Abstract
Objectives
The present study aims to determine the causal relationship between self-rated depression and experiences of injury and accidents in municipal firefighters.
Methods
A panel survey of 186 municipal firefighters measured with depressive symptoms according to the Beck's depression index (BDI) was conducted. The effects of job-related injuries and accidents were evaluated using self-administered questionnaires that were taken once in a 12-month period from 2005 to 2006. Firefighters were classified into the Depression Group or Control Group based on follow-up BDI results with a cutoff level that was set to having "over mild depression."
Results
The depression Group was comprised of 17 (9.1%) workers, including 9 firefighters who met had sufficient BDI scores twice in the 2-year test period and newly sufficient BDI scores in the follow-up test. A significantly higher number of subjects in the Depression Group experienced injuries and accidents in the 2-year test period as compared to the Control Group (15.4% vs. 1.5%, p=0.04). Firefighters who experienced injuries and accidents in the 2-year test period had a 7.4 times higher risk of being in the Depression Group than those who had not. As compared to accidents, near-miss accidents revealed stronger risks related to being classified as in the Depression group (adjusted odds ratio [OR] = 4.58, 95% confidence interval [CI] = 1.15-18.18 vs. Adjusted OR = 4.22, 95% CI = 1.08-16.58).
Conclusion
The above results suggest that we should establish an effective program to promote mental health for groups at high risk for self-rated depression, including persons who have experienced consecutive injuries and accidents as well as near-miss injuries.
Keywords: Depression, Occupational accidents, Rescue work, Municipalities
Introduction
Municipal firefighters in charge of firefighting and emergency services are exposed to various physical and chemical hazards including high temperatures, chemicals, and noise, and they experience a considerable number of accidents and injuries at their various workplaces. It is known that experiences of accidents and injury may cause depression, post-traumatic stress disorder (PTSD), and other disorders [1,2]. Therefore, municipal firefighters are known as a group with a high-risk for mental sequelae, such as depression or PTSD [3,4]. Firefighting is also known as a job that has is high-risk with respect to cerebrovascular and cardiovascular diseases, as stress has been a speculative risk factor for these diseases [5].
Municipal firefighters are routinely exposed to accidents, injuries, and severe stress more frequently than in other jobs, and the relation of such stresses to depression appears cyclical, making it difficult to determine a causal relationship. For example, a post-trauma depressive episode and avoidance of the event can cause adjustment disorder and failure of interpersonal relations [6], and work performance can deteriorate due to psychological exhaustion, so-called 'burn-out' [7], so depressed persons are more prone to accidents and injuries, and mental sequelae of injuries can worsen.
Though many studies have been conducted on the mental health of municipal firefighters, most published studies were cross-sectional, and the temporal sequence in the relationship between psychological disorders and risk factors was unclear [8-10]. A longitudinal study that observes whether continuation, worsening, or new onset of depression is caused by accidents and injuries is needed in order to more clearly evaluate how accidents and injuries affect levels of depression. In addition, in terms of identifying hazards, the self-rating scale has been used as a handy alternative for diagnosis by specialists, especially with respect to workplace health promotion. The present study was longitudinally conducted in order to determine the characteristics of injuries related to self-rated depression in municipal firefighters, observe shifts in the Depression Group with the mild depression cutoff level by repeatedly measuring its level for 2 years in the same study panel, and evaluate the relationship between the experience of accidents or injury in the previous 3 months and shifts in the Depression Group population.
Materials and Methods
Study population
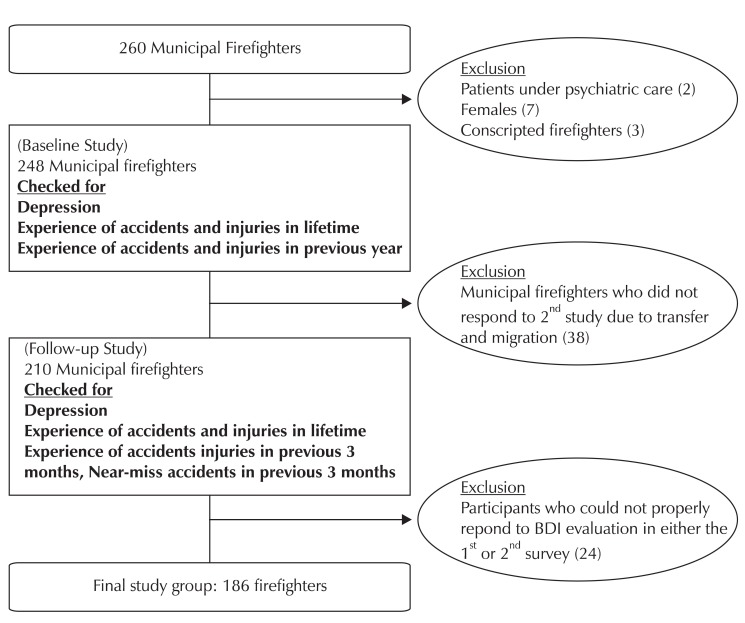
One of 22 municipal fire stations in Seoul was selected as the study panel, and five police stands, 5 special rescue teams, and 5 other administrative inspection divisions were assigned to this municipal fire station. The baseline study was conducted with 248 of 260 municipal firefighters. Of the twelve firefighters excluded from baseline study: 7 were female, 2 were patients with mental illness under expert care at the time of the baseline study, and 3 were conscripted firefighters. They were excluded because their progression and risk factors for depression were thought to be very different from those of other current municipal firefighters due to their different socioeconomic and job-related characteristics and emotions. Among the 210 municipal firefighters who responded to the follow-up study on their self-rated depression level after one year, 24 firefighters who did not respond to details of the required items, including the depression scales, were excluded, with the remaining 186 firefighters being selected as the final study group (Fig. 1).
