted to the burn centre four hours after a suicide attempt by self-immolation. He sustained 40% TBSA burns mainly in the lower limbs of which 30% were third degree. The patient also had active bleeding from deep intentional venesections of the two forearms which, in addition to the expected fluid loss due to the burn injury, resulted in hypovolaemic shock. Fluid resuscitation with crystalloids, colloids, and four units of blood and norepinephrine continuous infusion were all necessary to maintain adequate perfusion (mean arterial pressure > 60 mm Hg). Control of upper limb haemorrhage and escharotomies of both lower extremities were immediately performed. The patient was intubated, sedated continuously, and ventilated mechanically. Enteral nutrition was started on day 2. The patient developed acute renal and liver failure associated with a temporary increase of serum transaminases (more than 100 times mean values).
Six days later, methicillin-sensitive Staphylococcus aureus hypoxic pneumonia required antibiotic treatment with oxacillin (Bristopen®, Bristol-Myers Squibb, Rueil-Malmaison France) and gentamicin (Gentalline®, MSD France, Courbevoie France).
Eight days following the burn injury, the patient had the first session of excision and skin auto-grafting.
On day 13, the patient developed bowel obstruction even if a few days before this complication manifested itself, enteral nutrition was well tolerated. A perforation was diagnosed by abdominal CT scan necessitating emergency exploratory laparotomy. A perforation of a sigmoid diverticulum was detected and was managed by sigmoid colectomy and Hartman's colostomy (exteriorization of the proximal stump and placing the closed distal stump within the peritoneal cavity). Temporary closure of the midline incision using vacuum Assisted Closure (VAC®, KCI, San Antonio, TX, USA) was performed to avoid increased abdominal wall tension.
Second-look laparatomy was performed 48 h later; the necrotic left omentum was resected, and the abdominal wall was closed using staples 22 days after the burn injury. Definitive abdominal wound closure was obtained following 9 days of VAC therapy. Mechanical ventilation was discontinued on day 47 post-burn and the patient was discharged from the burn centre on day 89.
Case report 2
A 56-yr-old male was admitted to the burn unit following an accidental house fire. He sustained a 31% TBSA burn injury including 21% TBSA third-degree burns. He was intubated before hospital admission. Bronchoscopy confirmed severe inhalation injury with mucosal haemorrhages. Midazolam (Hypnovel®, Roche, Boulogne-Billancourt, France) and fentanyl (Fentanyl®, Mylan, Saint-Priest, France) were required for continuous intravenous sedation. One day after admission, enteral nutrition was started. The inhalation burn was complicated by acute respiratory distress syndrome (ARDS). To maintain PaO2 above 80 mm Hg, the patient required early deep sedation, tracheotomy, aggressive ventilation including high PEEP, FiO2 100%, and high frequency percussive ventilation (HFPV). A postoperative acute renal failure on day 6 required daily dialysis for 10 days. Pneumonia was diagnosed, also on day 6, and the patient remained hypoxic despite ventilation and adequate antibiotics. He was also treated for ARDS with corticosteroids from day 10 for 21 days (methylprednisolone 2 mg/kg/day).
Four surgical operations including temporary allografts and definitive autografts were performed. Forty-two days post-burn, a clinical intestinal obstruction was noted. This was followed by septic shock requiring norepinephrine infusion. Enterococcus faecalis and Escherichia coli were identified in blood cultures.
The cause of sepsis was a late diagnosed peritonitis. An abdominal CT scan was performed and the patient was operated on on day 47 post-burn. A sigmoid diverticulum perforation with multiple intra abdominal abscesses and purulent peritonitis were treated with Hartmann's colostomy of the left descending colon. Two days later a secondlook procedure was planned for peritoneal lavage. Despite intensive treatment, the patient developed multi-organ failure and died on day 56.
Case report 3
A 43-yr-old male was admitted following 30% TBSA (26% TBSA third degree) thermal burn due to a work accident. Burns were located mainly on the chest, neck, and upper limbs. He was immediately intubated, sedated, and mechanically ventilated because of inhalation injury. Enteral nutrition was started on day 1.
