Abstract
Objectives
Seven cases of malignant lymphohematopoietic (LHP) disorder were claimed to have developed from occupational exposure at two plants of a semiconductor company from 2007 to 2010. This study evaluated the possibility of exposure to carcinogenic agents for the cases.
Methods
Clinical courses were reviewed with assessing possible exposure to carcinogenic agents related to LHP cancers. Chemicals used at six major semiconductor companies in Korea were reviewed. Airborne monitoring for chemicals, including benzene, was conducted and the ionizing radiation dose was measured from 2008 to 2010.
Results
The latency of seven cases (five leukemiae, a Non-Hodgkin's lymphoma, and an aplastic anemia) ranged from 16 months to 15 years and 5 months. Most chemical measurements were at levels of less than 10% of the Korean Occupational Exposure Limit value. No carcinogens related to LHP cancers were used or detected. Complete-shielded radiation-generating devices were used, but the ionizing radiation doses were 0.20-0.22 uSv/hr (background level: 0.21 µSv/hr). Airborne benzene was detected at 0.31 ppb when the detection limit was lowered as low as possible. Ethylene oxide and formaldehyde were not found in the cases' processes, while these two were determined to be among the 263 chemicals in the list that was used at the six semiconductor companies at levels lower than 0.1%. Exposures occurring before 2002 could not be assessed because of the lack of information.
Conclusion
Considering the possibility of exposure to carcinogenic agents, we could not find any convincing evidence for occupational exposure in all investigated cases. However, further study is needed because the semiconductor industry is a newly developing one.
Keywords: Semiconductors, Leukemia, Lymphoma, Epidemiologic studies, Korea
Introduction
There have been several reports of cancer outbreaks in semiconductor companies, such as IBM in the United States [1,2] and the National Semiconductor UK (NSUK) in the United Kingdom [3,4]. Recently, the Health and Safety Executive (HSE) of the UK announced that there was no evidence linking working at NSUK and cancer development [5]. However, there is still some debate on this matter [6].
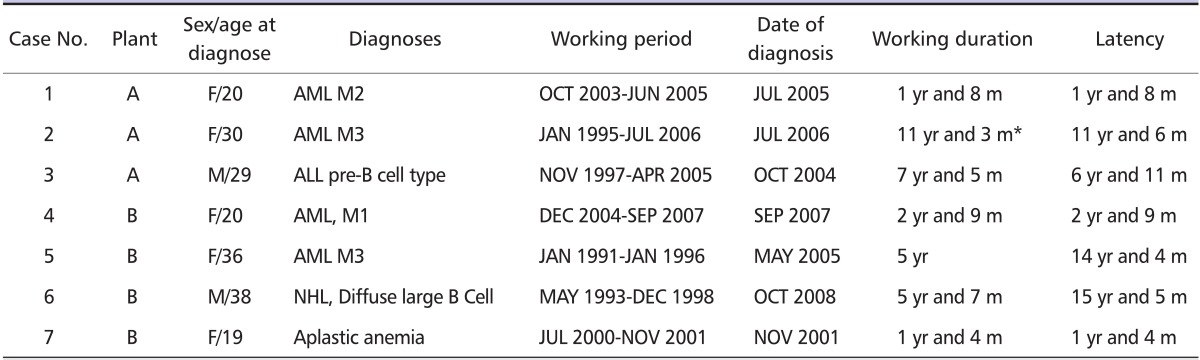
From 2007 to 2010, the Occupational Safety and Health Research Institute (OSHRI) of the Korea Occupational Safety and Health Agency (KOSHA) investigated seven cases of malignant lymphohematopoietic (LHP) disorders, such as leukemia, malignant lymphoma, and aplastic anemia, in a semiconductor company (Table 1) to evaluate work-relatedness, as requested by the Korea Workers' Compensation & Welfare Service (COMWEL). OSHRI conducted an environmental assessment to find occupational carcinogens related with malignant LHP disorder, focusing on benzene and ionizing radiation in the victims' workplaces. OSHRI also reviewed the seven patients' medical records.
Table 1.
Latency and working period of the cases
AML: acute myeloid leukemia, ALL: acute lymphoblstic leukemia, NHL: non-Hodgkin's lymphoma, yr: year, m: month.
*Except 3 months for the leave for child delivery.
In 2008, OSHRI also conducted a retrospective cohort study in eight semiconductor factories to assess the mortality and incidence for LHP cancers of Korean semiconductor workers. The results of this cohort showed no significant increase of leukemia. The standardized incidence ratio (SIR) of leukemia was 0.69 [95% confidence interval (CI): 0.30-1.37] in males and 1.28 (95% CI: 0.61-2.36, 10 cases) in females. However, non-Hodgkin's lymphoma (NHL) in females was significantly increased (2.31, 95% CI: 1.23-3.95) even though there was no definite association between work and those diseases in subgroup analysis according to work duration. The detailed result of this cohort study will be presented in another paper [7]. In the cohort study paper, the specific working environment and clinical course of the cases are not described. The purpose of this study is to provide details on the clinical course and the job exposures experienced by the seven LHP cases.
Materials and Methods
From July 2007 to October 2010, OSHRI investigated seven cases of malignant LHP disorder from two plants of a semiconductor company in Korea. Three of the subjects had worked in the wafer fabrication (FAB) department in Plant A, and the others were from the assembly (AS) departments in Plant B, which was located in a different city. Personal characteristics and the clinical course, the manufacturing process of the plants, and the specific working environment and tasks of the cases were reviewed.
Results
Clinical characteristics and latency
The following cases were reviewed: four females with acute myeloid leukemia (AML) and a male with acute lymphoblastic leukemia (ALL, pre-B cell type), all 20-30 years old; a 38 year-old male with NHL; and a 19 year-old female with aplastic anemia. Their working periods ranged from 1991 to 2007. The aplastic anemia case developed with the shortest latency (1 year and 4 months) of exposure. The longest latency was observed in the NHL case (15 years and 5 months) (Table 1). Two cases (Case No. 5 and 6) had been diagnosed 9-10 years after leaving the company.
All cases were non-smokers and all female workers had never drunk alcohol. The two male workers had drunk small amounts of alcohol (about 6-12 ml for each worker) twice a month. No cases had a history of habitual drug use. All the cases answered that none of their immediate family had been diagnosed with hematologic cancer or a related disorder.
Case No. 1
A 20-year-old (at the age of diagnosis) female worker began working at a semiconductor company in October 2003 immediately after she graduated high school. In 2004, she had a regular medical checkup, with normal findings for red blood cell counts (RBC), hemoglobin (Hb), hematocrit (HCT), and white blood cell counts (WBC). In May 2005, she visited a hospital due to various symptoms, such as bruising, vomiting, fatigue, and dizziness. She was subsequently diagnosed with leukemia in June 2005, which was classified as AML with granulocytic maturation (M2) by the French-American-British classification system. She received bone marrow transplantation in December 2005; in November 2006, her clinical status aggravated and she died in March 2007 during re-remission treatment.
Case No. 2
A 30-year-old (at the age of diagnosis) female worker began working in the semiconductor industry in January 1995. She visited outpatient clinics several times due to respiratory (acute and chronic laryngitis, allergic rhinitis, and chronic sinusitis) and dermatologic (xerodermia and allergic contact dermatitis) problems, and a miscarriage during 1998 to 2006. From 2003 to 2005, the annual medical examination revealed that her RBC, WBC, and HCT were normal except for a mild decrease in Hb. In 2005, she became pregnant and gave a birth in April 2006. She returned back to the work in June 2006. One month later after she returned to work, she visited a clinic due to productive cough and gum bleeding, prompting a hospital visit in July 2006. She was then diagnosed with promyelocyte dominant AML (M3, variant type by the FAB classification system) without abnormal chromosomal finding. She started remission chemotherapy right after diagnosis, but died in October 2006.
