Abstract
Introduction:
Rates of nicotine use are high in American Indians. Anxiety and depression tend to be associated with cigarette use, but the association of anxiety and depression with smokeless tobacco (ST) is less clear. We asked if panic disorder, major depression, and posttraumatic stress disorder (PTSD) are related to lifetime ST use in 2 American Indian tribes.
Methods:
Logistic regression analyses examined the association between lifetime panic disorder, major depression, and PTSD and the odds of lifetime ST use status after controlling for sociodemographic characteristics, smoking status, and alcohol use disorders in 1,506 Northern Plains and 1,268 Southwest tribal members.
Results:
Odds of lifetime ST use was 1.6 times higher in Northern Plains tribal members with a lifetime history of PTSD after controlling for sociodemographic variables and smoking (95% CI: 1.1, 2.3; p = .01). This association remained significant after further adjustment for panic disorder and major depression (odds ratio [OR] = 1.5; 95% CI: 1.0, 2.2; p = .04) but was diminished after accounting for alcohol use (OR = 1.3; 95% CI: 0.9, 1.9; p = .23). In the Southwest, lifetime psychiatric disorders were not associated with lifetime ST use status. Increasing psychiatric comorbidity was significantly linked to increased odds of ST use in both tribes.
Conclusions:
This study is the first to examine psychiatric conditions and lifetime ST use in a large, geographically diverse American Indian community sample. Although approximately 30% of tribal members were lifetime users of ST, the association with lifetime psychiatric disorders was not as strong as those observed with cigarette smoking. Understanding shared mechanisms between all forms of tobacco use with anxiety and depressive disorders remains an important area for investigation.
Introduction
The use of smokeless tobacco (ST) products confers greater risk for several oral health problems, such as cancer, leukoplakia, gingivitis, and periodontitis (Critchley & Unal, 2003; Savitz, Meyer, Tanzer, Mirvish, & Lewin, 2006) and adverse pregnancy outcomes (England et al., 2003) relative to nonusers. Although ST has also been linked to diseases of the cardiovascular system (Bolinder, Alfredson, Englund, & de Faire, 1994), this association is not as well established as cigarette smoking (Rodu, 2011; Savitz et al., 2006). Reducing the incidence of preventable diseases through improved tobacco control strategies was a primary goal of Healthy People 2010 (U.S. Department of Health and Human Services, 2002). Unfortunately, population trends in ST use by 2005 noted that reducing its prevalence to 0.4% in the U.S. population was not going to be reached (Nelson et al., 2006). In 2005, the prevalence of current ST use was 2.3%, with rates considerably higher among men (4.5%) than women (0.2%; Centers for Disease Control and Prevention, 2006). In the 2009 Behavioral Risk Factor and Surveillance System survey, current ST use across all 50 States ranged from 1.3% to 9.1% (Centers for Disease Control and Prevention, 2010). Although males remain the primary consumers of ST (Centers for Disease Control and Prevention, 2010), other demographic factors, such as younger adults, lower education, and rural areas are also associated with higher rates of usage (Bell et al., 2009; Howard-Pitney & Winkleby, 2002; Marcus, Crane, Shopland, & Lynn, 1989; Nelson et al., 2006).
Caucasians and American Indians have the highest rates of cigarette and ST use relative to all other racial/ethnic groups (Caraballo, Yee, Gfroerer, & Mirza, 2008; Gilliland, Mahler, & Davis, 1998; Nelson et al., 2006; Redwood et al., 2010). The National Survey on Drug Use and Health found rates of current ST use highest among American Indians (7.1%), followed by Whites (4.1%), Native Hawaiians or Other Pacific Islanders (2.9%), and African Americans (1.4%; Substance Abuse and Mental Health Services Administration, 2009). The use of commercial, nonceremonial tobacco products is particularly high among American Indians (American Lung Association, 2006; Centers for Disease Control and Prevention, 1998). Surprisingly, few studies have examined sociodemographic correlates of ST use in this population. Among rural American Indians residing in New Mexico, approximately 25% of 1,266 respondents were classified as lifetime users of ST, with men, younger age, and less education associated with current use (Gilliland et al., 1998). In a community sample of American Indians drawn from North Carolina, older age and lower education were significant predictors of ST use (Spangler et al., 2001). A recent large-scale study of American Indians and Alaska Natives found male gender, less education, and speaking their native tongue at home to be factors associated with current ST use (Redwood et al., 2010). American Indian ethnicity was also the only racial/ethnic group significantly associated with ever using ST products (Bell et al., 2009). Lower educational attainment and male gender appear to be consistent correlates with ST use in both majority and American Indian populations. However, the disproportionately high rates of ST in American Indians suggest that other factors need to be considered.
Symptoms and disorders of anxiety and depression have been found to be significantly related to cigarette smoking in both majority (Wilhelm, Wedgwood, Niven, & Kay-Lambkin, 2006; Ziedonis et al., 2008) and American Indian populations (Sawchuk et al., 2011). The association of anxiety and depression with ST is not as well established (Goodwin, Zvolensky, & Keyes, 2008). ST users are more likely to report concurrent depressive symptoms in both adult (Rouse, 1989) and adolescent (Coogan, Geller, & Adams, 2000; Tercyak & Audrain, 2002) samples relative to nonusers. The odds of ST use among American Indian adolescents with a history of externalizing anger, characterized by yelling and fighting, is approximately three times higher than those without a history of anger-related problems (Kerby, Brand, & John, 2003). Some studies suggest that nicotine dependence status influences the ST–psychiatric disorders association. Among individuals with current nicotine dependence, the odds of any 12-month anxiety disorder was nearly two times higher among ST users compared with those who were not currently using cigarettes or ST products (Goodwin et al., 2008). However, ST use was not associated with any current mental disorder among those without current nicotine dependence (Goodwin et al., 2008). Although ST use is high among American Indians (Redwood et al., 2010), it is not known whether ST is significantly associated with anxiety and depression in this population. American Indians represent a unique sample to further investigate ST use given that lifetime anxiety disorders are nearly 1.5 times higher than lifetime depressive disorders among tribal members (Beals et al., 2005). Furthermore, the lifetime prevalence of posttraumatic stress disorder (PTSD) is approximately two times greater than Caucasians, yet lifetime rates of major depression are comparable (Beals et al., 2005). Hence, studying ST rates among American Indians with anxiety and depression may yield unique associations not observed in other racial/ethnic groups.