The initial evolution was worrying because of severe respiratory damage due to smoke inhalation. Daily bronchoscopy was performed to clear soot and casts. During the first week, he developed septic shock caused by Klebsiella pneumoniae (identified in two blood cultures and in bronchoalveolar lavage). Antibiotic treatment included ciprofloxacin (Ciflox®, Bayer Santé, Loos, France) piperacillin-tazobactam (Piperacilline/Tazobacatamt®, Panpharma, Luitré, France) for ten days. Sepsis required continuous infusion of norepinephrine for 72 h. Excision and grafts were performed four times without any noticeable difficulties.
Twenty-six days post-burn, a ventilator-associated pneumonia and bacteriaemia caused by Acinetobacter baumannii was treated with imipenem (Tienam®, MSD, Courbevoie, France). The respiratory status deteriorated progressively into ARDS. To avoid pulmonary fibrosis, corticosteroid treatment was planned for 21 days starting on day 33 post-burn (methylprednisolone 2 mg/kg/day).
Forty-eight days post-burn, the patient developed generalized faecal peritonitis. On surgical exploration the sigmoid was noted to have a two-cm perforation on one of its multiple diverticulae. A Hartmann's colostomy was performed. Post-operatively, the patient developed an acalculous cholecystitis treated initially with antibiotics, then with a radio-guided percutaneous drainage of the gall bladder. The patient's evolution was progressively favourable. He was ventilated for 93 days and discharged after 114 days.
Discussion
A review of the literature reports only a few cases of gastrointestinal perforation in burns and none specifically on perforation of a sigmoid diverticulum.
Colonic ulceration and necrosis in burn patients are rare and usually occur in the caecum: Still JM, jr, et al. reported a case of caecal perforation secondary to non-specific ulceration in a patient with 26% TBSA burns.1
Ghoneim IE et al. reported a similar case.2 We also found a case report of a colonic necrosis and perforation following oral sodium polystyrene sulphate treatment (Kayexalate®, Sanofi-Aventis, Paris, France).3
Desai MH et al.4 reported 16 burn patients (seven children and nine adults) requiring surgery for necrotic bowel. These colon and small bowel lesions were thought to be ischaemic in nature. A retrospective 8-yr single-centre study including 2114 patients with burn injuries highlighted 19 patients with either ischaemic necrotic bowel disease (n=10) or other gastrointestinal tract complications (n=9).5 The severity of thermal injury and presence of systemic infection were identified as risk factors for the development of ischaemic necrotic bowel disease. Fitzgerald et al. described a perforation of the transverse colon caused by ischaemia due to a prolonged low flow state.6
A recent study published by Markell et al., not cited here, reported a frequency of 2.8% abdominal catastrophe after severe burns defined as abdominal compartment syndrome (ACS) and/or ischemic bowel. Most often these complications occurred within three days of the injury, and 80% of the cases occurred within 14 days. The frequency of ACS increased linearly with the burn size. However, unlike our cases, no cases were described of sigmoid diverticulum perforation which occurred later during hospitalization (days 13, 47 and 48).
Regarding more specifically diverticular perforation, there are no data in the burn literature. One study measured abscess and peritonitis frequency secondary to diverticular perforation in Norfolk, UK.7 The incidence of perforation in this study was 4.0 cases per 100,000 population per year and an estimated 2000 cases per year were estimated to occur in the UK.
In perforated diverticular disease, several small case series have implicated non-steroidal anti-inflammatory drugs (NSAIDs) as a possible aetiological factor.8,9 One study found that 11 of 49 patients (22%) with perforation were taking steroids and that those on steroids had more severe inflammatory complications.10 Corticosteroids have powerful immunosuppressive effects as well as anti-inflammatory effects and it is likely that these drugs impair a person's ability to contain a perforation in its early stages. Other studies have shown similar findings in patients receiving corticosteroids.11 Five patients who underwent surgery for primary and metastatic brain and spinal tumours experienced a sigmoid diverticular perforation at a mean dose of 3947 mg of methylprednisolone over at least 7 days.12 Only one comparative study has looked specifically at diverticular perforation, comparing the use of medication in 115 cases of diverticular disease presenting with extracolonic sepsis (fistula, abscess, peritonitis) and 77 cases of diverticular disease without extracolonic sepsis (inflammatory mass, peridiverticulitis).13 In this study, both NSAIDs and corticosteroids were associated with the most severe clinical manifestations of perforation, namely peritonitis and abscess.