Case No. 3
A 29-year-old (at the age of diagnosis) male worker began working in the semiconductor industry in November 1997. He had previously worked for two years in porcelain panel and clothes manufacturing companies where he packed cloths. Results of the periodic medical checkups were normal during 2001 to 2004. His only previous health problem was contact dermatitis around the mouth due to wearing a mask at work. He was diagnosed with ALL (pre-B cell type) in October 2004. Before diagnosis, he had experienced a common cold, blood-tinged sputum, and epistaxis for 3 weeks. After repeated remission and aggravation, he died in July 2007.
Case No. 4
A 20-year-old (at the age of diagnosis) female worker began working in the semiconductor industry in December 2004. Routine blood tests in the pre-placement medical examination before entering the company and regular medical checkups in 2005 and 2006 were normal. In May 2007, blood test results showed mild leukopenia (WBC count 3,180/mm3, Hb 10.2 g/dL, and RBC count 321 × 104/mm3). She began to experience dyspnea, nausea, vomiting, and dizziness in August 2007, she visited a hospital in September 2007, and was then diagnosed with AML (M1, myeloblastic leukemia without maturation). The chromosomal study revealed deletion of 11q23 in September 2007, but was normal in repeated analysis in October 2007. She received bone marrow transplantation in April 2008, but her condition aggravated the following month. She died in March 2010 after repeated chemotherapy.
Case No. 5
A 36-year-old (at the age of diagnosis) female worker began working in the semiconductor industry in January 1991 and quit in January 1996. In 2003, seven years after leaving the company, she felt severe fatigue and bruised frequently (no medical record existed before 2003, but she denied any health problems before then). She visited an outpatient clinic and was found to have mild leucopenia. She received a treatment for acute pyelonephritis in 2003 and 2004, and leucopenia was also found. In January 2005, she visited a hospital emergency room for high fever and pharyngitis and was found to have pancytopenia. After detailed tests, she was diagnosed with AML (M3) in May 2005. She started chemotherapy in March 2005 and was still undergoing treatment as of December 2010.
Case No. 6
A 38-year-old (at the age of diagnosis) male worker with no remarkable past medical history began working in the semiconductor industry in May 1993 and left the company in December 1998 when he began working in real estate. Ten years later (October 2008), he felt an abnormal lump in his neck and enlargement of a lymphatic gland. He visited a hospital immediately and was diagnosed with non-Hodgkin's lymphoma of the diffuse large B cell type. His health checkup records during employment at Plant B could not be reviewed because these records are retained for only 3 years after employment termination, whereas this worker ceased employment at Plant B 10 years before his lymphoma diagnosis. He is still being treated as of December 2010.
Case No. 7
A 19-year-old (at the age of diagnosis) female worker began working in the semiconductor industry in July 2000. Routine blood tests in the periodic medical checkup found mild anemia (Hb 11.8 g/dL) in March 2001, and 8 months later (November 2001) she visited a hospital due to subconjunctival hemorrhage, epistaxis, and vitreous hemorrhage. Bone marrow pathology revealed less than 5% cellularity and she was diagnosed with aplastic anemia. After the diagnosis was confirmed, she started chemotherapy; however, it did not work because of repeated fever and her respiratory symptoms relapsed. She is currently waiting for bone marrow transplantation as of July 2010.
Overview of Semiconductor manufacturing process
The semiconductor manufacturing process consists of the following three steps: production of silicon wafers from very pure silicon ingots; fabrication of integrated circuits onto these wafers (FAB); assembly of every integrated circuit on the wafer into a finished product (AS) and testing of the finished products. The first step is purifying the silicon to make the raw material for a chip. The chip is a semiconductor product through which ingot bare wafers are produced. The bare wafers, then, are transferred to the second step, where various chemicals are used to create circuits by adding and removing layers on the wafer. FAB processes are followed by assembly, testing, marking, packing, and shipping [8].
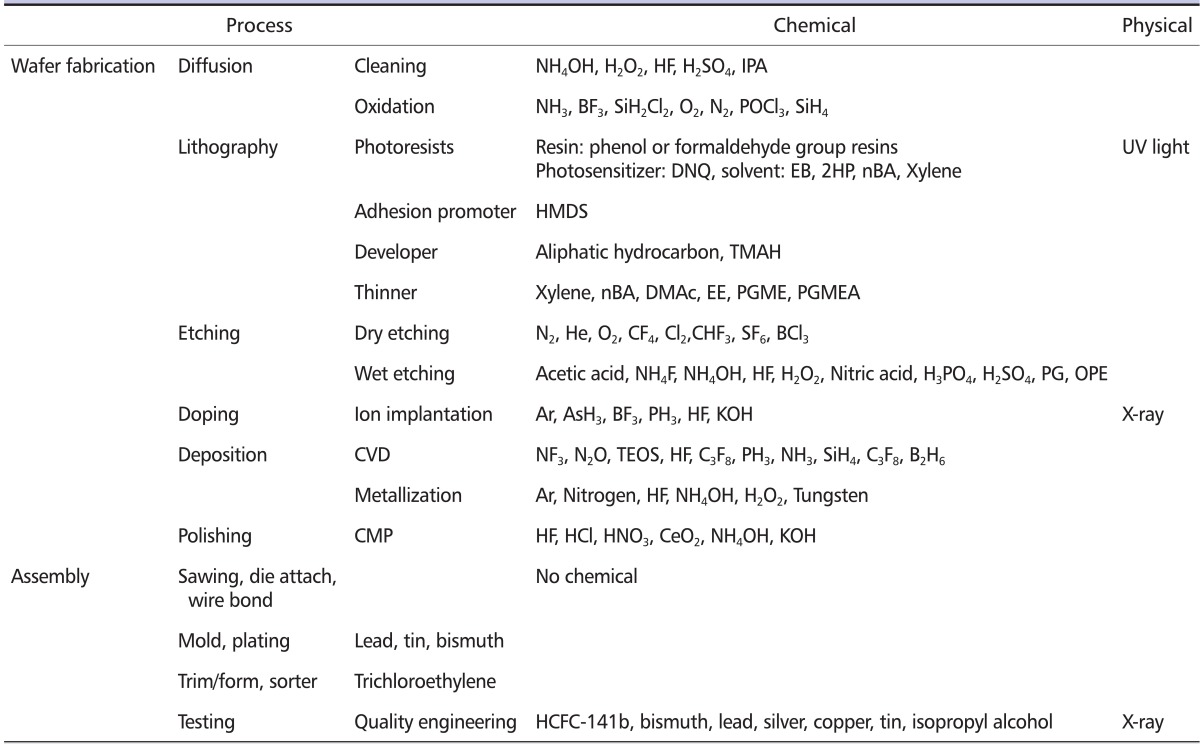
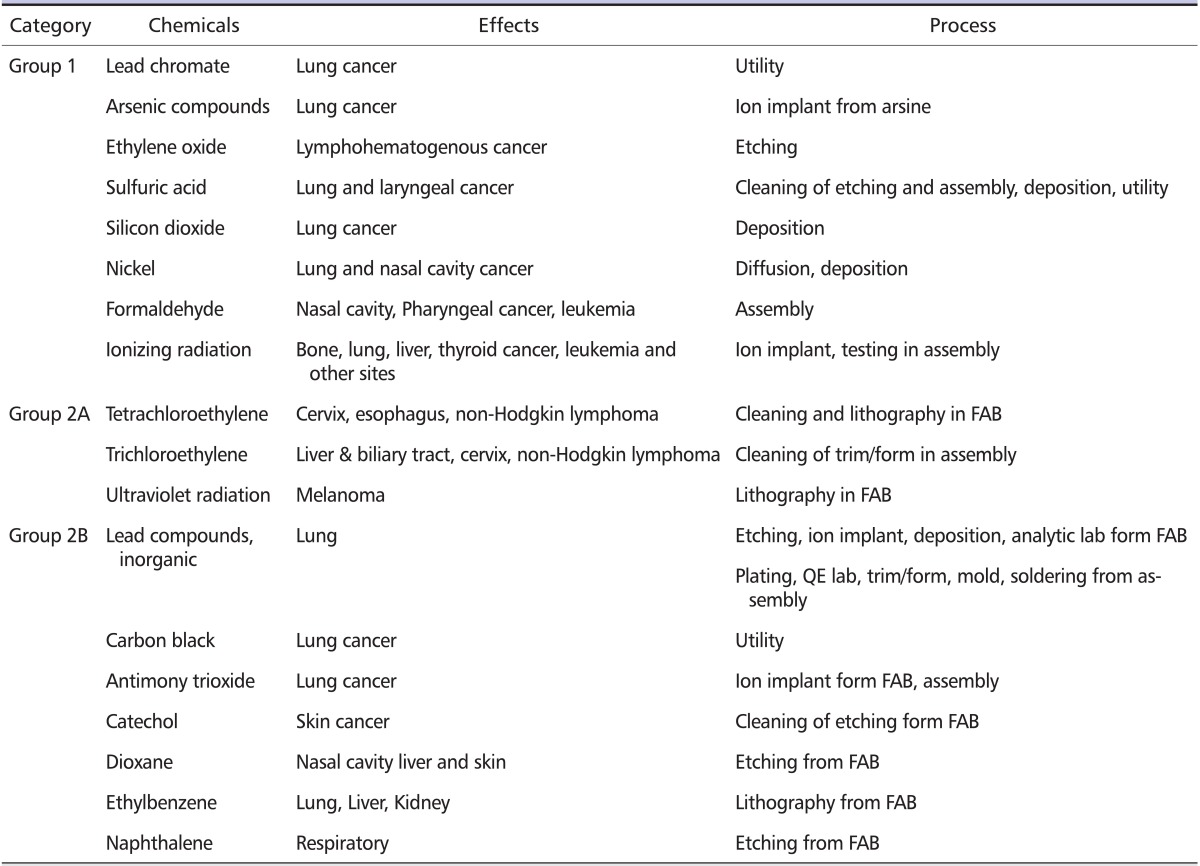
