Abstract
Objectives
The purpose of this retrospective cohort study was to investigate the relationship between exposure of Korean workers to petrochemicals in the refinery/petrochemical industry and lymphohematopoietic cancers.
Methods
The cohort consisted of 8,866 male workers who had worked from the 1960s to 2007 at one refinery and six petrochemical companies located in a refinery/petrochemical complex in Korea that produce benzene or use benzene as a raw material. Standardized mortality ratios (SMRs) and standardized incidence ratios (SIRs) were calculated for 1992-2007 and 1997-2005 based on the death rate and cancer incidence rate of the Korean male population according to job title (production, maintenance, laboratory, and office workers).
Results
The overall mortality and most cause-specific mortalities were lower among these workers than those of the general Korean population. Increased SMRs were observed for leukemia (4/1.45; SMR 2.77, 95% CI: 0.75-7.09) and lymphohematopoietic cancers (5/2.51; SMR 2, 95% CI: 0.65-4.66) in production workers, and increased SIRs were also observed in leukemia (3/1.34; SIR 2.24, 95% CI: 0.46-6.54) and lymphohematopoietic cancers (5/3.39; SIR 1.47, 95% CI: 0.48-3.44) in production workers, but the results were not statistically significant.
Conclusion
The results showed a potential relationship between leukemia and lymphohematopoietic cancers and exposure to benzene in refinery/petrochemical complex workers. This study yielded limited results due to a short observational period; therefore, a follow-up study must be performed to elucidate the relationship between petrochemical exposure and cancer rates.
Keywords: Petrochemical, Leukemia, Refinery, Non-Hodgkin's lymphoma, Multiple myeloma, Cancer
Introduction
The refinery/petrochemical industry is indispensable because it produces fuels, plastic resins, rubber, and various chemicals including agricultural chemicals. However, employees working in the refinery/petrochemical industry are exposed to many hazardous chemicals. Among them, benzene, 1,3-butadiene, and ethylene oxide are representative carcinogens.
Many studies have been conducted to determine the relationship between exposure in the refinery/petrochemical industry and the increasing risk of cancer [1-9]. But no published report has been conducted on the cancer risk of Korean workers working in the refinery/petrochemical industry.
The refining industry began in the 1960s, and the full-scale petrochemical industry started in the 1970s in Korea. The refinery/petrochemical industry began first in Ulsan city, and other complexes were built in Yosu and Daesan. This retrospective cohort comprised 8,866 male workers who worked at a refinery/petrochemical complex where benzene was manufactured or used as a raw material.
We investigated the relationship between benzene exposure and lymphohematopoietic cancer mortality and morbidity in refinery/petrochemical industry workers.
Materials and Methods
Study population
The study population consisted of male workers in a refinery and petrochemical complex composed of one refinery and six large petrochemical factories. Among these, four factories and the refinery produce benzene, three factories had naphtha cracking centers, and two factories used benzene as a raw material to make other chemical products. Employee data for the seven factories, including resident registration numbers (a unique Korean identification number), date of employment and retirement, and departments were collected from the date of business initiation (the early 1960s) to Dec 31, 2007. Female workers were excluded from the study population. In total, 8,866 male workers with a work history of one or more days in the refinery/petrochemical complex were included in this study.
The most recent departments of the employees were used to categorize the workers into four groups: production, maintenance, laboratory, or office workers. The employees were also divided into manufacturing and office worker groups. The manufacturing workers included those employed in the processing operation (production), maintenance, and laboratory departments. The office workers included those in the sales department and the general office.
Cancer mortality and morbidity data
Mortality data are readily accessible in Korea, given the resident registration numbers, and the data were attained from the Korea National Statistical Office (KNSO). Data on mortality and causes of death were obtained for 16 years from Jan 1, 1992 to Dec 31, 2007. Causes of death were coded using the 10th Revision of the International Classification of Diseases. The cancer classification was in accordance with the KNSO classification (Korea Classification of Diseases and Causes of Death, 4th edition).
Cancer incidence was identified using the Central Registry of Cancer in Korea. Morbidity of the subjects was observed retrospectively for a 9-year period from Jan 1, 1997 to Dec 31, 2005.
Data analysis
The observation period for cancer mortality of the subjects was 16 years from Jan 1, 1992 to Dec 31, 2007. The 16-year observation period was divided into four calendar periods; 1992-1996, 1997-2001, 2002-2006, and 2007. National population data for 1994, 1999, 2005, and 2007 with 5-year age group intervals of those aged 20-80 years were used as the reference population.
For workers who were employed before Jan.1, 1992, and who died during the observation period, the number of person years was calculated from Jan 1, 1992 to the date of death. Subjects who survived throughout the study period were observed until the final date of this study, Dec 31, 2007. If workers were hired during the observational period, their person years were considered from the date of hire to the date of death or Dec 31, 2007. Workers who retired before the beginning of the observation period, Jan 1, 1992, were excluded from the study, as their mortality before 1992 could not be determined.
Standardized mortality ratios (SMRs) of all-cause mortality, overall cancer mortality, lymphohematopoietic cancer mortality, and other cancer mortalities were calculated after dividing the subjects into production, maintenance, laboratory and office workers, and into manufacturing and office workers. The expected numbers were calculated from age-specific national mortality rates for the 5-year age groups and 4 calendar periods.
