Abstract
Objective
To determine whether there are disparities in postacute stroke rehabilitation based on type of stroke, race/ethnicity, sex/gender, age, socioeconomic status, geographic region, or service area referral patterns in a large integrated health system with multiple levels of care.
Design
Cohort study tracking rehabilitation services for 365 days after acute hospitalization for a first stroke.
Setting
The Northern California Kaiser Permanente Health System (approximately 3.3 million membership population)
Participants
A total of 11,119 patients hospitalized for acute stroke from 1996 to 2003. The cohort includes patients discharged from acute care after a stroke. Postacute care rehabilitation services were evaluated according to the level of care ever-received within the 365 days after discharge from acute care, including inpatient rehabilitation hospital (IRH), skilled nursing facility (SNF), home health and outpatient, or no rehabilitation services.
Interventions
Not applicable.
Main Outcome Measure
Service delivery.
Results
Patients discharged to an IRH had longer lengths of stay in acute care. Patients with hemorrhagic stroke were less likely to be treated in an IRH. Patients whose highest level of rehabilitation was SNF were older and more likely to be women. After adjusting for age and other covariates, women were less likely to go to an IRH than men. Asian and black patients were more likely than white patients to be treated in an IRH or SNF. Also more likely to go to an IRH were patients from higher socioeconomic groups, from urban areas, and from geographic areas close to the regional rehabilitation hospital.
Conclusions
These results suggest variation in care delivery and extent of postacute care based on differences in patient demographics and geographic factors. Results also varied over time. Some minority populations in this cohort appeared to be more likely to receive IRH care, possibly because of disease severity, family support systems, cultural factors, or differences in referral patterns.
INTRODUCTION
According to a recent report, the annual incidence of stroke, including recurrent stroke, in the United States is approximately 780,000, and the prevalence of stroke is estimated to be 5.8 million [1]. Stroke is the third-leading cause of death in the United States, after heart disease and cancer. Although stroke mortality rates have declined during the last 30 years, the death rate is still approximately 25%, and mortality rates have decreased little, if at all, since 1990 [2]. Differences in death rates for subpopulations grouped by race/ethnicity, socioeconomic status, and geography are “striking,” according to findings of a national consensus group [3]. A leading cause of disability among adults, stroke is associated with estimated direct and indirect costs in 2008 of 65.5 billion dollars; nursing home costs alone account for an estimated 15.7 billion dollars [2].
Rehabilitation services and programs are required for patients who experience disabling effects from a stroke. Functional recovery or restoration of some functional abilities—with improvements in activity and participation in life roles—may continue for months or years after the acute event. Stroke rehabilitation guidelines have been developed and implemented by many organizations, including the health system that was the site for this study, and emphasize the work of specialized teams over a care continuum [4].
Rehabilitation after acute inpatient medical and, in some cases, surgical care may be provided at an inpatient rehabilitation hospital (IRH), a skilled nursing facility (SNF), an outpatient clinic (OP), or by home health care (HH). During the last several decades in the United States, the average acute length of stay for patients with stroke has decreased to approximately 5.2 days [2].
Health disparities are differences in health care processes or health outcomes that exist among population groups as defined by social or other factors. Health inequity is a term used to signify unequal treatment or injustices that are a cause of health disparities [5,6]. The factors that contribute to health disparities or health inequities usually are multiple for any one group of individuals and, as a consequence, are difficult to analyze. Disparities or inequities may relate to overall health status or health care access or quality. In this study, the focus was on health care services and health care utilization, not quality of care or health care outcomes.
Differences are evident among racial/ethnic groups and between men and women in stroke type, incidence, severity, and mortality [7–9]. Black subjects have almost twice the risk of stroke compared with white subjects, and the incidence peaks at a younger age [10]. Black subjects, and in particular low-income ones, experience severer strokes [11] and a worse “trajectory of functional recovery” in the first year after stroke [12,13]. The incidence of stroke in Hispanic populations is also greater than in white populations, although not to the same degree as black populations [2]. Hispanics and Asian populations have a greater incidence of hemorrhagic stroke, and hemorrhagic strokes are associated with greater degrees of functional impairment than ischemic strokes [14].
Evidence has been accumulating that poststroke rehabilitation services are not equally delivered among populations, although the findings are not consistent. A Los Angeles study of community-dwelling patients with stroke and other diagnoses found that minority populations, less-educated individuals, and the oldest patients were significantly less likely to use physical and occupational therapy services [15]. However, results of a study in Maryland suggested that black patients experiencing a stroke were more likely than white patients to go to an IRH [16]. A Medicare sample analysis from 297 hospitals in 5 states showed more black patients than white patients receiving physical and occupational therapy, but black patients had more motor deficits [13]. A study of stroke patients in the Veterans Administration system found no racial differences in IRH care [13,17]. Racial disparities in outcomes at discharge from an IRH and at 3 months after discharge were evident in a recent study in California, with black and Asian patients demonstrating less functional improvement at 3 months after discharge [18].
Minority groups other than blacks have been relatively unstudied. No study has focused on the array of factors that may be associated with disparities in the delivery of postacute care (PAC) and rehabilitation services to patients with stroke, namely type of stroke, age, sex/gender, race/ethnicity, socioeconomic status (as reflected by income and education), geographic factors such as rural/urban residence and proximity to an IRH, and hospital referral patterns. Although previous studies have been illuminating, none has assessed health care disparities in a prepaid, integrated health system.
The hypothesis of this study was that disparities exist in PAC delivery. It was expected that social determinants of health such as race/ethnicity, income, and rural/urban residence would be identified as contributing factors in determination of PAC sites. The authors focused on identifying disparities across the range of inpatient and outpatient rehabilitation services. This study explored health care delivery and disparities among members of the Kaiser Permanente Medical Care Program in Northern California, a prepaid health plan delivering care in an integrated model to 3.3 million individuals at the time of the study. The system has multiple settings for PAC, and rehabilitation and providers use regional guidelines to promote greater uniformity in decision-making.
In the health system under study, patients are referred after acute hospitalization to a variety of settings of care that are part of an integrated system of care. The relationship of the medical group and the hospital and health plan is illustrated in Figure 1. This Northern California Kaiser Permanente health system includes medical centers, ambulatory care centers, one rehabilitation hospital, and a home health system. Contracts are made with skilled nursing facilities throughout the region except in the case of one skilled nursing facility that is operated by the health system.
Figure 1.
Health plan, medical group, health plan relationships.