Fig. 1.
Study flow chart with tools. BDI: Beck's depression index.
Study tools
Self-administered questionnaire on socioeconomic and job-related characteristics
Socioeconomic characteristics which may affect depression, such as age, education, salary, and marital status, were surveyed with self-administered questionnaires. Surveyed job-related characteristics were rank (firefighting class), job content, shiftwork, and working years. Rank was classified as firefighter, senior fire sergeant, fire sergeant, fire lieutenant, and fire captain or higher. Job content was classified as administrative, firefighting, rescue (accident), and emergency (health). Shiftwork was classified as no-shift, 3 shifts, 2 shifts, and 1 shift for 24 hours.
Beck's depression index (BDI)
Both initial and follow-up studies assessed self-rated depression scales using BDI that was validated for the Korean version [11]. BDI is measured by 21 questions with a 4-point Likert scale, and it has been known as an excellent evaluation indicator for identifying depression and for following up with subjects. Based on Beck's criteria [12], a BDI of 10 or higher was classified as 'depression', and a BDI under 10 was classified as 'normal'. The evaluation of both states at a baseline and repeating the evaluation a year later (follow-up) led to the classification of 4 groups according to shifts in the depression category: depression-onset (9 subjects), depression-continuation (8 subjects), normal (152 subjects), and depression-recovery (17 subjects). The operational definition was clarified as follows: The Depression Group (17 subjects) consisted of the former 2 groups, and the Control Group (169 subjects) consisted of the latter 2 groups.
The self-administered questionnaire on experience of accidents and injuries
Injury, a result of an accident, was defined as a loss of life or property caused by an accident, and a near-miss accident was defined as an accident without injury. In principle, the accidents and injuries investigated in this study were limitedly defined as job-related experiences. Therefore, questions on the self-administered questionnaires were limited to 'accidents or injuries that occurred while performing the job' in the baseline study; in the follow-up study, full explanations of all accidents and injuries in memory were collected, and those who responded with 'before work', 'damage during exercise', or 'on the way to the workplace' were excluded. Frequency and types of accidents, injuries, and near-miss accidents experienced in the 3 months prior to the survey were evaluated. Diseases caused by accidents and injury were investigated, allowing duplication of up to 3 per capita. The forms and types of the most memorable accidents and near-miss accidents were also investigated. Variables related with accidents and injuries were based on the guideline for records and classification of industrial injuries provided by Korea Occupational Safety and Health Agency [13]. Forms of accidents and injuries were supplemented by compensation records at International Firefighter Assistance [14].
Data collection
A letter describing the objective and content of the study and the self-administered questionnaire were sent to subjects for both the baseline and follow-up studies. Once questionnaires were collected, trained researchers reviewed the questions and checked for non-response.
The first baseline study surveyed depression with BDI and the Center for Epidemiologic Studies Depression Scale (CES-D) [15] as well as experiences of job-related accidents and injuries in each respondent's lifetime. The follow-up study surveyed the self-rated depression again with BDI and experiences of accidents and injuries in the 3 months prior to the survey were also surveyed.
Questionnaires were distributed to 248 subjects, and 210 subjects responded to both surveys with a response rate of 84.7%. 24 subjects who did not properly respond to the questions related to depression in either of the surveys were excluded from the 210 subjects, resulting in data from a total of 186 subjects being available for analysis.
Informed consent regarding privacy protection was provided. In the questionnaire there was information about socioeconomic status and past medical history as well as depression, and the opportunity to talk to a doctor was provided if desired.
Data processing and analysis
Whether classification into the 'depression' and 'normal' groups, as determined by scores of 10 in the BDI test, significantly changed after a year was analyzed by the McNemar test. Socioeconomic, job-related, accident-related, and injury-related characteristics were comparatively analyzed between the Depression and Control Groups and shifts in who was categorized in which group. For continuous variables, mean values were analyzed by t-tests, and categorical variables were analyzed by chi-square tests or Mantel-Haenszel tests. While logistic regression analysis was performed on dependent variables and characteristics related to experiences of accidents and injuries as independent variables for both groups, multivariate analysis was performed with adjustments for age, rank, and shiftwork, and univariate analysis was also performed. Statistical significance was applied with a 95% confidence interval (CI), and data were analyzed using SPSS v12.0 software (SPSS Inc., Chicago, IL, USA).
Results
Classification of study groups by shifts in depression category
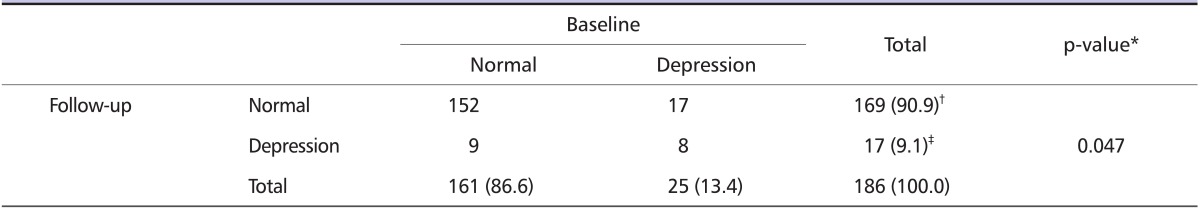
The point prevalence of the Depression Group which was measured by self-rated BDI was 13.4% at the baseline and 9.1% at the one-year follow-up mark. The depression-onset group (9 subjects) and depression-continuation group (8 subjects) together formed the Depression Group, and this accounted for 9.1% of the total subjects (Table 1).