Cancer morbidity was observed from Jan 1, 1997 to Dec 31, 2005. The standard population age groups with 5-year intervals who were aged 20-80 years of age in 2003 were used as the reference population. Standardized incidence rations (SIRs) were calculated, after calculating the expected numbers from age-specific cancer incidence rates for the 5-year age groups in 2003.
A SAS macro program was used to tabulate the number of case and person-years [10]. After indirect age standardization, SMRs, SIRs, and exact Poisson confidence intervals (CIs) were computed using another SAS macro program [11].
Results
General characteristics of subjects
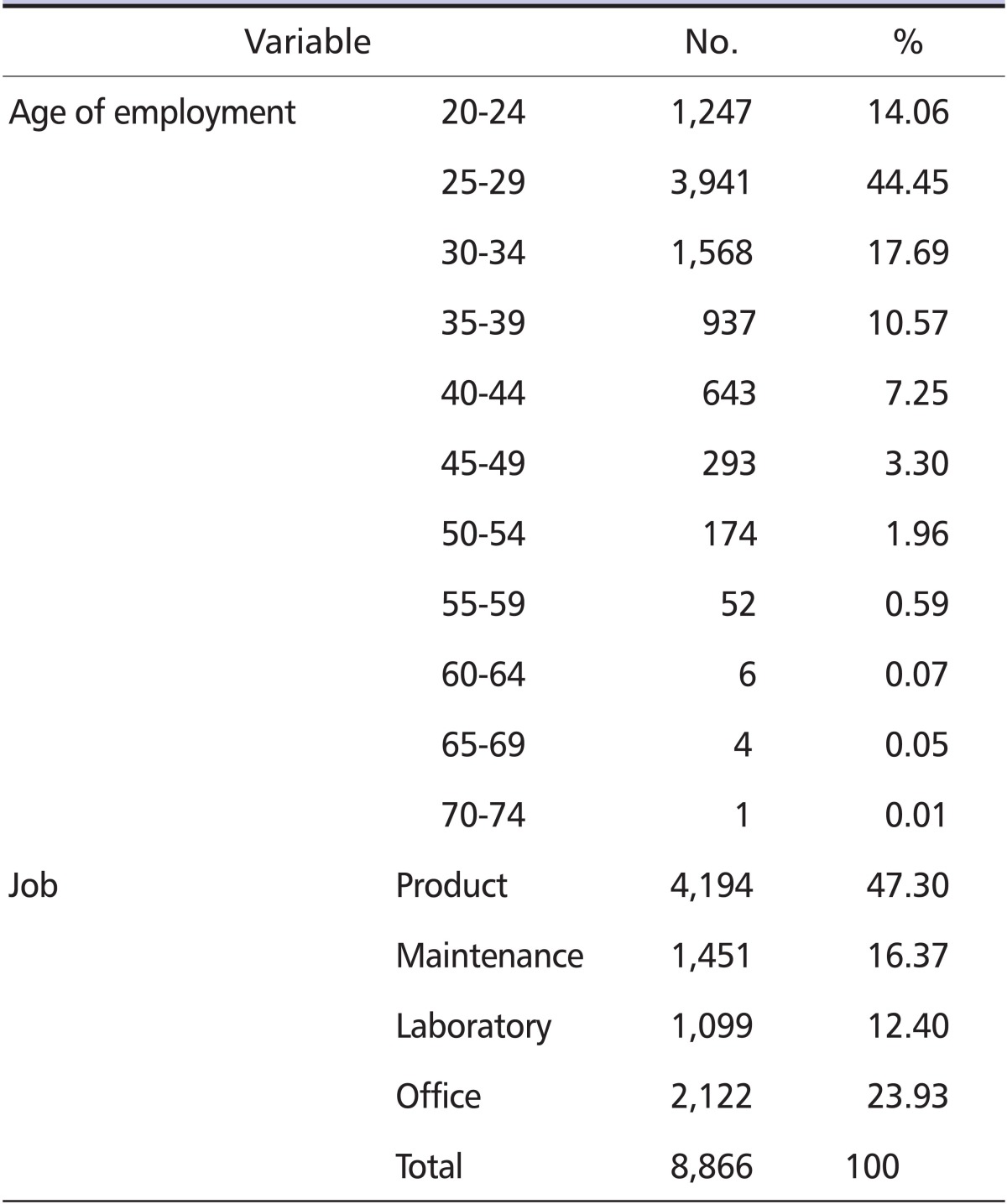
Subjects aged 20-29 years at the time of employment were 58.51% of all subjects. The largest proportion among the four job categories was production, with 47.3%. Manufacturing jobs, including production, maintenance, and laboratory jobs, were 76.07% of all jobs (Table 1).
Table 1.
