Abstract
The majority of people diagnosed with diabetes mellitus are in the working age group in developing countries. The interrelationship of diabetes and work, that is, diabetes affecting work and work affecting diabetes, becomes an important issue for these people. Therapeutic options for the diabetic worker have been developed, and currently include various insulins, insulin sensitizers and secretagogues, incretin mimetics and enhancers, and alpha glucosidase inhibitors. Hypoglycemia and hypoglycaemic unawareness are important and unwanted treatment side effects. The risk they pose with respect to cognitive impairment can have safety implications. The understanding of the therapeutic options in the management of diabetic workers, blood glucose awareness training, and self-monitoring blood glucose will help to mitigate this risk. Employment decisions must also take into account the extent to which the jobs performed by the worker are safety sensitive. A risk assessment matrix, based on the extent to which a job is considered safety sensitive and based on the severity of the hypoglycaemia, may assist in determining one's fitness to work. Support at the workplace, such as a provision of healthy food options and arrangements for affected workers will be helpful for such workers. Arrangements include permission to carry and consume emergency sugar, flexible meal times, self-monitoring blood glucose when required, storage/disposal facilities for medicine such as insulin and needles, time off for medical appointments, and structured self-help programs.
Keywords: Blood glucose awareness training (BGAT), Fitness to work, Hypoglycemic unawareness, Safety sensitive, Self-monitoring blood glucose
Introduction
Diabetes mellitus (DM) is now a major global health threat [1]. Worldwide numbers of affected people are expected to increase from an estimated 235 million in 2010 to 435 million in the year 2030 [2]. Statistics such as these have prompted the World Economic Forum to rank chronic diseases, of which diabetes is unarguably dominant, among three major risk areas in order to discuss the diseases in its Global Risks Network Report [3]. The growing burden of the disease is more acute in developing countries because of the higher prevalence of diabetes in the working age group of 40 to 60 years, compared to developed countries, where the majority with the disease is above 60 years of age [2].
Diabetes Mellitus Affecting Work
The multidimensional nature of diabetes is well known. A holistic approach for its management is necessary [4] to reduce both microvascular and macrovascular complications [5,6]. Time and effort is required for adherence to a treatment regime that requires scheduled screening for retinopathy, foot, renal, and cardiovascular risk factors [7]. Most of these factors take time to develop, and its impact on work is probably not immediate, allowing time for affected workers, their supervisors, and physicians to adjust to changing circumstances.
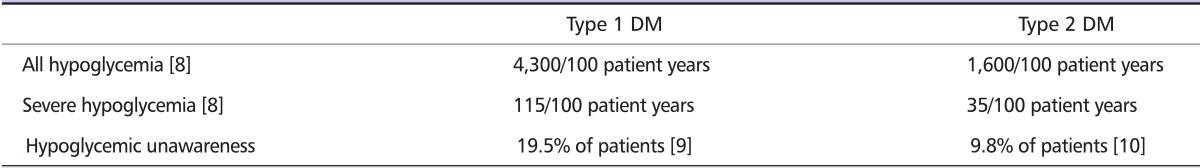
A major immediate concern in the management of workers with diabetes is the impact of hypoglycemia, quite often an iatrogenic effect of diabetes management. This condition is not rare (Table 1). In one study, 101 of 518 type1 diabetics above 16 years of age with diabetes durations exceeding two years had hypoglycemic unawareness in the preceding year [9]. In another study, twelve out of 122 insulin type2 diabetics using two or more insulin injections a day were noted to have hypoglycemic unawareness in the preceding year [10].
Table 1.
Prevalence of hypoglycemia and type 1 and type 2 DM patients
DM: diabetes mellitus.
Hypoglycemia - A Safety Risk
Glucose is the obligate fuel for the brain. Glucose deprivation will result in cognitive impairment. When the blood sugar falls below 4 mmol/l, the response of the normal human body is to stop all endogenous insulin secretion. Protective behavioral responses, such as feeding, commence, together with the stimulation of glucagon. This response may, however, be inadequate in a diabetic patient.
The neurogenic and neuroglycopenic effects elicited through sympathetic arousal, such as perspiration, palpitations, hunger, giddiness, and tremors are often familiar to diabetic patients. This response is mediated by catecholamines. The level of distress caused by such effects is not often appreciated by others, even by doctors. Secretion of cortisol and growth hormones form the latter stages of the hypoglycemic response [11].