Table 1.
Classification of study groups by shift in depression category
*McNemar test (p < 0.05).
†Control group.
‡Depression group.
Characteristics of the Depression Group analyzed by univariate analysis
Socioeconomic characteristics and job-related characteristic of subjects
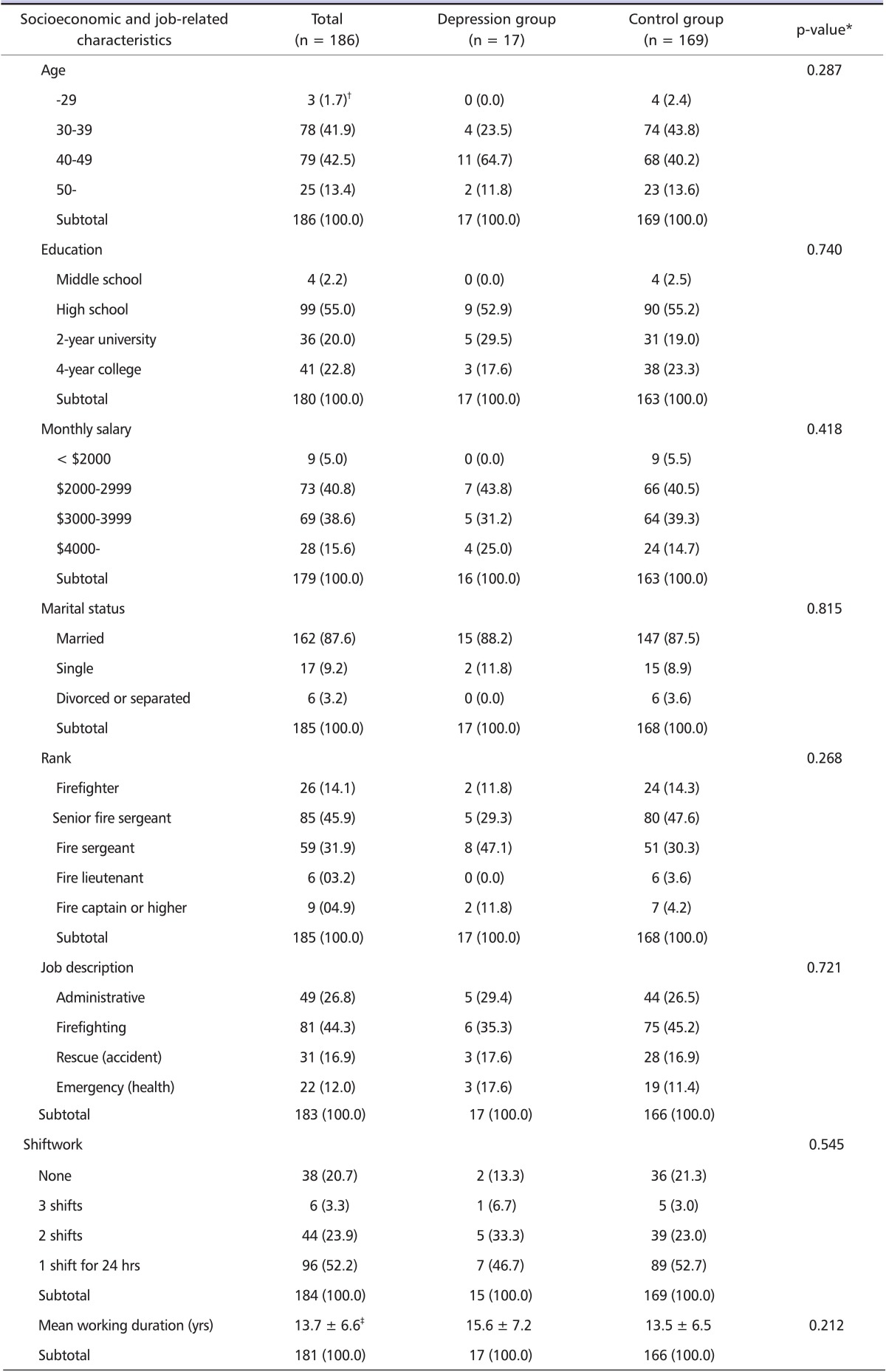
Most study subjects were in their 30s or 40s, 55% were high school graduates, 87.5% were married, and monthly salaries frequently ranged from 2 to 4 million won. At the baseline, 94.4% had been examined as an outpatient within a year, and 60.1% had been hospitalized. None of these socioeconomic characteristics were a statistically significant difference between the Depression and Control Groups. However, the number of subjects in their 30s and the number of subjects in their 40s were almost the same in the Control Group, while subjects in their 40s accounted for most of the Depression Group (64.7%). A poor home environment, such as divorce and separation, was more common in the Control Group, but the difference was not statistically significant. Job-related characteristics of the subjects were as follows: 60% were of the rank of senior fire sergeant or firefighters; 44% worked for firefighting, 17% worked for rescue, and 12% worked for emergency; the majority of subjects (50%) worked more than 84 hours on average per week; 52.2% worked 1 shift in 24 hours; and the mean working years were 13.7 years. Of these job-related characteristics, none indicated statistically significant differences between the Depression and Control Groups. In terms of rank, the number of fire sergeants (47.1%) outnumbered the number of senior fire sergeants (29.3%) in the Depression Group, but the difference was not significant. The mean working years was 15.6 years [standard deviation (SD) of 7.2 years] in the Depression Group and 13.5 years (SD of 6.5 years) in the Control Group, but the difference was not statistically significant (Table 2).