General characteristics of study subjects
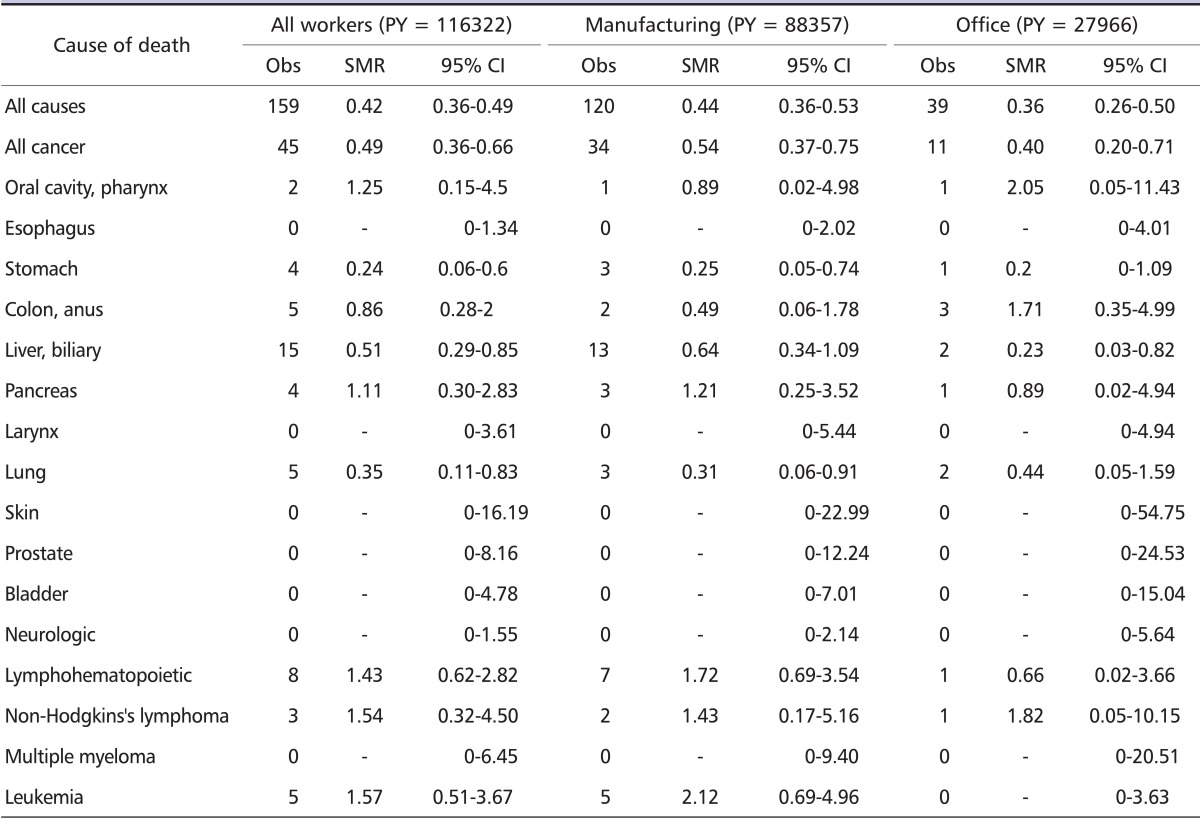
SMRs for all workers and by manufacturing/office job
SMRs of all-cause mortality and overall cancer mortality were calculated after dividing the subjects into manufacturing and office workers (Table 2). Although the SMRs of the two groups were significantly lower when compared with those of the general population, SMRs for leukemia (2.12; 95% CI: 0.69-4.96) and lymphohematopoietic cancers (1.72; 95% CI: 0.69-3.54) tended to be higher in manufacturing workers, compared with the general population. However the result was not significant.
Table 2.
Mortality results for all workers and by manufacturing/office job
PY: person-year, Obs: observed number, SMR: standardized mortality ratio, CI: confidence interval.
SMRs according to the four job classifications
After dividing subjects into production, maintenance, laboratory, and office workers, the SMRs for all-cause mortality, overall cancer mortality, and specific cancer mortalities were calculated. The SMRs for leukemia and lymphohematopoietic cancers were 2.77 (95% CI: 0.75-7.09) and 2 (95% CI: 0.65-4.66), respectively, in production workers. (Table 3).
Table 3.
Mortality results by four job classification
PY: person-year, Obs: observed number, SMR: standardized mortality ratio, CI: confidence interval.
