Abstract
Background
We aimed to characterize patterns in the timing of initial emergency procedures for patients with open tibia fracture and examine the relationship between initial procedure timing and in-hospital amputation.
Study Design
Data were analyzed from the Nationwide Inpatient Sample, 2003–2009. Adult patients were included if they had a primary diagnosis code of open tibia fracture. Patients were excluded for the following: transferred from or to another hospital, an immediate amputation was performed, more than one amputation was performed, no emergency procedure was documented, or treated at a facility that did not perform any amputations. We evaluated the association between timing of the first procedure and the outcome of amputation using multiple logistic regression, controlled for patient risk factors and hospital characteristics.
Results
Of 7,560 patients included in the analysis, 1.3% (n=99 patients) underwent amputation on hospital day 2 or later. The majority of patients (52.6%) underwent first operative procedure on day 0 or 1. In adjusted analyses, timing of first operative procedure beyond the day of admission is associated with more than three times greater odds of amputation (day 1 OR 3.81, 95% CI 1.80–8.07).
Conclusions
Delay of first operative procedure beyond the day of admission appears to be associated with a significantly increased probability of amputation in patients with open tibia fracture. All practitioners involved in the management of patients with open tibia fracture should seek a solution for any barrier, other than medical stability of the patient, of achieving early operative intervention.
Keywords: amputation, debridement, emergent procedures, lower extremity reconstruction, lower extremity trauma, open tibial fracture
Advances in bone fixation techniques, vascular reconstruction, and soft tissue replacement make limb salvage possible for injuries that just three decades earlier were only amenable to amputation. Despite innovations in the treatment of severe lower extremity trauma, management of these injuries continues to be challenging and treatment decisions are a topic of debate for physicians and patients. Open fractures are at risk of developing severe complications and the most severe open tibia fractures often lead to amputation. Early operative debridement is considered one of the main factors in minimizing the risk of infection and improving the chance of limb salvage.
Nearly all studies reporting the impact of debridement timing on outcomes in open fracture treatment have evaluated outcomes of infection or nonunion (1–9). Despite the recommendation for emergency debridement in classic teaching and treatment protocols (10–12), the majority of the literature has been unable to show that delay of debridement beyond the six to eight hour window has adverse effects (2–5, 7–9, 13, 14). These findings may have been extrapolated by some providers to justify extending the time to first debridement beyond the day of initial injury. The impact of debridement delayed beyond 24 hours has not been addressed in the literature, and no studies have considered the outcome of amputation after open tibia fracture as a consequence of delayed initial treatment. There are few reports of practice patterns on a national level of timing of emergency procedures beyond what is reported at individual institutions, which are often tertiary care trauma centers (15, 16). Practice patterns in this population are particularly important because patients often receive multidisciplinary care, which may potentially help or hinder provision of prompt treatment.
A population-level analysis is necessary to understand whether providers are effectively treating patients with open tibia fracture on an emergent basis. The aim of this study is to characterize national patterns in the timing of the initial emergency procedures, including operative debridement, for patients with open tibia fracture and to examine whether there is a relationship between timing of the initial operation and the outcome of limb amputation. We hypothesize that performing emergency surgical intervention is not practiced at all centers on a national level, despite the recommendation for emergent treatment of open tibia fractures. In addition, we hypothesize that patients having delayed initial procedures will have an increased probability of amputation.
MATERIALS AND METHODS
Data Source
We performed a retrospective analysis of the Health Care Utilization Project Nationwide Inpatient Sample (NIS) administrative database from the years 2003 – 2009. The NIS is an annual stratified probability sample of approximately 20% of all U.S. non-federal (non-military) hospital admissions from the majority of states (44 states in 2009). The NIS is the largest allpayer inpatient care database, and each year contains approximately 8 million discharges from roughly 1,000 hospitals (17). The NIS has been utilized for many published analyses of national practice patterns and patient outcomes in the surgical literature (18–21). This study was given nonregulatory status by our Institutional Review Board.