Table 2.
Socioeconomic and job-related characteristics of study subjects
*Chi-square test, Mantel-Haenszel test, and t-test (p < 0.05).
†n (%).
‡Mean ± standard deviation.
Characteristics related with accidents and injuries
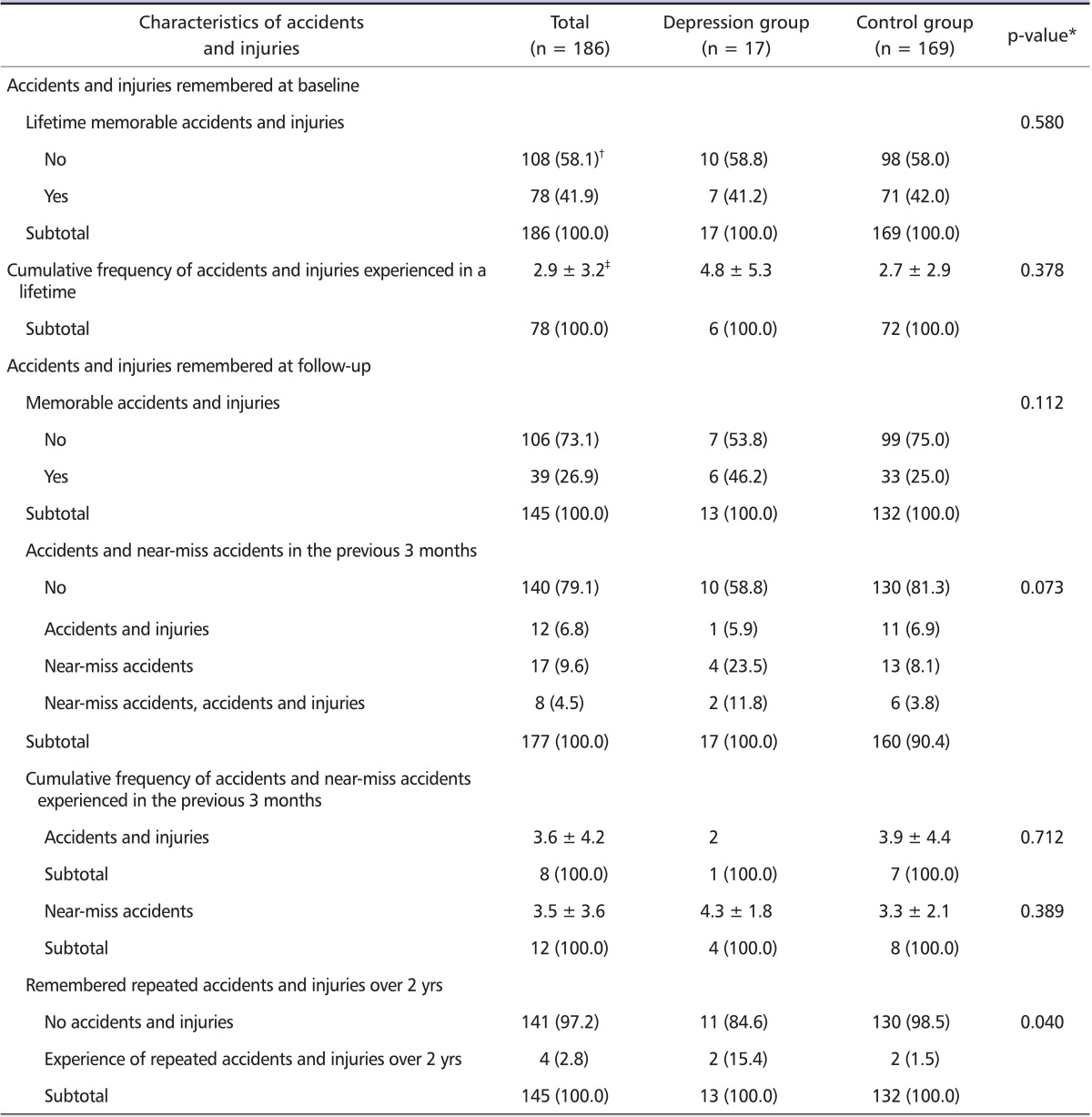
At the baseline, 108 subjects (42%) experienced accidents and injuries, and their mean cumulative frequency of accidents and injuries was 2.9 per person. Control subjects reported a mean of 2.7 accidents and injuries, while Depression Group subjects reported a mean of 4.8 accidents and injuries, showing that the Depression Group remembered more accidents and injuries than the Control Group; however, the difference was not statistically significant.
At the follow-up, 39 subjects (27%) had experienced memorable accidents and injuries, and 25 subjects (14.1%) experienced near-miss accidents. At this time, the mean number of accidents and injuries experienced within the last 3 months was 3.6, and the mean number of near-miss accidents was 3.5. Depression Group subjects reported a mean of 4.3 near-miss accidents, showing that they experienced and remembered more near-miss accidents than the Control Group, but the difference was not significant. For memorable near-miss accidents in a lifetime, 35.3% of the Depression Group reported related experiences, as compared to 11.9% of the Control Group, demonstrating that the Depression Group remembered more near-miss accidents than did the Control Group. While subjects remembering repeated accidents and injuries for 2 years were reported to be 2.8% of the total study group, 15.4% of the Depression Group remembered accidents and injuries, as compared to 1.5% of the Control Group, and the difference was statistically significant (p < 0.05) (Table 3).