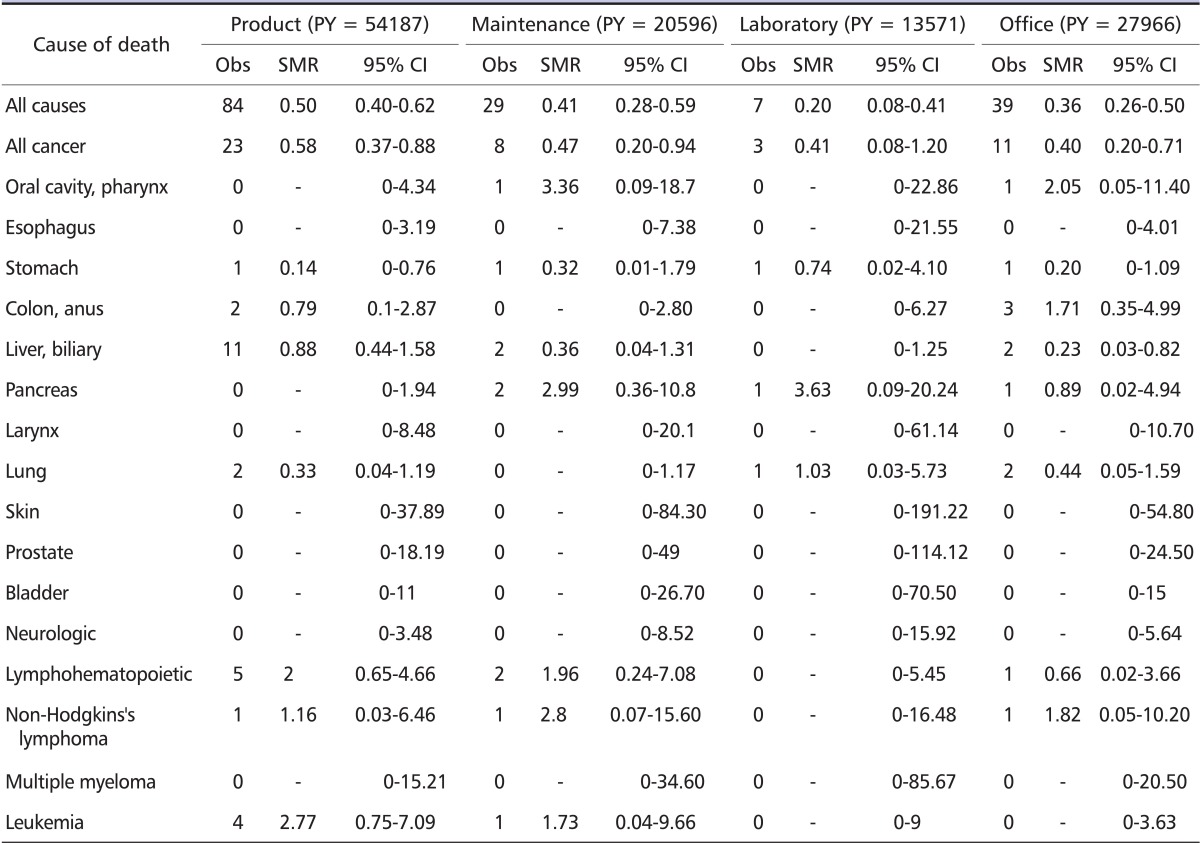
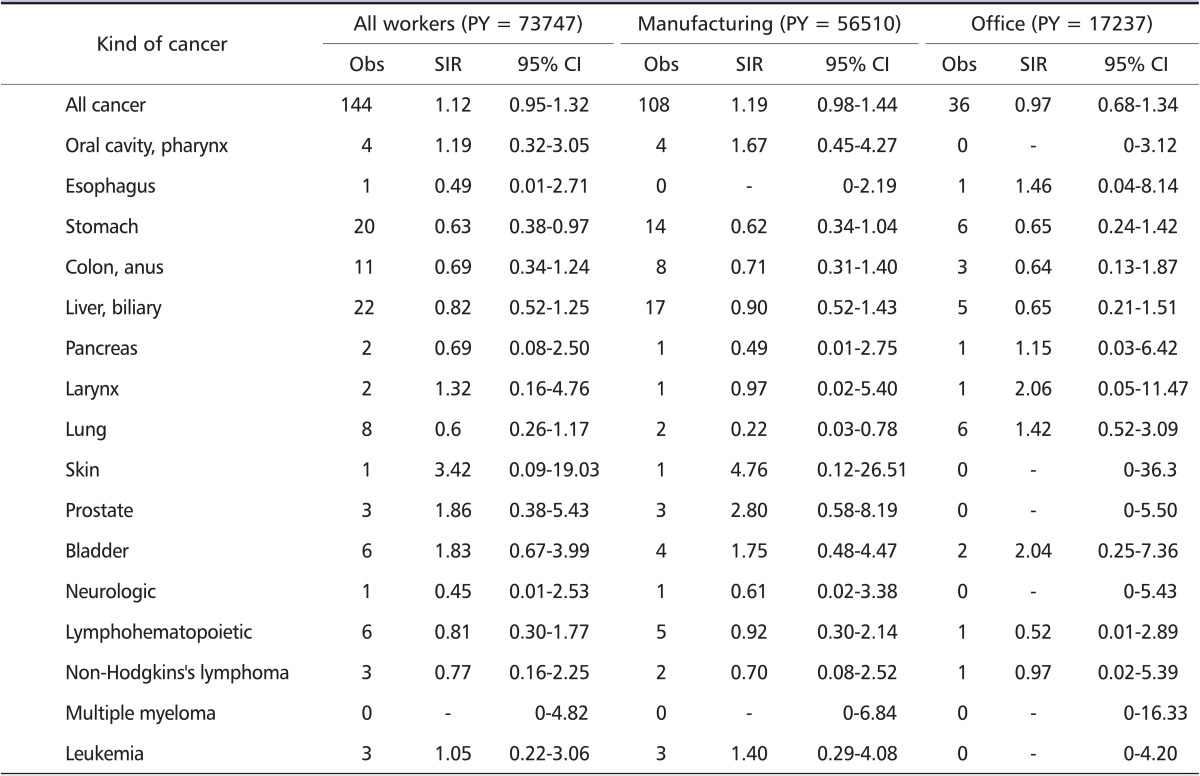
SIRs for all workers and by manufacturing/office job
SIRs for all overall cancer mortality and specific cancer mortalities were calculated after dividing subjects into manufacturing and office workers (Table 4). The SIR for leukemia (1.40; 95% CI: 0.29-4.08) increased in manufacturing workers, whereas the SIRs for non-Hodgkin's lymphoma (0.70; 95% CI: 0.08-2.52) and lymphohematopoietic cancers (0.92; 95% CI: 0.30-2.14) were lower than those in the general population.