Major chemical and physical hazards in the semiconductor processes are shown in Table 2. There are several major process stages in FAB, such as diffusion, lithography, etching, ion implantation, deposition process, and polishing. In the diffusion process, silicon dioxide (SiO2) is formed on a wafer using several gases. Before the oxidation, wafers should be cleaned thoroughly to remove particulates by using various kinds of acids and bases and isopropyl alcohol (IPA). Several different layers, each with a different pattern and all of which are required for circuits, are well defined by a process called lithography. Lithography uses a variety of solvent-based photoresists, developers, thinners, adhesion, and promoters. UV-light is used for exposure, from which secondary reactants can be generated. Etching removes deposited material on the wafer's surface that is not covered by photoresists. Etching can be accomplished by a 'wet' processing using various acids and bases or a 'dry' processing using gaseous species. In the ion implantation process, ion additives are shot into the wafer, creating the positively and negatively charged regions on the wafer. Arsine (AsH3), boron trifluoride (BF3), and phosphine (PH3) are the most common chemicals used in this process. Because ion additives are infused by an ion acceleration instrument, there might be a possible risk of ionizing radiation exposure. Deposition refers to the deposition of additional material on the wafer surface and is composed of chemical vapor deposition (CVD) and metallization. CVD uses diboran (B2H6), nitrogen trifluoride (NF3), nitrous oxide (N2O), silane (SiH4), and tetraethyl orthosilicate (TEOS). The most commonly used metals are aluminum, gold, nickel-chromium, and platinum, with copper being a recent addition. Polishing refers to planarization of the oxide layer of the wafer by chemical and physical means. A polishing fluid called slurry and several acids and bases are used. The third step involves putting the integrated circuit inside a package for shipping, and this process is known as semiconductor package assembly (AS). In general, AS consists of sawing off the wafer, attaching it to a support structure, bonding the wire, molding and plating, 'trim and form' and electrical testing. Most AS processes do not use chemicals. However, the molding and plating process may use resins or metals. Although the trim and form process does not use chemicals, solvents such as isopropyl alcohol are used for cleaning. During electrical testing, an X-ray-generating instrument and various chemicals, such as isopropyl alcohol or 1,1-dichloro-1-fluoroethane, are used. After a lot is tested, it is taped and labeled for shipment.
Table 2.
Chemical and physical hazards of major semiconductor processes
CVD: chemical vapor deposition, CMP: chemical mechanical polishing, NH3: ammonia, BF3: borontrifluoride, SiH2Cl2: dichlorosilane, O2: Oxygen, N2: Nitrogen , POCl3: phosphorus oxychloride, SiH4: silane, DNQ: diazonaphthoquinone, NH4OH: ammonium hydroxide, H2O2: hydrogen peroxide, HF: hydrofluoric acid, H2SO4: sulfuric acid, IPA: isopropyl alcohol, HMDS: hexamethyldisilazane, PGME: propylene glycol mono methyl ether, PGMEA: propylene glycol mono methyl ether acetate, DMAc: dimethylacetamide, EE: ethyl-3-ethyoxypropionate, EB: ethyl benzene, 2HP: 2-hepatinone, nBA: n-buthyl acetate, TMHA: tetramethyl ammonium hydroxide, He: helium, CF4: carbon tetrafluoride, Cl2: chlorine, CHF3: trifluoro methane, SF6: sulfur hexafluoride, BCl3: boron trichloride, NH4F: ammonium fluoride, H3PO4: phosphoric acid, PG: polyethylene glycol, OPE: octylphenoxy-polyethylene ethanol, Ar: argon, AsH3: arsine, PH3: phosphine, KOH: potassium hydroxide, NF3: nitrogen trifluoride, N2O: nitrous oxide, TEOS: tetraethyl orthosilicate, SiH4: Silane, C3F8: Octafluoropropane, B2H6: diborane, HCFC-141b: 1,1-Dichloro-1-fluoroethane, HCl: hydrogen chloride, HNO3: nitric acid, CeO2: cerium oxide.
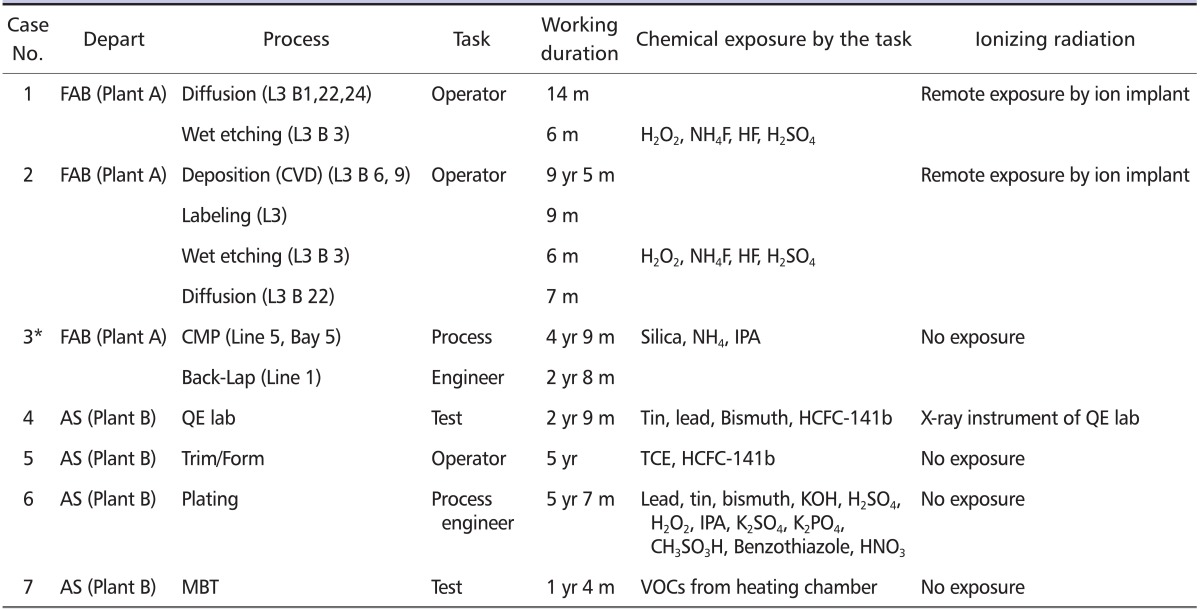
Specific working environment and tasks
Three of the investigated cases (two operators and an engineer) were from FAB in Plant A; the other four cases were from AS in Plant B. Plant A, founded in 1969, had approximately 24,000 workers in 2008 and produced dynamic random access memory (DRAM), static random access memory (SRAM), and flash memory. Plant B, founded in 1991, had approximately 6,000 workers in 2008 and produced DRAM, SRAM, and liquid crystal display (LCD) modules. All clean room workers (AS or FAB workers) should wear a protective suit known as a 'bunny suit' which is composed of all-in-one clothing, including a mask, safety glasses, gloves, and boots. However, this suit is not chemically-resistant, and chemicals can soak through to the skin.