Behavioral models propose anxiety sensitivity and negative affectivity, and stimulus regulation may increase a person’s susceptibility to nicotine use (Zvolensky, Sachs-Ericsson, Feldner, Schmidt, & Bowman, 2006) and failed quit attempts (Brown, Kahler, Zvolensky, Lejuez, & Ramsey, 2001), given their reinforcing function for regulating uncomfortable physiologic and emotional states. Biologic factors, such as exaggeration of the hypothalamic-pituitary-adrenal axis, have been implicated as a potentially shared neurobiological mechanism involved in panic disorder (Abelson, Khan, & Liberzon, 2007), PTSD (Rasmusson, Vythilingam, & Morgan, 2003), major depression (Pariante & Lightman, 2008), and nicotine use (Rohleder & Kirschbaum, 2006). Anxiety disorders and depression often co-occur in epidemiologic studies, including American Indian samples (Beals et al., 2005), and rates of nicotine dependence appear to increase with greater psychiatric comorbidity (Grant, Hasin, Chou, Stinson, & Dawson, 2004). The synergistic effects of behavioral and biological factors invite further inquiry as they may contribute to both the mediation and moderation of the psychiatric disorder–nicotine use relationship in different populations (Ziedonis et al., 2008).
This study explored the relationships between lifetime anxiety disorders and major depression with lifetime ST use among American Indians residing in the Northern Plains and Southwest regions. Our primary goals were to (a) describe rates of lifetime ST use among respondents with a lifetime history of panic disorder, major depression, PTSD, and alcohol abuse/dependence; (b) determine if panic disorder, major depression, and PTSD are independently associated with lifetime ST use after accounting for sociodemographic factors and lifetime alcohol use disorders; and (c) ascertain if comorbid panic disorder, major depression, PTSD, and alcohol use increases the odds ratio (OR) of lifetime ST use risk beyond its association with individual psychiatric disorders.
Methods
Study Design, Sample, and Procedures
The primary objective of the American Indian Service Utilization, Psychiatric Epidemiology, Risk and Protective Factors Project (AI-SUPERPFP) was to estimate the prevalence of psychiatric disorders and health service use among tribal members residing on two closely related Northern Plains reservations and one in the Southwest. The AI-SUPERPFP was patterned after the National Comorbidity Survey (Kessler et al., 1994) in order to allow for comparisons with other large-scale epidemiologic studies. A sample of individuals listed on tribal rolls (the legal record of tribal membership) that were between the ages of 15 and 54 in June 1997 and lived on or within 20 miles of their reservation at the time of the study were selected for participation. The total sample size for the Northern Plains cohort was 1,638, and 1,446 for the Southwest tribe. The sample was grouped by age (four strata) and sex (two strata) using stratified random sampling procedures (Cochran, 1977). Sample weights were used to account for differential probabilities of selection and nonresponse within strata (Kish, 1965). Considerable efforts were made by the AI-SUPERPFP team during the project development phase to involve participating communities in constructing content-valid, culturally relevant interview questions. A structured, comprehensive interview was administered by tribal members, intensively trained in research methods, and assisted by laptop computers. Extensive quality control efforts were made to ensure all phases of the interview process were conducted in a standardized, reliable manner. Data collection occurred between July 1997 and August 1999. The AI-SUPERPFP obtained the necessary tribal and university approvals, and written informed consent was obtained from each participant.
The AI-SUPERPFP study design and sampling methods are described in greater detail elsewhere (Beals, Manson, Mitchell, Spicer, & the AI-SUPERPFP Team, 2003; http://www.ucdenver.edu/academics/colleges/PublicHealth/research/centers/CAIANH/NCAIANMHR/ResearchProjects/Pages/AI-SUPERPFP.aspx). For our analyses, only participants who had complete data on lifetime ST history and lifetime psychiatric disorders were included.
Measures
Demographics
Sociodemographic information included sex, age, marital status, education, and employment status. Age was measured continuously in years. Marital status was dichotomized as currently married or cohabitating versus all other categories. Education was categorized as attending either less than 12 years of school or 12 years or more. Employment status was dichotomized as working full/part time versus all other categories.
Smokeless Tobacco History
Lifetime ST status was defined as those participants who reported using chewing tobacco products for 1 or more years. Participants were asked “Have you ever used chewing tobacco?” and “About how many years did you use chewing tobacco in total?” Participants who responded “yes” to the former and 1 or more years to the latter question were classified as lifetime ST users. The interview did not assess for frequency or amount of ST use during those years in which participants were actively using ST. The preface to the tobacco section in the AI-SUPERPFP specified the assessment of only commercial, nonceremonial ST products.
Cigarette Smoking History
Participants were classified as lifetime smokers if they responded “yes” to the following question: “Have you smoked at least 5 packs of cigarettes (100 cigarettes) in your entire life?”
Psychiatric Disorders
A version of the University of Michigan Composite International Diagnostic Interview was adapted for use in the AI-SUPERPFP (AI-SUPERPFP-CIDI) to assess lifetime panic disorder, major depression, and alcohol abuse/dependence according to the Diagnostic and Statistical Manual IV criteria. PTSD was diagnosed using a modified version of the World Health Organization Composite International Diagnostic Interview (CIDI; World Health Organization, 1990) and updated to Diagnostic and Statistical Manual IV standards. The PTSD module was drawn from the American Indian Vietnam Veterans Project (Beals et al., 2002) as it allowed for the assessment of up to three traumatic events. Cumulative trauma exposure is common in this population, and the CIDI only allowed for the assessment of Criteria B, C, and D for only one traumatic event (Beals et al., 2002). Generalized anxiety disorder was not included in the current analyses given its low prevalence in the AI-SUPERPFP, especially in the Northern Plains tribe (1.7%; Beals et al., 2005). Furthermore, social anxiety disorder, obsessive-compulsive disorder, and specific phobia were not assessed in the AI-SUPERPFP study.