Patient Selection
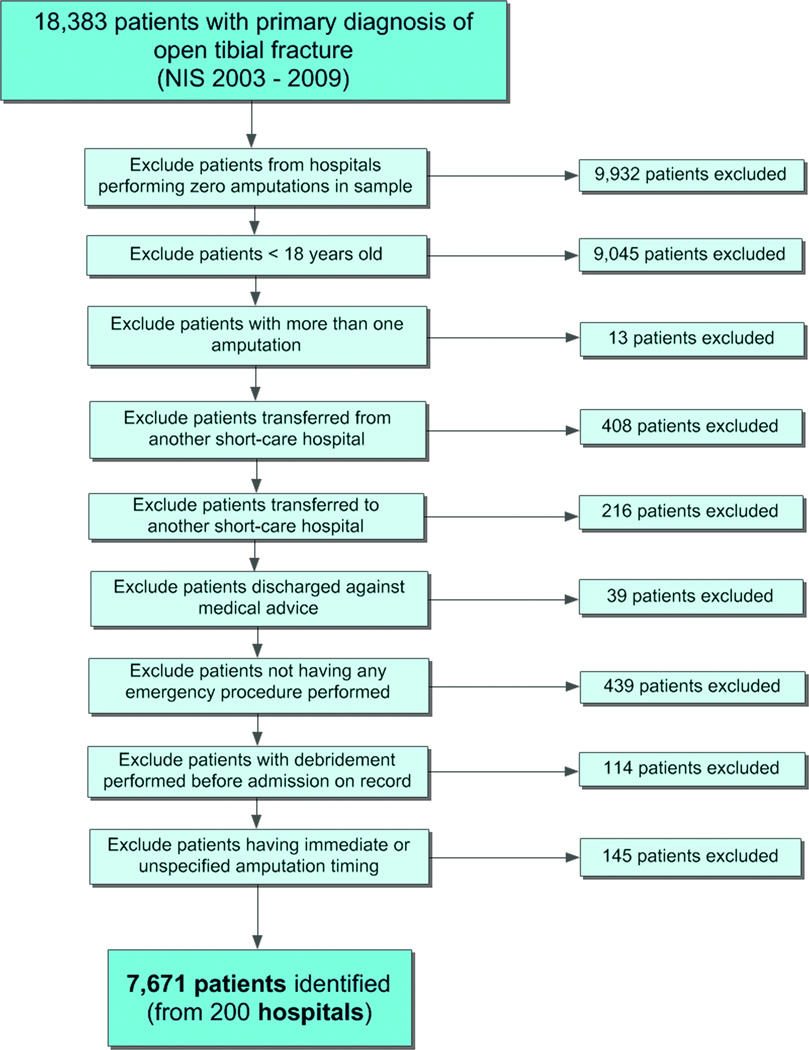
International Classification of Disease, Ninth Revision, Clinical Modification (ICD-9-CM) diagnosis codes were used to identify 18,383 patients with primary diagnosis of open tibia fracture (ICD-9-CM = 823.10, 823.12, 823.30, 823.32, 823.90 or 823.92). The goal was to identify a sample of adult patients admitted near the time of injury (i.e., not transferred from another facility) with acute primary injury of open tibia fracture in which immediate amputation was not performed. We made the assumption that it is rare to perform immediate amputation in patients who have a realistic chance of successful salvage. Thus, patients having immediate amputation on hospital day zero or one were excluded so that patients with the greatest likelihood of successful salvage are considered. In addition, we wanted to capture admissions at the facility that performed the definitive treatment and at facilities that perform amputations as a part of their practice. Patients were excluded from analysis in the following sequence (Figure 1): 8,451 patients treated at a facility that did not perform any amputations in the sample; 887 patients less than 18 years of age; 13 patients having more than one amputation; 408 patients transferred from another short-care hospital; 216 patients transferred to another short-care hospital; 50 patients discharged against medical advice; 439 patients not having any emergency procedure performed during admission; 114 patients with procedures performed before the admission on record (readmissions); and 145 patients having immediate amputation or timing of amputation unspecified. A total of 7,671 patients were identified for analysis.
Figure 1.
Patient selection criteria.
Predictor and Outcome Variables
The NIS database contains ICD-9-CM procedure codes and timing of procedures, measured in calendar days. The outcome of interest was measured as amputation occurring at or below the knee and up to the ankle, which was identified by ICD-9-CM procedure codes outlined in Figure 2. Timing of the initial operative debridement, measured in days since admission, was noted. Because some patients likely have procedures coded other than debridement due to differences in reimbursement, even if debridement was in reality performed, additional emergency procedures were recorded as part of the overall initial operative treatment. Arterial repair, vein repair, nerve repair, placement of external fixator, open reduction and internal fixation, and amputation were also included as emergency procedures in addition to debridement. Timing of the initial emergency procedure was recorded for each patient as the predictor variable of interest. ICD-9-CM procedure codes were used to identify patients having these emergency procedures (Figure 2). Codes for debridement proximal to the knee and distal to the ankle were included in the analysis with the assumption that patients with acute open tibia fracture going to the operating room for debridement of any part of the lower extremity would have debridement of the open fracture as well. Patients having emergency procedures coded but timing unspecified were included in the analysis as a separate category. Patients having no emergency procedure coded were excluded from analysis as mentioned above, because there was no variation in outcome; none of these patients went on to have in-hospital amputation.