Hypoglycaemic Unawareness
The ultimate fear and threat to safety in relation to hypoglycemia is the phenomena of hypoglycemic unawareness. Inadequate responses to antecedent repeated exposures to hypoglycemia can result in an altered lowered threshold to the activation and perception of hypoglycemia arousal.
Thus, such a diabetic worker may have lowered blood sugar levels, posing an increasing fuel deprivation risk to the brain without his realizing it. His window for corrective intervention becomes progressively narrower and narrower till he plunges directly into a state of severe cognitive impairment. Sometimes, a co-worker may be the best person to have observed this actually happening, as for example, noticing a diabetic colleague behaving in an uncharacteristic manner. Fortunately, for most diabetics who have had hypoglycemic unawareness, the condition can be reversed [12].
The impact of hypoglycemia on cognitive functioning will also depend on the complexity of the task at hand [13]. In an environment that demands multiple foci of attention and judgment, e.g., the cockpit of an airplane, or the intensive care unit in a hospital, this impact becomes critical.
Studies have also shown that following a hypoglycemic episode of 3.1 mmol/L, reaction times do not return to normal until 20 to 30 minutes after euglycemia has been restored [14]. Subsequent experimental data in type 1 DM patients also suggests that some aspects of cognitive function remain impaired for a clinically significant time after the correction of hypoglycemia [15].
Hypoglycemia and Safety Sensitive Jobs
Safety-sensitive jobs are ones where impaired performance, for whatever reason, could result in significant risks of harm to the health or safety of the worker. In addition, this risk may also affect the environment and the health or safety of co-workers [16]. To this, some legal authorities have further qualified that it must be also be a job performed with little or no supervision [17].
The concept of safety sensitive jobs is often traced to the implementation of drug and alcohol testing policies at the workplace. However, the classification of jobs as safety sensitive for this purpose is mainly for identifying who in the workplace should be included for drug and alcohol screening, in a just and fair manner. The actions that follow upon the identification of a positive test are driven by standard operational procedures.
In the context of diabetes, the identification of safety sensitive jobs and whether a diabetic worker should be allowed to work these jobs should be part of a much wider picture of risk assessment.
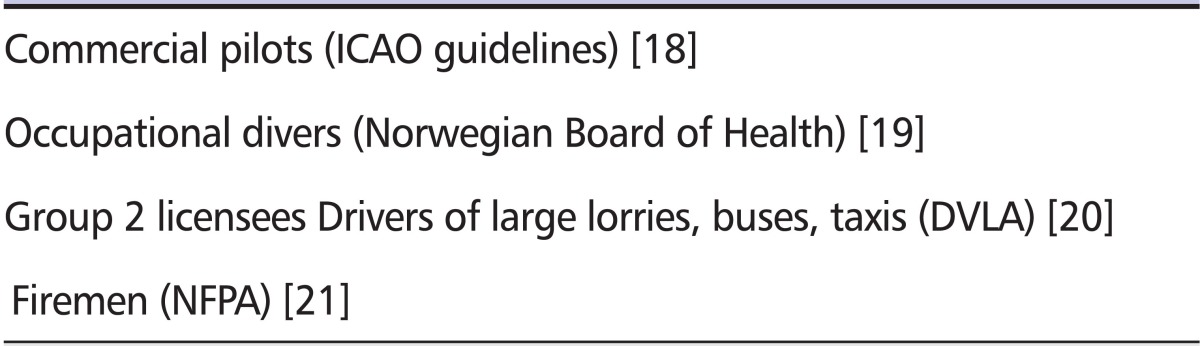
Arising from a fear of what can happen, people with diabetes, especially type1 DM, are usually barred from certain jobs, such as pilots, as a matter of policy (Table 2). In a way, it is the collective judgment of society being applied to a small select group of occupations, deemed to be complex and demanding of a state of high alertness. A number of these guidelines have international acceptance.
Table 2.
Insulin treatment and examples of restrictions for certain types of employment
ICAO: International Civil Aviation Organization, DVLA: Driver and Vehicle Licensing Agency, UK, NFPA: National Fire Protection Association, US.
In many countries, there are also regulations that specify restrictions on the driving of heavy goods vehicles, buses, or public transport vehicles, such as taxis, by insulin-treated patients.
Some inroads have been made to lift the restrictions for insulin-treated diabetics applying or continuing to be in employment in such jobs. These restrictions are almost universally qualified by fulfillment of strict documented conditions. These include stipulations that the diabetic worker has no episodes of severe hypoglycemia (defined as requiring assistance of another individual) in the preceding 1 year, and with no more than one episode of severe hypoglycemia in the preceding 5 years. Other requirements may include mandatory self-glucose monitoring with a meter that has a memory chip, and a signed statement testifying to satisfactory management by a diabetologist [18].