Statistical Analyses
Descriptive statistics included means and CI for continuous variables and percentages for categorical variables. We compared demographic characteristics and prevalence of lifetime panic disorder, major depression, PTSD, and alcohol use disorders according to lifetime ST use status (users vs. nonusers) across each tribe. Logistic regression analyses examined the strength of the association between the individual psychiatric disorders and the odds of lifetime ST use by fitting three separate models adjusted for age, sex, education, marital status, employment status, and smoking status. We then estimated each psychiatric disorder’s association with ST after adjusting for demographic variables, smoking status, and the two remaining psychiatric disorder diagnoses. We constructed a final model to estimate the association between the individual psychiatric disorders and ST after adjusting for demographics, smoking status, comorbid psychiatric conditions, and lifetime alcohol use disorder diagnosis. Results were reported using OR and 95% CI.
Next, regression analyses examined the association of psychiatric comorbidity and the odds of ST in the two tribes. We estimated the lifetime ST use OR for groups defined as having 0, 1, 2, and 3 or more psychiatric disorders, after adjusting for demographic factors. Participants with no psychiatric disorders were the reference group for all comparisons. In addition, we fit a similarly adjusted logistic model to allow a test for trend in the odds of lifetime ST with the increasing number of comorbid psychiatric diagnoses. All statistical tests were two-sided adjusted Wald tests. We conducted analyses with Stata 10 for Windows (Stata Corporation, College Station, TX) using “svy” commands to accommodate the weights for complex sampling and survey nonresponse.
Results
Sample Description
Three-hundred ten participants (10%) were excluded from analyses due to incomplete data on ST history or lifetime psychiatric disorders. Excluded and included participants had similar sociodemographic characteristics, with the exception of age. Excluded participants were, on average, 2.2 years older than included participants (p < .01). The analytic sample included 1,506 Northern Plains participants and 1,268 Southwest participants.
Table 1 presents participant characteristics by tribal region and lifetime ST use status. The prevalence of lifetime ST use was similar in the Northern Plains and Southwest tribes (31% vs. 30%). ST users in the Northern Plains were younger than nonusers (p < .01). Conversely, in the Southwest, users were older than nonusers (p < .01). In both tribes, a lower proportion of ST users were female (p < .01) than nonusers. ST users from both the Northern Plains and Southwest tribes were more likely to be married or living with their partner (p NP = .02, p SW < .01) and employed (p NP = .02, p SW < .01). Lifetime ST users in both tribes were also more likely to report lifetime cigarette use in comparison with nonusers (p < .01). Alcohol use disorder was more prevalent among lifetime ST users than nonusers in both locations (p < .01).
Table 1.
Participant Characteristics by Region and Lifetime Smokeless Tobacco Use Statusa
| Characteristic | Northern plains tribe N = 1,506b | Southwest tribe N = 1,268b | ||
| Lifetime users | Nonusers | Lifetime users | Nonusers | |
| Demographic and health | ||||
| Total, % | 31 | 69 | 30 | 70 |
| Age, mean years (SD) | 30 (8)** | 35 (12) | 36 (10)** | 33 (12) |
| Female, % | 40** | 56 | 31** | 67 |
| Attended ≥ 12 years of school, % | 33 | 30 | 40 | 39 |
| Married or living with partner, % | 56* | 49 | 67** | 56 |
| Currently employed, % | 61* | 54 | 67** | 58 |
| Lifetime smoker, % | 76** | 67 | 40** | 30 |
| Lifetime psychiatric diagnoses | ||||
| Panic disorder, % | 3 | 2 | 5 | 4 |
| Major depressive disorder, % | 9 | 8 | 11 | 10 |
| Posttraumatic stress disorder, % | 15 | 14 | 16 | 16 |
| Alcohol use disorder, % | 46** | 30 | 38** | 18 |
| Number of psychiatric diagnoses | ||||
| None, % | 78 | 81 | 75 | 77 |
| 1, % | 18 | 15 | 20 | 17 |
| 2, % | 4 | 4 | 5 | 5 |
| 3 or more, % | <1 | <1 | 1 | 1 |
Note. aSmokeless tobacco users defined as individuals who have used smokeless tobacco for at least 1 year in their lifetime.
Numbers shown here are actual counts. Survey-weighted sample sizes were 1,489 Northern Plains participants and 1,274 Southwest participants.
*p < .05; **p < .01.
Panic Disorder, Major Depression, PTSD, and Smokeless Tobacco Status
Panic Disorder and Major Depression
Panic disorder and major depression were not associated with lifetime ST use in either the Northern Plains or Southwest tribes (Table 2).
Table 2.
Adjusted Lifetime Smokeless Tobacco Usea O Rs and 95% CI According to Psychiatric Diagnosis and Tribe
| Basic modelb | Psychiatric comorbidity modelc | Psychiatric/alcohol comorbidity modeld | |
| OR (95% CI) | OwR (95% CI) | OR (95% CI) | |
| Northern Plains tribe | |||
| Panic disorder | 1.9 (0.8, 4.2) | 1.6 (0.7, 3.8) | 1.6 (0.7, 3.6) |
| Major depression | 1.4 (0.9, 2.2) | 1.2 (0.8, 2.0) | 1.1 (0.7, 1.7) |
| PTSD | 1.6* (1.1, 2.3) | 1.5* (1.0, 2.2) | 1.3 (0.9, 1.9) |
| Southwest tribe | |||
| Panic disorder | 1.3 (0.7, 2.3) | 1.2 (0.6, 2.1) | 1.1 (0.6, 2.1) |
| Major depression | 1.3 (0.9, 2.1) | 1.3 (0.8, 2.0) | 1.2 (0.8, 1.9) |
| PTSD | 1.2 (0.8, 1.8) | 1.2 (0.8, 1.7) | 1.1 (0.7, 1.6) |
Note. OR = odds ratio; CI = confidence interval; PTSD = posttraumatic stress disorder.