Table 4.
Cancer morbidity results for all workers and by manufacture/office job
PY: person-year, Obs: observed number, SIR: standardized incidence ratio, CI: confidence interval.
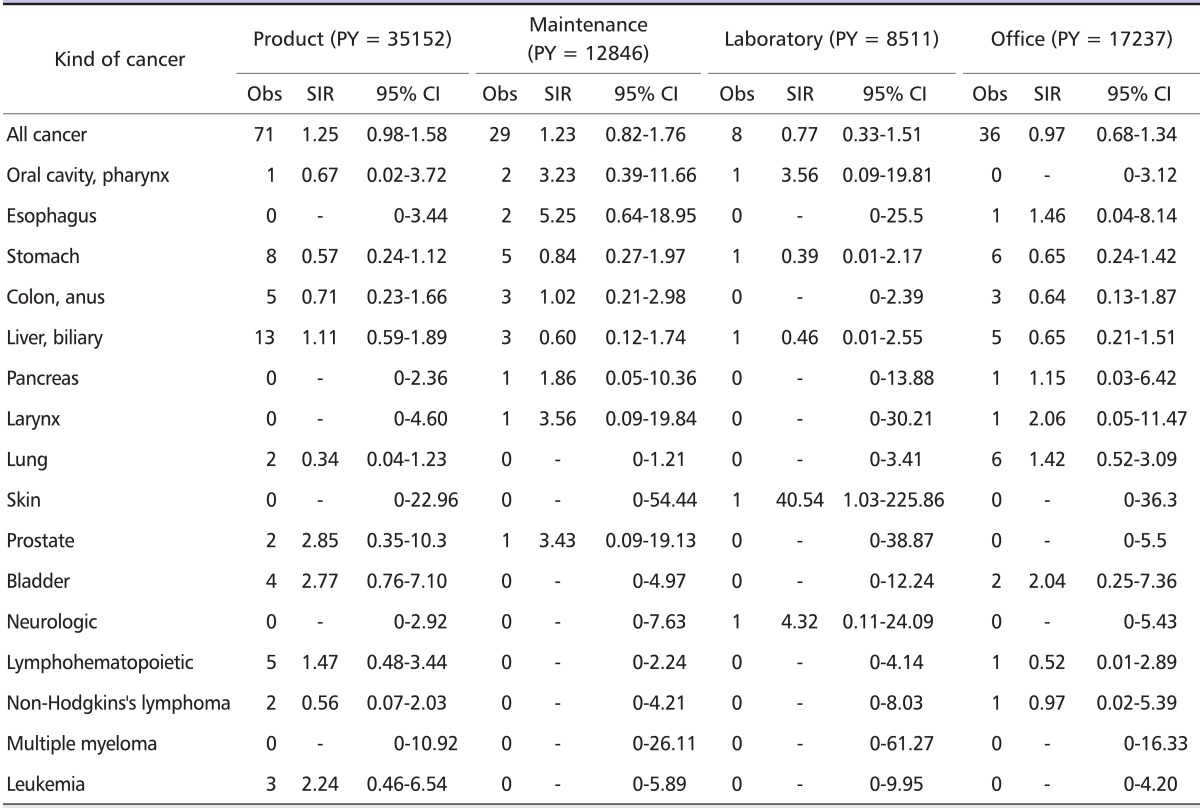
SIRs according to the four job classifications
SIRs for lymphohematopoietic cancers among production, maintenance, laboratory, and office workers were calculated (Table 5). The SIRs showed no significantly elevated risks for leukemia (2.24; 95% CI: 0.46-6.54) and lymphohematopoietic cancers (1.47; 95% CI: 0.48-3.44). The risk of non-Hodgkin's lymphoma among production workers (0.56; 95% CI: 0.07-2.03) appeared to be lower than that of the general Korean male population.
Table 5.
Cancer morbidity results by four job classification
PY: person-year, Obs: observed number, SIR: standardized incidence ratio, CI: confidence interval.
Discussion
According to the International Agency for Research on Cancer, the following are listed as carcinogens to humans (group 1) that cause lymphohematopoietic cancer. Benzene (acute non-lymphocytic leukemia and multiple myeloma), 1,3-butadiene (leukemia and lymphoma), ethylene oxide (leukemia), ionizing radiation (leukemia), the manufacture and repair of shoes/boot (leukemia), and the rubber industry (leukemia and lymphoma) for the use of benzene. Additionally, trichloroethylene (lymphoma) is classified as group 2A, probable carcinogens to humans, and chlorophenols and phenoxyacetic acid herbicides (lymphoma), gasoline (leukemia), hexachlorocyclohexane (leukemia), and 2,3,7,8-tetrachlorodibenzo-p-dioxin (lymphoma) are group 2B, possible carcinogens to humans [12]. Among these, benzene and 1,3-butadiene are largely used in the refinery and petrochemical industry, and might be exemplary carcinogens, causing lymphohematopoietic cancers in the refinery/petrochemical industry. Benzene exposure is generally accepted to cause acute myelogenous leukemia, but the association with multiple myeloma and non-Hodgkin's lymphoma seems to be controversial [13]. The number of workers possibly exposed to benzene was estimated to be 196,182 in Korea [14]. It is reported that Korean petrochemical workers can be exposed to high levels of benzene during turnaround maintenance [15].
