Abstract
Objective
To investigate the reinforcement of Bis-GMA/TEGDMA dental resins (without conventional glass filler) and the corresponding composites (with conventional glass filler)containing vari ed mass fractions of halloysite nanotubes (HNTs).
Methods
Three dispersion methods were studied to separate the silanized halloysite as individual HNTs and to uniformly distribute them into dental matrices. Photopolymerization induced volumetric shrinkage was measured by using a mercury dilatometer. Real time near infrared spectroscopy was adopted to study the degree of vinyl double bond conversion and the photopolymerization rate. Mechanical properties of the composites were tested by a universal mechanical testing machine. Analysis of Variance (ANOVA) was used for the statistical analysis of the acquired data. Morphologies of halloysite/HNTs and representative fracture surfaces of the reinforced dental resins/composites were examined by SEM and TEM.
Results
Impregnation of small mass fractions (e.g., 1% and 2.5%) of the silanized HNTs in Bis-GMA/TEGDMA dental resins/composites improved mechanical properties significantly; however; large mass fractions (e.g., 5%) of impregnation did not further improve the mechanical properties. The impregnation of HNTs into dental resins/composites could result in two opposite effects: the reinforcing effect due to the highly separated and uniformly distributed HNTs, and the weakening effect due to the formation of HNT agglomerates/particles.
Significance
Uniform distribution of a small amount of well-separated silanized HNTs into Bis-GMA/TEGDMA dental resins/composites could result in substantial improvements on mechanical properties.
Keywords: Dental composites, Bis-GMA, TEGDMA, Halloysite nanotubes
1. Introduction
Dental composites, consisting of polymeric resin matrices with mass fractions of ~30% and inorganic fillers with mass fractions of ~70%, were first developed approximately half a century ago; compared to dental amalgams, the composites possess better esthetic properties and fewer safety concerns, while have shown reasonably satisfactory clinic results. Hence, the dental composites have been widely adopted by the dental profession as restorative materials of choice.
Dental resins are typically cured/hardened by photo-initiated free radical polymerization. Camphorquinone (CQ) is a common visible-light initiator, and ethyl-4-(N,N’-dimethylamino) benzoate (4EDMAB) is a common co-initiator/accelerator. The dental monomer of 2.2’-bis-[4-(methacryloxypropoxy)-phenyl]-propane (Bis-GMA) has been widely used as a base monomer since it was invented in the early 1960’s [1,2]. Bis-GMA is a very viscous liquid; to improve the handling quality, a diluent monomer of tri (ethylene glycol) dimethacrylate (TEGDMA) is usually added to thin the resins. In the Bis-GMA/TEGDMA dental resin systems, Bis-GMA functions to reduce the photopolymerization induced volumetric shrinkage and to enhance the resin reactivity, while TEGDMA provides for the increased vinyl double bond conversion [3,4].
Compared to dental amalgams, dental composites reinforced with inorganic fillers (e.g., silanized glass/ceramic particles) have relatively low strength and durability, which limited their applications [5–8]. Presently, the commercially available dental composites have the values of flexural strength varying from 80 to 140 MPa, which can fulfill basic requirements of filling in small tooth-cavities but cannot be utilized for large stress-bearing restorations (e.g., crowns and bridges). Furthermore, the service time of dental composites is generally shorter than 5 years [5], while dental amalgams typically have the service time of 15 years or longer [9,10]. Investigations on the composite failures have revealed that, ironically, inorganic filler particles that are added to the dental resins for fortifying the materials are actually responsible, at least in part, for their demise [11,12]. Many inorganic filler particles are spherical or irregular in shape; during function, the masticatory stress is transmitted through boluses of foods onto surfaces of filler particles projecting from the occlusal surface. Since the filler particles are considerably harder than the resin matrices, much of the stress is transmitted through the particles into the resins. Wherever the submerged portions of particles are angular or irregular in shape, the stress concentration could become excessively high. Such a condition tends to generate small cracks around the particles, thereby weakening the composites locally.
The reinforcement of dental composites using micron-scaled fibers/whiskers with high mechanical strength has been demonstrated to result in dramatic improvements on the properties [13–16]. For example, Xu and co-workers revealed that, two-fold increase in strength and toughness could be readily achieved through the impregnation of extremely strong ceramic fibers/whiskers into dental composites; additionally, it would also lead to improvements on polishability, water-absorption, and strength-durability [17–21]. The bridging mechanism has been proposed to explain the reinforcement effect: if a micro-crack is initiated in a matrix under contact wear and/or other stresses, the fibrillar filler particles remain intact across the crack planes and support the applied load. Crack-opening is therefore resisted by the bridging fillers, and the matrix is reinforced consequently. The requirements for effective bridging fillers include high mechanical properties (e.g., strength and modulus) and large surface-to-volume ratios.