Smokeless tobacco users defined as individuals who have used smokeless tobacco for at least 1 year in their lifetime.
Sociodemographic/health factors include age, sex, education, marital status, employment status, and smoking status.
Adjusted for sociodemographic/health factors and the two remaining lifetime psychological disorder diagnoses.
Adjusted for sociodemographics/health, other lifetime psychiatric diagnoses, and alcohol use disorder diagnosis.
*p < .05; **p < .01.
PTSD
As shown in Table 2, the odds of lifetime ST use in the Northern Plains were 1.6 times higher among participants with PTSD compared with those without PTSD after adjustment for sociodemographic characteristics and lifetime smoking status (95% CI: 1.1, 2.3; p = .01). This association remained significant after further adjustment for panic disorder and major depression (OR = 1.5; 95% CI: 1.0, 2.2; p = .04). However, after adjustment for the diagnosis of an alcohol use disorder, the association between lifetime ST use and PTSD was attenuated (OR = 1.3) and no longer significant (95% CI: 0.9, 1.9; p = .23). In the Southwest, lifetime ST use was not significantly associated with PTSD.
Psychiatric Comorbidity and Smokeless Tobacco Use Status
Figure 1 depicts the lifetime ST use OR associated with the number of comorbid psychiatric diagnoses, adjusted for demographic factors. For each tribe, we found a significant trend for increased odds of ST use with the increasing number of comorbid psychiatric diagnoses (p trend’ < .001). The odds of lifetime ST use peaked among tribal members with two psychiatric disorders.
Figure 1.
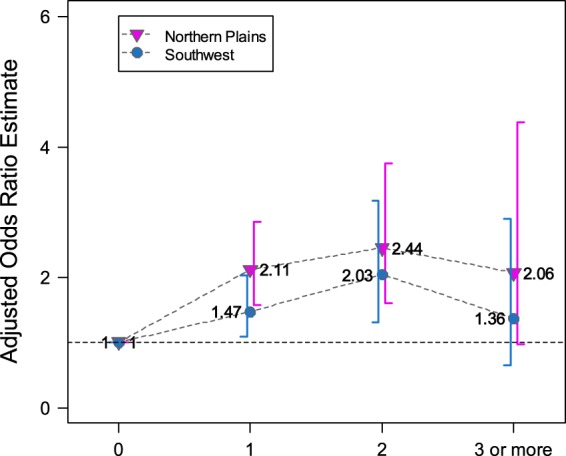
Adjusted odds ratios and 95% CI for lifetime smokeless tobacco use according to the number of comorbid lifetime psychiatric disorders. Data are adjusted for age, sex, education, marital status, employment status, and lifetime smoking status. p < .001 for the test for trends in odds ratios as the number of comorbid psychiatric disorders increases among Northern Plains and Southwest tribes.
Discussion
Approximately 30% of Northern Plains and Southwest tribal members were identified as lifetime ST users. A comparable study investigating lifetime regular users of ST, defined as those reporting ever using chewing tobacco or snuff and endorsed an age in which they used these substances “fairly regularly,” found a lifetime rate of 10.7% among non-Hispanic Whites, Blacks, and Mexican-American men (Howard-Pitney & Winkleby, 2002). Northern Plains and Southwest tribal members in our sample had a nearly threefold increase in lifetime ST rates. Additional signal detection analyses noted that the highest risk group for lifetime regular ST use was among rural, low-income White and Black men at 33% (Howard-Pitney & Winkleby, 2002), a rate comparable to our study. Likewise, lifetime cigarette smoking rates were high among lifetime ST users in both the Northern Plains and Southwest tribes, relative to nonusers. Previous studies have also reported significantly higher rates of cigarette smoking among those who use ST products relative to those who do not use ST (Tomar, Alpert, & Connolly, 2010). A considerable body of research has established the increased odds of cigarette smoking among those with histories of anxiety and depression (Grant et al., 2004; Wilhelm et al., 2006; Ziedonis et al., 2008). Although studies examining ST use and psychiatric disorders are sparse, these associations appear weaker and less reliable than those observed in cigarette smoking (Goodwin et al., 2008).
Consistent with other populations (Centers for Disease Control and Prevention, 2006; Howard-Pitney & Winkleby, 2002; Marcus et al., 1989; Nelson et al., 2006), males in both tribes were significantly more likely than females to use ST products. The observation that 40% of women in the Northern Plains and 31% in the Southwest were classified as lifetime ST users is high. Among U.S. women, the percentage of current users of any tobacco product (cigarettes or ST) is the highest among American Indian/Alaska Natives (37.9%), followed by Native Hawaiians/Pacific Islanders (27%), Whites (26.6%), Blacks (25.4%), Hispanics (18.2%), and Asians (8.4%). High rates of ST use among American Indian women may be partially reflective of the cultural acceptance of tobacco and use of various tobacco products in ceremonial functions (Henderson, Jacobsen, Beals, & the AI-SUPERPFP Team, 2005; Hodge & Struthers, 2006). Further assessment of gender-specific attitudes and beliefs about tobacco use may help clarify additional reasons that underlie differential consumption rates across racial/ethnic groups.