Another case series reported that a quarter of patients with perforation were taking opiate analgesics. Opiates have a plausible mechanism of action through their effects on raising intracolonic pressure and slowing intestinal transit, which might prolong the exposure of the diverticular wall to potentially damaging intracolonic pathogens or agents.
The risk of perforation increases with advanced age and appears to be greater in males.14 Although most people with diverticulosis remain asymptomatic, 10-25% develop complications including perforation lengthy sedation. All factors that could predispose diverticular perforations and bleeding.15
Regarding our patients, there are several explanations for the mechanism of diverticular perforation. All the patients presented a delayed state of septic shock, requiring support by vasopressors that promote intestinal ischaemia.
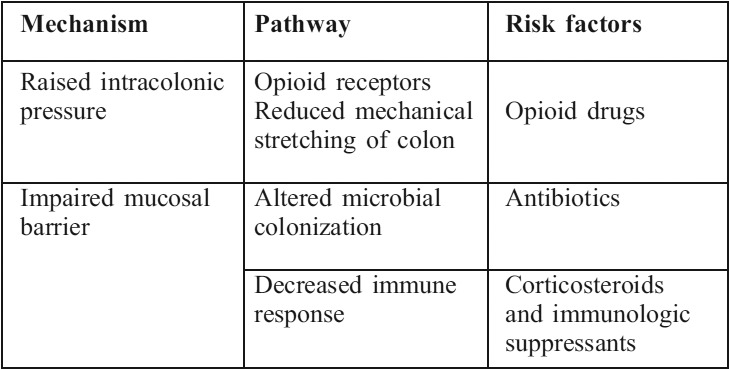
They also presented a low flow, especially in the splanchnic circulation. Another particularity concerns patients 2 and 3: administration of corticosteroids for the adsepjuvant treatment of ARDS (methylprednisolone a week before intestinal perforation). The presence of systemic infection that alters the integrity of the bowel, and systemic antibiotic therapy that alters intestinal flora could also be incriminated. Finally, these three burn patients received large doses of opioids because of their lengthy sedation. All factors that could predispose diverticular perforations are very common in burn patients and are summarized in Table I. In three patients the TBSA was 30 to 40%, less than what is reported by previous studies. Kowal-Vern A. et al. described ischaemic necrotic bowel disease in patients with more extensive burns (53% ± 10% TBSA).5
Table I. Potential risk factors in diverticular perforation in burn patients classified by biological mechanism of action (modified from Morris et al.14).
Large burns are commonly associated with a significant decrease in splanchnic perfusion. In animal studies, mesenteric blood flow usually decreases soon after the burn injury by more than 50% after a 40% TBSA burn.16 This is associated with an increase in mesenteric vascular resistance attributed to vasoactive mediators such as angiotensin II, vasopressin, and vasoactive intestinal polypeptide 4, and to inflammatory mediators released from burned tissues, such as thromboxane.17
Conclusion
Whether initial or late, the aim of burn resuscitation is to attain adequate vital organ perfusion in order to avoid multi-system organ failure. The vitality of the gastrointestinal barrier can be compromised by low blood flow, mucosal atrophy, or absence of enteral feeding. Our report demonstrates the need to optimize splanchnic perfusion in critically burned patients and highlights the multiple risk factors of sigmoid diverticulum perforation.