Table 3.
Characteristics of accidents and injuries in depression and control groups
*Chi-square test or t-test (p < 0.05).
†Frequency (percent).
‡Mean ± standard deviation.
Evaluation of the effects of risk factors on the Depression Group
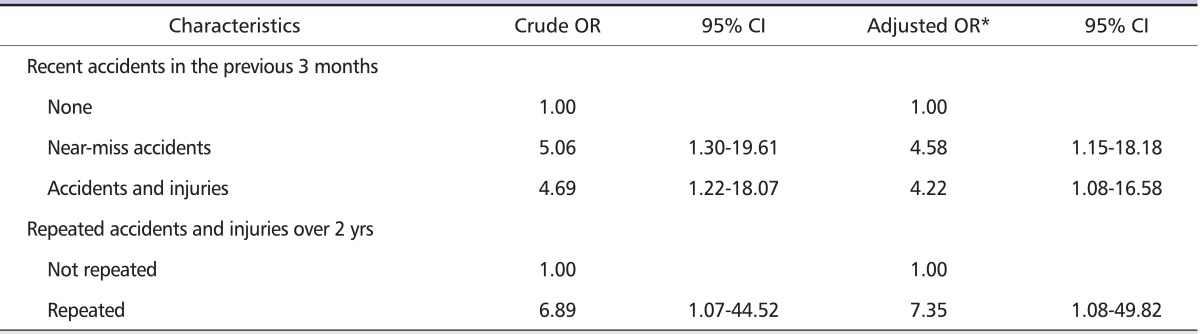
The effects of characteristics related with accidents and injuries on being classified as in the Depression Group were analyzed by univariate logistic regression analysis and multivariate logistic regression analysis that was adjusted for age, rank, and shiftwork (Table 4).
Table 4.
Logistic regression analysis for risk of being classified into the Depression Group due to accidents and injuries, near-miss accidents, and repeated accidents and injuries
OR: odds ratio, CI: confidence interval.
*Adjusted by age, rank, and shiftwork.
It was believed that the risk of being classified in the Depression Group depended on the characteristics of accidents, near-miss accidents, and would be higher when accidents were repeated over 2 years or the time of remembering the accidents was closer to the time of evaluating Depression Group prevalence. The risk of being classified into the Depression Group was significantly associated with those who had experienced accidents and injury in the previous 3 months. The risk of being classified into the Depression Group for those who had experienced near-miss accidents was 5 times higher than the risk for those who had not (95% CI 1.30-19.61), and > 4.6 times when adjusted for age, rank, and shift work (95% CI 1.15-18.18). The risk of being classified into the Depression Group in those who had experienced accidents and injuries was 4.2 times higher than the risk for those who had not when age, rank, and shiftwork were considered (95% CI 1.08-16.58).
The risk of being classified into the Depression Group for those who had experienced repeated accidents and injuries over 2 years was 6.9 times higher than the risk for those who had not (95% CI 1.07-44.52), and 7.4 times high when age, rank, and shiftwork were considered (95% CI 1.80-49.82).
Discussion
Municipal servants are known to be at high-risk for psychosocial risk factors due to limited budgets and strict regulations [16]. Among them, municipal firefighters are the most outstanding risk group for exposure to various hazards while working at an accident site. Workplace hazards for municipal firefighters include not only physical threats, such as noise, heat, and noxious gas [17], but also mental threats [18]. However, there are few studies focusing on mental sequelae arising from perceived stress due to accidents and injury.
Accidents and injuries happen frequently to municipal firefighters so it is an important issue. Among studies of mental health in firefighters, rescuing oneself could be a risk factor for stress [19]. In addition, extended working times, chronic sleep deprivation [20], and perceived job stress, including lack of job control [21], were reported to be potential risk factors for mental illness from a psychosocial perspective. The importance of prevention and management of workplace accidents and injury must be stressed. Otherwise, the frequency of accident risk may be too high to recognize causal relationships between accidents and injuries and mental sequelae from it. In addition, the cross-sectional study design used in previous studies is unable to determine causal relationships. In our study, a significant difference was not found between cumulative accident and injury experiences over a lifetime and depression that was measured at a baseline, which is different from the findings that may appear in a cross-sectional study setting. After we considered the follow-up survey with a panel study design, the experience of repeated injury and accidents was significantly higher in the Depression Group (15.4%) than in the Control Group (1.5%). Moreover, a worker exposed to repeated accidents and injuries over 2 yrs showed a 7.4-fold greater risk for being put into the Depression Group after adjusting for age, job rank, and shift work. Our result is in accordance with previous studies in which chronic repeated stress could be more detrimental with regard to depression than acute incidental stress [22]. It would follow that prevention and management of mental health should focus on repeated and frequent exposures to workplace accidents.
Young age, low socioeconomic status, being single, and low level of education were found to be risk factors for depression among the general population [23,24]. In our study, previously reported risk factors did not show a significant association with depression. In addition, our results showed depression point prevalences of 9.1% (follow-up survey) to 13.4% (baseline study), slightly higher than those found in the general population. The compared prevalence of depression in an interview study was shown to be 2.5% for lifetime prevalence and about 5% for point prevalence [25]. From the rating scale using CES-D, the point prevalence for men was assessed to be 6.8% [26], but in one study the point prevalence of male workers in service industries was as high as 15.6% [27]. Because the prevalence quoted in the study is different with respect to the scale and diagnosis situation, it is not comparable to the general population. However, the 'healthy worker effect' could attenuate the actual risk due to the 'toward null effect', that is, the actual burden of risk would be much higher than the result of our study.