In contrast to other studies, including those with American Indians and Alaska Natives (Redwood et al., 2010), education level did not differentiate users from nonusers in either tribe. Age was the only demographic characteristic associated with ST use that differed between the tribes. Users were more likely to be younger in the Northern Plains, which is a common pattern among lifetime (Bell et al., 2009; Howard-Pitney & Winkleby, 2002) and current ST users (Marcus et al., 1989; Nelson et al., 2006; Redwood et al., 2010). In contrast, lifetime ST use was associated with older age among those residing in the Southwest. Interestingly, a previous study on correlates of cigarette smoking in the AI-SUPERPFP found that current smokers in the Southwest tended to be younger than nonsmokers, yet no age differences were found between smokers and nonsmokers in the Northern Plains (Henderson et al., 2005). It is unclear if age by tribe differences in lifetime ST use and cigarette smoking represents a meaningful finding or if these patterns can be replicated in other American Indian cohorts. The tribes may vary in terms of age specific or generational beliefs and attitudes about different modes of tobacco administration. Age of ST usage does appear to play a role in predicting later cigarette smoking and the likelihood of tobacco abstinence. Specifically, younger males who regarded themselves as regular users of ST, but were not smoking cigarettes, were three times more likely to be smoking cigarettes 4 years later in comparison with the same-aged individuals who were not using ST products (Tomar, 2003). Further, younger age of initiating ST use tends to be inversely related to abstinence 1 year after bupropion sustained release treatment (Ebbert, Glover, Shinozaki, Schroeder, & Dale, 2008). Future studies with American Indians should assess for age of initiating ST use as this may be related to latter onset cigarette use, success of quit attempts, or responsiveness to cessation treatments.
An examination of the psychiatric disorder prevalence rates revealed no differences between users and nonusers in regards to panic disorder, major depression, and PTSD in both tribes. In contrast to cigarette smoking, substantially less research has investigated ST rates among individuals with anxiety and depressive disorders. Only a single study has reported higher rates of any 12-month anxiety disorder among individuals with current ST nicotine dependence (Goodwin et al., 2008). Rates of anxiety and depressive disorders are approximately 1.5–3.0 times higher among smokers relative to nonsmokers (Johnson & Breslau, 2006; Wilhelm et al., 2006), with the prevalence of psychiatric disorders continuing to increase among those individuals who are nicotine dependent (Goodwin et al., 2008; Ziedonis et al., 2008). Perhaps, significant associations between ST with anxiety and depressive disorders only emerge among those who are nicotine dependent. A further analysis of nicotine dependence among American Indians would appear warranted in order to assess this hypothesis and determine if findings of Goodwin et al. (2008) can be replicated.
Lifetime alcohol use disorders were significantly more common among users relative to nonusers in both the Northern Plains and Southwest tribes. Among a sample of female military recruits, daily or near-daily alcohol consumption was significantly associated with an increased likelihood of ST use (Vander Weg et al., 2005). Although comparable studies investigating the ST–alcohol link are limited, the high comorbidity between nicotine and alcohol use disorders has been well established. The majority of these studies have either examined cigarette smoking alone (Durazzo, Gazdzinski, & Meyerhoff, 2007; Jensen et al., 2003) or combined ST with all other forms of nicotine administration (Grant et al., 2004). Hence, future research may need to isolate ST from other forms of tobacco administration in an effort to better understand its unique association with alcohol use.
Logistic regression analyses with each psychiatric disorder on lifetime ST risk revealed differential findings between the tribes. In the Northern Plains, only PTSD had a significant association with lifetime ST use after adjusting for relevant sociodemographic variables, including lifetime cigarette smoking. This association was lost, however, after controlling for lifetime alcohol use disorders. Increased risk for ST use among those with PTSD but not major depression is generally consistent with previous studies (Goodwin et al., 2008). No significant associations emerged from the regression analyses with the Southwest tribe, underscoring the complexity of studying these relationships both within and across tribes. Psychiatric comorbidity showed a significant trend-level increase in the odds of ST use among both tribes. However, the rates were modest and actually peaked at two disorders before declining when three or more psychiatric disorders were present. Future research may wish to assess other cultural, demographic, biological, health, familial, and social factors that may mediate and moderate any latent association between psychiatric disorders and ST use among American Indians.
This study has several limitations. First, our operationalization of lifetime ST use was liberal which could have inflated our prevalence rates. Considerable variability is evident with how ST use has been surveyed, making comparisons with other samples challenging. For example, some studies have assessed ST based on ever using chewing tobacco or snuff at least 20 times in their lifetime (Centers for Disease Control and Prevention, 2006; Goodwin et al., 2008; Nelson et al., 2006; Redwood et al., 2010). Data from the Current Population Survey (Mumford, Levy, Gitchell, & Blackman, 2006) and the National Health Survey (Nelson et al., 2006) even showed changes in the wording of the lifetime ST use questions across repeated sampling periods. Our study also assessed only chewing tobacco use, whereas other studies have asked about both chewing tobacco and snuff together (Redwood et al., 2010) or chewing tobacco and snuff separately (Nelson et al., 2006). Differences in how tobacco use questions have been asked are also apparent in the cigarette smoking literature (Ziedonis et al., 2008). Second, we did not assess how much or how frequently tribal members used ST in their lifetime. A more refined measurement of both the quantity and frequency of ST could help determine if a dose-dependent relationship exists with psychiatric disorder status or if nicotine dependence is more strongly related to anxiety and depressive disorders. Defining cigarette smoking in terms of pack-years has been an accepted method of assessing cumulative exposure to tobacco use. Such a shared metric for lifetime ST is not readily available. Measuring quantity and frequency of ST use would provide a more accurate assessment of exposure risk than the generic “ever use” construct (Bell et al., 2009).
Third, data from the AI-SUPERPFP were collected between 1997 and 1999, and therefore, trends in ST use among the tribes may have changed over time. Fourth, our cross-sectional design does not permit inferences about the direction of the associations. Only recently have studies been able to speculate on the directionality of the relationship between psychiatric disorders and smoking risk (Ziedonis et al., 2008), although these relationships are not well established among consumers of ST. Fifth, our study assessed only lifetime diagnoses of anxiety and depression, rather than dimensional symptom measures. Other studies have found significant associations between ST use and symptoms of negative affectivity, such as depression (Rouse, 1989) and anger (Kerby et al., 2003). Finally, these results cannot be generalized to all American Indians as considerable diversity exists in geography, culture, urbanization, and availability of tobacco cessation programs.