Unlike micron-scaled fibers/whiskers, halloysite (Al2Si2O5(OH)4·2H2O) is composed of nano-scaled crystals (tubes); the halloysite nanotube (HNT) is a two-layered aluminosilicate with predominantly hollow/tubular structure [22,23]. Since halloysite is a naturally occurring mineral that is easy to purify, HNTs are available in large quantity; and it is much more cost-effective than many other nano-scaled fillers (such as carbon nanotubes/nanofibers) [24]. Furthermore, halloysite is safe, biocompatible, and easy to process [22,24]. HNTs have also been studied for clinical relevance; for example, Hughes and King reported that the naturally occurring HNTs could be used to enhance the capture of flowing cells [25]. The diameters of HNTs are typically in tens of nanometers, and the lengths are usually in the range from ~200 nm to 1–2 μm [23]. The outer surface of HNTs has chemical properties similar to SiO2, while the inner surface has chemical properties similar to Al2O3. Nano-scaled crystals of HNTs possess a high degree of structural perfection and the concomitant superior mechanical properties; for example, the Young’s modulus of HNTs is estimated in the range of 230–340 GPa, which is calculated via the same geometric optimization protocol as used for imogolite nanotubes [26,27]. Additionally, unlike layered silicates (such as montmorillonite), which are difficult to completely exfoliate into nano-scaled silicate layers and to uniformly distribute in dental matrices, halloysite is relatively easy to separate into individual HNTs and to distribute uniformly in dental matrices. This is because the spacing among agglomerated HNTs in halloysite is much larger than that among silicate layers in montmorillonite; as a result, the interaction of HNTs is considerably weaker than that of silicate layers in montmorillonite. Hence, there is no need for chemical substitution of metal ions with alkyl ammonium ions (a widely adopted method for intercalation/exfoliation of montmorillonite for the preparation of nanocomposites); the HNTs in halloysite can be well-separated by simply dispersing the halloysite powder in polar solvents (such as acetone) followed by mechanical stirring [28]. Furthermore, the interfacial bonding strength between the silanized HNT filler and the dental resin matrix can be reasonably high since there are abundant Si–OH groups on the outer surface of HNTs; and these groups can readily react with silane coupling agents such as 3-methacryloxypropyltrimethoxy (MPTMS).
The aim of this study was to investigate the Bis-GMA/TEGDMA dental resins (without conventional glass filler) and the corresponding composites (with conventional glass filler) reinforced with varied mass fractions of HNTs. The hypothesis was that uniform distribution of well-separated silanized HNTs into Bis-GMA/TEGDMA dental resins/composites would result in substantial improvements on the mechanical properties. To test the hypothesis, photo-cured Bis-GMA/TEGDMA dental resins/composites containing varied mass fractions of silanized HNTs were systematically fabricated; three dispersion methods were studied to separate the silanized halloysite as individual HNTs and to uniformly distribute them into dental matrices. The photopolymerization induced volumetric shrinkage was measured by a mercury dilatometer. The flexural strength, elastic modulus, and work of fracture were acquired from the standard three-point flexural test (ASTM D 790). The degree of vinyl double bond conversion and the photopolymerization rate were studied in situ by real time near infrared spectroscopy (RT-NIR). Analysis of Variance (ANOVA) was used for the statistical analysis of the acquired data. Morphological structures of HNTs and representative fracture surfaces of the reinforced dental resins/composites were examined by transmission electron microscope (TEM) and scanning electron microscope (SEM).
2. Materials and methods
2.1. Materials
Bis-GMA, TEGDMA, CQ, 4EDMAB, MPTMS, and acetone were purchased from the Sigma-Aldrich Co. (Milwaukee, WI) and used without further purification. Purified halloysite powder (1250 mesh) was provided by the Dalian Global Mineral Co. (Dalian, China). The conventional (dental) glass filler for this study was finely milled 7% (mass fraction) silanized barium borosilicate glass powder (V-117-2707) provided by the Esstech Co. (Essington, PA).
2.2. Fabrication
2.2.1. Silanization of HNTs
The as-received halloysite powder was first dispersed in acetone with a mass fraction of 5%. The suspension was then vigorously stirred for 4 h at 400 rpm using a Heidolph RZR 50 Heavy Duty Stirrer. This process would convert the halloysite powder into separated HNTs, but the separated HNTs (existing in suspension) could re-aggregate into agglomerates/particles, particularly if acetone was removed. Thereafter, MPTMS was added into the suspension with a mass fraction of 10% to halloysite; the system was then stirred mechanically for 4 h at 400 rpm followed by heated at 90 °C to remove the solvent of acetone.
2.2.2. Dispersion of silanized HNTs into dental matrix
The silanized HNTs (with mass fractions ranging from 0% to 5%) were added into a dental resin system, which consisted of 49.5% Bis-GMA, 49.5% TEGDMA (the mass ratio of Bis-GMA/TEGDMA was 1/1), 0.2% CQ, and 0.8% 4EDMAB. Three methods were studied to identify the optimal one for uniform dispersion of the silanized halloysite as highly separated HNTs into the dental matrix. The prepared systems of Bis-GMA/TEGDMA/HNT were further mixed with conventional dental glass fillers (with the combined mass fraction of glass filler and HNT being 70%) to prepare three dental pastes.
Method A: The silanized HNTs were first dispersed in TEGDMA followed by being mechanically stirred for 2 h at 400 rpm. Bis-GMA, CQ, and 4EDMAB were then added; after that, the system was mechanically stirred for another 30 min at 400 rpm.
Method B: The silanized HNTs were dispersed into the mixture of TEGDMA/acetone (mass ratio: 20/80) first followed by being mechanically stirred for 2 h at 400 rpm. Acetone was then removed by evaporation; thereafter, Bis-GMA, CQ, and 4EDMAB were added, and the system was then stirred for another 30 min at 400 rpm.
Method C: The silanized HNTs were first dispersed into 80% (mass fraction) acetone diluted dental resin system (composition as described above) followed by being stirred for 2 h at 400 rpm. Thereafter, acetone was removed by evaporation, and the system was further mechanically stirred for another 30 min at 400 rpm.