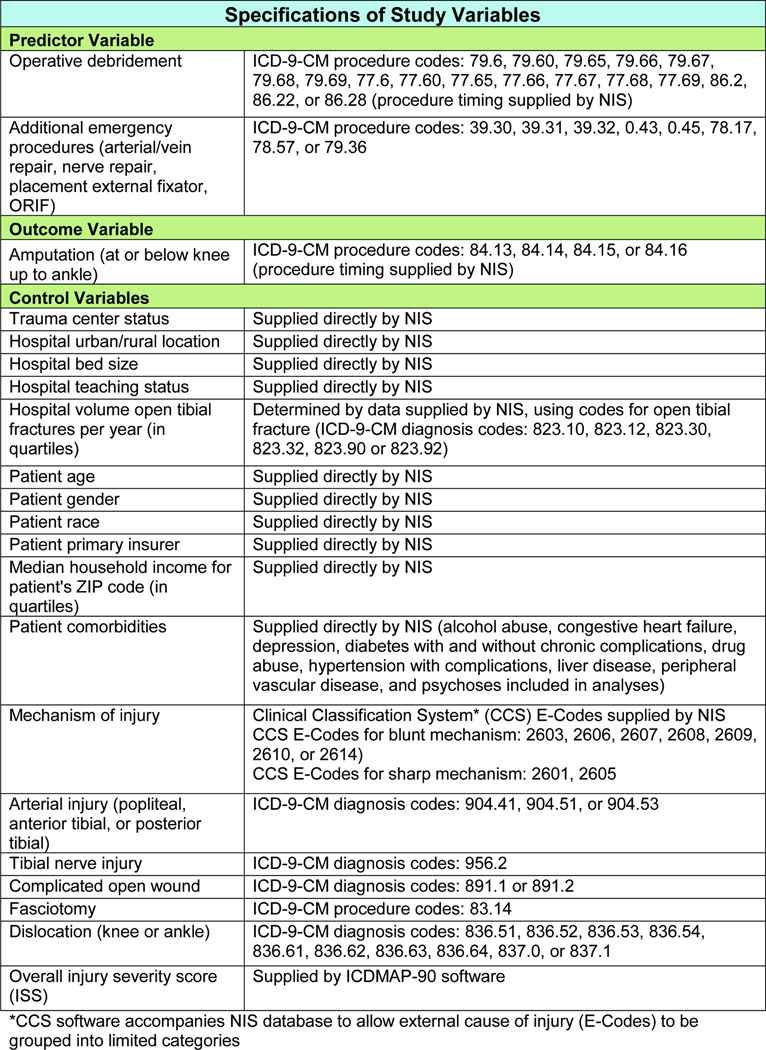
Figure 2.
Specifications of study variables. *CCS software accompanies NIS database to allow external cause of injury (E-Codes) to be grouped into limited categories.
Control Variables
General categories of control variables identified were hospital characteristics, patient demographic data, economic characteristics, comorbidities, and injury characteristics (Figure 2). Hospital characteristics included trauma center status, urban/rural location, bed size, teaching status, and volume of open tibia fractures treated per year in quartiles. Patient demographic data included age, gender, and race. Economic characteristics included primary source of insurance and median household income for the patient’s zip code. Patient comorbidities included alcohol abuse, congestive heart failure, depression, diabetes with and without chronic complications, drug abuse, liver disease, hypertension with complications, peripheral vascular disease, and psychoses. Patients with congestive heart failure, hypertension with complications, and peripheral vascular disease were grouped into one category of cardiac comorbidities. Patients with diabetes and diabetes with chronic complications were grouped into one category of diabetic comorbidities. Injury characteristics included mechanism of injury, the presence of associated injuries, and an overall injury severity score. Using external cause of injury codes (Ecodes), we divided mechanism of injury into blunt, sharp/penetrating, and other/unspecified categories. Associated injuries and procedures included arterial injury (popliteal, anterior tibial, and posterior tibial), complicated open wound, tibial nerve injury, fasciotomy, or dislocation (knee and ankle), which were identified using ICD-9-CM diagnosis and procedure codes (Figure 2). An overall injury severity score was calculated for each observation using the ICDMAP-90 software (Tri-Analytics, Baltimore, MD) (22). The injury severity score (ISS) is commonly used to control for overall injury severity and predict mortality after trauma. The ICDMAP-90 was developed to generate injury severity scores, such as the ISS, from ICD-9-CM codes contained in administrative databases. The program is useful in situations when clinical information for standard calculation of severity scores is not available.
Missing Data
Missing data were accounted for by creating separate “missing” categories within the variable when more than 1% of data were missing. Race (21% missing), trauma center status (10% missing), mechanism of injury (7% missing), and income for patient zip code (4% missing) had separate categories for missing values in order to include these observations in the analysis. An additional 111 observations, 1.4% of the total sample meeting the inclusion criteria, were not included in the final analysis due to having a missing value in the group of control variables that by themselves each had <1% missing. The final sample included 7,560 patients with open tibial fracture.
Data Analysis
We evaluated the association between timing of the initial emergency procedure and the outcome of in-hospital amputation. Initially, bivariate comparisons between control variables and the outcome of amputation were performed. Bivariate logistic regression was used for the continuous variable of age. The remainder of variables were categorical, for which chi-squared test was used. Fisher’s exact test was used when frequencies for any categorical group were less than or equal to five patients. Control variables having significant (P value <0.05) bivariate associations with amputation were included in the final multiple logistic regression model, robustly adjusted for clustered sampling at the hospital level. Findings from the models were used to generate adjusted probabilities of amputation as the outcome. For all analyses, we treated the NIS data as a clinical sample of patients who met the inclusion criteria for this study and did not use statistical weights. The chief rationale for this approach is that we wished to examine patients treated only at hospitals that perform amputations, which is possible when the analysis is performed on unweighted data. Given this approach, our findings should be interpreted as those of a large clinical sample that is national in scope, rather than nationally representative. Statistical analyses were completed using STATA statistical software program (StataCorp LP, College Station, TX).