We investigated the possible mental sequelae from workplace accidents and near-miss injuries, and our results supported the idea that near-miss accidents are also important in the control and management of depression in firefighters. In general, near-miss accidents occurred at a 33-fold more frequent rate than injury but it shared the same risk for workplace accidents [28]. Our results highlighted the importance of perceived stress - regardless of objective severity - due to accidents, as previous results have shown [29,30]. In the same context, perceived stress by near-miss injuries was probably more strongly related to mental health than the objective spectrum of harmful events.
Despite being the first such results to our knowledge, this study had the following limitations and countermeasure plans. Among 62 follow-up losses, 24 were from people whose operational definition was not applicable because BDI surveys with omitted answers were excluded. Moreover, 12 female workers who had substantially different characteristics and type of work were also excluded. Therefore, the characteristics of the 38 Follow-up losses due to job-circulation were comparable with the final panel. In Korea, where this study was based, municipal workers have to work in circulatory positions due to governmental policy. Despite this situation, so called "job-circulation", in terms of testing the internal consistency for the panel, we conducted additional analysis for the characteristics of the 38 Follow-up losses that were due to job-circulation. The results of analyzing the basic statistical characteristics of 34 Follow-up losses including 4 women showed that there were no significant differences in the distributions of age, shifts, or income. However, the proportion of workers engaging in medical rescue in the panel workforce was 12%, while only one person (2.9%) of the transferred workforce engaged in medical rescue. In addition, there was a limited number of subjects and the number of defined cases of depression was also limited in this study, so this may be a limitation of our study. However, since this study was planned as a specific panel study of those in charge of one area, only a limited number could be recruited as panel participants. Furthermore, since the Follow-up loss of 13% from the small study group was not largely different to the demographic characteristics of the final subjects for the study, it was decided that the original characteristics of the panel was maintained.
Female workers were excluded for the subject about mental illness. It is known that female workers are vulnerable to mental illnesses, but the reason female workers were excluded from the study was because their duties were completely different to male firefighters. The firefighters studied were people who had indirectly experienced shocking scenes of disaster that may cause psychological trauma, but female workers in fire stations work only in office administration for the majority of their time.
In addition, those who already have depression can influence the natural course. It is not clear whether an episode of depression is the first episode or a relapse, being treated with medication or not, or confirmed as depression, so they were excluded in the study. The occupational or non-occupational stress of these individuals could not be considered in this study, and that would be a major cause of depression in some points of view.
As was pointed out, the causes of mental aftereffects, the elements related to mental aftereffects, and psychological and biological influences were not considered. Occupational and non-occupational stress can be applied as mediating risk factors associated external event such as accident and injury. However, the direction of this study focused on the existence and characteristics of work-related accident and injury and its' detrimental mental effects, not the mechanisms by which depression occurred with mediating risk factors from stressful event. Accidents that influence depression and the stress and influence of biological change in the process can be handled in another study design. In the planning stage of this study, occupational stress was considered and researched together, but the results were excluded from the manuscript. Because relationships between trauma, stress, and depression were difficult to explain in a 2-year panel study, study results were interpreted in the parallel development of stress and self-rated depression. To minimize non-occupational stress, the study was limited to males and occupational stress, including social support, was checked. Stress related to organizational structure was notably 8 times higher (OR = 8.029, 95% CI 1.732-37.217) in Depression Group, while no other elements for occupational stress were shown to be significant with risk of Depression Group (The results not included).
The protective effect of psychosocial factors, such as social support [31] and self-efficacy [32], may need to be explored further. Even though we conducted examination with the self-rated symptoms and sign of depression by BDI, stress-related symptoms, such as sleep disturbance and migraines, would be helpful for explaining possible mechanisms relating injury to depression.
When designing the study, it was determined that self-administered questionnaires were the best option for obtaining data because the self-rated depression scale was a dependent variable in the utilized strategy. In terms of preventing bias from the use of self-rating scales and questionnaires, all efforts were made for the quantification of questionnaire results and apparatus against bias. Also, objective data, such as the classification of shift and rank, were verified. The fact that this study used BDI, which is a self-rating scale, instead of a structured interview tool for evaluating depression needs to be considered. The reliability of the self-rating scale methods for comparing BDI values was shown to be trustworthy before [33]. However, it should be specified that this study was not about medically diagnosed depression, but symptoms of depression. In a study conducted on 120 psychiatrists and clinical psychologists in the country, 70.89% answered that the BDI and other scales concur with clinical practice [34], supporting the claim that there would be little disconcordance between questionnaires and depression diagnosis.
In addition, panel studies are often vulnerable to instrumentation threat if the researcher in the panel studies is not confined to the variables measured in the original study. Therefore, variations in questionnaire design were implemented to avoid participants learning answer patterns. For instance, we measured the level of depression at baseline with 2 types of questionnaires, both including BDI and CES-D. At follow-up, however, we measured only BDI. When measuring the number of injuries and accidents, we mixed open and closed questions and used practical vignettes. In summary, we attempted to gather valid participant data with well-organized questionnaires despite repeated measurements of depression.