2.3. Characterization and evaluation
2.3.1. Volumetric shrinkage
The photopolymerization induced volumetric shrinkage was measured by a mercury dilatometer made by the Paffenbarger Research Center of the American Dental Association Foundation (Gaithersburg, MD). The essential component of this dilatometer is a mercury-filled tube with one end clamped against a glass slide, in which dental pastes are polymerized upon initiation by using a visible light-curing unit. The volume change is monitored by a Teflon plunger, which is sitting on top of the mercury column and connecting to a linear variable differential transducer (LVDT). Since the volume of mercury is affected by temperature, a thermistor is applied to monitor the temperature variation. The output of thermistor and the read of LVDT are collected by a computer, and the volume changes of the mercury are corrected by using the least-squares algorithm in considering of temperature fluctuations. During the measurement, after the reading of corrected LVDT was stabilized, the curing light was turned on for 1.0 min followed by the post-curing time of 1.0 h; thereafter, the curing light was turned on once more for another 30 s. If there was no significant change of the corrected LVDT reading during this time, the photopolymerization was considered complete and the data were recorded for further analysis. Three replicates were measured for each composite mixture (dental paste).
2.3.2. Photopolymerization kinetics
Real time near infrared spectroscopy (RT-NIR) was employed to investigate the photopolymerization kinetics of Bis-GMA/TEGDMA dental resins containing varied mass fractions of the silanized HNTs. The photopolymerization rate and the degree of vinyl double bond conversion were measured. A Bruker Tensor-27 FT-IR spectrometer equipped with a liquid nitrogen-cooled mercury-cadmium-telluride (MCT) detector was used to carry out this study. During the RT-NIR measurements, the spectrometer was continuously purged with dry nitrogen gas, and the uncured resin was placed in a U-shaped Teflon mold with both sides covered by glass slides (note that glass is transparent in the NIR region between wavenumbers of 4000 and 6500 cm−1). The length and width of the mold were 4 mm, and the thickness was 2 mm. The glass slides were tightly attached to the mold using small metal clamps. A standard visible light curing unit (Maxima 480), purchased from the L. D. Caulk Company (Milford, DE), was placed directly above the sample holder. The absorption band of vinyl double bond (6100 to 6250 cm−1) were monitored in situ by RT-NIR at ambient condition for 5 min, with 4 scans/spectrum and 8 wavenumber resolution, using series run. In RT-NIR series run, infrared spectra were collected periodically (the time interval of 1 s was used in this study) during the photopolymerization of the specimens. The curing light was manually turned on at 8 s and turned off at 38 s.
2.3.3. Mechanical properties
A standard three-point flexural test (ASTM D 793) with a span of 20 mm was used to fracture the specimens at crosshead speed of 0.5 mm/min using a computer-controlled universal mechanical testing machine (QTESTTM/10, MTS Systems Co., USA). Mechanical properties of both Bis-GMA/TEGDMA dental resins (without conventional glass filler) and the corresponding composites (with the glass fillers) containing varied mass fractions of the silanized HNTs were acquired. The dimensions of Teflon mold for making the three-point flexural testing specimens were 2 mm × 2 mm × 25 mm. The specimens were photo-cured for 2 min on each side, and then carefully removed from the molds; all four sides of each specimen were carefully hand-polished with 2400 and 4000 grit silicon carbide paper and water coolant in a longitudinal direction. Five replicates were prepared for each sample.
2.3.4. Morphology
A Zeiss Supra 40 VP field-emission scanning electron microscope (SEM) was employed to examine morphologies of HNTs and representative fracture surfaces of Bis-GMA/TEGDMA dental resins/composites containing varied mass fractions of HNTs. A Hitachi H-7000 FA transmission electron microscope (TEM) was used to examine the structure of HNTs. Prior to SEM examination, the specimens were sputter-coated with gold to avoid charge accumulation. Prior to TEM examination, the silanized halloysite was dispersed in acetone with a mass fraction of ~1%, and the suspension was then mechanically stirred for 30 min at 400 rpm. Thereafter, the carbon-coated TEM grids were dipped into the suspension and quickly removed; the samples were then used for TEM examination after the acetone on the TEM grids evaporated.
2.3.5. Statistical analysis
The acquired data of volumetric shrinkage, flexural strength (SF), elastic modulus (EY), and work of fracture (WOF) were analyzed with one-way Analysis of Variance (ANOVA) using SPSS software, version 20 (SPSS, Chicago, IL). Significant differences were detected using the Tukey-HSD (honestly significant difference) test. References to significant differences were based on a probability of p < 0.05 unless otherwise stated.
3. Results and discussion
3.1. Morphology of halloysite/HNTs
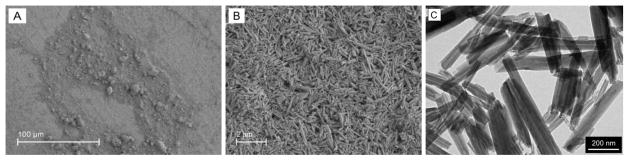
The naturally occurring halloysite mineral usually contains some impurities including dickite, kaolinite, and montmorillonite. These impurities were removed in the as-received halloysite powder. Two representative SEM images of the as-received halloysite powder are shown in Figs. 1A and 1B. It was evident that, the HNTs with diameters in tens of nanometers and lengths ranging from sub-microns to 1–2 microns stacked together as agglomerates/particles with sizes of several microns. A representative TEM image of the silanized HNTs is shown in Fig. 1C; the silanized HNTs were well-separated, indicating that the silanization of halloysite by MPTMS in acetone could effectively prevent/mitigate the agglomeration of HNTs.