FAB department cases in Plant A
Two female operators (Case No. 1 and 2) and one male engineer (Case No. 3) had worked in Plant A. Plant A operated 15 production lines, with each of them occupying one or two floors of the plant. Each line had 80-150 workers and some of the lines were located in separate buildings. The dimensions of each line were approximately 100 m length × 54 m width × 3 m height and they were composed of more than 25 bays. Each bay occupied an area of 3 m length × 25 m width × 3 m height. Case No. 1 and 2 had worked on the same line (line 3), and the other (Case No. 3) worked on different lines (1 and 5).
Case No. 1 worked in the diffusion process - in bays 1, 22, and 24 of line 3 - for 14 months since October 2003. Her duty was loading and unloading the wafer carrier to the diffusion instruments. All instruments were automated and the process was closed. She then moved to the cleaning part of the wet etching process in bay 3 of line 3. She worked there for 6 months while her leukemia was developing. She manually dipped wafer boxes into a cleaning bath containing hydrogen peroxide and buffered oxide etchant (BOE) solution (mixture of ammonium fluoride, hydrofluoric acid and surfactant) (Table 3).
Table 3.
Working process and task of the cases
FAB: fabrication, AS: assembly, L: line, B: bay, CVD: chemical vapor deposition, CMP: chemical mechanical polishing, QE: quality engineering, MBT: monitoring burn-In test, m: month, yr: year, VOC: volatile organic compounds, H2O2: hydrogen peroxide, NH4F: ammonium fluoride, HF: hydrofluoric acid, H2SO4: sulfuric acid, NH4: ammonium, HCFC-141b: 1,1-Dichloro-1-fluoroethane, TCE: trichloroethylene, KOH: potassium hydroxide, H2SO4: sulfuric acid, H2O2: hydrogen peroxide, IPA: isopropyl alcohol, K2SO4: potassium sulfate, K2PO4: potassium phosphate, CH3SO3H: methane sulfuric acid, HNO3: nitric acid.
*There is anecdotal evidence that case No. 3 may have worked in PM and could have been exposed to TCE and other chemical exposures.
Case No. 2 worked in the deposition process (especially CVD), which was in bays 6 and 9 of line 3, since January 1995 for 9 years and 5 months. In this process, her duty was loading and unloading the wafer carrier to the Sputter procedure (Table 3). All instruments were automated and the process was closed. She then worked in the labeling part of line 3 for 9 months. Next, she worked in wet etching, the same location as Case No. 1 (bay 3 of line 3) for 5 months and diffusing (bay 22 of line 3) for 7 months. After that, she took a 3-month maternity leave. She came back to wet etching after delivery and worked for 1 month until her leukemia was diagnosed. Her duties in diffusion and wet etching were the same as those of Case No. 1. Although diffusion and deposition were automated and closed systems, she may have been exposed to other chemicals, especially when equipment was opened for loading and unloading.
Case No. 3, a male FAB engineer, started his work in the chemical mechanical polishing (CMP) process in bay 5 of line 5 for 4 years and 9 months on November 1997 (Table 3). He maintained instruments in FAB processes for 6 hours a day and did paper work for the remaining 2 hours of his shift. The main chemicals used for maintenance were ammonia and IPA. He changed slurry (composed of silica and ammonia), which was a polishing material used in the CMP process. In 2002, he was involved in setting up a new process line. According to his family, he sometimes participated in cleaning facilities, known as process maintenance (PM) tasks when mechanical errors occurred, using several acids and solvents. However, a company manager denied this because all PM tasks had been outsourced to contractor engineers since 1995. Then he moved to the back-lap part, which was in line 1, and worked there until March 2005. The back-lap procedure involves grinding the wafer. His task was the same as the previous procedure. His family claimed that accidental high exposure to various chemicals occurred during passing through vessels of instruments during maintenance in the basement floor of the FAB process. However, the employer asserted that there was no accident. We interviewed coworkers who had worked with case 3. The coworkers agreed that the working environment and personal protective equipment were worse than the present equipment, and they used to use small amounts of trichloroethylene (TCE), which was unusual. Therefore, it seemed that if he had performed the PM task, he might have been exposed to remnants of various chemicals in the baths and tanks.
In summary, based on available company records, the main chemical exposure was contents of the BOE solution or hydrogen peroxide during manual dipping in the cleaning part of the wet etching process for Case No. 1 and 2, and silica, ammonia, and IPA for Case No. 3. Possible exposure to various secondary products generated from chemical reactions among UV-light, strong acids and bases, and several other chemicals may have also occurred. Because the FAB process was conducted in a closed system, called the CLEAN ROOM, the air was re-circulated in the whole line, which meant that all processes in the line might have similar exposure levels to certain chemicals generated from the instruments in the line. Another possible exposure was ionizing radiation, which was generated from an ion accelerating device during the ion implant process. The ion-accelerating device in this company was of a completely shielded type, which does not require permission to use. Devices generating radiation of less than 10 uSv/hr can be used just after reporting to a relevant agency, according to the notice of the Korean Ministry of Education, Science and Technology. The devices were located at both ends of the line 3 floor, which was more than 10 m from the bay where Case No. 1 and 2 worked. Because operators might pass through the aisle near the ion implanter while moving products, Case No. 1 and 2 might have been exposed to radiation from them. Because the CMP process where Case No. 3 had worked was separated from the ionizing radiation generating facilities, there was no possibility of exposure to ionizing radiation.
AS department cases in Plant B
Case No. 4 and 7 were female workers who had worked in the testing part of Plant B, where the electrical testing process is conducted. Case No. 4 started her duties in the FRONT procedure where wafers were ground and sliced, and the wire was bonded. She tested tensile strength and performed microscopic inspections. After 10 months, she was also involved in other procedures, such as quality control of MOLD, TIN and Trim/Form, PVI (package visual inspection), and TEST. In the MOLD and TIN procedures, she operated X-ray-generating devices, an ultrasound instrument, and a laser measurement tool. She handled three X-ray-generating instruments (50 kVp/1.5 mA - 100 kVp, 0.1 mA).
In the TIN procedure, she tested the reliability of the plating state using 1,1-dichloro-1-fluoroethane (HCFC-141b) and a solder bar (composed of tin, bismuth, and lead). The plating reliability test was conducted in a local vacuum system. The PVI task involved visual inspection of package exteriors, while TEST was the final visual inspection of the product. Case No. 7 worked in the Monitoring Burn-In Test (MBT) procedure for 16 months, where chips were subjected to various voltages and temperatures to determine their long-term quality and reliability, and to eliminate weak chips. The procedure involved insertion and removal of the chip to the sorter and test board and then heating it in a chamber to 125 degrees Celsius. She loaded and unloaded chips to the sorter, monitored them on a computer screen, and visually inspected the products.
Case No. 5 worked in the TRIM/FORM procedure for 5 years from 1991 to 1996. In Trim & Form, lead frames were loaded into trim-and-form machines where lead fingers were formed step-by-step until finally the chips were severed from the frames. She loaded and unloaded products to the instrument, operated machinery, and moved products. Sometimes, she did visual inspections of products and cleaned molds with an air gun. Until 1995, TCE was used as a solvent to remove dusts from products. Thus, Case No. 5 could have been exposed to TCE during this period. Nine years after leaving the company, she was diagnosed with leukemia.