The association between ST use and psychiatric disorders does not appear to be nearly as robust as the relationship between cigarette use with anxiety and depressive disorders. It is possible that ST does not carry the same reinforcement value (e.g., tension reduction, enjoyment) that cigarette smoking may confer among those who struggle with anxiety and depression. Anxiety and depressive disorders are common among American Indian communities, and use of all tobacco products can be frequent. Shared biological, environmental, and behavioral mechanisms may underlie tobacco use, anxiety, and depression, and illuminating these mechanisms may help inform successful tobacco quit programs. It remains questionable as to whether the presence of an anxiety or depressive disorder among ST users has any bearing on the ability to successfully quit. Only a single study to date found that ST users with a history of depression were more likely those without depression to continue using 1 year after participating in a pharmacologic trial (Ebbert et al., 2008). Replication of these findings is clearly warranted. The public health impact of tobacco use remains a serious issue, especially in the American Indian community where rates of usage are disproportionately high (Steele, Cardinez, Richardson, Tom-Orme, & Shaw, 2008). Further efforts are needed to develop and disseminate effective cessation programs to these historically underserved tribal communities.
Funding
This work was supported by the National Institutes of Health/National Institute on Aging (P30 AG15297 to S.M.M.), Agency for Healthcare Research and Quality (P01 HS10854 to S.M.M.), the National Institutes of Health/National Center for Minority Health and Health Disparities (P60 MD000507 to S.M.M.), the National Institutes of Health/National Institute of Mental Health (P01 MH42473 and R01 MH48174 to S.M.M.), and the National Cancer Institute (SR01 CA126620 to D.B.).
Declaration of Interests
C.N.S., P. R.- B., C.N. , A.B. , J.G. , S.M.M. , D.B. , and the members of the AI-SUPERPFP Team declare that they have no competing interests.
Acknowledgments
The AI-SUPERPFP team includes Janette Beals, Cecelia K. Big Crow, Buck Chambers, Michelle L. Christensen, Denise A. Dillard, Karen DuBray, Paula A. Espinoza, Candace M. Fleming, Ann Wilson Frederick, Joseph Gone, Diana Gurley, Lori L. Jervis, Shirlene M. Jim, Carol E. Kaufman, Ellen M. Keane, Suzell A. Klein, Denise Lee, Monica C. McNulty, Denise L. Middlebrook, Laurie A. Moore, Tilda D. Nez, Ilena M. Norton, Douglas K. Novins, Theresa O’Nell, Heather D. Orton, Carlette J. Randall, Angela Sam, James H. Shore, Sylvia G. Simpson, Paul Spicer, and Lorette L. Yazzie.
References
- Abelson JL, Khan S, Liberzon I, Young EA. HPA axis activity in patients with panic disorder: Review and synthesis of four studies. Depression and Anxiety. 2007;24:66–76. doi: 10.1002/da.20220. doi:10.002/da.20220. [DOI] [PubMed] [Google Scholar]
- American Lung Association. Estimated prevalence and incidence of lung disease report. Washington, DC: Author; 2006. [Google Scholar]
- Beals J, Manson SM, Mitchell CM, Spicer P the American Indian Service Utilization, Psychiatric Epidemiology, Risk and Protective Factors Project Team. Cultural specificity and comparison in psychiatric epidemiology: Walking the tightrope in American Indian research. Culture, Medicine, and Psychiatry. 2003;27:259–289. doi: 10.1023/a:1025347130953. doi:10.1023/A:1025347130953. [DOI] [PubMed] [Google Scholar]
- Beals J, Manson SM, Shore JH, Friedman M, Ashcraft M, Fairbank JA, et al. The prevalence of posttraumatic stress disorder among American Indian Vietnam veterans: Disparities and context. Journal of Traumatic Stress. 2002;15:89–97. doi: 10.1023/A:1014894506325. doi:10.1023/A:1014894506325. [DOI] [PubMed] [Google Scholar]
- Beals J, Manson SM, Whitesell NR, Spicer P, Novins DK, Mitchell CM. Prevalence of DSM-IV disorders and attendant help seeking in two American Indian reservation populations. Archives of General Psychiatry. 2005;62:99–108. doi: 10.1001/archpsyc.62.1.99. Retrieved from http://archpsyc.ama-assn.org/cgi/content/full/62/1/99. [DOI] [PubMed] [Google Scholar]
- Bell RA, Arcury TA, Chen H, Anderson AM, Savoca MR, Kohrman T, et al. Use of tobacco products among rural older adults: Prevalence of ever use and cumulative lifetime use. Addictive Behaviors. 2009;34:662–667. doi: 10.1016/j.addbeh.2009.03.031. doi:10.1016/j.addbeh.2009.03.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolinder G, Alfredsson L, Englund A, de Faire U. Smokeless tobacco use and increased cardiovascular mortality among Swedish construction workers. American Journal of Public Health. 1994;84:399–404. doi: 10.2105/ajph.84.3.399. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1614817/?tool=pubmed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Kahler CW, Zvolensky MJ, Lejuez CW, Ramsey SE. Anxiety sensitivity: Relationship to negative affect smoking and smoking cessation in smokers with past major depressive disorder. Addictive Behaviors. 2001;26:887–899. doi: 10.1016/s0306-4603(01)00241-6. doi:10.1016/SO306-4603(01)00241-6. [DOI] [PubMed] [Google Scholar]
- Caraballo RS, Yee SL, Gfroerer J, Mirza SA. Adult tobacco use among racial and ethnic groups living in the United States, 2002–2005. Preventing Chronic Disease. 2008;5:A78. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2483561/?tool=pubmed. [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Tobacco use among U.S. racial/ethnic minority groups: A report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services; 1998. [Google Scholar]