Fitness for Other Jobs
The fear of hypoglycemia, especially with insulin use, may also trigger reluctance for employers and doctors alike to recommend people as fit for jobs outside the select group of occupations that are governed by established regulations.
Such jobs and safety sensitive situations can be liberally contemplated - the helper working in a crowded hectic kitchen (slips and falls), the refinery operator who has to enter a confined space and work at heights (danger to plant safety), the police on his regular beat (firearms handling), and many other jobs that entail exposure to chemicals, moving parts, and mental stress.
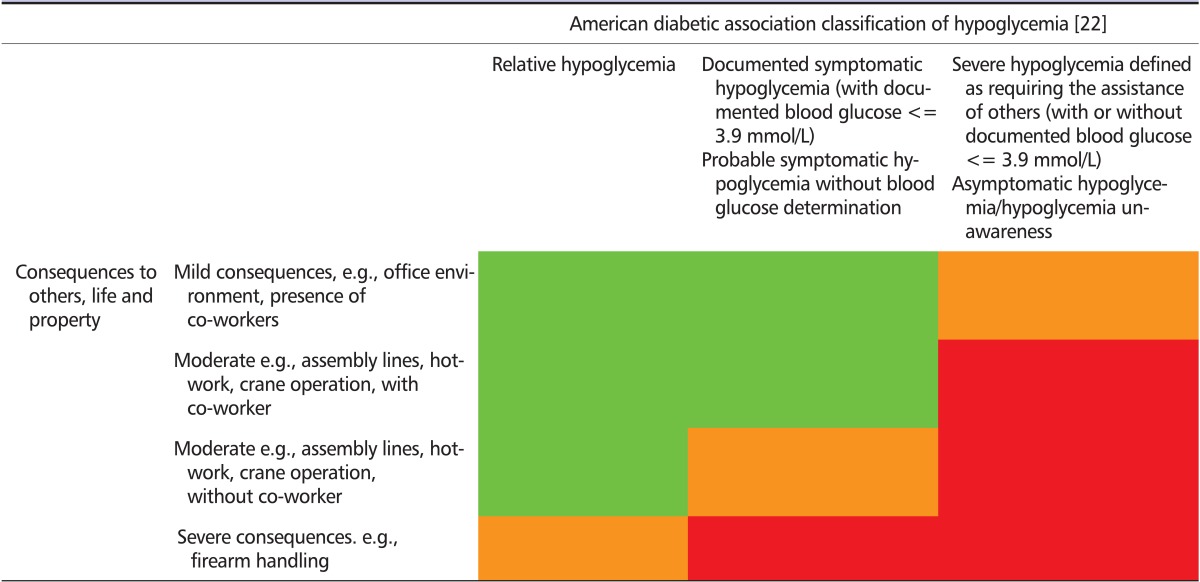
These concerns are real and should not be dismissed. A risk assessment and decision matrix, based on the extent to which a job is considered safety sensitive is suggested in Table 3. The aim is to rehabilitate the patient so that he can be helped to work safely in all these jobs. The interim decision on the fitness to work of a worker with hypoglycemia will be guided by its severity and his recovery, not only from the hypoglycemia, but also his recovery with respect to his hypoglycemia awareness and avoidance of future episodes.
Table 3.
Risk assessment and decision matrix for employment of diabetics with hypoglcyemia
 Intensify medical intervention Continuous improvement.
Intensify medical intervention Continuous improvement.
 Intensify medical intervention Urgent action, discuss with employer, may need to enhance work operations, including increased supervision and surveillance.
Intensify medical intervention Urgent action, discuss with employer, may need to enhance work operations, including increased supervision and surveillance.
 Intensify medical intervention Immediate action: discuss with employer, may need temporary removal from task and job until remedial action has been taken and completed.
Intensify medical intervention Immediate action: discuss with employer, may need temporary removal from task and job until remedial action has been taken and completed.
Many jobs which ostensibly have safety sensitive implications, may, on closer scrutiny, turn out not to be this sensitive.
A condominium guard who is not required to handle firearms and whose job is to alert for help in the event of emergency is an example. The presence of co-workers can also be a mitigating factor. Many work operations are also highly automated. Alarms are set in place for safety protection.