Case No. 6, a male engineer in the AS plant, worked in the plating procedure for 5 years and 7 months. In the plating procedure, tasks of the engineer included maintenance of the facility and exchanging machine parts. He also cleaned and prepared the facility, called "Make-Up", which involved the use of water and putting plating chemicals in baths or tanks. These duties were conducted manually until 2000. During this process, he might have been exposed to several chemicals used for plating (Table 3). Ten years after leaving the company, he was diagnosed with non-Hodgkin's lymphoma.
In summary, based on available company records, the main exposures of the test worker (Case No. 4) were HCFC-141b, metals such as tin, bismuth, and lead, and ionizing radiation. This is in contrast to the other test worker (Case No. 7) who might not have been exposed to chemicals. However, Case No. 7 might have been exposed to volatile organic chemicals (VOCs) during heating because products in the test procedure had undergone several chemical treatments, which could generate VOCs during the heating procedure. Case No. 5 also did not use many chemicals except for TCE, and Case No. 6 could have been exposed to various acids and bases with metals used in plating.
Measurement of carcinogenic factors
Among the agents listed as being used by the seven cases (Table 3), the only confirmed risk factor for LHP cancer was ionizing radiation. Ionizing radiation was measured using an ion chamber for Case No. 1 and 2 who had possibly been exposed to ionizing radiation indirectly, if any, and Case No. 4 who had handled X-ray-generating devices. The measuring points for Case No. 1 and 2 were located alongside their routine pathways during work because they were not operators for ion implants. Measuring points for Case No. 4 were placed in the X-ray room. The Korean Occupational Exposure Limit of ionizing radiation is 50 mSv/year.
For Case No. 1 and 2, the dose levels of 8 of the 9 points were 0.20-0.22 uSv/hr, which were similar with the background level (0.21 µSv/hr) measured in the rest room of the same floor. One point was 2.4 uSv/hr. All five points measured for Case 4 were 0.54-0.58 nC/hr, which were lower than the background level (0.59 nC/hr) measured in the workers' rest room of the same flour.
Although carcinogenic chemicals related to LHP were not used in all seven cases' processes, considering the possibility of generation from chemical reactions among the several agents used, airborne monitoring was conducted from June 2007 to May 2010, focusing on carcinogens related to LHP, such as benzene, and chemicals having hematologic effects. Benzene was measured for all processes, in which the seven cases were involved, and arsine, cellosolve, and ethylene glycols were measured for FAB workers. All the results of benzene, arsine, cellosolve, and ethylene glycols were lower than the minimum detection levels (3 ppb, 0.02 ppb, and 0.02 ppb, respectively). The detailed methods and results of these measurements for Case No. 1 and 2 in the FAB department conducted in 2008 were described in another paper [9]. In 2009, a following study was conducted to detect air benzene levels in three major FAB semiconductor companies, including the company where the cases occurred. The maximum concentration of benzene detected was 0.31 ppb (minimum detection level: 0.1 ppb) [10].
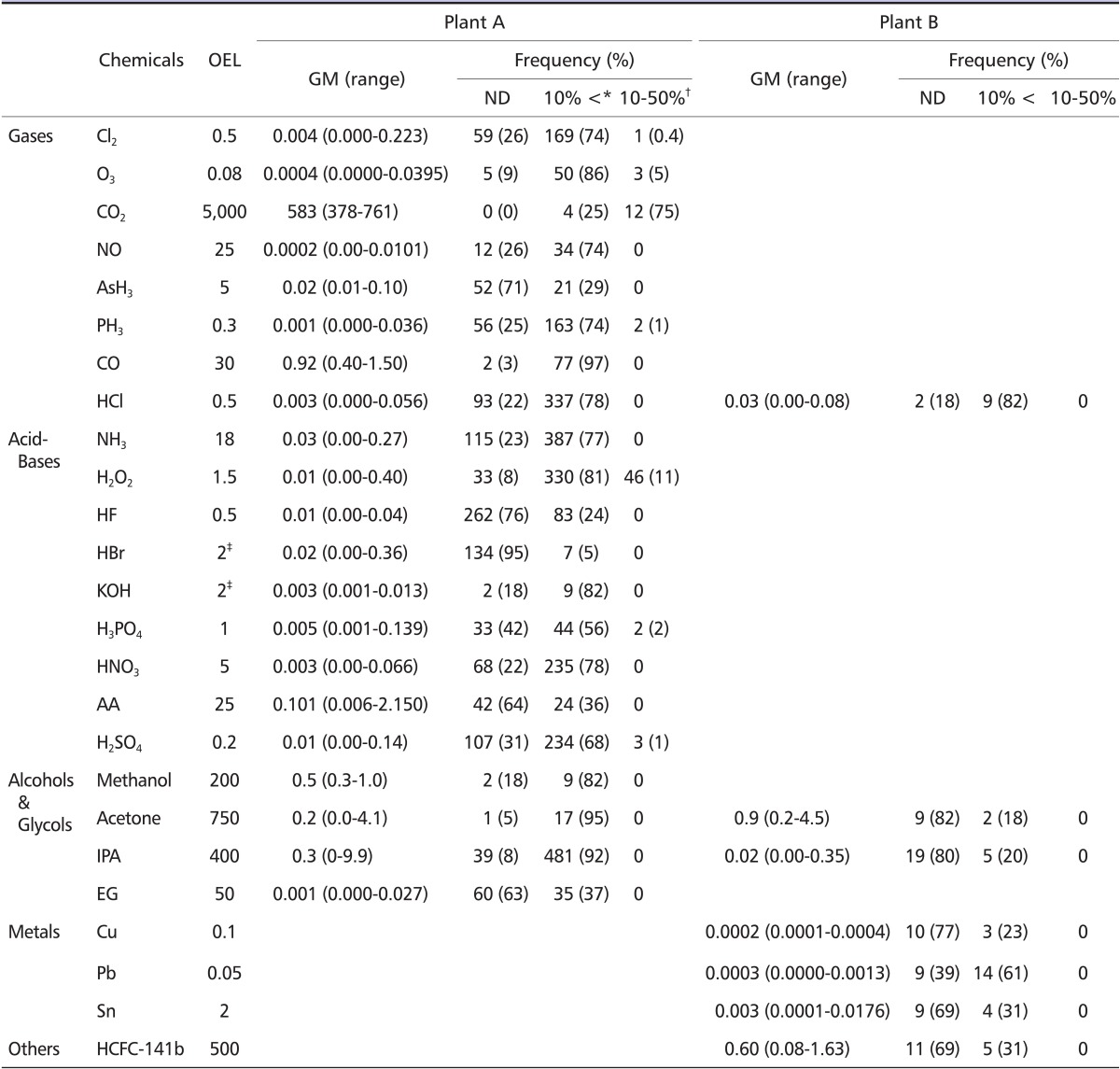
There were other records regarding chemical exposure in the company. By the Enforcement Regulation of the Occupational Safety and Health Act [11], employers should perform airborne measurements for 190 chemicals and physical agents at worksites. The major results of airborne measurement for the seven cases' processes from 2002 to 2007 are summarized in table 4. There were eight gases, three metals, nine acid-bases, four alcohols, eight glycols, and a chlorofluorocarbon compound measured at the worksites, and the values were based on the 8-hour time weighted average. Most of the chemicals were measured at levels below 10% of the Korean Occupational Exposure Limit (OEL) [11] (Table 4). Some of the higher values of gases (ozone, chloride, carbon dioxide, chloride, and phosphine), acids, and bases (hydrogen peroxide, phosphoric acid, and sulfuric acid) were 10-50% of the OEL (Table 4). The measurement records before 2002 were not available because of a lack of information.
Table 4.
Results of airborne measurement of chemicals (2002-2007)
All the chemicals were measured during 8 working hour for a full time shift.