On the other hand, we were unable to develop questionnaires for both injury and accidents specific for firefighters. To minimize this study limitation, we selected questionnaire items based on standardized categories for injury and accidents according to government documentation of a 'survey for severe accidents', and modified the items with standardized codes for compensation claims developed by the International Firefighter Association.
In terms of study validity, interviewers assisted participants with the self-administrative questionnaire and used practical vignettes to help them fully understand survey items, which may help to prevent recall and information bias. In contrast, the number of respondents for injury was limited. To validate our findings, a nation-wide follow-up study is needed. Between accidents and depression, the identification of risk factors as underlying mechanisms could help explain new perspectives for the effect of injury.
Despite several possibilities for under- or over-estimation, this is the first attempt to estimate the causal relationship between injury and accidents and self-rated depression in municipal firefighters through a longitudinal study.
In conclusion, the present study investigated the causal relationship between self-rated depression and the experiences of injury and accidents in male municipal firefighters through a longitudinal panel study design. The classification into a Depression or Control Group was determined by a BDI questionnaire.
The point prevalence in our final survey was 9.1%, which was higher than that in the general population. With regard to injury and accidents, the Depression Group reported significantly more experiences of repeated injury and accidents over a 2-yr period. The risk for the Depression Group was 4.6-fold higher for firefighters experiencing near-miss accidents and 4.2-fold higher for firefighters experiencing injury and accidents compared to those who did not. Moreover, firefighters reporting memorable repeated accidents and injuries over 2 yrs had a 7.4-fold higher risk for being classified into the Depression Group. Based on our results, it seems reasonable that the development of a control and management strategy for mental health in male municipal firefighters should focus on not only injury and accidents, but also on near-miss injury and repeated injury and accidents as well. A broad approach should be considered, encompassing social and academic-based issues when assessing psychosocial risk or mental health in high-risk groups, as well as the practical issue of training and equipment availability.
Acknowledgements
We thank Hyoung-Ryoul Kim MD.Ph.D. and Yong-kyu Kim MD Ph.D. for review of an early version of this paper and Jung-wan Koo MD.Ph.D. for support with periodic medical screening for firefighters. An earlier version was presented as the thesis for the board of M.PH at the Catholic Graduate School of Public Health in 2006. An earlier version was presented at the 29th International Congress of Occupational Health in 2009.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Ehring T, Ehlers A, Glucksman E. Do cognitive models help in predicting the severity of posttraumatic stress disorder, phobia, and depression after motor vehicle accidents? A prospective longitudinal study. J Consult Clin Psychol. 2008;76:219–230. doi: 10.1037/0022-006X.76.2.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ward CL, Lombard CJ, Gwebushe N. Critical incident exposure in South African emergency services personnel: prevalence and associated mental health issues. Emerg Med J. 2006;23:226–231. doi: 10.1136/emj.2005.025908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Guidotti TL, Clough VM. Occupational health concerns of firefighting. Annu Rev Public Health. 1992;13:151–171. doi: 10.1146/annurev.pu.13.050192.001055. [DOI] [PubMed] [Google Scholar]
- 4.Fullerton CS, McCarroll JE, Ursano RJ, Wright KM. Psychological responses of rescue workers: fire fighters and trauma. Am J Orthopsychiatry. 1992;62:371–378. doi: 10.1037/h0079363. [DOI] [PubMed] [Google Scholar]
- 5.Haas NS, Gochfeld M, Robson MG, Wartenberg D. Latent health effects in firefighters. Int J Occup Environ Health. 2003;9:95–103. doi: 10.1179/oeh.2003.9.2.95. [DOI] [PubMed] [Google Scholar]
- 6.Thornton PI. The relation of coping, appraisal, and burnout in mental health workers. J Psychol. 1992;126:261–271. doi: 10.1080/00223980.1992.10543360. [DOI] [PubMed] [Google Scholar]
- 7.Ahola K, Honkonen T, Kivimäki M, Virtanen M, Isometsä E, Aromaa A, Lönnqvist J. Contribution of burnout to the association between job strain and depression: the health 2000 study. J Occup Environ Med. 2006;48:1023–1030. doi: 10.1097/01.jom.0000237437.84513.92. [DOI] [PubMed] [Google Scholar]
- 8.McLellan TM, Selkirk GA. The management of heat stress for the firefighter: a review of work conducted on behalf of the Toronto Fire Service. Ind Health. 2006;44:414–426. doi: 10.2486/indhealth.44.414. [DOI] [PubMed] [Google Scholar]
- 9.Chen YS, Chen MC, Chou FH, Sun FC, Chen PC, Tsai KY, Chao SS. The relationship between quality of life and posttraumatic stress disorder or major depression for firefighters in Kaohsiung, Taiwan. Qual Life Res. 2007;16:1289–1297. doi: 10.1007/s11136-007-9248-7. [DOI] [PubMed] [Google Scholar]