Fig. 1.
(A) and (B): representative SEM micrographs (with different magnifications) of the as- received halloysite powder; (C): a representative TEM micrograph of the silanized HNTs.
3.2. Dispersion of silanized HNTs into dental matrix
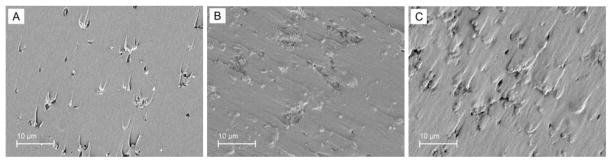
As shown in Fig. 1C, the silanized HNTs were well-separated and could be uniformly dispersed in acetone; however, it was still a challenge to achieve the high degree of separation and/or uniform dispersion of the silanized HNTs in Bis-GMA/TEGDMA. This is because the viscosity of Bis-GMA/TEGDMA is orders of magnitude higher than that of acetone, and its polarity is much lower. Hence, three methods (as described in the experimental section) were studied to identify the optimal condition/procedure for uniform dispersion of the silanized halloysite as well-separated HNTs into the dental matrix. Representative fracture surfaces of the photo-cured Bis-GMA/TEGDMA (mass ratio: 50/50) dental resins containing 2.5% (mass fraction) silanized HNTs are shown in Fig. 2. The images of A, B, and C in Fig. 2 represent the fracture surfaces acquired from the dispersion methods of A, B, and C, respectively.
Fig. 2.
Typical SEM micrographs of fracture surfaces of the photo-cured Bis-GMA/TEGDMA dental resins containing 2.5% (mass fraction) silanized HNTs. The images of A, B, and C were acquired from the samples prepared from the dispersion methods of A, B, and C, respectively.
As shown in Fig. 2A, the method A would result in smooth fracture surface, and the silanized HNTs in the Bis-GMA/TEGDMA dental resin existed predominantly as agglomerates, only a small amount of halloysite seemed to exist as individual HNTs. This suggested that direct dispersion of the silanized halloysite in dental monomers (even in the monomer of TEGDMA alone) could barely acquire the highly separated HNTs. In comparison, the fracture surfaces were rough and the degrees of separation and dispersion were much higher when the methods B and C were adopted; as shown in Figs. 2B and 2C, many individual HNTs were identifiable in the SEM images. These results suggested that the use of acetone during the dispersion process could greatly improve the degree of separation and uniform dispersion of the silanized HNTs. It is noteworthy that, there were still a few agglomerates found in Figs. 2B and 2C. This suggested that, unlike acetone, acetone solutions containing TEGDMA and/or Bis-GMA/TEGDMA might not be able to highly separate the silanized halloysite as individual HNTs. It is also possible that some separated HNTs might re-form agglomerates upon the removal/evaporation of acetone.
Compared to the method B, the method C appeared to be more effective since the fracture surface was rougher and more individual HNTs (rather than agglomerates) could be identified in the SEM image (Fig. 2C). The method C was thus adopted as the dispersion method to prepare specimens for the photopolymerization kinetics studies, the mechanical property measurements, and the volumetric shrinkage tests. It was also attempted to further improve the separation and/or dispersion of the silanized halloysite in the Bis-GMA/TEGDMA/HNT systems (prepared by the method C) by using a 200 W ultrasonic probe purchased from the Fisher Scientific Co. (Pittsburgh, PA); however, no distinguishable difference was identified.
3.3. Volumetric shrinkage
During the photopolymerization of dental methacrylate-based monomers, typical resins undergo volumetric shrinkages of 6–10%; while the highly filled dental composites still exhibit significant shrinkages of 2.6–7.1% [29]. The volumetric shrinkage is closely related to the methacrylate double bond conversion, which is a major factor influencing the properties of the cured composites [30]. For monomers with the same functionality, the higher the double bond conversion of monomers, the better the mechanical strength of cured resins; nevertheless, the concomitant increase of volumetric shrinkage would also lead to undesired consequences such as resin-filler de-bonding, internal stress development, and reduced marginal adaptation in dental restorations. It is still a technological challenge for dental composites to possess both low volumetric shrinkage and high double bond conversion at the same time.
Volumetric shrinkages for the Bis-GMA/TEGDMA dental composites containing varied mass fractions of silanized HNTs were measured, and the values are shown in Table 1. Note that each dental composite had the total filler mass fraction of 70%, while the filler was either the conventional dental glass powder (V-117-2707) alone or the combination with silanized HNTs. With increase of HNT percentage, the volumetric shrinkage of the dental composites increased. It was also noticed that the volumetric shrinkage of the dental composite containing 2.5% HNTs was 3.353%, indicating that the HNT mass fraction of 2.5% did not result in undesired large volumetric shrinkage of the Bis-GMA/TEGDMA dental composite. However, the volumetric shrinkage of the dental composite increased significantly to 4.807% when 5.0% HNT was incorporated. It is known that, the core structure of diphenyl isopropane in Bis-GMA provides high hydrophobicity while the two hydroxyl groups provide the hydrophilicity for the molecule; and the outer surface of HNTs is covered by hydroxyl groups and possesses chemical properties similar to SiO2. During the light curing process, as the mass fraction of HNTs reaches 5.0%, the HNTs have the tendency to agglomerate together; such a phenomenon can be observed from the SEM results (Figs. 5C and 5F). Additionally, Bis-GMA molecules and HNTs would be enforced tightly via intermolecular interactions (such as hydrogen bonding among hydroxyl groups). As a result, the high mass fraction of HNTs will lead to high volumetric shrinkage.