Unit: parts per million (PPM) for gases except AsH3, alcohols and glycols and hydrofluoric acid, parts per billion (PPB) for AsH3, mg/m3 for and metals and acid-bases except hydrofluoric acid, OEL: occupational exposure limit of Korea for 8 hour working time.
GM: geometric mean, ND: non-detectable, Cl2: chloride, O3: ozone, CO2: carbon dioxide, NO: nitrogen monoxide, AsH3: Arsin, PH3: phosphine, CO: carbon monoxide, NH3: ammonia, HCL: Hydrochloric acid, H2O2: hydrogen peroxide, HF: hydrofluoric acid, HBr: hydrobromic acid, H2SO4: sulfuric acid (Group 1 carcinogen in International Agency of Research on Cancer), HNO3: nitric acid, KOH: Potassium hydroxide, H3PO4: phosphoric acid, AA: acetic acid, IPA: isopropyl alcohol, EG: ethylene glycol, Cu: copper, Pb: lead, Sn: Tin.
*Lower than 10% of OEL.
†10-50% of OEL.
‡Ceiling limit.
For general features of chemical hazards in the Korean semiconductor industry, material safety data sheets (MSDS) from 9 plants of 6 major semiconductor companies including the cases' company were reviewed in 2008. As a result, 263 different chemicals were compiled. Among them, 18 agents were group 1 and 2 carcinogens, classified by the International Agency of Research on Cancer (IARC), of which 5 agents (ethylene oxide, formaldehyde, ionizing radiation, perchloroethylene, and trichloroethylene) were correlated with leukemia or NHL (Table 5). Among 263 chemicals, ethylene oxide and formaldehyde were not found in the cases' company. However, ethylene oxide was found in one chemical at a level of 0.001% in another company and formaldehyde was found in a resin at a level of 0.1% in an ink in another company. Ionizing radiation was detected in the process conducted by Case No. 1, 2, and 4, even though the dose was at a background level. Case No. 3 and Case No. 5 may have been exposed to TCE from 1991 through 1995. Perchloroethylene was detected in only one sample, of which the level was 0.003 ppm at Plant A.
Table 5.
Carcinogens with some chemicals having hematologic effects using in plant A and B
FAB: fabrication, QE: quality engineering.
Discussion
Several confirmed human carcinogenic agents for occupational LHP cancer have been identified by IARC (Group 1), including benzene, ionizing radiation, ethylene oxide, 1,3-butadiene, and formaldehyde [12]. Among the chemicals used as raw materials and additives in the company where the seven cases occurred, none were IARC Group 1 human carcinogenic chemicals for LHP cancers (Table 2). The MSDSs for ethylene oxide and formaldehyde were found at some other major semiconductor companies, although their use has been very limited, but not from Plants A and B (Table 5).
It was suspected that various kinds of chemicals, including carcinogens, have been used in the semiconductor industry [2,13]. However, the detailed figures of chemicals and their carcinogenic risk in the industry have been veiled because of trade secrets in the high technology industry. In 2010, HSE found seven kinds of group 1 and 2 carcinogens designated by IARC (antimony trioxide, arsenic compounds, carbon tetrachloride, ceramic fiber, chromium, sulfuric acid, and trichloroethylene) [5], but none of them were LHP cancer-related. In 2007, the National Institute for Occupational Safety and Health in the US (NIOSH) reported the chemicals list used in an IBM plant (Endicotte) [14]. The report listed 20 known human carcinogens (IARC group 1) among 198 chemicals used from the late 1970s to 2004. Of these 20 carcinogens, benzene and formaldehyde were known human carcinogens with strong associations with LHP. However HSE and NIOSH did not measure air levels in the companies at that time.
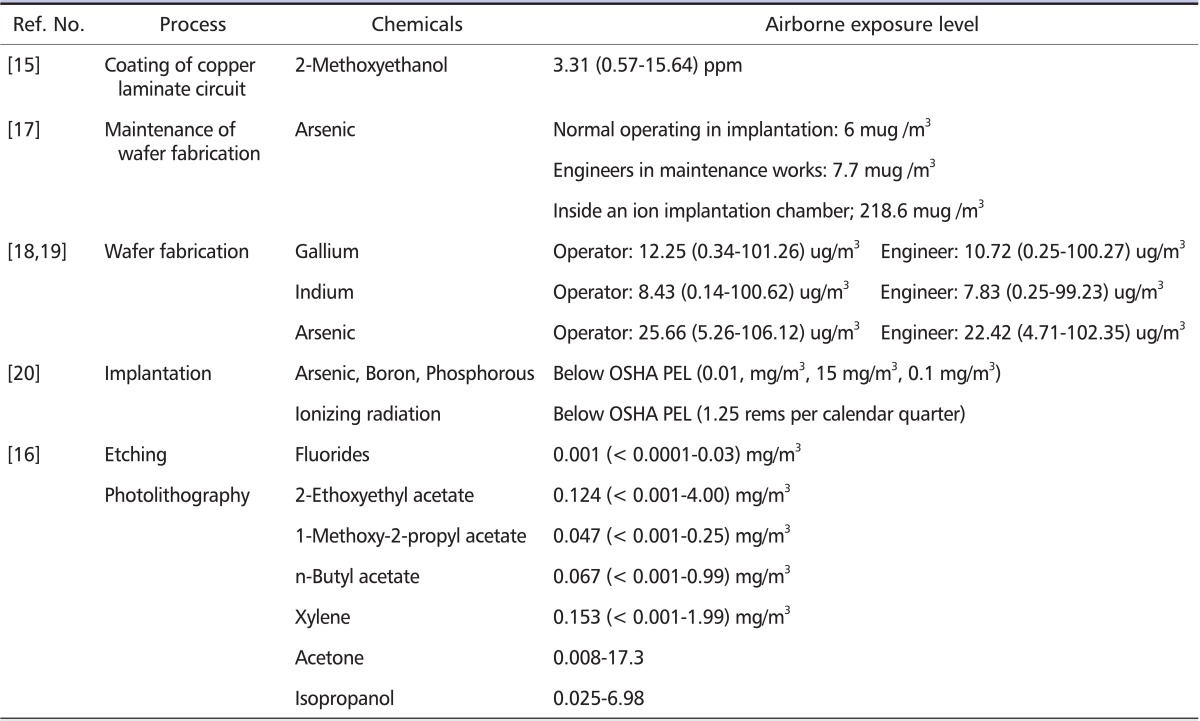
To the best of our knowledge, air measurements of carcinogenic agents related with LHP cancer in the semiconductor industry have not been previously reported. During 2007 to 2010, OSHRI measured air benzene levels at the workplace of the seven cases, but benzene was not detected from all samples [9]. The maximum benzene level from another study conducted in 2009 [10] was 0.31 ppb (minimum detection level: 0.1 ppb), which did not differ from the outside air concentration (less than 0.30 ppb) measured at the same time. Because most major chemicals used in the FAB department are passed through closed vessels in the automated system, exposure levels of most chemicals are low during normal procedures. The chemical levels from the annual work environment measurements required by the law (Table 4) were also low. Low concentration chemical exposure has also been reported in other studies. The most frequently studied chemicals in the semiconductor industry were [15,16], halides [16], highly toxic gases such as arsine [17], and rare-earth metals [18,19] such as gallium, indium, and arsenic (Table 6). The concentration of gases, metals, glycols, and other organic solvents from FAB industries [16-19] were low.
Table 6.
Review of exposure level of chemicals in semiconductor processes
OSHA: Occupational Safety and Health Administration in United States, PEL: permissible exposure limit.
The exact level of exposures before 2002 at this company remains unknown, because the details of the cases' previous working environments are unavailable at present. However, considering the working process and measurement results, we cannot conclude that the concentration of chemicals, including carcinogens related to LHP cancer, in previous workplaces might be much higher than the current level.