References
- 1.Still JM, jr, Scheirer RC, Law EJ. Caecal perforation due to colonic ulcer in a burn patient. Burns. 1994;20:85–6. doi: 10.1016/0305-4179(94)90116-3. [DOI] [PubMed] [Google Scholar]
- 2.Ghoneim IE, Bang RL. Caecal perforation in a burn patient. Burns. 1995;21:619–21. doi: 10.1016/0305-4179(95)00043-b. [DOI] [PubMed] [Google Scholar]
- 3.Cheng ES, Stringer KM, Pegg SP. Colonic necrosis and perforation following oral sodium polystyrene sulfonate (Resonium A®/Kayexalate®) in a burn patient. Burns. 2002;28:189–90. doi: 10.1016/s0305-4179(01)00099-7. [DOI] [PubMed] [Google Scholar]
- 4.Desai MH, Hemdon DN, Rutan RL, et al. Ischemic intestinal complications of patients with bums. Surg Gynecol Obstet. 1991;172:257. [PubMed] [Google Scholar]
- 5.Kowal-Vern A, McGill V, Gamelli RL. Ischemic necrotic bowel disease in thermal injury. Arch Surg. 1997;132:440–3. doi: 10.1001/archsurg.1997.01430280114020. [DOI] [PubMed] [Google Scholar]
- 6.Fitzgerald AM, Fried MJ, Anderson DN, et al. Colonic perforation following prolonged hypovolaemia in a major burns injury. Burns. 1999;25:527–30. doi: 10.1016/s0305-4179(99)00027-3. [DOI] [PubMed] [Google Scholar]
- 7.Hart AR, Kennedy HJ, Stebbings WS, et al. How frequently do large bowel diverticula perforate? An incidence and cross-sectional study. Eur J Gastroenterol Hepatol. 2000;12:661–5. doi: 10.1097/00042737-200012060-00016. [DOI] [PubMed] [Google Scholar]
- 8.Day TK. Intestinal perforation associated with osmotic slow release indomethacin capsules. BMJ. 1983;287:1671–2. doi: 10.1136/bmj.287.6406.1671-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Coutrot S, Roland D, Barbier J, et al. Acute perforation of colonic diverticula associated with short-term indomethacin. Lancet. 1978:1055–6. doi: 10.1016/s0140-6736(78)92385-1. [DOI] [PubMed] [Google Scholar]
- 10.Canter JW, Shorb PE., jr Acute perforation of colonic diverticula associated with prolonged adrenocorticosteroid therapy. Am J Surg. 1971;121:46–51. doi: 10.1016/0002-9610(71)90076-6. [DOI] [PubMed] [Google Scholar]
- 11.Candelas , Jover JA, Fernandez B, et al. Perforation of the sigmoid colon in a rheumatoid arthritis patient treated with methylprednisolone pulses. Scand J Rheumatol. 1998;27:152–3. doi: 10.1080/030097498441056. [DOI] [PubMed] [Google Scholar]
- 12.Weiner HL, Rezai AR, Cooper PR. Sigmoid diverticular perforation in neurosurgical patients receiving high-dose corticosteroids. Neurosurgery. 1993;33:40–3. doi: 10.1227/00006123-199307000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Corder A. Steroids, non-steroidal anti-inflammatory drugs, and serious septic complications of diverticular disease. BMJ ?1987;295:1238. doi: 10.1136/bmj.295.6608.1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Morris CR, Harvey IM, Stebbings WS, et al. Epidemiology of perforated colonic diverticular disease. Postgrad Med J. 2002;78:654–9. doi: 10.1136/pmj.78.925.654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Makela J, Kiviniemi H, Laitinen S. Prevalence of perforated sigmoid diverticulitis is increasing. Dis Colon Rectum. 2002;45:955–61. doi: 10.1007/s10350-004-6335-5. [DOI] [PubMed] [Google Scholar]
- 16.Herndon DN, Zeigler ST. Bacterial translocation after thermal injury. Crit Care Med. 1993;21(S2):S50–S54. doi: 10.1097/00003246-199302001-00010. [DOI] [PubMed] [Google Scholar]
- 17.Markell KW, Renz AM, White CE, et al. Abdominal complications after severe burns. J Am Coll Surg. 2009;208:940–7. doi: 10.1016/j.jamcollsurg.2008.12.023. [DOI] [PubMed] [Google Scholar]