RESULTS
Characteristics of the Clinical Sample
Of 7,650 patients with open tibial fracture at 200 hospitals, 1.3% (n=99) underwent amputation on hospital day 2 or later (Table 1). The sociodemographic characteristics of patients in the sample are presented in Table 1, comparing patients who underwent amputation versus those who did not. Most patients were treated at teaching (84.3%), nontrauma centers (77.3%), in urban locations (98.3%) (Table 2). In addition, most patients had blunt mechanism of injury (81.5%) (Table 3). Associated arterial and tibial nerve injury were rare in the total sample (2.3% and 0.2% respectively). However, patients undergoing amputation had higher percentages of these associated injuries (Table 3).
Table 1.
Demographic and Economic Characteristics of Patients with Open Tibial Fracture
| Amputation | Salvage | All Patients | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| 99 | 1.3 | 7,461 | 98.7 | 7,560 | 100 | ||
| Demographics | |||||||
| Age | |||||||
| Mean, SD | 46.0 | 16.3 | 40.3 | 15.7 | 40.4 | 15.7 | |
| Gender | |||||||
| Male | 84 | 84.9 | 5,610 | 75.2 | 5,694 | 75.3 | |
| Female | 15 | 15.2 | 1,851 | 24.8 | 1,866 | 24.7 | |
| Race | |||||||
| White | 61 | 61.6 | 3,696 | 49.5 | 3,757 | 49.7 | |
| Black | 11 | 11.1 | 1,014 | 13.6 | 1,025 | 13.6 | |
| Hispanic | 11 | 11.1 | 917 | 12.3 | 928 | 12.3 | |
| Other | 4 | 4.0 | 292 | 3.9 | 296 | 3.9 | |
| Unspecified | 12 | 12.1 | 1,542 | 20.7 | 1,554 | 20.6 | |
| Economic Characteristics | |||||||
| Median household income for ZIP | |||||||
| 1st quartile | 25 | 25.3 | 2,495 | 33.4 | 2,520 | 33.3 | |
| 2nd quartile | 32 | 32.3 | 1,826 | 24.5 | 1,858 | 24.6 | |
| 3rd quartile | 29 | 29.3 | 1,711 | 22.9 | 1,740 | 23.0 | |
| 4th quartile | 10 | 10.1 | 1,148 | 15.4 | 1,158 | 15.3 | |
| Unspecified | 3 | 3.0 | 281 | 3.8 | 284 | 3.8 | |
| Insurance | |||||||
| Uninsured | 22 | 22.2 | 2,578 | 34.6 | 2,600 | 34.4 | |
| Medicare | 15 | 15.2 | 543 | 7.3 | 558 | 7.4 | |
| Medicaid | 16 | 16.2 | 850 | 11.4 | 866 | 11.5 | |
| Private insurance | 46 | 46.5 | 3,490 | 46.8 | 3,536 | 46.8 | |
Table 2.
Hospital Characteristics of Patients Treated with Open Tibial Fracture
| Amputation | Salvage | All Patients | ||||||
|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |||
| 99 | 1.3 | 7,461 | 98.7 | 7,560 | 100 | |||
| Admission type | ||||||||
| Trauma center | 20 | 20.2 | 971 | 13.0 | 991 | 13.1 | ||
| Nontrauma center | 69 | 69.7 | 5,774 | 77.4 | 5,843 | 77.3 | ||
| Unspecified | 10 | 10.1 | 716 | 9.6 | 726 | 9.6 | ||
| Location | ||||||||
| Urban | 94 | 95.0 | 7,338 | 98.4 | 7,432 | 98.3 | ||
| Rural | 5 | 5.0 | 123 | 1.7 | 128 | 1.7 | ||
| Bed size | ||||||||
| Small | 2 | 2.0 | 81 | 1.1 | 83 | 1.1 | ||
| Medium | 29 | 29.3 | 1,441 | 19.3 | 1,470 | 19.4 | ||
| Large | 68 | 68.7 | 5,939 | 79.6 | 6,007 | 79.5 | ||
| Teaching status | ||||||||
| Nonteaching | 11 | 11.1 | 1,176 | 15.8 | 1,187 | 15.7 | ||
| Teaching | 88 | 88.9 | 6,285 | 84.2 | 6,373 | 84.3 | ||
| # cases open tibial fracture per year by hospital | ||||||||
| 1st quartile (<=21 cases/yr.) | 30 | 30.3 | 1,996 | 26.8 | 2,026 | 26.8 | ||
| 2nd quartile (21 – 35 cases/yr.) | 22 | 22.2 | 1,876 | 25.1 | 1,989 | 25.1 | ||
| 3rd quartile (36 – 57 cases/yr.) | 18 | 18.2 | 1,805 | 24.2 | 1,823 | 24.1 | ||
| 4th quartile (>57 cases/yr.) | 29 | 29.3 | 1,784 | 23.9 | 1,813 | 24.0 | ||
Table 3.