Balanced against this are factors that can worsen a hypoglycemic risk, e.g. sleep deprivation resulting in fatigue often seen in shift work may worsen hypoglycemic unawareness.
A decision based on fitness should be individualized, based on the person and the circumstances of his job.
Danger of Hypoglycemia Resulting from Treatment
Despite modern advances, the pharmacological mimicry of the normal physiological glycemic response is not perfect. All pharmacological agents, with their fixed mode and duration of action, are unable to achieve the kind of fine tuned glucose homeostasis seen in normal human physiology, which keep glucose levels within a narrow range.
In the continuing efforts to overcome hyperglycemia, hypoglycemia will continue to be a common challenge in treatment - especially as standards of care continue to drive patients to optimal A1C targets of 7% or even lower.
The risk of hypoglycaemia from pharmacological modalities to treat hyperglycemia varies, with insulin use carrying the highest risk compared to oral agents [23]. In a study of type 2 patients randomized to various treatments for 6 years from the time of diagnosis, the risk was estimated to vary from 5.3% for those on a basal and bolus insulin combination to 3.8% for those on a basal insulin monotherapy, to 1.2% for those on sulphonylurea [23].
Evidence for the benefits of early and effective achievement of glycemic targets to avoid long term macrovascular and microvascular complications related to hyperglycemia frequently results from a combination of agents being used.
Understanding the Use and Effects of Diabetic Medication
The use of insulin cannot be avoided in many patients, besides those with type1 DM. Patients with type2 DM who are at the insulinopenic end of the disease spectrum will require the use of insulin. Indeed, of all the agents in the armamentarium for hyperglycemia, insulin remains the most potent, without a limit to its A1C lowering capability, unlike the other agents.
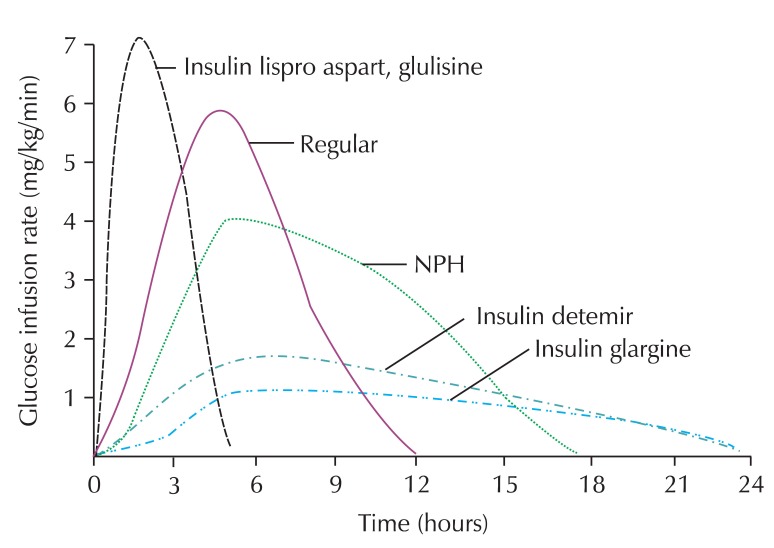
The peak action of insulin corresponds generally to the highest potential hypoglycemic risk. Understanding this and the duration of action of the different insulins and correlating these to lifestyle factors such as meal times and physical activity become crucial (Fig. 1). There is some variation between individuals in their response to the same medication. The peak of administered insulin or insulin secretagogues action must coincide with the estimated glucose peak from food absorption.
Fig. 1.
Activity profiles of different types of insulin. Reprinted with permission from diabetes education online, diabetes teaching center. NPH: neutral protamine hagedorn.
Copyright © 2009 The Regents of the University of California, all rights reserved, www.deo.ucsf.edu.
The rapid acting insulin analogues (insulin aspart, glulisine, and lispro) have an onset of action within fifteen minutes and peak relatively early. For workers requiring bolus insulin, its use has the flexible advantage of allowing them to eat almost immediately following the injection.
Choice of Insulins for the Working Patient
The choice of insulins for the physician and the patient has widened considerably in recent years. Therefore, selecting the appropriate insulin to best suit an individual's lifestyle and their occupational profile can and should be done.
Basal insulin analogues, being relatively peakless, may be administered as an insulin monotherapy. These include glargine, which has a duration of action lasting 24 hours [24]. Another option is detemir, which, depending on the dose, has a variable duration of action between 16 to 24 hours and a small weight gain effect [25,26]. Such insulin use may find favor with shift workers, who have erratic sleep/wake schedules and meal times.