For benzene, the risk of LHP cancer has been reported to double from 40 ppm-years of cumulative doses of benzene [20]. Compared to this level, exposure duration of the seven cases was not enough to develop LHP cancer, especially at this low level of exposure. One study reported that even under low levels of exposure, exposure durations longer than 20 years [21], or very high levels of peak exposure (higher than 100 ppm) [22], might increase the risk of LHP cancers. However, the exposure periods of all cases in this study were less than 20 years (6 of them were < 10 years) (Table 1), and the peak exposure level was far below 100 ppm. There was no known benzene in major raw materials and ingredients in the semiconductor industry. We can assume that benzene could be generated from chemical interaction of other chemicals, however, this may result in very low levels. Therefore, accidental high levels of exposure to benzene is very unlikely. In addition, two cases (Case No. 1 and 7) had exposure durations of less than two years, and LHP cancer developed 9 to 10 years after leaving the company in two other cases (Case No. 5 and 6).
Two cases were presumed to be exposed to ion implantation instrument radiation for 20 months and 11 years, respectively; however, these instruments were located far from their working areas. Another case operated X-ray-generating instruments for 33 months. All three cases were diagnosed with AML, which is compatible with radiation-related cancer. However, all ionizing radiation measurements for these cases were similar to background levels except one measurement point for 5 samples (2.4 uSv/hr). Under normal working conditions, radiation exposure may not be regarded as a risk in the semiconductor industry; consequently, exposure levels have rarely been studied until now. One study reporting on ionizing radiation using personal badge dosimetry in an ion implant process [19], and it showed levels less than the Permissible Exposure Limit (PEL) of Occupational Safety and Health Administration (OSHA) in the US, which is 1.25 rem per calendar quarter for whole body radiation. In 2009, another study on the ionizing radiation exposure in the semiconductor industry was conducted by OSHRI. In this study, the ionizing radiation level was 0.15 ± 6.49 (0.01-13.32) uSv/hr.
Therefore, this information indicated that serious exposures are unlikely to occur while engineering controls remain intact. Because the ion implant and X-ray-generating instruments operated by Case No. 1, 2, and 5 had safety guards to prevent accidental exposure during operation and did not operate when the safety guards were released, there was no accidental exposure to radiation according to company records. Some of the co-workers claimed there might have been accidental radiation exposure because they had been told that some of the previous workers used to open the ion implant operation to speed up operation. If this happened, the workers would be exposed to high doses of radiation over short periods. However, after reviewing the cases' medical records we found no evidence of any acute health effects, such as radiation dermatitis, which would result from acute exposure to high doses of radiation.
Although LHP cancer is one of the most important occupational cancers, increased risk in the semiconductor industry is inconclusive. Major studies on standardized mortality ratios (SMR) or standardized rate ratios of cancers in semiconductor workers have been conducted in the UK [4,5,23-25] and the US [1,26,27]. The cancer risks found in these studies were not consistent. The facilities studied by HSE in the UK were the NSUK [4,5] and West midlands semiconductor factory [23-25]. Increased risk was found in the LHP, buccal cavity, and skin from West midlands factory workers, and in the central nervous system, oral cavity, stomach, and lung from the NSUK study. However, none of them were statistically significant. Facilities in the US were located in East Fishkill, New York, and San Jose, California [1,26,27]. East Fishkill and San Jose showed increased risks in various sites (colorectum, pancreas, skin, breast, prostate, kidney, NHL, and multiple myeloma); however, none of them were statistically significant except for prostate cancer. In contrast, a 2005 Taiwanese study reported a statistically significant increase of leukemia (SMR 3.3, 1.1-7.8) in 5 male cases [28], however, no detailed articles have been reported in peer-reviewed journals to date.
The differences according to country and factory may be due to the difference of the main product and its processes, and the operation period of each factory. The main process of East Fishkill, NSUK, and West midlands was wafer fabrication, and San Jose was storage devices. NSUK and West midlands had been operating since the 1970s, but East Fishkill and San Jose began earlier (1963 and 1956, respectively). Therefore, at this moment, estimations of cancer risk in semiconductor industries have been inconsistent, and no specific cancer sites for increased risk have been indicated.
The Epidemiological Investigation Review Board, which is one of the committees that issues scientific opinions on work-relatedness for claimed cases to COMWEL, concluded that the evidence of a causal relationship between malignant LHP disorder and the semiconductor industry is insufficient. The Board recommended that retrospective cohort studies which were conducted in 2008 by OSHRI should be continued until enough person-years have been accumulated in the cohort, in order to determine more consistent and scientific conclusions.
The major limitation of this study is the lack of exposure information before 2002 and many of the cases had started to work before 2002. Especially, Case No. 2, 3, 5, and 6 had begun to work in 1990s, for which we could not obtain exact information of exposure, such as to TCE or other chemicals at the time. Although we assume that the exposure level of carcinogenic agents related to LHP cancers, such as benzene and radiation, were not high based on the exposure assessments which OSHRI conducted in 2008 [9] and 2009 [10], it is impossible to confirm this assumption regarding the detailed situations of the exposures.
The association between benzene and leukemia was first announced in 1974 [29] and confirmed in 1982 [30]. Since then, ionizing radiation was confirmed as having a strong association with leukemia [31]. In 2008, ethylene oxide and 1,3-butadiene were found to have a strong link with LHP cancer [32]. And most recently (2009), the IARC concluded that formaldehyde was strongly correlated with leukemia [33]. To seek out more scientific facts on occupational cancers in the semiconductor industries, devoted research with international collaboration is essential. Long enough follow up of the cohort study including workers of contractors would be necessary for drawing scientific conclusion about causal-relationship for LHP disorders in the semiconductor industry.
In conclusion, from this investigation, we could not find sufficient evidence of exposure to occupational carcinogens in all seven cases. Known carcinogens related to LHP cancers were not found. Some carcinogenic chemicals like benzene were measured and were determined to be at background levels when the sensitivity of detection levels were increased. The risk of LHP cancer seems to be very low, when we consider the possible exposure level to carcinogenic agents such as benzene, formaldehyde, ethylene-oxide, and ionizing radiation, although detailed information for exposure levels before 2002 was not available.