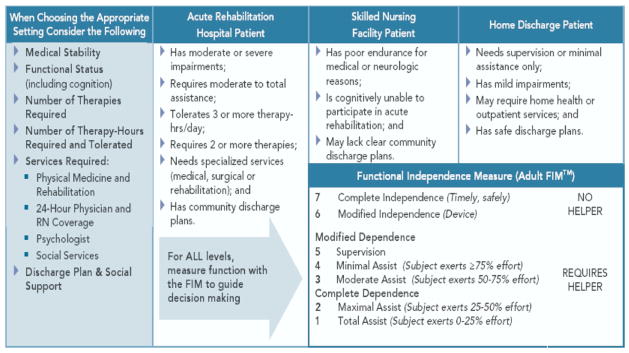
Hospital-based physicians in The Permanente Medical Group (TPMG) are key decision-makers about the appropriate next level of care after the acute hospital; discharge planners and in some cases social workers and case managers help to facilitate the discharge from this setting. In the SNF setting, physicians and SNF coordinators are involved in the care of the patient and in determinations about the next level of care. In outpatient and home care, the primary care physician and in some cases a TPMG physiatrist are involved in the care of the patient, making decisions about services or next level of care. The TPMG Stroke Guidelines have been used since the late 1990s; revisions are made to the guidelines every 2 years. The rehabilitation section of the guideline has been updated every 2 years during the time period of this study, but the criteria for the various levels of postacute care have not been substantially revised during this period (Figure 2).
Figure 2.
Stroke levels of care.
In this study, the authors considered IRH care the most intensive level of PAC, given the number of providers with expertise and skills in treating patients with stroke, and the number of hours of treatment and the structure and process of care requirements in that setting [19]. In the conceptual hierarchy, the next level of care was SNF, followed by HH, followed by OP, and finally no PAC. In the health system, patients often are referred to a SNF initially and then may be referred to IRH if they are in need of, and can tolerate, a more intensive level of care. A high percentage of patients treated in IRH and SNF go home eventually with HH in most cases. This is a different pattern of referral than many health systems. This referral pattern created a problem for our data analyses, as many patients received multiple levels of care but at varying points in their recovery. Therefore, it was decided that both first level of care and also highest level or most intensive (IRH) level of care ever received would be investigated.
METHODS
Study Design and Study Sample
The comprehensive Kaiser Permanente Northern California (KPNC) claims database, California state mortality data, and U.S. Census data were used for the study. The authors identified adult patients hospitalized with a primary diagnosis of stroke and discharged from hospitals in the KPNC system from 1996 to 2003 and identified those patients with a primary diagnosis of stroke, which was defined by using the International Classification of Disease Codes, Version 9 (ICD-9). The following ICD-9 codes were used to define acute stroke: 430.x, 431.x, 433.01– 433.99, 434.01– 434.99, 436.x, 997.02. The original stroke cohort included 22,522 patients who had only 1 acute stroke hospitalization during the study period.
The initial exclusion was conducted based on the following criteria: in-hospital death (n = 3269); invalid medical record number (n = 35); age at discharge younger than 18 years (n = 49); brain tumor, abscess, and traumatic brain injuries at the time of acute stroke or follow-up period (n = 708); patients listed in KPNC “No Contact File,” ie, members who did not wish to be or could not be contacted (n = 4), non-KPNC members at acute care discharge (n = 1011), and patients with 2 or more months membership gap during follow-up (n = 137). A total of 17,309 patients remained for further data exploration. Additional exclusions removed patients who were not followed up for 1 year after acute care discharge because of death or membership discontinuation (n = 4655); treatment at a non-Kaiser hospital for acute care (n = 1129); unspecified patient gender (n = 2); missing race/ethnicity (n = 125), or instances in which race/ethnicity was other than Asian, black, Hispanic, or white (n = 213). The final study sample was 11,119 patients.
Covariates and PAC Services
Patient social demographic data included age at acute care hospital discharge, sex/gender, self-reported race/ethnicity (Asian, black, Hispanic, white), urban or rural residential area, and median household income. Patients’ residential zip codes were linked to the Rural-Urban Commuting Area Codes (i.e., RUCAs). The KPCN system does not record the individual’s income. Therefore, for each person in the sample, a median household income level was assigned based on the U.S. 2000 census block group where the person lived. Taking into consideration the median household income and poverty line in California as well as data distributions, the median household income of the study cohort also was grouped into 3 categories: less than $40,000; $40,001 to $80,000; and $80,001 or more.
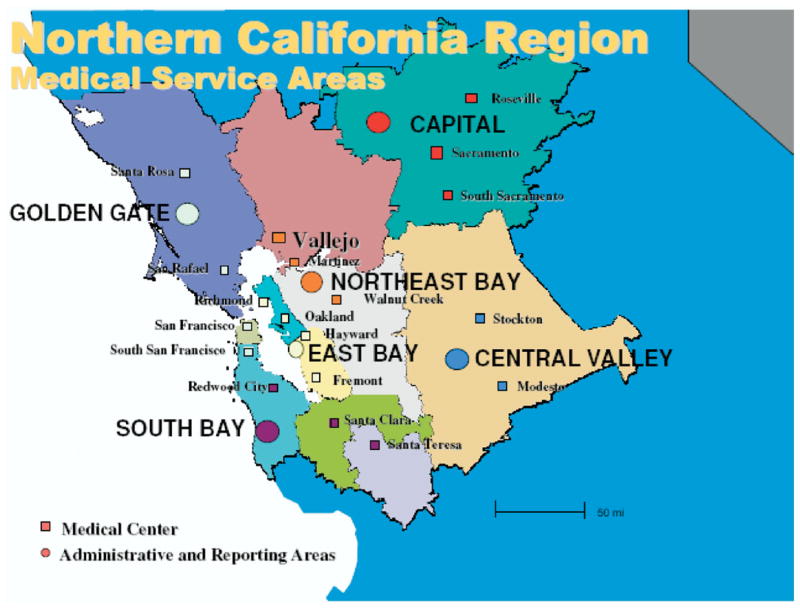
On the basis of ICD-9 codes, patients were categorized with acute stroke into (1) hemorrhagic stroke: 997.02 (postoperative stroke); 430 (subarachnoid hemorrhage), and 431 (intracerebral hemorrhage) and (2) ischemic stroke (433, 434, 436). Length of acute care hospital stay after stroke was obtained as a measure of acute care utilization as well as a proxy for stroke severity. Twenty-one KPNC acute care facilities were included in the study, representing 6 administrative and reporting areas: East Bay, Central Valley, Northeast Bay, Capital, South Bay, and Golden Gate (Figure 3).
Figure 3.
Map of the study’s medical service areas, Northern California region.
PAC data were collected over the course of 1 year after acute hospitalization, including hospitalization in the IRH serving the region, treatment in a SNF, HH, and/or an OP clinic. Only one centrally located rehabilitation hospital, located in Vallejo, served the adult population at the time of this study and, for some patients and families, may have been geographically remote. (After 2003, additional IRH sites became available in the Central Valley and South Bay.) In the years represented by the study, there was little variation in the health plan coverage of the membership. The membership grew from 2.8 million members to 3.3 million members during the time period under study. In this integrated health system, a patient may receive care in SNF after hospital discharge and then be transferred to the IRH, or from IRH to SNF. Thus, the first level of PAC after hospital discharge as well as “ever treated” were identified so as to capture all patients treated in all settings. A summary PAC variable was created based on the type of care that a patient ever received during follow-up, ie, IRH, SNF, HH, OP, or None (no care in the other categories).