However, its use alone may not be adequate for glycemic control, especially if postprandial glucose levels remain high. Thus, its combination with short acting insulins, such as human regular insulin, or rapid acting insulin analogues, such as glulisine, aspart, and lispro, may be medically indicated.
In other instances, pre-mix insulins may also be administered. Continuous subcutaneous insulin infusion is another modality favored by a select group of motivated patients. It may be necessary to seek the advice of a physician with the necessary experience in insulin use to help the worker achieve the twin goals of target A1C and safety at work.
Insulin Secretagogues
Insulin secretagogues, such as the sulphonylureas, have been used for many years. As a class, the side effect of hypoglycemia is well known. Some of the newer generation secretagogues, such as the metaglitinides, have been promoted based on their shorter durations of action, minimizing the risk of hypoglycemia.
Insulin Sensitizers
The risk of hypoglycemia in this class of agents, which includes metformin and the peroxisome proliferator activated receptor gamma (ppar-gamma) agonists, collectively known as thiazolidinediones, is considered minimal when used as a monotherapy [27].
Incretin Mimetic and Enhancer
The "incretin effect" is the difference in glucose-stimulated insulin secretion from an oral versus an intravenous glucose bolus, mediated through intestinal peptide hormones - glucagon like peptide-1 and glucose-dependent insulinotropic polypeptide [28]. Recent years have seen the advent of incretin mimetics, such as exenatide and liraglutide (in injections forms), and incretin enhancers, such as the gliptins, being used in the effort to intensify diabetes treatment. As their actions are glucose dependent, it is presumed that there is less or no hypoglycemic risk [27].
Alpha Glucosidase Inhibitors
This agent acts within the gut and impedes the action of enzymes that break down carbohydrates in the gut. The hypoglycemic risk is also considered low [27].
How Should the Individual Diabetic Worker Be Assessed?
History
The causes, symptoms, and signs of any hypoglycemic episode should always be sought at each physician visit. A recounting of an experience of disorientation and recovery without a recollection of what happened is a strong indication of hypoglycemic unawareness. The impact of this is potentially more profound than mild symptomatic hypoglycemia episodes that are rapidly and easily amenable to self-correction and which, for all intents and purposes, are less likely to result in harm.
Workers with a high A1C while undergoing intensive treatment may also experience hypoglycemic symptoms at the treated and lowered, but non-hypoglycemic, blood glucose levels. This is relative hypoglycemia, which though uncomfortable, is a benign and self-limiting condition, easily relieved by some feeding.
The corresponding action at work of whether the affected person should be removed from the job (Table 3 - red cells), and for how long, or whether some urgent remedial measures should be applied (remaining in the job, but with additional measures, such as intensifying supervision) should then be planned.
State of Glycemic Control
The state of glycemic control has to be examined. It is intuitive to worry less about hypoglycemic risk if the diabetic worker has glucose levels constantly in the poorly controlled hyperglycemic range, compared to one managed to optimal A1C targets. However, even then, one has to be alert to the vagaries of "averages". An A1C of 8% or more could also be accounted for by wide swings in glycemic variation.
The planned action in all cases should include counseling and expert medical advice to prevent, minimize, and manage hypoglycemia.
Self-Monitoring of Blood Glucose (SMBG)
Diabetic workers should always be encouraged to perform SMBG. Perhaps more important than the timing of these readings (e.g. fasting, post meal, pre-sleep, bedtime) is the ability of the worker concerned to weave a story around the particular reading, correlating it to the timing and nature of meals, his level of physical exertion, his medication, and his mental state. Doctors requesting SMBG from patients must help the patient make a meaningful interpretation of his reading.
How frequent these readings should be taken will depend on the personal glycemic circumstances and the safety sensitive content of the work involved. For instance, a diabetic worker who has embarked on increased physical activity (either at work or at leisure) or a change in dietary habits will need more SMBG in the interim. Adjustment in treatment may be necessary. Similarly, a driver embarking on a long driving trip will probably require SMBG to be done during his trip. The higher the implied extent of safety sensitivity in the job, the more readily one should recommend SMBG.
Blood Glucose Awareness Training (BGAT) [29]
Psycho-educational intervention training programs, such as BGAT, have been proven to be effective in reducing unfavorable events, notably driving mishaps among patients with diabetes. It is reasonable to infer that structured programs such as this can be applied for workers in safety sensitive jobs as well. An important component of this program is training the diabetic person to recognize his internal cues and to correlate this to his blood glucose levels.