Cmorbidities and Injury Characteristics of Patients with Open Tibial Fracture
| Amputation | Salvage | All Patients | |||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| 99 | 1.3 | 7,461 | 98.7 | 7,560 | 100 | ||
| Comorbidities | |||||||
| Alcohol abuse | 11 | 11.5 | 974 | 13.2 | 985 | 13.2 | |
| Cardiac (CHF, PVD, HTN w/ complications) | 30 | 30.3 | 1,213 | 16.3 | 1,243 | 16.4 | |
| Depression | 7 | 7.3 | 271 | 3.7 | 278 | 3.7 | |
| Diabetes | 16 | 16.2 | 406 | 5.4 | 422 | 5.6 | |
| Drug abuse | 7 | 7.3 | 494 | 6.7 | 501 | 6.7 | |
| Liver disease | 2 | 2.1 | 88 | 1.2 | 90 | 1.2 | |
| Psychoses | 4 | 4.1 | 197 | 2.7 | 210 | 2.7 | |
| Associated injuries/procedures | |||||||
| Arterial injury (popliteal, AT, PT) | 16 | 16.2 | 157 | 2.1 | 173 | 2.3 | |
| Complicated open wound | 9 | 9.1 | 345 | 4.6 | 354 | 4.7 | |
| Tibial nerve injury | 3 | 3.0 | 8 | 0.1 | 11 | 0.2 | |
| Fasciotomy | 12 | 12.1 | 396 | 5.3 | 408 | 5.4 | |
| Dislocation | 1 | 1.0 | 42 | 0.6 | 43 | 0.6 | |
| Injury severity score (ISS) | |||||||
| <10 | 62 | 62.6 | 4,806 | 64.4 | 4,868 | 64.4 | |
| 10–20 | 30 | 30.3 | 2,056 | 27.6 | 2,086 | 27.6 | |
| >20 | 7 | 7.1 | 599 | 8.0 | 606 | 8.0 | |
| Mechanism of injury | |||||||
| Blunt | 83 | 83.8 | 6,078 | 81.5 | 6,161 | 81.5 | |
| Sharp/penetrating | 4 | 4.0 | 529 | 7.1 | 533 | 7.1 | |
| Other | 5 | 5.1 | 327 | 4.4 | 332 | 4.4 | |
| Unspecified | 7 | 7.1 | 527 | 7.1 | 534 | 7.1 | |
Day of Initial Emergency Procedure and Limb Amputation
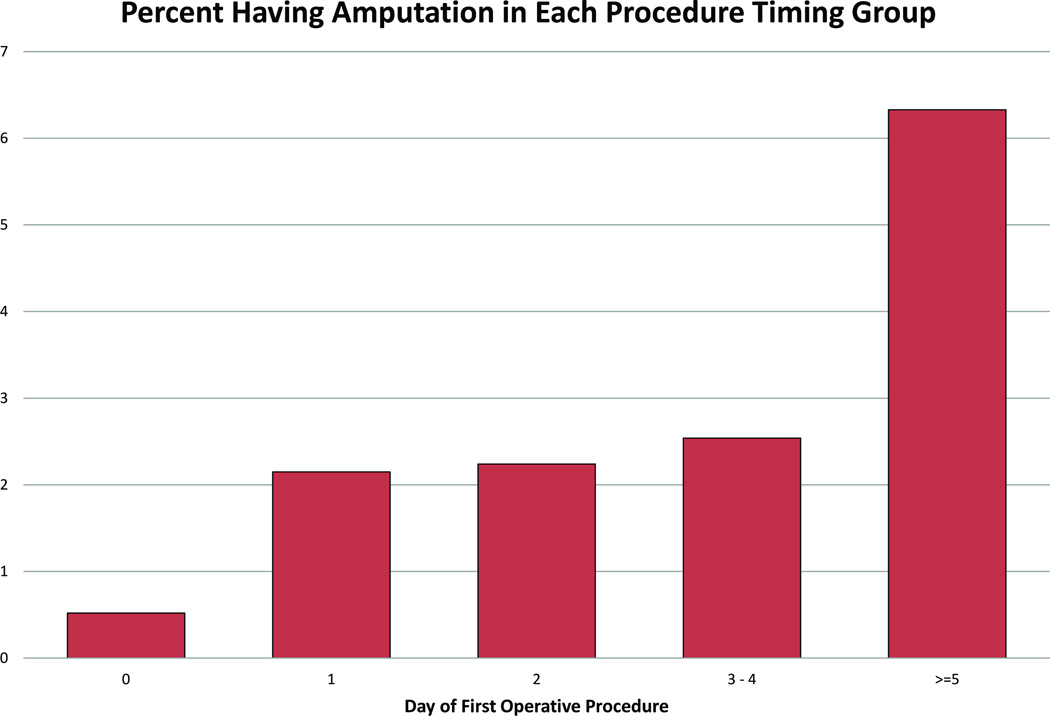
The majority of patients (52.6%) underwent initial emergency procedure on hospital day 0 or 1 (Table 4). Smaller proportions of patients underwent an initial procedure between hospital days 2 – 4 (10.5%) or beyond 4 days after admission (7.9%). Approximately thirty-percent of patients (29.0%) did not have timing of the emergency procedure documented. We found that the percent of patients undergoing amputation increases as the time to initial procedure increases (Figure 3). 0.5% of patients having emergency procedure on day 0 versus 6.3% of patients having initial procedure after day 4 had in-hospital amputation.