Table 1.
Values of volumetric shrinkage (%) for the Bis-GMA/TEGDMA dental composites containing varied mass fractions of silanized HNTs.
| Percentage of HNTs in dental composite* | 1st measurement | 2nd measurement | 3rd measurement | Average** | SD |
|---|---|---|---|---|---|
| 0% | 2.871 | 2.417 | 2.591 | 2.626b | 0.187 |
| 1% | 3.151 | 2.904 | 3.163 | 3.073b | 0.119 |
| 2.5% | 3.495 | 3.559 | 3.006 | 3.353b | 0.247 |
| 5% | 4.629 | 4.842 | 4.950 | 4.807a | 0.133 |
Each dental composite had the total filler mass fraction of 70%. The filler was either the conventional dental glass powder (V-117-2707) alone or the combination with silanized HNTs.
Lowercase letters indicate statistical differences (p < 0.05).
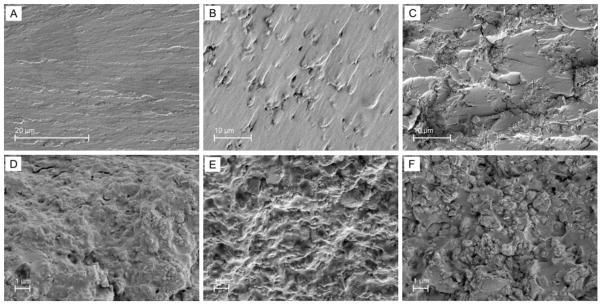
Fig. 5.
Representative fracture surfaces of three-point flexural specimens: (A) neat/unfilled Bis-GMA/TEGDMA resin, (B) Bis-GMA/TEGDMA resin filled with 2.5% (mass fraction) HNTs, (C) Bis-GMA/TEGDMA resin filled with 5.0% HNTs, (D) Bis-GMA/TEGDMA composite filled with 70% (mass fraction) glass filler of V-117-2707 alone, (E) Bis-GMA/TEGDMA composite filled with 2.5% HNTs and 67.5% glass filler, (F) Bis-GMA/TEGDMA composite filled with 5.0% HNTs and 65% glass filler.
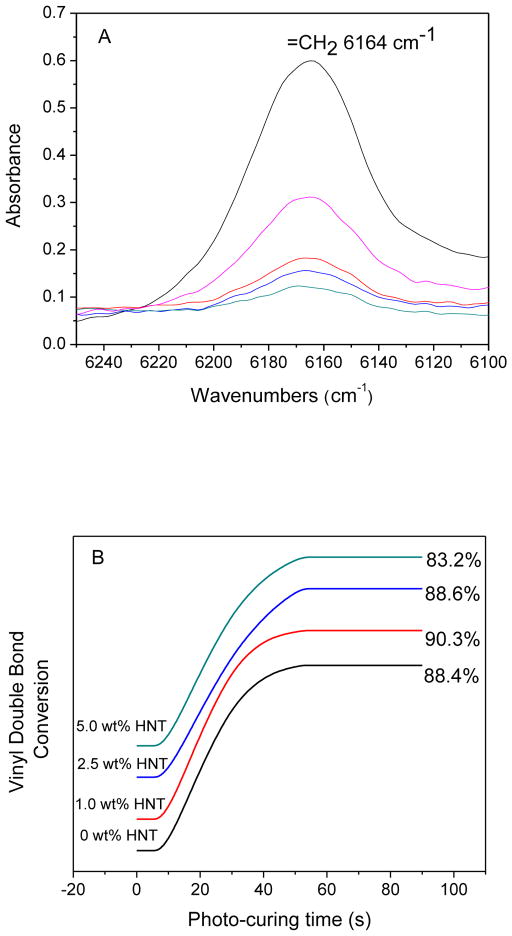
3.4. Photo-polymerization kinetics
Photo-polymerization kinetics was studied to examine whether the Bis-GMA/TEGDMA dental resins reinforced by HNTs could be appropriately photo-cured. The technique to monitor the photo-curing behaviors of dental methacrylate-based resins was demonstrated by Stansbury and Dickens [31]. During the measurement, the RT-NIR series run would provide valuable insights about the photopolymerization; meanwhile, the conversion of vinyl double bond in the resins could be monitored by the overtone band located in the range of 6100 to 6250 cm−1.
RT-NIR spectra of the Bis-GMA/TEGDMA dental resin filled with 2.5% HNTs during the photo-curing are shown in Fig. 3A. From top to bottom, the spectra were collected at the photo-curing times of 8, 23, 48, 63, and 90 s, respectively. The spectra indicated variations of the vinyl double bond absorbance in situ during the photopolymerization. After the curing light was turned on (i.e., the photopolymerization was initiated), the absorbance decreased quickly during the initial 48 s. Thereafter, the absorbance remained almost at the same level for the rest of the period. The absorbance band in Fig. 3A could be integrated to obtain the curing profiles. By using the absorbance of the vinyl double bond before photopolymerization as the reference, the curing profiles were converted to the degrees of vinyl double bond conversion, which is depicted in Fig. 3B. The tangent of each curve in Fig. 3B represents the photopolymerization rate at that particular time. Figs. 3A and 3B indicated that the Bis-GMA/TEGDMA dental resins filled with varied mass fractions (up to 5%) of HNTs could be photo-cured in ~50 s to achieve the vinyl double bond conversions in the range of ~83–90%. Hence, it was concluded that the addition of HNTs into Bis-GMA/TEGDMA did not appreciably vary the vinyl double bond conversion or the photo-polymerization rate.