Cohort studies on lymphohematopoietic cancers among workers exposed to benzene in the refinery/petrochemical industry have been conducted mainly in large enterprises. Some studies have presented significantly elevated risks of lymphohematopoietic cancers. For example, Lewis et al. performed a follow-up study with employees working in oil refining companies from 1964 to 1994 and showed that the SMR of multiple myeloma alone increased to 1.94 (16/8.26; 95% CI: 1.11-3.15) among marketing and distribution workers [2]. However, many studies have shown insignificant or even decreased risks of lymphohematopoietic cancers. A follow-up study on the incidence of cancer in 5,614 workers of a petrochemical research facility in 1986-1997 conducted by Sathiakumar et al. found that the SIR of non-Hodgkin's lymphoma rose to 182 (95% CI: 94-318) [3]. Rodu et al. showed that the SMRs of non-Hodgkin's lymphoma and leukemias were 125 (95% CI: 51-259) and 38 (95% CI: 5-136), respectively, by performing a follow-up study on 6,956 employees of a petrochemical research facility from 1970 to 1996 [4]. Gamble et al. reported that the SMR of lymphohematopoietic cancers (113; 95% CI: 92-138) slightly increased in a study of 6,238 retired workers [16]. Tsai et al. performed a follow-up study with 4,639 active and former employees and retirees of Shell Oil Company from 1983 to 1999 and showed that the SIRs of non-Hodgkin's lymphoma (0.41; 95% CI: 0.13-0.95) and leukemia (0.43; 95% CI: 0.09-1.25) were rather reduced and only the SIR of multiple myeloma was slightly increased at 1.23 (95% CI: 0.34-3.15) [7]. According to the results of a follow-up study conducted by Tsai et al. with 4,221 workers in the Louisiana oil refining and petrochemical industries, the SMR of overall lymphohematopoietic cancers (0.83; 95% CI: 0.47-1.38) was lower compared with the reference population, with concurrent lower SMRs for the workers employed for more than 10 years [6]. Through a follow-up study of 28,480 subjects from 1947 to 1993, the Texaco Mortality Study performed by Divine et al. reported that the SMRs of lymphohematopoietic cancers and leukemia were not higher in refinery/petrochemical workers compared with a reference population of 99 (95% CI: 87-113) and 101 (95% CI: 81-123), respectively [1]. Gun et al. also reported that the SIRs of all leukemia and acute non-lymphocytic leukemia were not significantly different from unity in an Australian petroleum industry cohort [17]. This inconsistency of results may be mainly due to sparse cases of lymphohematopoietic cancer and improvement of the work environment. Nonetheless, even low-level exposure to benzene at levels of < 1 ppm could decrease progenitor cells and affect the genetically susceptible subpopulation [18]. Therefore, follow-up studies must continue despite the recent low level exposure in the work environment.
Our study revealed significantly lower SMRs for allcause mortality and overall cancer mortality in refinery and petrochemical workers compared with the general population. These very low SMRs of all-cause mortality and overall cancer mortality represent a large healthy worker effect. However, the SMRs of leukemia and lymphohematopoietic cancers among the subjects were increased to 2.77 (95% CI: 0.75-7.09) and 2 (95% CI: 0.65-4.66). Furthermore, the SIRs of leukemias (2.24; 95% CI: 0.46-6.54) and lymphohematopoietic cancers (1.47; 95% CI: 0.48-3.44) among manufacturing workers also increased. SMRs and SIRs rose compared with the reference population, but the differences were not statistically significant, because the statistical power was low due to the small number of lymphohematopoietic cancers and short follow-up duration. Compared with very low all-cause and overall cancer mortalities, even non-significant elevations in mortalities might suggest an association between benzene exposure and lymphohematopoietic cancers.
The latent period for lymphohematopoietic cancers is about 5 years, which is shorter than that for solid tumors, which have a latency of 10-20 years. However, the short latent period may be applicable when workers are exposed to high concentrations of carcinogens, such as benzene. If workers are exposed to low concentrations, the latent period could be prolonged for much longer. In this regard, Aksoy, Vigliani, and Yin et al. reported average latent periods of 6-14, 3-23, and 11.4 years for lymphohematopoietic cancers caused by benzene, respectively [19-21]. In our study, we could not apply a lag time because the follow-up period was short and the cases were scarce. However, follow-up studies are necessary in the future, as the current study may have underestimated the risk due to the short observation period and lack of exposure assessment.