Data Analysis
Descriptive statistical analyses were conducted for all explanatory and outcome variables under study to examine data distribution, including mean, standard deviation (SD), median, interquartile range (IQR) for continuous variables, and frequency tables and percentages for categorical data. The relationship between highest level of care and year of discharge from hospitalization after stroke was tested using χ2 tests for independence and trend.
Trends of PAC services over time were also evaluated. Multiple regression models were used to explore associations of explanatory variables and PAC services. Two logistic regressions were used to model the binary variable of ever-received-IRH or ever-received-SNF care during the 12-month follow-up period and by using age, sex/gender, race/ethnicity, median household income, acute length of stay, and Kaiser Permanente service area as explanatory variables. An ordinal logistic regression model was used to model most intensive PAC service received during the follow-up period using the same explanatory variables. A significance level of .05 was set for all of the analyses. Initially, all the relevant explanatory variables were entered into the model. Backwards selection was used for model selection. Odds ratios and 95% confidence intervals are presented for associations between factors and study outcomes. SAS 9.13 [20] was used for data analysis.
RESULTS
Description of the Cohort
Table 1 presents the descriptive data for the final cohort. Of the 11,119 stroke patients in the cohort, mean age at acute care discharge was 69.7 years (SD = 13.0), 51.1% of the cohort were female, 70.2% white, 10.8% black, 8.8% Asian, and 7.4% Hispanic. Most of the patients (99.0%) resided in California, with a majority (96.0%) residing in urban areas. Patient income and educational level was obtained from 2000 U.S. Census Data. From these data, it was found that 22% of the participants lived in areas in which the median income was $40,000 or less, 59.7% lived in areas with the median income was between $40,000 and $80,000, and the remaining 18.5% lived in areas with median income greater than $80,000. Although the median percentage of the patients ages 25 or older with at least a high school education was 87.0%, the median percentage of patients ages 25 or older who had 4 years or higher college education was 27.6%. According to discharge diagnoses, 85.5% patients had an ischemic stroke and 14.5% had a hemorrhagic or postoperative stroke. The KPNC medical facility distribution by geographic region is depicted in Figure 3. The largest percentage of the cohort was from the Capital area (Greater Sacramento area, 21.5%), and the smallest percentage from the Central Valley area (5.2%). Median acute care length of stay was 3 days (IQR = 3 or present minimum, and maximum, or present 25th and 75th percentile).
Table 1.
Patient characteristics and PAC access 365 days after acute care discharge
| Parameters | All | White | Black | Asian | Hispanic |
|---|---|---|---|---|---|
| n (%) | 11,119 (100) | 8038 (70.2) | 1232 (10.8) | 1006 (8.8) | 843 (7.4) |
| Age, mean (SD) | 69.7 (13.0) | 71.6 (12.3) | 65.4 (13.2) | 63.7 (12.9) | 64.9 (13.9) |
| Sex, % | |||||
| Female | 51.1 | 51.6 | 53.9 | 47.2 | 46.1 |
| Male | 48.9 | 48.4 | 46.1 | 52.8 | 53.9 |
| Residential area, % | |||||
| Rural | 4.0 | 4.9 | 0.4 | 0.9 | 3.6 |
| Urban | 96.0 | 95.1 | 99.6 | 99.1 | 96.4 |
| Median household income, % | |||||
| <$40,001 | 21.8 | 19.0 | 40.7 | 17.0 | 26.7 |
| 40,001–$80000 | 59.7 | 61.0 | 49.9 | 61.1 | 60.6 |
| >$80,000 | 18.5 | 20.0 | 9.4 | 21.9 | 12.7 |
| ≥High school, % | |||||
| Mean (SD) | 83.5 (12.7) | 85.8 (11.0) | 75.9 (14.6) | 81.9 (12.2) | 75.3 (16.5) |
| Median (IQR) | 87.0 (77.6,92.8) | 88.7 (80.8,93.7) | 77.7 (66.4,87.9) | 84.3 (75.4,90.9) | 78.4 (65.0,88.6) |
| ≥4-year college, % | |||||
| Mean (SD) | 30.7 (18.4) | 32.3 (18.4) | 23.3 (17.2) | 32.5 (17.8) | 23.1 (15.6) |
| Median (IQR) | 27.6 (15.9,44.2) | 29.3 (17.5,44.8) | 19.0 (9.5,32.5) | 30.2 (18.7,42.3) | 20.2 (11.0,31.9) |
| Stroke type, % | |||||
| Hemorrhagic | 14.5 | 12.8 | 14.1 | 26.4 | 17.6 |
| Ischemic | 85.5 | 87.2 | 86 | 73.7 | 82.4 |
| KPNC service area, % | |||||
| East Bay | 16.7 | 49.7 | 30.5 | 12.3 | 7.5 |
| Central Valley | 5.2 | 77.2 | 5.2 | 3.3 | 14.4 |
| Northeast Bay | 18.8 | 78.7 | 8.4 | 8.3 | 4.6 |
| Capital | 21.5 | 83.6 | 7.2 | 3.9 | 5.3 |
| South Bay | 19.0 | 69.9 | 6.2 | 11.8 | 12.1 |
| Golden Gate | 18.9 | 74.0 | 7.5 | 11.6 | 6.9 |
| Acute care LOS, days | |||||
| Mean (SD) | 3.9 (3.5) | 3.8 (3.4) | 4.0 (3.9) | 3.0 (2.9) | 3.3 (3.2) |
| Median (IQR) | 3.0 (2.0,5.0) | 3.0 (2.0,5.0) | 3.0 (2.0,5.0) | 3.0 (2.0,5.0) | 3.0 (2.0,5.0) |
| PAC, % | |||||
| IRH | 11.8 | 10.8 | 15.1 | 16.9 | 11.5 |
| SNF | 40.9 | 41.9 | 41.4 | 37.7 | 34.6 |
| Highest level of PAC, % | |||||
| IRH | 11.8 | 10.8 | 15.1 | 16.9 | 11.5 |
| SNF | 32.8 | 34.4 | 30.7 | 26.3 | 27.4 |
| HH | 20.0 | 20.2 | 20.9 | 18.0 | 19.2 |
| OP | 28.9 | 28.2 | 27.3 | 31.5 | 34.3 |
| None | 6.5 | 6.4 | 6.1 | 7.3 | 7.6 |
Table 1 also shows the distribution of all variables by race/ethnicity. Self-reported patient race/ethnicity was statistically associated with all of the explanatory and outcome measures listed (P < .001 for all). White patients were older at acute stroke diagnosis than other race/ethnicity groups, with a mean age of 71.6 years in comparison with black (65.4 years), Asian (63.2), and Hispanic (64.9) populations. There were greater percentages of women in white (51.6%) and black (53.9%) groups than Asian (47.2%) and Hispanic (46.1%) groups. Greater percentages of white (4.9%) and Hispanic (3.6%) populations were living in rural areas than black (0.4%) and Asian (0.9%) populations. Black and Hispanic patients more often lived in areas of lower median household income than white and Asian patients. Asians were more likely to have had a hemorrhagic stroke (26.4%) than other race/ethnicity groups (12.8 –17.6%). White patients were in the majority in data from all areas, but the greatest percentage of white patients was in the Capital area. A large percentage of black patients resided in the East Bay area, and the largest percentages of Hispanics lived in the Central Valley and South Bay areas.