Table 4.
Timing of First Emergency Procedure in Patients with Open Tibial Fracture
| Amputation | Salvage | All Patients | ||||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| 99 | 1.3 | 7,461 | 98.7 | 7,560 | 100 | |
| Days to first emergency procedure | ||||||
| HD #0 | 16 | 16.16 | 3077 | 41.2 | 3093 | 40.91 |
| HD #1 | 19 | 19.19 | 863 | 11.6 | 882 | 11.67 |
| HD #2 | 9 | 9.09 | 392 | 5.3 | 401 | 5.3 |
| HD #3–4 | 10 | 10.1 | 384 | 5.2 | 394 | 5.21 |
| HD #5 or greater | 38 | 38.38 | 562 | 7.5 | 600 | 7.94 |
| Timing unspecified | 7 | 7.07 | 2183 | 29.3 | 2190 | 28.97 |
Figure 3.
Percentage of patients having amputation in each emergency procedure timing group.
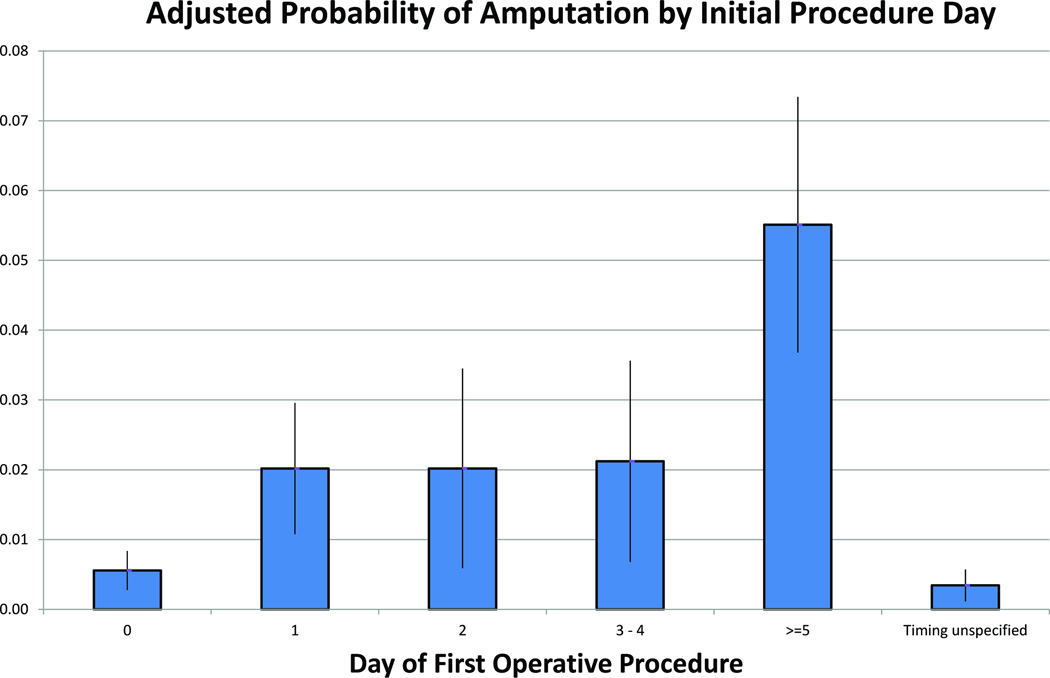
In analyses adjusted for patient and hospital characteristics and clinical risk factors, timing of the first operative procedure on hospital day 1 or later is associated with more than three times greater odds of amputation (day 1 odds ratio [OR] 3.81, 95% CI 1.80–8.07) compared to patients having initial procedures on hospital day 0 (Table 5). The odds of amputation continue to increase as timing of the initial operative procedure is delayed (day 2 OR 3.82, CI 1.51–9.64; day 3–4 OR 4.02, CI 1.83–8.83; day >4 OR 11.42, CI 5.93–21.99). Having timing of procedure unspecified was not associated with significantly increased odds of amputation (OR 0.61, CI 0.25–1.48). As anticipated, associated injuries of arterial and tibial nerve injury have increased odds of amputation. Meanwhile, urban hospitals have decreased odds of amputation. These findings help to validate our model and are concordant with what clinicians would anticipate from experience and prior studies. When accounting for control variables, including injury severity, the marginal probability of amputation increases from 0.6% if initial procedures are performed on day 0 to 2.0–2.1% if initial procedures are performed on day 1–4, increasing to 5.6% if the initial procedure is performed day 5 or later (Figure 4).
Table 5.