Although, we could not find convincing evidence on known carcinogens for LHP cancers, and the epidemiological studies on that were inconclusive, we do not know the possibility of an unknown cause of LHP cancer or effects of multiple exposures of several chemicals in the semiconductor industry. Therefore, long-term future studies are needed to confirm the current result.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Beall C, Delzell E, Cole P, Brill I. Brain tumors among electronics industry workers. Epidemiology. 1996;7:125–130. doi: 10.1097/00001648-199603000-00004. [DOI] [PubMed] [Google Scholar]
- 2.Bailar JC, 3rd, Greenberg M, Harrison R, LaDou J, Richter E, Watterson A Trades Union Congress. Santa Clara County Center for Occupational Safety and Health and Silicon Valley Toxics Coalition. Cancer risk in the semiconductor industry: a call for action. Int J Occup Environ Health. 2002;8:163–168. doi: 10.1179/107735202800338948. [DOI] [PubMed] [Google Scholar]
- 3.McElvenny DM, Darnton AJ, Hodgson JT, Clarke SD, Elliott RC, Osman J. Cancer among current and former workers at National Semiconductor (UK) Ltd, Greenock. Sudbury, Suffolk (UK): Health and Safety Executive (HSE); 2001. Results of an investigation by the Health and Safety Executive; 91 pp. [Google Scholar]
- 4.McElvenny DM, Darnton AJ, Hodgson JT, Clarke SD, Elliott RC, Osman J. Investigation of cancer incidence and mortality at a Scottish semiconductor manufacturing facility. Occup Med (Lond) 2003;53:419–430. doi: 10.1093/occmed/kqg111. [DOI] [PubMed] [Google Scholar]
- 5.Darnton A, Wilkinson S, Miler B, MacCalman L, Galea K, Shafrir A, Cherrie J, McElvenny D, Osman J. A further study of cancer among the current and former employees of National Semiconductor (UK) Ltd., Greenock. Sudbury, Suffolk (UK): Health and Safety Executive and Institute of Occupational Medicine; 2010. 135 pp. [Google Scholar]
- 6.Clapp RW, Hoffman K. Cancer mortality in IBM Endicott plant workers, 1969-2001: an update on a NY production plant. Environ Health. 2008;7:1–4. doi: 10.1186/1476-069X-7-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee HE, Kim EA, Kang SK. Cancer mortality and incidence in Korean semiconductor workers. Saf Health Work. 2011;2:135–147. doi: 10.5491/SHAW.2011.2.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wald RH, Williams ME. Semiconductor Manufacturing. In: Hamilton RJ, Phillips SD, McCluskey GJ, editors. Occupational industrial, and Environmental Toxicology. 2nd ed. Philadelphia (PA): Mosby; 2003. pp. 550–563. [Google Scholar]
- 9.Park H, Jang JK, Shin JA. Quantitative exposure assessment of various chemical substances on wafer fabrication industry. Saf Health Work. 2011;2:39–51. doi: 10.5491/SHAW.2011.2.1.39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Park SH, Shin JA, Park HH, YI GY, Chung KJ, Park HD, Kim KB, Lee IS. Concentration levels of volatile organic compounds in photolithography process of semiconductor manufacturing company. Saf Health Work. 2011;2:210–217. doi: 10.5491/SHAW.2011.2.3.210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Occupational Safety and Health Act Enforcement Rules, Labor Employment Ordinance No.1. Korea: Ministry of Employment and Labor; 2010. [Google Scholar]
- 12.IARC monographs on the evaluation of carcinogenic risks to humans [Internet] Lyon (France): IARC; 2010. [cited 2010 Oct]. Available from: http://monographs.iarc.fr/ENG/Monographs/PDFs/index.php. [Google Scholar]
- 13.LaDou J, Rohm T. The international electronics industry. Int J Occup Environ Health. 1998;4:1–18. doi: 10.1179/oeh.1998.4.1.1. [DOI] [PubMed] [Google Scholar]
- 14.Pinkerton LE. An assessment of the Feasibility of a study of Cancer among former emplyees of the IBM facility in Endicotte, New York, Fianl Draft Report. Cincinnati (OH): National Institutue for Occupational Safety and Health (NIOSH); 2007. [Google Scholar]
- 15.Chang HY, Lin CC, Shih TS, Chan H, Chou JS, Huang YS. Evaluation of the protective effectiveness of gloves from occupational exposure to 2-methoxyethanol using the biomarkers of 2-methoxyacetic acid levels in the urine and plasma. Occup Environ Med. 2004;61:697–702. doi: 10.1136/oem.2003.011171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Woskie SR, Hammond SK, Hines CJ, Hallock MF, Kenyon E, Schenker MB. Personal fluoride and solvent exposures, and their determinants, in semiconductor manufacturing. Appl Occup Environ Hyg. 2000;15:354–361. doi: 10.1080/104732200301476. [DOI] [PubMed] [Google Scholar]
- 17.Park D, Yang H, Jeong J, Ha K, Choi S, Kim C, Yoon C, Park D, Paek D. A Comprehensive review of arsenic levels in the semiconductor manufacturing industry. Ann Occup Hyg. 2010;54:869–879. doi: 10.1093/annhyg/meq051. [DOI] [PubMed] [Google Scholar]
- 18.Chen HW. Exposure and health risk of gallium, indium, and arsenic from semiconductor manufacturing industry workers. Bull Environ Contam Toxicol. 2007;78:123–127. doi: 10.1007/s00128-007-9079-9. [DOI] [PubMed] [Google Scholar]
- 19.Ungers LJ, Jones JH. Industrial hygiene and control technology assessment of ion implantation operations. Am Ind Hyg Assoc J. 1986;47:607–614. doi: 10.1080/15298668691390322. [DOI] [PubMed] [Google Scholar]
- 20.Hayes RB, Yin SN, Dosemeci M, Li GL, Wacholder S, Travis LB, Li CY, Rothman N, Hoover RN, Linet MS. Benzene and the dose-related incidence of hematologic neoplasms in China. Chinese Academy of Preventive Medicine--National Cancer Institute Benzene Study Group. J Natl Cancer Inst. 1997;89:1065–1071. doi: 10.1093/jnci/89.14.1065. [DOI] [PubMed] [Google Scholar]
- 21.Ireland B, Collins JJ, Buckley CF, Riordan SG. Cancer mortality among workers with benzene exposure. Epidemiology. 1997;8:318–320. doi: 10.1097/00001648-199705000-00016. [DOI] [PubMed] [Google Scholar]
- 22.Collins JJ, Ireland B, Buckley CF, Shepperly D. Lymphohaematopoeitic cancer mortality among workers with benzene exposure. Occup Environ Med. 2003;60:676–679. doi: 10.1136/oem.60.9.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nichols L, Sorahan T. Cancer incidence and cancer mortality in a cohort of UK semiconductor workers, 1970-2002. Occup Med (Lond) 2005;55:625–630. doi: 10.1093/occmed/kqi156. [DOI] [PubMed] [Google Scholar]
- 24.Sorahan T, Pope DJ, McKiernan MJ. Cancer incidence and cancer mortality in a cohort of semiconductor workers: an update. Br J Ind Med. 1992;49:215–216. doi: 10.1136/oem.49.3.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sorahan T, Waterhouse JA, McKiernan MJ, Aston RH. Cancer incidence and cancer mortality in a cohort of semiconductor workers. Br J Ind Med. 1985;42:546–550. doi: 10.1136/oem.42.8.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Beall C, Bender TJ, Cheng H, Herrick R, Kahn A, Matthews R, Sathiakumar N, Schymura M, Stewart J, Delzell E. Mortality among semiconductor and storage device-manufacturing workers. J Occup Environ Med. 2005;47:996–1014. doi: 10.1097/01.jom.0000183094.42763.f0. [DOI] [PubMed] [Google Scholar]
- 27.Clapp RW. Mortality among US employees of a large computer manufacturing company: 1969-2001. Environ Health. 2006;5:1–10. doi: 10.1186/1476-069X-5-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hsieh GY, Wang JD, Cheng TJ, Chen PC. Exploring cancer risks among workers in the semiconductor industry in Taiwan. [cited 2011 April];Occup Environ Med [Internet] 2005 62:e15. Available from: http://oem.bmj.com/content/62/11.toc#Electronicpages. [Google Scholar]
- 29.Some Anti-Thyroid and Related Substances, Nitrofurans and Industrial Chemicals [Internet] Lyon (France): IARC; 1974. [cited 2010 Oct]. Available from: http://monographs.iarc.fr/ENG/Monographs/allmonos49.php. [Google Scholar]
- 30.Some Industrial Chemicals and Dyestuffs [Internet] Lyon (France): IARC; 1982. [cited 2010 Oct]. Available from: http://monographs.iarc.fr/ENG/Monographs/allmonos49.php. [Google Scholar]
- 31.Ionizing Radiation, Part 1: X- and Gamma (g)-Radiation, and Neutrons [Internet] Lyon (France): IARC; 2001. [cited 2010 Oct]. Available from: http://monographs.iarc.fr/ENG/Monographs/PDFs/index.php. [Google Scholar]
- 32.1,3-Butadiene, Ethylene Oxide and Vinyl Halides (Vinyl Fluoride, Vinyl Chloride and Vinyl Bromide) [Internet] Lyon (France): IARC; 2008. [cited 2010 Oct]. Available from: http://monographs.iarc.fr/ENG/Monographs/PDFs/index.php. [Google Scholar]
- 33.Baan R, Grosse Y, Straif K, Secretan B, El Ghissassi F, Bouvard V, Benbarahim-Tallaa L, Guha N, Freeman C, Galichet L, Cogliano V WHO International Agency for Research on Cancer Monograph Working Group. A review of human carcinogens--Part F: chemical agents and related occupations. Lancet Oncol. 2009;10:1143–1144. doi: 10.1016/s1470-2045(09)70358-4. [DOI] [PubMed] [Google Scholar]