PAC Population Distribution Over Time
Between the years 1996 and 2003, the numbers of acute stroke cases increased as the membership population also increased. Changes in PAC utilization for stroke patients at KPNC were observed during that period. In 1996, there were 2.4% stroke patients discharged from acute care hospitals to IRH, 43.6% to SNF, 18.9% to HH, and 33.7% to home. In 2003, there were 4.3% acute stroke patients discharged to IRH, 32.6% to SNF, 13.5% to HH, and 46.6% to home. Percentages of patients discharged directly to IRH and home significantly increased over time whereas percentages of patients discharged directly to SNF and HH decreased over time.
Columns 3 and 4 of Table 2 show the percentage of individuals ever receiving IRH or SNF care, whereas columns 5 to 9 show percentages of individuals in each category of highest PAC services received during the follow-up period. On average, 11.8% of the study cohort was ever admitted to IRH and 40.9% were ever treated at SNF during the 1-year follow-up. The highest level of PAC services received was as follows: 11.8% IRH, 32.8% SNF, 20.0% HH, 28.9% OP, and 6.5% no PAC treatment. SNF and HH care as the highest PAC treatment received decreased over time while outpatient clinic visits as the sole PAC treatment increased over time.
Table 2.
Major PAC ever received during follow-up over time
| Year | n | IRH, % | SNF, % | Highest Level of PAC, %
|
||||
|---|---|---|---|---|---|---|---|---|
| IRH | SNF | HH | OP | None | ||||
| All | 11,119 | 11.8 | 40.9 | 11.8 | 32.8 | 20.0 | 28.9 | 6.5 |
| 1996 | 1159 | 12.5 | 48.0 | 12.5 | 38.1 | 22.5 | 14.5 | 11.5 |
| 1997 | 1047 | 11.6 | 46.3 | 11.6 | 37.2 | 20.3 | 21.0 | 9.9 |
| 1998 | 1308 | 11.2 | 43.9 | 11.2 | 34.4 | 21.6 | 23.9 | 8.9 |
| 1999 | 1475 | 11.8 | 43.4 | 11.8 | 34.6 | 21.2 | 25.3 | 7.1 |
| 2000 | 1475 | 12.7 | 37.6 | 12.7 | 28.8 | 22.8 | 33.6 | 2.2 |
| 2001 | 1543 | 11.4 | 36.9 | 11.4 | 29.8 | 19.6 | 39.0 | 0.2 |
| 2002 | 1589 | 13.0 | 38.2 | 13.0 | 30.1 | 15.5 | 35.8 | 5.6 |
| 2003 | 1523 | 10.6 | 37.1 | 10.6 | 32.1 | 17.2 | 31.0 | 9.1 |
| P | ||||||||
| χ2 | – | .4372 | <.0001 | <.0001 | ||||
| Trends | – | .6877 | <.0001 | – | ||||
Disparities in PAC Access
The distribution of PAC services by race/ethnicity groups are shown in Table 1. Findings from logistic regression analyses are presented in Table 3 (for ever-received IRH) and Table 4 (ever-received SNF). Table 5 shows the results of the ordinal logistic regression for highest level of PAC received. The initial explanatory variables in all models were age and length of stay (entered as continuous), and sex/gender, stroke type, year of discharge, category of median income, race/ethnicity, and rural/urban (entered as categorical variables). The models presented are the final models using backward selection. The tables contain the odds ratio estimates, its 95% confidence bounds, and the P-value for each estimate.
Table 3.
Logistic regression using “Ever Received IRH” as the outcome variable
| Variables | P Value | Estimated Odds Ratio | 95% Confidence Interval |
|---|---|---|---|
| All patients | |||
| Age | <.0001 | 0.97 | 0.97–0.98 |
| Sex: female (reference: male) | <.0001 | 0.70 | 0.62–0.79 |
| Hemorrhagic stroke (reference: ischemic stroke) | .0073 | 0.78 | 0.65–0.94 |
| Acute care LOS | <.0001 | 1.14 | 1.12–1.15 |
| KP service area (reference: capital) | |||
| Central CA* | – | – | – |
| East Bay | <.0001 | 1.90 | 1.55–2.33 |
| Golden Gate | <.0001 | 1.74 | 1.42–2.13 |
| North East Bay | <.0001 | 2.37 | 1.95–2.87 |
| South Bay | .0040 | 1.34 | 1.10–1.64 |
| With hemorrhagic stroke | |||
| Age | .0694 | 0.99 | 0.99–0.99 |
| Sex | <.0001 | 0.50 | 0.37–0.68 |
| Race/ethnicity (reference: white) | |||
| Asian | .0163 | 1.60 | 1.09–2.34 |
| Black | .7288 | 0.91 | 0.53–1.57 |
| Hispanic | .4879 | 1.21 | 0.70–2.10 |
| Median household income (Reference: >$80,000) | |||
| 0–$40,000 | .0005 | 0.40 | 0.24–0.67 |
| $40,000–$80,000 | .0043 | 0.60 | 0.42–0.85 |
| Acute care LOS | <.0001 | 1.10 | 1.10–1.10 |
| KP service area (reference: capital) | |||
| Central CA* | – | – | – |
| East Bay | .0502 | 1.74 | 1.00–3.04 |
| Golden Gate | .1899 | 1.44 | 0.84–2.46 |
| North East Bay | .0011 | 2.39 | 1.42–4.04 |
| South Bay | .9724 | 0.99 | 0.65–1.52 |
| With ischemic strokes | |||
| Age | <.0001 | 0.97 | 0.96–0.97 |
| Sex: female (reference: male) | <.0001 | 0.77 | 0.67–0.88 |
| Acute care LOS | <.0001 | 1.17 | 1.15–1.19 |
| KP service area (reference: capital) | |||
| Central CA* | – | – | – |
| East Bay | <.0001 | 1.79 | 1.43–2.24 |
| Golden Gate | <.0001 | 1.66 | 1.33–2.07 |
| North East Bay | <.0001 | 2.24 | 1.81–2.76 |
| South Bay | .0040 | 1.41 | 1.12–1.78 |
No patient at KP Central CA region received IRH during the 1-year follow-up.