Self-treatment
Self-treatment in hypoglycemic emergencies should be emphasized. When in doubt, stop whatever activity and treat. The recommendation is to check SMBG if possible, and to consume 15 gm of rapidly absorbable carbohydrates in the event of hypoglycemia. This is to be followed by a SMBG check after fifteen minutes to ensure that glucose levels are ascending and normalized. Additional carbohydrates or snacks may be needed if the next meal is more than an hour away [30].
Sweets should always be kept within reach of the diabetic worker for such emergencies. Trained colleagues can and should provide help spontaneously, especially if the worker is experiencing difficulties.
Should the Diabetic Worker Inform His Co-worker or Supervisor?
Medical information is sensitive. The reluctance to share this with others at work is understandable. Balanced against this is the benefit of receiving appropriate assistance from others in the event of diabetic emergencies, especially during hypoglycemia. Workers should be encouraged to reflect on this and to share knowledge of their medical condition with a close colleague or supervisor. The use of a medic alert bracelet or tag should be also considered.
The diabetic worker who refuses to cooperate with medical advice and whose hypoglycemic risk poses a threat at his workplace is hopefully a rarity. However, should such a situation arise, the public interest argument of breaching confidentiality and informing the relevant authorities at the workplace may supersede the privilege of medical confidentiality.
Case 1
Mr. X is a type2 DM, and he works as a handler for a courier service company. A bolus insulin has been added to his treatment pre-lunch in order to optimize control. His work duty is a mix of office work and operations work on fixed days of the week. On the operations days, he is required to lift and load up packages in the afternoons. He gives a history of discomfort - which he thinks is due to hypoglycemia on the afternoons of his operations days. In particular, he is able to recount a history of perspiration occurring around the lips, which is different from whole body perspiration due to heat.
The hypoglycemia can be easily confirmed by SMBG. Downward adjustment of his pre-lunch insulin would be one option. Rapid acting insulin analogues may be preferred over regular human short acting insulin. Another alternative, which may not be favored as a long-term solution, especially if weight gain is an issue, is to have a snack to relieve the hypoglycemia. The likelihood of severe potential consequences is moderate, but overall, there is probably no need to recommend an immediate removal from work duties.
Case 2
Mr. Y is a 29-year-old type1 DM on multiple doses of insulin a day. He has been trained and employed as a croupier in a casino for the past three years. He is well respected among his peers and management for his numeracy talent. There has been no problem with his work until recently for the past three months when he changed his diet, and started to reduce his intake of carbohydrates. There were two clinical episodes while at work, one when he experienced blurring of vision and another when he nearly 'blanked out' and had to be helped by a colleague to the medical center to seek treatment. His blood glucose level was 1.5 mmol/L.
Acute measures to correct this will have to be taken. Given the history, it must be assumed that Mr. Y has hypoglycemic unawareness. Allowing the glucose levels to rise and scrupulously avoiding further exposure to hypoglycemia can restore awareness by two to three weeks [12]. Obviously this time frame is one important consideration in the assessment of any return to work fitness assessment. The physician will also have to be guided by frequent blood glucose monitoring. A continuous glucose monitoring system is one useful tool in such cases. This makes use of a sensor inserted beneath the skin that captures blood glucose trend data, up to 288 readings over a 24-hour period, without the need for intermittent finger pricking for SMBG.
Medical advice would include carbohydrate counting as well as insulin adjustments to match carbohydrate intake. Medical and occupational health input is, of course, crucial to the company's employment decision with respect to the worker.
Work Affecting Diabetes: Support at the Workplace
Diabetic workers in the community are becoming increasingly common. A restrictive policy on employment may not be realistic or tenable. Losing in the competition for talent is one thing, but being labeled as biased is another. Whilst efforts at prevention must continue, society and employers must also be proactive in their support for such workers.
Very often, such support need not be elaborate. A provision of healthy food options at workplace canteens, flexible meal times, and arrangements for affected workers (permission to carry and consume emergency sweets or sugary drinks) are some such supports. Permission and privacy for SMBG when required is also a way employers can help such employees. The employer can also assist with facilities for storage of medications, such as insulin, and for safe disposal of used needles and other consumables. Management support for medical appointments and structured programs that improve self-help and education in diabetic care is also important.
Supportive employers are also less likely to have to deal with issues of concealment and unexpected consequences.
Take Home Messages
Workers with diabetes, especially when on treatment with insulins and/or insulin secretagogues are at risk for hypoglycemia. This can affect cognitive function.