Adjusted Multiple Logistic Regression Results
| Multiple Logistic Regression* | |||
|---|---|---|---|
| n = 7,560 | |||
| OR** | 95% CI | P | |
| Demographics | |||
| Age (unit = 10 years) | 1.177 | 0.998–1.388 | 0.054 |
| Gender | |||
| Male | Reference group | ||
| Female | 0.407 | 0.244–0.680 | 0.001 |
| Economic Characteristics | |||
| Insurance | |||
| Uninsured | 0.681 | 0.413–1.123 | 0.132 |
| Medicare | 1.571 | 0.823–2.997 | 0.171 |
| Medicaid | 1.477 | 0.778–2.804 | 0.233 |
| Private insurance | Reference group | ||
| Treatment Characteristics | |||
| Days to first emergency procedure | |||
| HD #0 | Reference group | ||
| HD #1 | 3.814 | 1.801–8.074 | <0.001 |
| HD #2 | 3.816 | 1.511–9.638 | 0.005 |
| HD #3–4 | 4.023 | 1.832–8.832 | 0.001 |
| HD #5 or greater | 11.417 | 5.928–21.991 | <0.001 |
| Timing unspecified | 0.611 | 0.251–1.484 | 0.276 |
| Patient/Injury Characteristics | |||
| Injury severity score (ISS) | |||
| <10 | Reference group | ||
| 10 – 20 | 1.067 | 0.712–1.600 | 0.754 |
| >20 | 0.714 | 0.318–1.602 | 0.414 |
| Comorbidities | |||
| Diabetes | 2.599 | 1.115–6.058 | 0.027 |
| Cardiac (CHF, PVD, HTN w/ complications) | 1.106 | 0.548–2.234 | 0.778 |
| Associated injuries/procedures | |||
| Arterial injury (popliteal, AT, PT) | 7.279 | 3.446–15.376 | <0.001 |
| Tibial nerve injury | 15.669 | 1.950–125.927 | 0.010 |
| Complicated open wound | 1.664 | 0.928–2.984 | 0.087 |
| Fasciotomy | 1.111 | 0.434–2.842 | 0.827 |
| Hospital Characteristics | |||
| Admission type | |||
| Trauma center | 1.390 | 0.872–2.215 | 0.167 |
| Nontrauma center | Reference group | ||
| Unspecified | 1.049 | 0.559–1.971 | 0.881 |
| Location | |||
| Rural | Reference group | ||
| Urban | 0.280 | 0.137–0.570 | <0.001 |
| Bed size | |||
| Small | 2.655 | 0.590–11.942 | 0.203 |
| Medium | 1.844 | 1.098–3.095 | 0.021 |
| Large | Reference group | ||
grey boxes indicate nonsignificant odds ratio
All odds ratios (OR) adjusted for patient demographic, economic, injury risk factors, and hospital control variables that appear in Figure 2.
Figure 4.
Adjusted marginal probability of amputation in each emergency procedure timing group (vertical lines represent 95% confidence interval of estimates).
DISCUSSION
The findings of this national study over a 7-year period indicate that delay of the first operative procedure is associated with a significantly increased probability of amputation in patients with open tibial fracture. Based on our findings, patients who do not have immediate amputation and who are medically stable for surgery should undergo debridement on the day of admission to reduce the probability of amputation. Plastic surgeons should be involved in care immediately, rather than days after admission, to ensure proper steps have been taken to maximize successful outcome.
Despite the preference for limb salvage by patients and physicians (23, 24), some patients clearly benefit from amputation over reconstruction, and we have learned from prior studies that the average patient has similar functional outcome after amputation compared to limb salvage (25, 26). It is clear from clinical experience that not all amputations are avoidable, even for cases in which early intervention is performed. However, despite the widely accepted practice of emergency treatment of open fractures (10, 27), it appears that at least 30% of patients in our national sample had initial procedures performed on hospital day 1 or later. These results are similar to findings in a recent population study by Namdari et al. (16) that reported 24% of open tibial fracture patients in the National Trauma Data Bank experienced wait time to treatment greater than 24 hours. Patient injury severity may partially account for the delay in initial operative intervention. However, we controlled for overall injury severity score and limited our analysis to patients with primary diagnosis of open tibial fracture to minimize bias of associated traumatic injury on timing of procedures. We hypothesize that hospital or physician culture, practice patterns, and resource limitations likely play a role in determining initial operative timing in these patients. For example, some patients may have bedside irrigation of open fractures performed in the emergency department with delay of additional operative procedures the following day when treating surgeons are available. Such practices may be associated with higher probability of amputation. Contributing factors leading to delay at the provider and facility levels merit further examination, and are beyond the scope of this study. However, a growing body of literature has reported poor adherence to practice guidelines when the passive dissemination of information is employed, such as publishing clinical practice guidelines or studies (28, 29).