Fig. 3.
(A): RT-NIR spectra of Bis-GMA/TEGDMA resin reinforced with 2.5% (mass fraction) HNTs. As the order from top to bottom, the spectra were collected at the photo-curing times of 8, 23, 48, 63, and 90 s, respectively. (B): Photo-curing profiles of Bis-GMA/TEGDMA dental resins filled with varied mass fractions of HNTs, the profiles are offset for clarity.
3.5. Mechanical properties
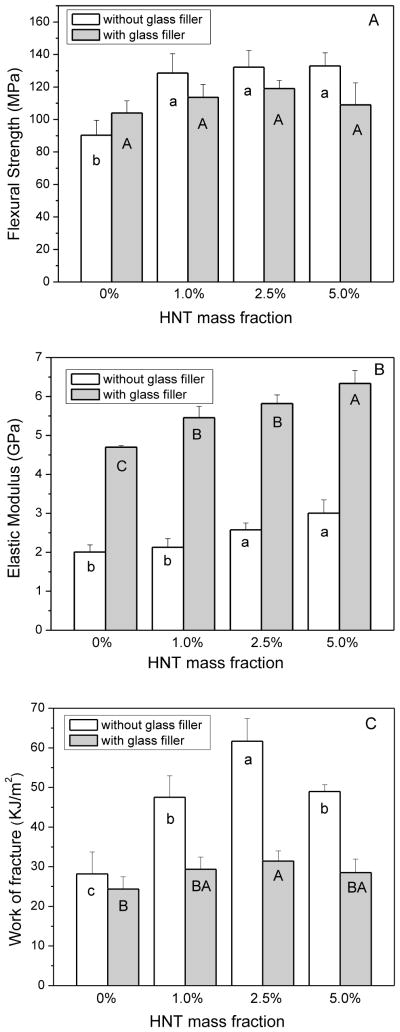
Flexural strength (SF), elastic modulus (EY), and work of fracture (WOF) of Bis- GMA/TEGDMA (mass ratio: 50/50) dental resins/composites containing varied mass fractions of the silanized HNTs were tested, and the results are showed in Fig. 4. The control sample was the resin/composite without HNTs. Each datum in the plots provides for the mean value of five replicates with the error bar representing one standard deviation.
Fig. 4.
The flexural strength (A), elastic modulus (B), and work of fracture (C) of Bis-GMA/TEGDMA dental resins/composites filled with varied mass fractions of silanized HNTs. Each datum is the mean value of five replicates, while the error bar represents one standard deviation. Letters indicate statistical differences (p < 0.05).
As shown in Fig. 4, the values of SF, EY, and WOF were all significantly increased upon the impregnation of small mass fractions of HNTs into the Bis-GMA/TEGDMA dental resins (without conventional glass filler). The values of SF, EY, and WOF for unfilled/neat resin were (90.4 ± 8.2) MPa, (2.0 ± 0.2) GPa, and (28.2 ± 3.0) KJ/m2, respectively. For the resin filled with 1.0% (mass fraction) HNTs, the values of SF, EY, and WOF were (128.6 ± 10.5) MPa, (2.1 ± 0.2) GPa, and (47.5 ± 4.7) KJ/m2, respectively. Thus, the SF was improved by 42.3%, the EY was improved by 5.0%, and the WOF was improved by 68.4%. For the resin filled with 2.5% HNTs, the measured values of SF, EY, and WOF were all increased significantly to (132.2 ± 9.0) MPa, (2.6 ± 0.2) GPa, and (61.7 ± 5.1) KJ/m2; and the improvements were 46.2%, 30.0%, and 118.8%, respectively. However, further increase of the HNT mass fraction did not improve the mechanical properties. For the resin filled with 5.0% HNTs, the respective SF, EY, and WOF values were (132.0 ± 6.9) MPa, (3.0 ± 0.3) GPa, and (48.9 ± 1.5) KJ/m2. These results indicated that the impregnation of small mass fractions (i.e., 1% and 2.5%) of the silanized HNTs into Bis-GMA/TEGDMA dental resin could substantially improve the mechanical properties. The following were the suggested reasons: (1) the HNTs, which were strongly bonded to the resin, strengthened the composites and resulted in the improvement of SF; (2) the modulus of HNTs was higher than that of the resin, leading to the improvement of EY; and (3) the HNTs, which were weakly bonded to the resin, could be separated and/or pulled out when the load was applied; this created frictional force that allowed the stress to transfer across matrix cracks, increasing the material resistance to fracture (i.e., WOF). Similar to the Bis-GMA/TEGDMA resins filled with small mass fractions of HNTs, the mechanical properties of the corresponding composites filled with both conventional glass filler and small mass fractions of silanized HNTs showed the same trend of improvements. The SF, EY, and WOF of the composites filled with 1% or 2.5% of silanized HNTs were higher than those of the control sample; nevertheless, the composites filled with 5% of the HNTs had SF and WOF values of (109.0 ± 5.9) MPa and (24.2 ± 2.4) KJ/m2, which were similar to those of the control sample. These results indicated that the effective reinforcement would not be achieved at high mass fraction of impregnation probably due to the formation of HNT agglomerates, which could be mechanical weak points (structural defects); and the presence of such agglomerates would reduce mechanical properties (especially strength) of the HNT reinforced dental composites.