In a follow-up study on cancer with 8,942 oil refining and petrochemical workers for 1983-1994, Huebner et al. divided subjects into processing operators, mechanical workers, technicians, and office-based workers, and investigated the SIRs of lymphohematopoietic cancers [22]. We also divided subjects into two groups of manufacturing and office workers, and four groups of production, maintenance, laboratory, and office workers, and calculated SMRs and SIRs for the lymphohematopoietic cancers. Merely dividing subjects by their job titles would have led to severe misclassification. Moreover, their assigned jobs were classified according to the last department they worked in. It would be preferable to classify individuals by their first job, because manufacturing workers with long job durations can move to office jobs. However, we could not obtain enough data about employees' first jobs, and this shortage of data may have caused a dilution effect by including unexposed subjects in the analysis of cohort [23].
In a study on the relationship between exposure to benzene and leukemia with 74,828 workers exposed to benzene and 35,805 non-exposed workers in China conducted by Hayes et al., it was concluded that the risk of leukemia increased significantly with cumulative doses of benzene over 40 ppm-years (for example, 1 ppm exposure for 40 years) [24]. The amount of exposure could differ with employment time period, and generally the amount of exposure is considered to have been higher in the past. Huebner et al. conducted a follow-up study with 7,637 and 7,007 workers of the oil refining and petrochemical industries in Baton Rouge and Baytown, respectively, during 1970-1997 [5]. They showed that, after dividing workers' hire years into three groups; before 1940, 1940-1944, and 1945-1949, the SMRs for total lymphohematopoietic cancers were higher in the earlier years of employment, at 1.87, 1.65, and 1.36, respectively. The SMRs for non-Hodgkin's lymphoma were 2.11, 1.38, and 1.39, and those for leukemia were 2.41, 1.96, and 1.33, respectively. Our cohort was young, so the exposure amount would be lower than those of the earlier studies, and this might have resulted in underestimation of the effect of benzene.
A dose-response relationship should be considered to determine the correlation between exposure to hazardous chemicals and an outbreak of cancer. For this, it is ideal to evaluate the relationship by making a job-exposure matrix using the amount and duration of exposure. However, determining the amount and duration of exposure were impossible in our study, as it was performed with workers in seven factories and we could not obtain enough information about work environment exposure and old job history. A re-analysis after constructing a job-exposure matrix might lead to different results.
The classification of outcome variables is very important in cohort studies. In particular, as the number of lymphohematopoietic cancers is very low, misclassification of output can affect results to a large degree. We matched cohort subjects' data with national death and cancer registries; however, the precision of the output is dependent on the completeness and accuracy of the registry. Incompleteness of registries might be a limitation to some degree.
Another limitation of our study is that we could not control for possible confounding variables acting on the relationship between exposure and cancer, such as smoking, drinking, and socioeconomic status.
In conclusion, the SMRs for leukemia (2.77; 95% CI: 0.75-7.09) and lymphohematopoietic cancers (2; 95% CI: 0.65-4.66), and the SIRs for leukemia (2.24; 95% CI: 0.46-6.54) and lymphohematopoietic cancers (1.47; 95% CI: 0.48-3.44) tended to be higher in production workers, but the results were not statistically significant. Although lymphohematopoietic cancers mortality did not increase significantly in this study, the overall mortality and overall cancer mortality were significantly lower in these subjects than in the general population. The results suggest a possible correlation between occupational exposure and lymphohematopoietic cancers.
Acknowledgements
This study was performed as a part of a cohort project on cancer outbreaks among workers of petrochemical complex and was conducted by the Occupational Safety and Health Research Institute (OSHRI) in 2007-2009.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Divine BJ, Hartman CM, Wendt JK. Update of the Texaco mortality study 1947-93: Part I. Analysis of overall patterns of mortality among refining, research, and petrochemical workers. Occup Environ Med. 1999;56:167–173. doi: 10.1136/oem.56.3.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lewis RJ, Schnatter AR, Katz AM, Thompson FS, Murray N, Jorgensen G, Thériault G. Updated mortality among diverse operating segments of a petroleum company. Occup Environ Med. 2000;57:595–604. doi: 10.1136/oem.57.9.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sathiakumar N, Delzell E, Rodu B, Beall C, Myers S. Cancer incidence among employees at a petrochemical research facility. J Occup Environ Med. 2001;43:166–174. doi: 10.1097/00043764-200102000-00017. [DOI] [PubMed] [Google Scholar]