- Centers for Disease Control and Prevention. Tobacco use among adults: United States, 2005. Morbidity and Mortality Weekly Report. 2006;55:1145–1148. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5542a1.htm. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. State-specific prevalence of cigarette smoking and smokeless tobacco use among adults: United States, 2009. Morbidity and Mortality Weekly Report. 2010;59:1400–1406. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5943a2.htm. [PubMed] [Google Scholar]
- Cochran WG. Sampling techniques. New York, NY: John Wiley and Sons; 1977. [Google Scholar]
- Coogan PF, Geller A, Adams M. Prevalence and correlates of smokeless tobacco use in a sample of Connecticut students. Journal of Adolescence. 2000;23:129–135. doi: 10.1006/jado.2000.0303. doi:10.1006/jado.2000.0303. [DOI] [PubMed] [Google Scholar]
- Critchley JA, Unal B. Health effects associated with smokeless tobacco: A systematic review. Thorax. 2003;58:435–443. doi: 10.1136/thorax.58.5.435. doi:10.1136/thorax.58.5.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durazzo TC, Gazdzinski S, Meyerhoff DJ. The neurobiological and neurocognitive consequences of chronic cigarette smoking in alcohol use disorders. Alcohol and Alcoholism. 2007;42:174–185. doi: 10.1093/alcalc/agm020. Retrieved from http://alcalc.oxfordjournals.org/content/42/3/174.long. [DOI] [PubMed] [Google Scholar]
- Ebbert JO, Glover ED, Shinozaki E, Schroeder DR, Dale LC. Predictors of smokeless tobacco abstinence. American Journal of Health Behavior. 2008;32:735–740. doi: 10.5555/ajhb.2008.32.6.735. doi:10.5555/ajph.2008.32.6.735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- England LJ, Levine RJ, Mills JL, Klebanoff MA, Yu KF, Cnattingius S. Adverse pregnancy outcomes in snuff users. American Journal of Obstetrics and Gynecology. 2003;189:939–943. doi: 10.1067/s0002-9378(03)00661-6. doi:10.1067/S0002-9378(03)00661-6. [DOI] [PubMed] [Google Scholar]
- Gilliland FD, Mahler R, Davis SM. Non-ceremonial tobacco use among southwestern rural American Indians: The New Mexico American Indian Behavioral Risk Factor Survey. Tobacco Control. 1998;7:156–160. doi: 10.1136/tc.7.2.156. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1759690/?tool=pubmed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodwin RD, Zvolensky MJ, Keyes KM. Nicotine dependence and mental disorders among adults in the USA: Evaluating the role of the mode of administration. Psychological Medicine. 2008;38:1277–1286. doi: 10.1017/S0033291708003012. doi:10.1017/S0033291708003012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Hasin DS, Chou P, Stinson FS, Dawson DA. Nicotine dependence and psychiatric disorders in the United States: Results from the national epidemiologic survey on alcohol and related conditions. Archives of General Psychiatry. 2004;61:1107–1115. doi: 10.1001/archpsyc.61.11.1107. Retrieved from http://archpsyc.ama-assn.org/cgi/content/full/61/11/1107. [DOI] [PubMed] [Google Scholar]
- Henderson PN, Jacobsen C, Beals J the American Indian Service Utilization, Psychiatric Epidemiology, Risk and Protective Factors Project Team. Correlates of cigarette smoking among selected Southwest and Northern Plains tribal groups: The AI-SUPERPFP study. American Journal of Public Health. 2005;95:867–872. doi: 10.2105/AJPH.2004.050096. doi:10.2105/AJPH.2004.050096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hodge FS, Struthers R. Persistent smoking among Northern Plains Indians: Lenient attitudes, low harm value, and partiality toward cigarette smoking. Journal of Cultural Diversity. 2006;13:181–185. Retrieved from http://tuckerpub.com/jcd.htm. [PubMed] [Google Scholar]
- Howard-Pitney B, Winkleby MA. Chewing tobacco: Who uses and who quits? Findings from NHANES III, 1988–1994. National Health and Nutrition Examination Survey III. American Journal of Public Health. 2002;92:250–256. doi: 10.2105/ajph.92.2.250. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1447052/?tool=pubmed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen MK, Sorensen TL, Andersen AT, Thorsen T, Tolstrup JS, Godtfredsen NS, et al. A prospective study of the association between smoking and later alcohol drinking in the general population. Addiction. 2003;98:355–363. doi: 10.1046/j.1360-0443.2003.00304.x. doi:10.1046/j.1360-0443.2003.00304.x. [DOI] [PubMed] [Google Scholar]
- Johnson EO, Breslau N. Is the association of smoking and depression a recent phenomenon? Nicotine & Tobacco Research. 2006;8:257–263. doi: 10.1080/14622200600576644. doi:10.1080/14622200600576644. [DOI] [PubMed] [Google Scholar]
- Kerby DS, Brand MW, John R. Anger types and the use of cigarettes and smokeless tobacco among Native American adolescents. Preventive Medicine. 2003;37:485–491. doi: 10.1016/s0091-7435(03)00174-9. doi:10.1016/S0091-7435(03)00174-9. [DOI] [PubMed] [Google Scholar]
- Kessler RC, McGonagle KA, Zhao S, Nelson CB, Hughes M, Eshlemann S, et al. Lifetime and 12-month prevalence of DSM-III-R psychiatric disorders in the United States: Results from the National Comorbidity Survey. Archives of General Psychiatry. 1994;51:8–19. doi: 10.1001/archpsyc.1994.03950010008002. Retrieved from http://archpsyc.ama-assn.org/cgi/content/abstract/51/1/8. [DOI] [PubMed] [Google Scholar]
- Kish L. Survey sampling. New York, NY: John Wiley; 1965. [Google Scholar]
- Marcus AC, Crane LA, Shopland DR, Lynn WR. Use of smokeless tobacco in the United States: Recent estimates from the current population survey. NCI Monographs. 1989;8:17–23. Retrieved from http://jncimono.oxfordjournals.org/ [PubMed] [Google Scholar]