Representative fracture surfaces of the Bis-GMA/TEGDMA dental resins (without the conventional dental glass filler of V-117-2707) containing 0% (i.e., neat resin), 2.5%, and 5.0% HNTs are shown in Figs. 5A, 5B, and 5C; while Figs. 5D, 5E, and 5F show the fracture surfaces of Bis-GMA/TEGDMA composites (with the glass filler of V-117-2707) containing 0%, 2.5%, and 5.0% HNTs. The total mass fraction of fillers in every composite was 70%; for example, Fig. 5E was acquired from the composite with 2.5% HNTs and 67.5% glass filler. The neat resin (Fig. 5A) fractured as typical ductile resin, and the fracture surface was smooth with oriented fracture lines resulted from the extension of crazings. In comparison, the fracture surface of the resin reinforced with 2.5% HNTs (Fig. 5B) was rough with no clearly identifiable fracture lines. These results suggested that the presence of HNTs could defect micro-cracks and effectively increase the resistance to applied force. When the crack finally broke away from the HNTs, a rough fracture surface was created, suggesting energy consumption during breaking. However, some voids/holes were identifiable on fracture surface of the resin/composite reinforced with 2.5% HNTs (Figs. 5B and 5E). These voids/holes were generated from the failure/fallout of the HNT particles. For the Bis-GMA/TEGDMA resin/composite reinforced with 5% HNTs, some agglomerations were formed, and could be obviously observed on the fracture surfaces (Figs. 5C and 5F). As explained before, the agglomerates could act as structural defects and weaken the materials. In summary, the impregnation of the silanized HNTs into Bis-GMA/TEGDMA dental resins/composites may result in two opposite effects: the reinforcing effect due to the highly separated and uniformly distributed HNTs, and the weakening effect due to the formation of HNT agglomerates/particles. This present study further suggested that mechanical properties of the resulting dental composites would be substantially higher than those of the commercially available composites, as long as the halloysite could be uniformly distributed in dental matrices as highly separated HNTs.
4. Conclusion
The aim of this study was to investigate the reinforcement of Bis-GMA/TEGDMA dental resins/composites with varied mass fractions of silanized halloysite/HNTs; the mechanical properties, as well as the volumetric shrinkage, degree of vinyl double bond conversion, and photopolymerization kinetics were studied. The results indicated that, impregnations of small mass fractions (e.g., 1% and 2.5%) of the silanized HNTs into the dental resins/composites significantly improved the mechanical properties; however, high mass fractions of impregnation (e.g., 5%) did not further improve the mechanical properties. The incorporation of HNTs into Bis-GMA/TEGDMA dental resins/composites could result in two opposite effects: the reinforcing effect due to highly separated and uniformly distributed HNTs, and the weakening effect due to formation of HNT agglomerates/particles. Since the uniform distribution of a small mass fraction of highly separated HNTs into dental resins/composites could effectively improve the mechanical properties, naturally occurring halloysite and/or HNTs may potentially be utilized as the nano-scaled reinforcement for dental composites.
Acknowledgments
This research was supported by the National Institute of Dental and Craniofacial Research (R03 DE16042) and by the Nanoscience and Nanoengineering Program at the South Dakota School of Mines and Technology. The authors are also grateful to the Esstech Co. for providing the silanized barium borosilicate glass powder (V-117-2707).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bowen RL. Dental filling material comprising vinyl-silane treated fused silica and a binder consisting of the reaction product of bisphenol and glycidyl methacrylate. U.S. Pa. 3,066,112. 1962
- 2.Bowen RL. Properties of a silica-reinforced polymer for dental restoration. J Am Dent Assoc. 1963;66:57–64. doi: 10.14219/jada.archive.1963.0010. [DOI] [PubMed] [Google Scholar]
- 3.Antonucci JM, Stansbury JW. Molecular designed dental polymer. In: Arshady R, editor. Desk reference of functional polymers: synthesis and application. American Chemical Society Publication; 1997. pp. 719–38. [Google Scholar]
- 4.Reed BB, Choi K, Dickens SH, Stansbury JW. Effect of resin composition of kinetics of dimethacrylate photopolymerization. Polym Prep. 1997;38(2):108–9. [Google Scholar]
- 5.Leinfelder KF, Sluder TB, Santos JFF, Wall JT. Five-year clinical evaluation of anterior and posterior restorations of composite resin. Oper Dent. 1980;12:52–78. [Google Scholar]
- 6.Lacy AM. A critical look at posterior composite restorations. J Am Dent Assoc. 1987;114:357–62. doi: 10.14219/jada.archive.1987.0077. [DOI] [PubMed] [Google Scholar]