Table 4.
Logistic regression using “Ever Received SNF” as the outcome variable
| Variables | P Value | Estimated Odds Ratio | 95% Confidence Interval |
|---|---|---|---|
| All patients | |||
| Age | <.0001 | 1.05 | 1.05–1.06 |
| Sex: female (reference: male) | .0046 | 1.13 | 1.04–1.23 |
| Median household Income (reference: >$80,000) | |||
| 0–$40,000 | .0232 | 1.18 | 1.02–1.36 |
| $40,000–$80,000 | .5036 | 1.04 | 0.92–1.17 |
| Hemorrhagic stroke (reference: ischemic stroke) | .0002 | 0.78 | 0.68–0.89 |
| Acute care LOS | <.0001 | 1.16 | 1.14–1.17 |
| KP service area (reference: Capital) | |||
| Central CA | .0020 | 0.72 | 0.59–0.89 |
| East Bay | <.0001 | 1.59 | 1.39–1.82 |
| Golden Gate | .0312 | 1.16 | 1.01–1.32 |
| North East Bay | .0046 | 0.82 | 0.72–0.94 |
| South Bay | .0005 | 0.78 | 0.68–0.90 |
| Year of acute care discharge (reference: 2003) | |||
| 1996 | <.0001 | 1.84 | 1.55–2.18 |
| 1997 | <.0001 | 1.81 | 1.52–2.16 |
| 1998 | <.0001 | 1.61 | 1.37–1.91 |
| 1999 | <.0001 | 1.57 | 1.33–1.84 |
| 2000 | .2599 | 1.10 | 0.93–1.29 |
| 2001 | .7641 | 1.03 | 0.87–1.20 |
| 2002 | .4848 | 1.06 | 0.90–1.24 |
| With hemorrhagic stroke | |||
| Age | <.0001 | 1.06 | 1.05–1.07 |
| Acute care LOS | <.0001 | 1.08 | 1.06–1.11 |
| KP service area (reference: Capital) | |||
| Central CA | .0518 | 0.54 | 0.29–1.00 |
| East Bay | <.0001 | 2.35 | 1.59–3.48 |
| Golden Gate | .3742 | 1.18 | 0.82–1.70 |
| North East Bay | .0494 | 1.49 | 1.00–2.21 |
| South Bay | .0037 | 0.64 | 0.47–0.86 |
| Year of acute care discharge (reference: 2003) | |||
| 1996 | .0032 | 2.04 | 1.27–3.29 |
| 1997 | .0024 | 2.14 | 1.31–3.49 |
| 1998 | .0024 | 1.95 | 1.27–3.00 |
| 1999 | .0096 | 1.73 | 1.14–2.62 |
| 2000 | .4028 | 1.20 | 0.78–1.83 |
| 2001 | .1033 | 1.42 | 0.93–2.15 |
| 2002 | .9546 | 0.99 | 0.64–1.53 |
| With ischemic stroke | |||
| Age | <.0001 | 1.05 | 1.05–1.05 |
| Sex: female (reference: male) | <.0001 | 1.21 | 1.10–1.32 |
| Median household income (Reference: 80,000) | |||
| 0–$40,000 | .0007 | 1.31 | 1.12–1.52 |
| $40,000–$80,000 | .0765 | 1.12 | 0.99–1.27 |
| Acute care LOS | <.0001 | 1.22 | 1.20–1.24 |
| KP service area (reference: Capital) | |||
| Central CA | .0022 | 0.71 | 0.57–0.88 |
| East Bay | <.0001 | 1.48 | 1.28–1.71 |
| Golden Gate | .1148 | 1.12 | 0.97–1.29 |
| North East Bay | .0002 | 0.76 | 0.66–0.88 |
| South Bay | .0717 | 0.86 | 0.74–1.01 |
| Year of acute care discharge (reference: 2003) | |||
| 1996 | <.0001 | 1.83 | 1.52–2.20 |
| 1997 | <.0001 | 1.74 | 1.44–2.11 |
| 1998 | <.0001 | 1.60 | 1.33–1.91 |
| 1999 | <.0001 | 1.55 | 1.30–1.84 |
| 2000 | .3450 | 1.09 | 0.91–1.30 |
| 2001 | .7126 | 0.97 | 0.81–1.15 |
| 2002 | .5558 | 1.05 | 0.88–1.25 |
Table 5.
Ordinal logistic regression using highest level of PAC received as the outcome
| Variables | P Value | Estimated Odds Ratio | 95% Confidence Interval |
|---|---|---|---|
| All patients | |||
| Age | <.0001 | 1.03 | 1.03–1.04 |
| Sex: female (reference: male) | .0092 | 1.09 | 1.02–1.17 |
| Race/ethnicity (reference: white) | |||
| Asian | .0035 | 1.21 | 1.06–1.37 |
| Blacks | .0112 | 1.16 | 1.03–1.31 |
| Hispanic | .6281 | 1.03 | 0.91–1.18 |
| Acute care LOS | <.0001 | 1.18 | 1.16–1.19 |
| Hemorrhagic stroke (reference: ischemic stroke) | <.0001 | 0.65 | 0.58–0.72 |
| KP service area (reference: Capital) | |||
| Central CA | <.0001 | 0.65 | 0.56–0.77 |
| East Bay | <.0001 | 1.33 | 1.18–1.49 |
| Golden Gate | .0273 | 1.13 | 1.01–1.25 |
| North East Bay | .1682 | 1.08 | 0.97–1.20 |
| South Bay | .0016 | 0.84 | 0.75–0.93 |
| Year of acute care discharge (reference: 2003) | |||
| 1996 | <.0001 | 1.57 | 1.37–1.81 |
| 1997 | <.0001 | 1.49 | 1.29–1.73 |
| 1998 | <.0001 | 1.38 | 1.21–1.58 |
| 1999 | <.0001 | 1.41 | 1.24–1.61 |
| 2000 | .0004 | 1.26 | 1.11–1.44 |
| 2001 | .0178 | 1.17 | 1.03–1.33 |
| 2002 | .2389 | 1.08 | 0.95–1.23 |
| With hemorrhagic stroke | |||
| Age | <.0001 | 1.04 | 1.03–1.05 |
| Sex: female (reference: male) | .0552 | 0.84 | 0.70–1.00 |
| Median household income (reference: >$80,000) | |||
| 0–$40,000 | .0076 | 0.66 | 0.49–0.90 |
| $40,000–$80,000 | .0156 | 0.74 | 0.58–0.95 |
| Acute care LOS | <.0001 | 1.08 | 1.06–1.11 |
| KP service area (reference: Capital) | |||
| Central CA | .0585 | 0.62 | 0.38–1.02 |
| East Bay | <.0001 | 1.92 | 1.39–2.66 |
| Golden Gate | .0291 | 1.41 | 1.04–1.91 |
| North East Bay | .0022 | 1.69 | 1.21–2.37 |
| South Bay | .0679 | 0.79 | 0.61–1.02 |
| With ischemic stroke | |||
| Age | <.0001 | 1.03 | 1.03–1.03 |
| Sex: female (reference: male) | .0001 | 1.16 | 1.08–1.25 |
| Race/ethnicity (reference: whites) | |||
| Asian | .1436 | 1.12 | 0.96–1.29 |
| Blacks | .0096 | 1.19 | 1.04–1.35 |
| Hispanic | .9136 | 1.01 | 0.87–1.17 |
| Median household income (reference: >$80,000) | |||
| 0–$40,000 | .0048 | 1.21 | 1.06–1.37 |
| $40,000–$80,000 | .0983 | 1.09 | 0.98–1.21 |
| Acute care LOS | <.0001 | 1.23 | 1.21–1.25 |
| KP service area (reference: Capital) | |||
| Central CA | <.0001 | 0.60 | 0.51–0.72 |
| East Bay | .0006 | 1.25 | 1.10–1.42 |
| Golden Gate | .1115 | 1.10 | 0.98–1.24 |
| North East Bay | .8493 | 1.01 | 0.90–1.14 |
| South Bay | .4165 | 0.95 | 0.83–1.08 |
| Year of acute care discharge (reference: 2003) | |||
| 1996 | <.0001 | 1.63 | 1.40–1.91 |
| 1997 | <.0001 | 1.52 | 1.30–1.79 |
| 1998 | <.0001 | 1.41 | 1.21–1.64 |
| 1999 | <.0001 | 1.45 | 1.26–1.68 |
| 2000 | .0005 | 1.29 | 1.12–1.50 |
| 2001 | .0898 | 1.13 | 0.98–1.31 |
| 2002 | .3722 | 1.07 | 0.92–1.23 |
Outcome 1: Ever Received IRH Care
Only age, sex/gender, stroke type, length of stay (LOS), and KP service area were statistically significant in the final model. Older individuals, women, and individuals who had a hemorrhagic stroke were less likely to ever receive IRH services, whereas an increase in LOS increased the likelihood of ever receiving IRH. Patients who did not receive IRH care may or may not have received other services. Compared with the KP facility in the Capital area, all other areas were more likely to have outpatients who received IRH at some point during the 12-month period after discharge from hospitalization.