Hypoglycemic unawareness can have dangerous consequences. This risk can be prevented and be reversed, if already present.
Causes should be identified and measures taken to mitigate the risk of hypoglycaemia.
Physicians with responsibility for diabetic workers should be alert to this risk. Risk assessment for fitness to work should be performed.
Support from employers to the needs of the diabetic worker is crucial in terms of management of his condition.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.The international diabetes federation [Internet] Brussels: International Diabetes Federation; 2010. [cited 2010 Nov 18]. Available from: http://www.idf.org/international-diabetesfederation. [Google Scholar]
- 2.Shaw JE, Sicree RA, Zimmet PZ. Global estimates of the prevalence of diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87:4–14. doi: 10.1016/j.diabres.2009.10.007. [DOI] [PubMed] [Google Scholar]
- 3.Global risks 2010 - A global risk network report [Internet] Geneva: World Economic Forum; 2010. [cited 2010 Nov 30]. Available from: http://www.preventionweb.net/files/12826_globalrisks2010.pdf. [Google Scholar]
- 4.Gaede PH, Jepsen PV, Larsen JN, Jensen GV, Parving HH, Pedersen OB. Multifactorial intervention and cardiovascular disease in patients with type 2 diabetes. N Engl J Med. 2003;348:383–393. doi: 10.1056/NEJMoa021778. [DOI] [PubMed] [Google Scholar]
- 5.The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329:977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 6.UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) Lancet. 1998;352:837–853. [PubMed] [Google Scholar]
- 7.American Diabetes Associaton. Standards of medical care in diabetes-2010. Diab Care. 2010;33(Suppl 1):S11–S61. doi: 10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cryer PE, Axelrod L, Grossman AB, Heller SR, Montori VM, Seaquist ER, Service FJ Endocrine Society. Evaluation and management of adult hypoglycemic disorders: an Endocrine Society Clinical Practice Guideline. J Clin Endocrinol Metab. 2009;94:709–728. doi: 10.1210/jc.2008-1410. [DOI] [PubMed] [Google Scholar]
- 9.Geddes J, Schopman JE, Zammitt NN, Frier BM. Prevalence of impaired awareness of hypoglycaemia in adults with Type 1 diabetes. Diabet Med. 2008;25:501–504. doi: 10.1111/j.1464-5491.2008.02413.x. [DOI] [PubMed] [Google Scholar]
- 10.Schopman JE, Geddes J, Frier BM. Prevalence of impaired awareness of hypoglycaemia and frequency of hypoglycaemia in insulin-treated type 2 diabetes. Diabetes Res Clin Pract. 2010;87:64–68. doi: 10.1016/j.diabres.2009.10.013. [DOI] [PubMed] [Google Scholar]
- 11.Briscoe VJ, Davis SN. Hypoglycemia in type 1 and type 2 diabetes: physiology, pathophysiology, and management. Clinical Diabetes. 2006;24:115–121. [Google Scholar]
- 12.Cryer PE. Diverse causes of hypoglycemia-associated autonomic failure in diabetes. N Engl J Med. 2004;350:2272–2279. doi: 10.1056/NEJMra031354. [DOI] [PubMed] [Google Scholar]
- 13.Holmes CS, Koepke KM, Thompson RG. Simple versus complex performance impairments at three blood glucose levels. Psychoneuroendocrinology. 1986;11:353–357. doi: 10.1016/0306-4530(86)90021-1. [DOI] [PubMed] [Google Scholar]
- 14.Holmes CS, Hayford JT, Gonzalez JL, Weydert JA. A survey of cognitive functioning at difference glucose levels in diabetic persons. Diabetes Care. 1983;6:180–185. doi: 10.2337/diacare.6.2.180. [DOI] [PubMed] [Google Scholar]
- 15.Zammitt NN, Warren RE, Deary IJ, Frier BM. Delayed recovery of cognitive function following hypoglycemia in adults with type 1 diabetes: effect of impaired awareness of hypoglycemia. Diabetes. 2008;57:732–736. doi: 10.2337/db07-0695. [DOI] [PubMed] [Google Scholar]
- 16.Martin S. Determing Fitness to work at safety sensitive jobs. BCMJ. 2010;52:48. [Google Scholar]