- 10.Ward CL, Lombard CJ, Gwebushe N. Critical incident exposure in South African emergency services personnel: prevalence and associated mental health issues. Emerg Med J. 2006;23:226–231. doi: 10.1136/emj.2005.025908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hahn HM, Yum TH, Shin YW, Kim KH, Yoon DJ, Chung KJ. A standardization study of beck depression inventory in Korea. J Korean Neuropsychiatr Assoc. 1986;25:487–502. [Google Scholar]
- 12.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 13.Korea Occupational Safety and Health Agency. The code for documentation and classification for occupational injury and accident. Incheon (Korea): Korea Occupational Safety and Health Agency; 2006. KOSHA CODE-G-8-2006. Korean. [Google Scholar]
- 14.Death and injury survey, 1998. Washington, DC: International Association of Firefighters; 1999. [Google Scholar]
- 15.Chon KK, Choi SC, Yang BC. Integrated adaptation of CESD in Korea. Korean J Clin Psychol. 2001;6:59–76. [Google Scholar]
- 16.Higgins P, Ezike C, Orris P. Occupational health services for municipal employees. Occup Med. 2001;16:11–21. [PubMed] [Google Scholar]
- 17.Bolstad-Johnson DM, Burgess JL, Crutchfield CD, Storment S, Gerkin R, Wilson JR. Characterization of firefighter exposures during fire overhaul. AIHAJ. 2000;61:636–641. doi: 10.1080/15298660008984572. [DOI] [PubMed] [Google Scholar]
- 18.Corneil W, Beaton R, Murphy S, Johnson C, Pike K. Exposure to traumatic incidents and prevalence of posttraumatic stress symptomatology in urban firefighters in two countries. J Occup Health Psychol. 1999;4:131–141. doi: 10.1037//1076-8998.4.2.131. [DOI] [PubMed] [Google Scholar]
- 19.Moran C, Britton NR. Emergency work experience and reactions to traumatic incidents. J Trauma Stress. 1994;7:575–585. doi: 10.1007/BF02103008. [DOI] [PubMed] [Google Scholar]
- 20.Takeyama H, Itani T, Tachi N, Sakamura O, Murata K, Inoue T, Takanishi T, Suzumura H, Niwa S. Effects of a modified ambulance night shift system on fatigue and physiological function among ambulance paramedics. J Occup Health. 2009;51:204–209. doi: 10.1539/joh.l7040. [DOI] [PubMed] [Google Scholar]
- 21.Salazar MK, Beaton R. Ecological model of occupational stress. Application to urban firefighters. AAOHN J. 2000;48:470–479. [PubMed] [Google Scholar]
- 22.Tennant C. Life events, stress and depression: a review of recent findings. Aust N Z J Psychiatry. 2002;36:173–182. doi: 10.1046/j.1440-1614.2002.01007.x. [DOI] [PubMed] [Google Scholar]
- 23.Brown GW, Harris TO, Eales MJ. Aetiology of anxiety and depressive disorders in an inner-city population. 2. Comorbidity and adversity. Psychol Med. 1993;23:155–165. doi: 10.1017/s0033291700038940. [DOI] [PubMed] [Google Scholar]
- 24.Kendler KS, Karkowski LM, Prescott CA. Stressful life events and major depression: risk period, long-term contextual threat, and diagnostic specificity. J Nerv Ment Dis. 1998;186:661–669. doi: 10.1097/00005053-199811000-00001. [DOI] [PubMed] [Google Scholar]
- 25.The epidemiological survey of psychiatric illnesses in Korea. Seoul (Korea): Ministry of Health and Welfare (KR); 2006. p. 6. Korean. [Google Scholar]
- 26.Cho MJ, Nam JJ, Suh GH. Prevalence of symptoms of depression in a nationwide sample of Korean adults. Psychiatry Res. 1998;81:341–352. doi: 10.1016/s0165-1781(98)00122-x. [DOI] [PubMed] [Google Scholar]
- 27.Byun CB, Youn K, Jung-Choi K, Cho Y, Paek D. Depressive symptoms of workplace violence exposed subjects in Korea. Korean J Occup Environ Med. 2009;21:314–323. [Google Scholar]
- 28.Heinrich HW. Industrial accident prevention. New York: McGraw-Hill; 1931. 153 pp. [Google Scholar]
- 29.Reno RM, Halaris AE. The relationship between life stress and depression in an endogenous sample. Compr Psychiatry. 1990;31:25–33. doi: 10.1016/0010-440x(90)90051-s. [DOI] [PubMed] [Google Scholar]
- 30.Mundt C, Reck C, Backenstrass M, Kronmüller K, Fiedler P. Reconfirming the role of life events for the timing of depressive episodes A two-year prospective follow-up study. J Affect Disord. 2000;59:23–30. doi: 10.1016/s0165-0327(99)00127-5. [DOI] [PubMed] [Google Scholar]
- 31.Suttajit S, Punpuing S, Jirapramukpitak T, Tangchonlatip K, Darawuttimaprakorn N, Stewart R, Dewey ME, Prince M, Abas MA. Impairment, disability, social support and depression among older parents in rural Thailand. Psychol Med. 2010;40:1711–1721. doi: 10.1017/S003329170999208X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Konttinen H, Silventoinen K, Sarlio-Lähteenkorva S, Männistö S, Haukkala A. Emotional eating and physical activity self-efficacy as pathways in the association between depressive symptoms and adiposity indicators. Am J Clin Nutr. 2010;92:1031–1039. doi: 10.3945/ajcn.2010.29732. [DOI] [PubMed] [Google Scholar]
- 33.Lee YH, Song JY. A Study of the reliability and the validity of the BDI, SDS, and MMPI-D scales. Korean J Clin Psychol. 1991;10:98–113. [Google Scholar]
- 34.Lee EJ, Kim JB, Shin IH, Lim KH, Lee SH, Cho GA, Sung HM, Jung SW, Zmimmerman M, Lee Y. Current use of depression rating scales in mental health setting. Psychiatry Investig. 2010;7:170–176. doi: 10.4306/pi.2010.7.3.170. [DOI] [PMC free article] [PubMed] [Google Scholar]