- Mumford EA, Levy DT, Gitchell JG, Blackman KO. Smokeless tobacco use 1992–2002: Trends and measurement in the Current Population Survey-Tobacco Use Supplements. Tobacco Control. 2006;15:166–171. doi: 10.1136/tc.2005.012807. doi:10.1136/tc.2005.012807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson DE, Mowery P, Tomar S, Marcus S, Giovino G, Zhao L. Trends in smokeless tobacco use among adults and adolescents in the United States. American Journal of Public Health. 2006;96:897–905. doi: 10.2105/AJPH.2004.061580. doi:10.2105/AJPH.2004.061580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pariante CM, Lightman SL. The HPA axis in major depression: Classical theories and new developments. Trends in Neurosciences. 2008;31:464–468. doi: 10.1016/j.tins.2008.06.006. doi:10.1016/j/tins.2008.06.006. [DOI] [PubMed] [Google Scholar]
- Rasmusson AM, Vythilingam M, Morgan CA. The neuroendocrinology of PTSD: New directions. CNS Spectrums. 2003;8:651–667. doi: 10.1017/s1092852900008841. Retrieved from http://www.cnsspectrums.com/aspx/archivedissues.aspx. [DOI] [PubMed] [Google Scholar]
- Redwood D, Lanier AP, Renner C, Smith J, Tom-Orme L, Slattery ML. Differences in cigarette and smokeless tobacco use among American Indian and Alaska Native people living in Alaska and the Southwest United States. Nicotine & Tobacco Research. 2010;12:791–796. doi: 10.1093/ntr/ntq087. doi:10.1093/ntr/ntq087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodu B. The scientific foundation for tobacco harm reduction, 2006–2011. Harm Reduction Journal. 2011;8:19. doi: 10.1186/1477-7517-8-19. doi: 10.1186/1477-7517-8-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohleder N, Kirschbaum C. The hypothalamic-pituitary-adrenal (HPA) axis in habitual smokers. International Journal of Psychophysiology. 2006;59:236–243. doi: 10.1016/j.ijpsycho.2005.10.012. doi:10.1016/j/ijpsycho.2005.10.012. [DOI] [PubMed] [Google Scholar]
- Rouse BA. Epidemiology of smokeless tobacco use: A national study. NCI Monographs. 1989;8:29–33. Retrieved from http://jncimono.oxfordjournals.org/ [PubMed] [Google Scholar]
- Savitz DA, Meyer RE, Tanzer JM, Mirvish SS, Lewin F. Public health implications of smokeless tobacco use as a harm reduction strategy. American Journal of Public Health. 2006;96:1934–1939. doi: 10.2105/AJPH.2005.075499. doi:10.2105/AJPH.2005.075499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sawchuk, C. N., Roy-Byrne, P., Noonan, C., Bogart, A., Goldberg, J., Manson, S. M., et al. (2011). The association of panic disorder, PTSD, and major depression with smoking in American Indians. Manuscript under review. [DOI] [PMC free article] [PubMed]
- Spangler JG, Michielutte R, Bell RA, Knick S, Dignan MB, Summerson JH. Dual tobacco use among Native American adults in southeastern North Carolina. Preventive Medicine. 2001;32:521–528. doi: 10.1006/pmed.2001.0835. doi:10.1006/pmed.2001.0835. [DOI] [PubMed] [Google Scholar]
- Steele CB, Cardinez CJ, Richardson LC, Tom-Orme L, Shaw KM. Surveillance for health behaviors of American Indians and Alaska Natives: Findings from the Behavioral Risk Factor Surveillance System, 2000–2006. Cancer. 2008;113:1131–1141. doi: 10.1002/cncr.23727. Retrieved from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2893297/pdf/ntq087.pdf. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration, Office of Applied Studies. The NSDUH report: Smokeless tobacco use, initiation, and relationship to cigarette smoking: 2002 to 2007. Rockville, MD: Office of Applied Studies; 2009. Retrieved from http://oas.samhsa.gov/2k9/smokelessTobacco/smokelessTobacco.pdf. [Google Scholar]
- Tercyak KP, Audrain J. Psychosocial correlates of alternate tobacco product use during early adolescence. Preventive Medicine. 2002;35:193–198. doi: 10.1006/pmed.2002.1060. doi:10.1006/pmed.2002.1060. [DOI] [PubMed] [Google Scholar]
- Tomar SL. Is use of smokeless tobacco a risk factor for cigarette smoking? The U.S. experience. Nicotine & Tobacco Research. 2003;5:561–569. doi: 10.1080/1462220031000118667. Retrieved from http://ntr.oxfordjournals.org/ [DOI] [PubMed] [Google Scholar]
- Tomar SL, Alpert HR, Connolly GN. Patterns of dual use of cigarettes and smokeless tobacco among US males: Findings from national surveys. Tobacco Control. 2010;19:104–109. doi: 10.1136/tc.2009.031070. doi:10.1136/tc.2009.031070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. Healthy people 2010. Washington, DC: Author; 2002. [Google Scholar]
- Vander Weg MW, DeBon M, Peterson AL, Sherrill-Mittleman D, Klesqes RC, Relyea GE. Prevalence and correlates of lifetime smokeless tobacco use in female military recruits. Nicotine & Tobacco Research. 2005;7:431–441. doi: 10.1080/14622200500125781. Retrieved from http://ntr.oxfordjournals.org/ [DOI] [PubMed] [Google Scholar]
- Wilhelm K, Wedgwood L, Niven H, Kay-Lambkin F. Smoking cessation and depression: Current knowledge and future directions. Drug and Alcohol Review. 2006;25:97–107. doi: 10.1080/09595230500459560. Retrieved from http://www.wiley.com/bw/journal.asp?ref=0959-5236. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Composite International Diagnostic Interview, version 1.0. Geneva, Switzerland: World Health Organization; 1990. [Google Scholar]
- Ziedonis D, Hitsman B, Beckham JC, Zvolensky M, Adler LE, Audrain-McGovern J, et al. Tobacco use and cessation in psychiatric disorders: National Institute of Mental Health report. Nicotine & Tobacco Research. 2008;10:1691–1715. doi: 10.1080/14622200802443569. Retrieved from http://ntr.oxfordjournals.org/ [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Sachs-Ericsson N, Feldner MT, Schmidt NB, Bowman CJ. Neuroticism moderates the effect of maximum smoking level on lifetime panic disorder: A test using an epidemiologically defined national sample of smokers. Psychiatry Research. 2006;141:321–332. doi: 10.1016/j.psychres.2005.07.019. doi:10.1016/j.psychres.2005.07.019. [DOI] [PubMed] [Google Scholar]