- 7.Jordan RE, Suzuki M. Posterior composite restorations. J Am Dent Assoc. 1991;122:31–7. doi: 10.14219/jada.archive.1991.0321. [DOI] [PubMed] [Google Scholar]
- 8.O’Brien WJ. Dental materials and their selection. 3. Quintessence Publishing Co, Inc; 2002. [Google Scholar]
- 9.Corbin SB, Kohn WG. The benefits and risks of dental amalgam. J Am Dent Assoc. 1994;125:381–8. doi: 10.14219/jada.archive.1994.0055. [DOI] [PubMed] [Google Scholar]
- 10.Berry TG, Nicholson J, Troendle K. Almost two centuries with amalgam, where are we today? J Am Dent Assoc. 1994;125:392–9. doi: 10.14219/jada.archive.1994.0053. [DOI] [PubMed] [Google Scholar]
- 11.Kusy RP, Leinfelder KF. Pattern of wear in posterior composite restorations. J Dent Res. 1977;56(5):544–8. doi: 10.1177/00220345770560052101. [DOI] [PubMed] [Google Scholar]
- 12.Abell AK, Leinfelder KF, Turner DT. Microscopic observations of the wear of a tooth restorative composite in vivo. J Biomed Mat Res. 1983;17(3):501–7. doi: 10.1002/jbm.820170309. [DOI] [PubMed] [Google Scholar]
- 13.Grave AMH, Chandler HD, Wolfaardt JF. Denture base acrylic reinforced with high modulus fibre. Dent Mater. 1985;1:185–7. doi: 10.1016/s0109-5641(85)80015-4. [DOI] [PubMed] [Google Scholar]
- 14.Goldberg AJ, Burstone CJ. The use of continuous fiber reinforcement in density. Dent Mater. 1992;8:197–202. doi: 10.1016/0109-5641(92)90083-o. [DOI] [PubMed] [Google Scholar]
- 15.Giordano R. Fiber reinforced composite resin systems. Gen Dent. 2000;48(3):244–9. [PubMed] [Google Scholar]
- 16.Behr M. Comparison of three types of fiber-reinforced composite molar crowns on their fracture resistance and marginal adaptation. J Dent. 2001;29(3):187–96. doi: 10.1016/s0300-5712(01)00007-0. [DOI] [PubMed] [Google Scholar]
- 17.Xu HHK, Martin TA, Antonucci JM, Eichmiller FC. Ceramic whisker reinforcement of dental composite resins. J Dent Res. 1999;78:706–12. doi: 10.1177/00220345990780021101. [DOI] [PubMed] [Google Scholar]
- 18.Xu HHK. Dental composite resins containing silica-fused ceramic single-crystalline whiskers with various filler levels. J Dent Res. 1999;78:1304–11. doi: 10.1177/00220345990780070401. [DOI] [PubMed] [Google Scholar]
- 19.Xu HHK. Whisker-reinforced heat-cured dental resin composites: Effects of filler level and heat-cure temperature and time. J Dent Res. 2000;79:1392–7. doi: 10.1177/00220345000790060701. [DOI] [PubMed] [Google Scholar]
- 20.Xu HHK, Schumacher GE, Eichmiller FC, Antonucci JM. Strengthening composite resin restorations with ceramic whisker reinforcement. Pract Periodont Aesthet Dent. 2000;12:111–6. [PubMed] [Google Scholar]
- 21.Xu HHK, Quinn JB, Smith DT, Giuseppetti AA, Eichmiller FC. Effects of different whiskers on the reinforcement of dental resin composites. Dent Mater. 2003;19:359–67. doi: 10.1016/s0109-5641(02)00078-7. [DOI] [PubMed] [Google Scholar]
- 22.Joussein E, Petit S, Churchman J. Halloysite clay minerals – a review. Clay Minerals. 2005;40(4):383–426. [Google Scholar]
- 23.Hope E, Kittrick J. Surface tension and the morphology of halloysite. The American Mineralogist. 1964;49:859–63. [Google Scholar]
- 24.Vergaro V, Abdullayev E, Lvov YM, Zeitoun A, Cingolani R, Leporatti S. Cytocompatibility and uptake of halloysite clay nanotubes. Biomacromolecules. 2010;11:820–6. doi: 10.1021/bm9014446. [DOI] [PubMed] [Google Scholar]
- 25.Hughes AD, King MR. Use of naturally occurring halloysite nanotubes for enhanced capture of flowing cells. Langmuir. 2010;26(14):12155–64. doi: 10.1021/la101179y. [DOI] [PubMed] [Google Scholar]
- 26.Guimaraes L, Enyashin NA, Seifert G, Duarte AH. Structural, electronic, and mechanical properties of single-walled halloysite nanotube models. J Phys Chem C. 2010;114:11358–63. [Google Scholar]
- 27.Guimaraes L, Enyashin NA, Luciana, Frenzel J, Heine T, Duarte AH, Seifert G. Imogolite nanotubes: stability, electronic, and mechanical properties. ACS Nano. 2007;1:362–8. doi: 10.1021/nn700184k. [DOI] [PubMed] [Google Scholar]
- 28.Ye YP, Chen HB, Chan C-M. Interlaminar properties of carbon fiber composites with halloysite nanotube-toughened epoxy matrix. Compo Sci Technol. 2011;71(5):717–723. [Google Scholar]
- 29.Feilzer AJ, deGee AJ, Davidson CL. Curing contraction of composites and glass-ionomer cements. J Prosthet Dent. 1988;59:297–300. doi: 10.1016/0022-3913(88)90176-x. [DOI] [PubMed] [Google Scholar]
- 30.Ferracane JL, Greener EH. The effect of resin formulation on the degree of conversion and mechanical properties of dental restorative resin. J Biomed Mater Res. 1986;20:121–31. doi: 10.1002/jbm.820200111. [DOI] [PubMed] [Google Scholar]
- 31.Stansbury JW, Dickens DH. Determination of double bond conversion in dental resins by near infrared spectroscopy. Dent Mater. 2001;17:71–9. doi: 10.1016/s0109-5641(00)00062-2. [DOI] [PubMed] [Google Scholar]