Outcome 2: Ever Received SNF Care
Age, sex/gender, stroke type, LOS, median household income of the residence area, KP service area, and year of discharge were statistically significant in the model. There was a greater likelihood of receiving SNF care at some point during follow-up for older individuals, women, patients with a longer LOS, and those in the lowest income category. Compared with the Central Valley area, East Bay, Capital, and Golden Gate areas were more likely to have individuals who received SNF at some point, whereas North Bay and South Bay areas were not statistically different from the Central Valley area. Compared with the year 2003, data from early years (1996 –1999) suggested that patients were more likely to have received some SNF care, whereas in later years (2000 –2002), findings were not statistically different.
Outcome 3: Highest Level of PAC Services Received
Age, sex/gender, stroke type, LOS, race/ethnicity, KP service area, and year of discharge were statistically significant in the model. The likelihood that a person received a greater level of PAC service increased with increasing age, being female, having a longer LOS, and having an ischemic stroke. Hispanic patients were not different from white patients, whereas black and Asian subjects were more likely to receive greater levels of PAC than white subjects. All areas were more likely than the Central Valley area to have participants in greater levels of PAC service. Participants in the East Bay area, for example, were twice as likely to receive institutional care than patients in the Central area. Except for the year 2002, patients in all other years were more likely to receive greater levels of PAC services when compared to the year 2003.
DISCUSSION
Results were expected in some areas and unexpected in others. Despite integration and uniformity in many aspects of the system, the interplay of patient and subregional characteristics that contributed to different PAC utilization as well as some variation during the time period of the study were observed.
Rather than demonstrating differences in care based solely on minority status, the findings indicate that disparities in rehabilitation services provided after stroke may be caused by complex interrelationships of socioeconomic factors, including income, age, sex/gender, race/ethnicity, geographic factors, and type or severity of stroke. Cultural factors, yet to be determined, also may play a role in the determination of the types of services and the settings of care for subpopulations from various ethnic groups.
Unexpectedly, it was found that white patients in our population were less likely to go to an IRH and, in fact, other racial/ethnic groups, namely Asian and black populations, were more likely to receive care in this setting. White women were more likely to be treated in an SNF even after adjusting for other explanatory variables, including age and type of stroke. Median household income was a significant factor in receipt of SNF care, ie, patients with lower income were more likely to go to SNF. Proximity to the regional IRH also was associated with the care health plan members received.
The longer average LOS in acute hospital for patients going to IRH may be a proxy for severity or may represent the longer period required to secure a bed in an IRH as compared with other settings that are more accessible because of geographic proximity, admission criteria, and process of referral and decision-making. Discharge to a SNF under Centers for Medicare and Medicaid reimbursement guidelines allows for a longer LOS (up to 100 days) in a SNF as compared with an IRH (not reimbursed under Medicare for more than 30 days for a patient with a stroke) [21]. In addition, SNFs are more available in a wider geographic area and more readily accessible than the one IRH in the system at the time of this study.
The variation in discharge level of care by acute hospitals within the system may reflect differences in decision-making by discharge planners or physicians. Referral patterns may vary because of the availability of PM&R physicians for consultation and assistance in functional prognostication, medical appropriateness, and determination of the best setting for rehabilitation after acute hospitalization.
Educational factors such as patient and family knowledge about the differences in PAC and rehabilitation services and the availability of information through professional contacts may lead to more likely placement in an IRH than SNF. Acculturation and health practices among racial/ethnic groups must be considered important in the investigation of health care disparities in health care delivery and outcomes. Recent research by Gordon [22] in this health system, in which the author investigated educational level and race/ethnicity and health practices, suggests that differences in health status cannot be fully explained by differences in age and educational attainment within racial-ethnic groups.
Social and cultural factors, such as the number of caregivers available to secure a discharge plan for IRH placement, may be important determinants of sites of care after stroke. For certain populations, the culturally associated shame of placement in a long-term care facility may be operative in the process of decisions by patients and families about placement. When language barriers exist, choices may be uninformed or incompletely understood. For older white women, the absence of a caregiver, attributable to the more common lack of a spouse, partner, or other family member to provide care, may result in placement in a SNF rather than an IRH. Further research is necessary to clarify the contribution of cultural, linguistic, and other factors to decisions about PAC and stroke rehabilitation made by patients, families, physicians and other care providers.