- 4.Rodu B, Delzell E, Beall C, Sathiakumar N. Mortality among employees at a petrochemical research facility. Am J Ind Med. 2001;39:29–41. doi: 10.1002/1097-0274(200101)39:1<29::aid-ajim3>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 5.Huebner WW, Wojcik NC, Rosamilia K, Jorgensen G, Milano CA. Mortality updates (1970-1997) of two refinery/petrochemical plant cohorts at Baton Rouge, Louisiana, and Baytown, Texas. J Occup Environ Med. 2004;46:1229–1245. [PubMed] [Google Scholar]
- 6.Tsai SP, Wendt JK, Cardarelli KM, Fraser AE. A mortality and morbidity study of refinery and petrochemical employees in Louisiana. Occup Environ Med. 2003;60:627–633. doi: 10.1136/oem.60.9.627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tsai SP, Chen VW, Fox EE, Wendt JK, Cheng Wu X, Foster DE, Fraser AE. Cancer incidence among refinery and petrochemical employees in Louisiana, 1983-1999. Ann Epidemiol. 2004;14:722–730. doi: 10.1016/j.annepidem.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 8.Satin KP, Wong O, Yuan LA, Bailey WJ, Newton KL, Wen CP, Swencicki RE. A 50-year mortality follow-up of a large cohort of oil refinery workers in Texas. J Occup Environ Med. 1996;38:492–506. doi: 10.1097/00043764-199605000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Collins JJ, Ireland B, Buckley CF, Shepperly D. Lymphohaematopoeitic cancer mortality among workers with benzene exposure. Occup Environ Med. 2003;60:676–679. doi: 10.1136/oem.60.9.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Examples and programs for splitting follow-up tiem in cohort studeis [Internet] Copenhagen: Institute of Public Health, University of Copenhagen; 2005. [cited 2009 Nov 3]. Available from: http://staff.pubhealth.ku.dk/~bxc. [Google Scholar]
- 11.Daly L. Simple SAS macros for the calculation of exact binomial and Poisson confidence limits. Comput Biol Med. 1992;22:351–361. doi: 10.1016/0010-4825(92)90023-g. [DOI] [PubMed] [Google Scholar]
- 12.Complete list of agents and their classification [Internet] Lyon: International Agency for Research on Cancer (IARC); [cited 2009 Nov 3]. Available from: http://www.iarc.fr. [Google Scholar]
- 13.Kirkeleit J, Riise T, Bråtveit M, Moen BE. Increased risk of acute myelogenous leukemia and multiple myeloma in a historical cohort of upstream petroleum workers exposed to crude oil. Cancer Causes Control. 2008;19:13–23. doi: 10.1007/s10552-007-9065-x. [DOI] [PubMed] [Google Scholar]
- 14.Chung EK, Shin JA, Lee BK, Kwon JW, Lee JW, Chung KJ, Lee JH, Lee IS, Kang SK, Jang JK. Characteristics of occupational exposure to benzene during turnaround in the petrochemical industries. Saf Health Work. 2010;1:51–60. doi: 10.5491/SHAW.2010.1.1.51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kang SK, Lee MY, Kim TK, Lee JO, Ahn YS. Occupational exposure to benzene in South Korea. Chem Biol Interact. 2005;153:65–74. doi: 10.1016/j.cbi.2005.03.011. [DOI] [PubMed] [Google Scholar]
- 16.Gamble JF, Lewis RJ, Jorgensen G. Mortality among three refinery/petrochemical plant cohorts. II. Retirees. J Occup Environ Med. 2000;42:730–736. doi: 10.1097/00043764-200007000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Gun RT, Pratt N, Ryan P, Roder D. Update of mortality and cancer incidence in the Australian petroleum industry cohort. Occup Environ Med. 2006;63:476–481. doi: 10.1136/oem.2005.023796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lan Q, Zhang L, Li G, Vermeulen R, Weinberg RS, Dosemeci M, Rappaport SM, Shen M, Alter BP, Wu Y, Kopp W, Waidyanatha S, Rabkin C, Guo W, Chanock S, Hayes RB, Linet M, Kim S, Yin S, Rothman N, Smith MT. Hematotoxicity in workers exposed to low levels of benzene. Science. 2004;306:1774–1776. doi: 10.1126/science.1102443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aksoy M. Benzene and leukemia. Environ Health Perspect. 1991;91:165–166. doi: 10.1289/ehp.9191165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Vigliani EC. Leukemia associated with benzene exposure. Ann N Y Acad Sci. 1976;271:143–151. doi: 10.1111/j.1749-6632.1976.tb23103.x. [DOI] [PubMed] [Google Scholar]
- 21.Yin SN, Li GL, Tain FD, Fu ZI, Jin C, Chen YJ, Luo SJ, Ye PZ, Zhang JZ, Wang GC. Leukaemia in benzene workers: a retrospective cohort study. Br J Ind Med. 1987;44:124–128. doi: 10.1136/oem.44.2.124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Huebner WW, Chen VW, Friedlander BR, Wu XC, Jorgensen G, Bhojani FA, Friedmann CH, Schmidt BA, Sales EA, Joy JA, Correa CN. Incidence of lymphohaematopoietic malignancies in a petrochemical industry cohort: 1983-94 follow up. Occup Environ Med. 2000;57:605–614. doi: 10.1136/oem.57.9.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Parodi S, Gennaro V, Ceppi M, Cocco P. Comparison bias and dilution effect in occupational cohort studies. Int J Occup Environ Health. 2007;13:143–152. doi: 10.1179/oeh.2007.13.2.143. [DOI] [PubMed] [Google Scholar]
- 24.Hayes RB, Yin SN, Dosemeci M, Li GL, Wacholder S, Travis LB, Li CY, Rothman N, Hoover RN, Linet MS Chinese Academy of Preventive Medicine--National Cancer Institute Benzene Study Group. Benzene and the dose-related incidence of hematologic neoplasms in China. J Natl Cancer Inst. 1997;89:1065–1071. doi: 10.1093/jnci/89.14.1065. [DOI] [PubMed] [Google Scholar]