- 17.Esso Petroleum Canada and C.E.P. Local 614 [1994] 56 L.A.C. (4th) 440 and supported in Entrop v. Imperial Oil Ltd.; 2000. O.J. No. 2689. [Google Scholar]
- 18.Part III - medical assessment October 2008 [Internet] Montreal: ICAO Documents; 2008. [cited 2010 Nov 11]. Manual of civil aviation. Available from: http://www.icao.int/icaonet/dcs/8984/index.html. [Google Scholar]
- 19.Norwegian guidelines for medical examination of occupational divers [Internet] Oslo: Statens Helsetilsyn; 2000. [cited 2010 Nov 16]. Available from: http://www.helsetilsynet.no/upload/Publikasjoner/veiledningsserien/guideline_examination_divers_ik-2708.pdf. [Google Scholar]
- 20.At a glance guide to the current medical standards of fitness to drive [Internet] Swansea: Drivers Medical Group, DVLA; 2010. [cited 2010 Nov 16]. Available from: http://www.dft.gov.uk/dvla/medical/ataglance.aspx. [Google Scholar]
- 21.NFPA 1582 - Standard on comprehensive occupational medical program for fire departments [Internet] Quincy: NFPA; 2007. [cited 2010 Nov 16]. Available from: http://www.diabetes.org/assets/pdfs/know-your-rights/for-lawyers/nfpa-1582-diabetes-standard.pdf. [Google Scholar]
- 22.Workgroup on Hypoglycemia, American Diabetes Association. Defining and reporting hypoglycemia in diabetes: a report from the American Diabetes Association Workgroup on Hypoglycemia. Diabetes Care. 2005;28:1245–1249. doi: 10.2337/diacare.28.5.1245. [DOI] [PubMed] [Google Scholar]
- 23.Wright AD, Cull CA, Macleod KM, Holman RR for the UKPDS Group. Hypoglycemia in Type 2 diabetic patients randomized to and maintained on monotherapy with diet, sulfonylurea, metformin, or insulin for 6 years from diagnosis: UKPDS73. J Diabetes Complications. 2006;20:395–401. doi: 10.1016/j.jdiacomp.2005.08.010. [DOI] [PubMed] [Google Scholar]
- 24.Edelman SV, Morello CM. Strategies for insulin therapy in type 2 diabetes. South Med J. 2005;98:363–371. doi: 10.1097/01.SMJ.0000149424.50849.00. [DOI] [PubMed] [Google Scholar]
- 25.Porcellati F, Rossetti P, Busciantella NR, Marzotti S, Lucidi P, Luzio S, Owens DR, Bolli GB, Fanelli CG. Comparison of pharmacokinetics and dynamics of the long-acting insulin analogs glargine and detemir at steady state in type 1 diabetes: a double-blind, randomized, crossover study. Diabetes Care. 2007;30:2447–2452. doi: 10.2337/dc07-0002. [DOI] [PubMed] [Google Scholar]
- 26.Dornhorst A, Lüdeke HJ, Koenen C, Meriläinen M, King A, Robinson A, Sreenan S PREDICTIVE Study Group. Transferring to insulin detemir from NPH insulin or insulin glargine in type 2 diabetes patients on basal-only therapy with oral antidiabetic drugs improves glycaemic control and reduces weight gain and risk of hypoglycaemia: 14-week follow-up data from PREDICTIVE. Diabetes Obes Metab. 2008;10:75–81. doi: 10.1111/j.1463-1326.2007.00816.x. [DOI] [PubMed] [Google Scholar]
- 27.Hypoglycemia during therapy of diabetes [Internet] Diabetes Manager; 2009. [cited 2010 Nov 9]. Available from: http://diabetesmanager.pbworks.com/w/page/17680209/Hypoglycemia-During-Therapy-of-Diabetes- [Google Scholar]
- 28.McIntyre N, Holdsworth CD, Turner DS. New interpretation of oral glucose tolerance. Lancet. 1964;2:20–21. doi: 10.1016/s0140-6736(64)90011-x. [DOI] [PubMed] [Google Scholar]
- 29.Cox DJ, Gonder-Frederick L, Polonsky W, Schlundt D, Kovatchev B, Clarke W. Blood glucose awareness training (BGAT-2): long-term benefits. Diabetes Care. 2001;24:637–642. doi: 10.2337/diacare.24.4.637. [DOI] [PubMed] [Google Scholar]
- 30.How to treat a low blood glucose [Internet] Boston: Joslin Diabetes Center; 2010. [cited 2010 Nov 30]. Available from: http://www.joslin.org/info/how_to_treat_a_low_blood_glucose.html. [Google Scholar]