In addition, further research is necessary to investigate whether the severity of the stroke or the rate of recovery from stroke varies across these populations. Factors other than stroke severity may contribute to LOS and, in ongoing research of the authors, the National Institutes of Health Stroke Scale [23] is being used as an impairment measure so that groups can be stratified for further investigation of disparities and outcomes.
Kaiser Permanente health system’s regional and national offices have dedicated substantial resources to the identification and elimination of health care disparities through national and regional initiatives and research [24]. This study will provide the basis for subsequent research and programmatic initiatives to further understand and ameliorate health care disparities within the health system. Geographic factors obviously played a role in access to care in our study, ie, the greater access to SNF beds than IRH beds in rural areas and areas not as close to the IRH facility, even though it was centrally located. The number of IRH beds in contrast to available SNF beds did play a role, as predicted, in the numbers of patients served in these settings [25].
The findings in this study may not be generalizable to other health systems or other geographic regions. Differences among fee-for-service and managed health care in both utilization and outcomes of stroke patients have been demonstrated in previous studies [26]. Racial/ethnic disparities in the delivery of health care services have been demonstrated to vary geographically, and variation in care practices do not fully explain these disparities [27]. Further identification and investigation of provider and patient characteristics (including patient severity of illness and co-morbidities) within a health system such as this one will be necessary to fully explain the reasons for these disparities. Ethnic designations within data sets may be fraught with errors as the result of misclassifications and missing data, resulting in limitations to research in disparities. This problem is one that is identified in other health care systems such as the Veterans Administration system [28]. In addition, the racial/ethnic groupings are quite broad in this and other studies (particularly for Asian and Hispanic populations), and further studies of subpopulations would be useful to identify the role of cultural and linguistic factors that may influence patient choice and access to rehabilitation services among these diverse groups.
As Buntin points out, nonclinical factors clearly affect PAC utilization, and access to care may be caused by a lack of clinical consensus about care pathways and appropriate settings of care as well as financial factors [29]. The system under study here is a health system with prepayment financing and capitated rate-setting for Medicare populations, a quite different system of care from most systems in the United States. In addition, the population includes non-Medicare members. Access to care may be influenced by geographic factors, availability of beds for institutional care in IRH and SNF, or other types of care. The direct influence of these factors could not be determined.
When compared with other studies that included Medicare beneficiaries, the rates of treatment in IRH in our health system are lower (11.8%, range, 10.6–13.0 over the time period), with the percentages in three other Medicare studies being 16.2% [30], 26.7% [31], and 21.1% [32]. The authors of these studies also acknowledge the challenges related to investigating the delivery of PAC in multiple settings, and the effects of changes in payment systems that may be influencing decision-making in other health systems during the period of this study.
The reasons for, or the effects of, these differences in utilization is beyond the scope of this study. Clearly, more research is needed to determine the best care settings and care pathways for patients with stroke [33]. Further research into the reasons for variation in care delivery and utilization among culturally and otherwise-diverse populations must address patient and family characteristics, as well as physician/other provider, facility, health system, and financial factors that contribute to decision-making and outcomes after stroke.
Acknowledgments
This study was supported with funding from the Centers for Disease Control and Prevention. Additional resources were provided by the Intramural Research Program (Clinical Center) of the National Institutes of Health, the Centers for Medicare and Medicaid Services, and Kaiser Permanente.
Footnotes
Disclosure Key can be found on the Table of Contents and at www.pmrjournal.org
Contributor Information
M. Elizabeth Sandel, Physical Medicine and Rehabilitation, Napa Solano Service Area, and Research and Training, Kaiser Foundation Rehabilitation Center, 975 Sereno Drive, Vallejo, CA 94589. Disclosure: 8, CDC; 8, NIH.
Hua Wang, Kaiser Foundation Rehabilitation Center, Vallejo, CA Disclosure: nothing to disclose.
Joseph Terdiman, Kaiser Permanente Division of Research, Oakland, CA Disclosure: nothing to disclose.
Jeanne M. Hoffman, University of Washington, Seattle, WA Disclosure: nothing to disclose.
Marcia A. Ciol, University of Washington, Seattle, WA Disclosure: nothing to disclose.
Steven Sidney, Kaiser Permanente Division of Research, Oakland, CA Disclosure: nothing to disclose.
Charles Quesenberry, Kaiser Permanente Division of Research, Oakland, CA Disclosure: nothing to disclose.
Qi Lu, Kaiser Permanente Division of Research, Oakland, CA Disclosure: nothing to disclose.
Leighton Chan, National Institutes of Health, Bethesda, MD Disclosure: 8, NIH.
References
- 1.American Heart Association. [Accessed December 15, 2008]; Available at: www.americanheart.org/downloadable/heart/1200078608862HS_Stats%202008.final.pdf.
- 2.Centers for Disease Control and Prevention. [Accessed December 15, 2008]; Available at: www.cdc.gov/nchs/data/nvsr/nvsr56/nvsr56_10.pdf.
- 3.Cooper R, Cutler J, Desvigne-Nickens P, et al. Trends and disparities in coronary heart disease, stroke, and other cardiovascular diseases in the United States: Findings of the National Conference on Cardiovascular Disease Prevention. Circulation. 2000;102:3137–3147. doi: 10.1161/01.cir.102.25.3137. [DOI] [PubMed] [Google Scholar]
- 4.The Permanente Medicine Guideline: Stroke. Oakland, CA: The Permanente Medical Group; 2008. [Google Scholar]
- 5.Smedley BD, Stith AY, Nelson AR. Unequal Treatment: Confronting Racial and Ethnic Disparities in Healthcare. Washington, DC: National Academies Press; 2002. [PubMed] [Google Scholar]
- 6.Marmot MG. Understanding social inequalities in health. Perspect Biol Med. 2003;46(3 Suppl):S9–23. [PubMed] [Google Scholar]
- 7.Ayala C, Greenlund KJ, Croft JB, et al. Racial/ethnic disparities in mortality by stroke subtype in the United States, 1995–1998. Am J Epidemiol. 2001;154:1057–1063. doi: 10.1093/aje/154.11.1057. [DOI] [PubMed] [Google Scholar]
- 8.Ayala C, Croft JB, Greenlund, et al. Sex differences in US mortality rates for stroke and stroke subtypes by race/ethnicity and age, 1995–1998. Stroke. 2002;33:1197–1201. doi: 10.1161/01.str.0000015028.52771.d1. [DOI] [PubMed] [Google Scholar]
- 9.Stansbury JP, Jia H, Williams LS, Voegl WB, Duncan PW. Ethnic disparities in stroke: Epidemiology, acute care, and postacute outcomes. Stroke. 2005;36:374–387. doi: 10.1161/01.STR.0000153065.39325.fd. [DOI] [PubMed] [Google Scholar]
- 10.Kissela B, Schneider A, Kleindorfer, et al. Stroke in a biracial population: The excess burden of stroke among blacks. Stroke. 2004;35:426–431. doi: 10.1161/01.STR.0000110982.74967.39. [DOI] [PubMed] [Google Scholar]
- 11.Jones MR, Horner RD, Edwards LJ, et al. Racial variation in initial stroke severity. Stroke. 2000;31:563–567. doi: 10.1161/01.str.31.3.563. [DOI] [PubMed] [Google Scholar]
- 12.Horner RD, Hoenig H, Sloane R, Rubenstein LV, Kahn KL. Racial differences in utilization of inpatient rehabilitation services among elderly stroke patients. Stroke. 1997;28:19–25. doi: 10.1161/01.str.28.1.19. [DOI] [PubMed] [Google Scholar]
- 13.Horner RD, Swanson JW, Bosworth HB, et al. Effects of race and poverty on the process and outcome of inpatient rehabilitation services among stroke patients. Stroke. 2003;34:1027–1031. doi: 10.1161/01.STR.0000060028.60365.5D. [DOI] [PubMed] [Google Scholar]
- 14.Kelly PJ, Furie KL, Shafqat S, Rallis N, Chang Y, Stein J. Functional recovery following rehabilitation after hemorrhagic and ischemic stroke. Arch Phys Med Rehabil. 2003;84:968–972. doi: 10.1016/s0003-9993(03)00040-6. [DOI] [PubMed] [Google Scholar]
- 15.Mayer-Oakes SA, Hoenig H, Atchison KA, Lubben JE, De Jong F, Schweitzer SO. Patient-related predictors of rehabilitation use for community-dwelling older Americans. J Am Geriatr Soc. 1992;40:336–342. doi: 10.1111/j.1532-5415.1992.tb02131.x. [DOI] [PubMed] [Google Scholar]
- 16.Gregory PC, Morozova HE, Kuhlemeier KV. Do racial disparities exist in access to inpatient stroke rehabilitation in the state of Maryland? Am J Med Phys Rehabil. 2006;85:814–819. doi: 10.1097/01.phm.0000237870.07136.24. [DOI] [PubMed] [Google Scholar]
- 17.Goldstein LB, Matchar DB, Hoff-Linquist J, Samsa GP, Horner RD. Veterans Administration Acute Stroke (VASt) Study: Lack of race/ethnic-based differences in utilization of stroke-related procedures or services. Stroke. 2003;34:999–1004. doi: 10.1161/01.STR.0000063364.88309.27. [DOI] [PubMed] [Google Scholar]
- 18.Bhandari VK, Kushel M, Price L, Schillinger D. Racial disparities in outcomes of inpatient stroke rehabilitation. Arch Phys Med Rehabil. 2005;86:2081–2086. doi: 10.1016/j.apmr.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 19.Hoenig H, Duncan PW, Horner RD, et al. Structure, process, and outcomes in stroke rehabilitation. Med Care. 2002;40:1036–1047. doi: 10.1097/00005650-200211000-00005. [DOI] [PubMed] [Google Scholar]
- 20.SAS Institute Inc. Base SAS® 9.13 Procedures Guide. 2. 1, 2, 3, and 4. Cary. NC: SAS Institute Inc; 2006. [Google Scholar]; SAS/STAT 9.1 User’s Guide. Cary, NC: SAS Institute Inc; 2004. [Google Scholar]
- 21.Deutsch A, Granger C, Heinemann A. Post stroke rehabilitation: Outcomes and reimbursement of inpatient rehabilitation facilities and subacute rehabilitation programs. Stroke. 2006;37:1477–1482. doi: 10.1161/01.STR.0000221172.99375.5a. [DOI] [PubMed] [Google Scholar]
- 22.Gordon NP. Educational attainment as a mediating influence on racial/ethnic health disparities, or why it is important to capture education as a categorical variable in the electronic medical record. Poster presented at: Bay Area Clinical Symposium; November 16, 2007; San Francisco, CA. [Google Scholar]
- 23.National Institute of Neurological Disorders and Stroke. [Accessed November 3, 2008];Neurology information for doctors and other clinicians. Available at: http://ww-w.ninds.nih.gov/doctors/
- 24.Institute for Health Policy. [Accessed November 3, 2008];Racial and ethnic health disparities: influences, actors, and policy. Available at: http://kpihp.org/publications/docs/disparities.pdf.
- 25.Buntin MB, Garten AD, Paddock S, Saliba D, Totten M, Escarce JJ. How much is post-acute care use affected by its availability? Health Serv Res. 2005;40:413–434. doi: 10.1111/j.1475-6773.2005.00365.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kramer AM, Kowalsky JC, Lin M, Grigsby J, Hughes R, Steiner JF. Outcome and utilization differences for older persons with stroke in HMO and fee for service systems. J Am Geriatr Soc. 2000;48:726–734. doi: 10.1111/j.1532-5415.2000.tb04745.x. [DOI] [PubMed] [Google Scholar]
- 27.Baicker K, Chandra A, Skinner JS. Geographic variation in health care and the problem of measuring racial disparities. Perspect Biol Med. 2005;48(1 Suppl):S42–S53. [PubMed] [Google Scholar]
- 28.Stansbury J, Reid KJ, Reker DM, Duncan PW, Marshall CR, Rittman M. Why ethnic designation matters for rehabilitation research: Comparing VA administrative data and clinical records. J Rehabil Res Dev. 2004;4:269–278. doi: 10.1682/jrrd.2004.04.0046. [DOI] [PubMed] [Google Scholar]
- 29.Buntin MB. Access to postacute rehabilitation. Arch Phys Med Rehabil. 2007;88:1488–1493. doi: 10.1016/j.apmr.2007.07.023. [DOI] [PubMed] [Google Scholar]
- 30.Berg K, Intrator O. Postacute care following stroke or hip fracture. J Aging Health. 1999;11:27–48. doi: 10.1177/089826439901100102. [DOI] [PubMed] [Google Scholar]
- 31.McCall N, Korb J, Petersons A, Moore S. Reforming Medicare payment: Early effects of the 1997 Balanced Budget Act on postacute care. Milbank Q. 2003;81:277–303. doi: 10.1111/1468-0009.t01-1-00054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Buntin M, Escarce J, Hoverman C, Paddock S, et al. Technical Report. Santa Monica, CA: RAND Corporation; 2005. Effects of payment changes on trends in access to post-acute care. [Google Scholar]
- 33.Ward D, Severs M, Dean T, Brooks N. The Cochrane Library. 1. Vol. 2004. Chichester, UK: John Wiley & Sons, Ltd; 2004. Care home versus hospital and own home environments for rehabilitation of older people (Cochrane Review) [DOI] [PubMed] [Google Scholar]