This study has limitations inherent in the analysis of administrative data, such as the retrospective nature and absence of accompanying detailed clinical data. Unique to this database, there is lack of longitudinal continuity beyond the admission on record. Thus, we were unable to capture late amputations or other late complications such as osteomyelitis. Late amputations occurred in approximately 3% of patients in the attempted reconstruction group of the Lower Extremity Assessment Project (LEAP) study, the largest prospective longitudinal multicenter study to date (25). We would expect this proportion to be lower in our national sample because our sample included all open tibia fracture types, whereas the LEAP study included only severe open tibia fractures. In addition, the timing of the initial procedure was recorded in calendar days rather than hours. Despite this limitation, we are able to add to current knowledge surrounding delayed treatment in open fracture treatment, as the current literature does not address consequences of delay beyond 24 hours or the relationship between delay and limb amputation.
Another limitation is that we were constrained to using ICD-9-CM diagnosis and procedure codes to control for injury severity. As a consequence, we were unable to classify the open tibia fractures according to the commonly used Gustilo grading system (11). However, we were able to control for arterial injury, nerve injury, and presence of a complex wound based on available ICD-9-CM codes, which account for the most severe types of open tibia fractures. Unfortunately, we are unable to distinguish the precise severity of soft tissue injury with presence of the complex wound diagnosis. Lastly, we could not consider patient social and psychological factors, such as family support and self-efficacy, which may impact the decision to pursue reconstruction versus amputation. In the literature these factors have been shown to impact functional outcomes after either treatment (25, 26, 30). However, patient social and psychological factors have not been shown to impact the decision to perform amputation over limb salvage in the literature. Demonstration of the relationship between delay of treatment and increased probability of amputation can be strengthened in the future through separate analysis of another independent national data source or analysis of individual institution’s outcomes of open tibial fractures. However, review of data from institutions that do not treat large numbers of patients with open tibial fractures may not have sufficient power to fully evaluate the relationship.
Despite the limitations of this study, we were able to demonstrate a relationship between delay in initial operative intervention and an increased probability of amputation in patients with open tibia fracture. Hospitals and clinical departments treating these patients should examine practice patterns and limitations in being able to achieve early treatment. Medical stability is the only reason for delay that is in the best interest of the patient. All practitioners involved in managing these patients should seek a solution for any other barrier to achieving early operative intervention in order to prevent unnecessary amputation that may be attributed to delay in operative management. Changes in the process of care, such as immediate plastic surgery consultation and performing immediate operative intervention in medically stable patients, are unlikely to cause harm; rather these changes offer the potential to improve the likelihood of successful limb salvage.
ACKNOWLEDGMENTS
We would like to thank Dr. Rodney Hayward for methodological input and Bradley Larson for his assistance with preparation of tables.
Disclosure: Support for this study was provided by a grant from the Robert Wood Johnson Foundation Clinical Scholars Program/VA Scholar (to Dr. Erika Davis Sears) and by a Midcareer Investigator Award in Patient-Oriented Research (K24 AR053120) (to Dr. Kevin C. Chung).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Dellinger EP, Miller SD, Wertz MJ, et al. Risk of infection after open fracture of the arm or leg. Arch Surg. 1988;123:1320–1327. doi: 10.1001/archsurg.1988.01400350034004. [DOI] [PubMed] [Google Scholar]
- 2.Harley BJ, Beaupre LA, Jones CA, et al. The effect of time to definitive treatment on the rate of nonunion and infection in open fractures. J Orthop Trauma. 2002;16:484–490. doi: 10.1097/00005131-200208000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Khatod M, Botte MJ, Hoyt DB, et al. Outcomes in open tibia fractures: relationship between delay in treatment and infection. J Trauma. 2003;55:949–954. doi: 10.1097/01.TA.0000092685.80435.63. [DOI] [PubMed] [Google Scholar]
- 4.Merritt K. Factors increasing the risk of infection in patients with open fractures. J Trauma. 1988;28:823–827. doi: 10.1097/00005373-198806000-00018. [DOI] [PubMed] [Google Scholar]
- 5.Noumi T, Yokoyama K, Ohtsuka H, et al. Intramedullary nailing for open fractures of the femoral shaft: evaluation of contributing factors on deep infection and nonunion using multivariate analysis. Injury. 2005;36:1085–1093. doi: 10.1016/j.injury.2004.09.012. [DOI] [PubMed] [Google Scholar]
- 6.Patzakis MJ, Wilkins J. Factors influencing infection rate in open fracture wounds. Clin Orthop Relat Res. 1989:36–40. [PubMed] [Google Scholar]
- 7.Skaggs DL, Friend L, Alman B, et al. The effect of surgical delay on acute infection following 554 open fractures in children. J Bone Joint Surg Am. 2005;87:8–12. doi: 10.2106/JBJS.C.01561. [DOI] [PubMed] [Google Scholar]
- 8.Spencer J, Smith A, Woods D. The effect of time delay on infection in open long-bone fractures: a 5-year prospective audit from a district general hospital. Ann R Coll Surg Engl. 2004;86:108–112. doi: 10.1308/003588404322827491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Webb LX, Bosse MJ, Castillo RC, MacKenzie EJ. Analysis of surgeon-controlled variables in the treatment of limb-threatening type-III open tibial diaphyseal fractures. J Bone Joint Surg Am. 2007;89:923–928. doi: 10.2106/JBJS.F.00776. [DOI] [PubMed] [Google Scholar]
- 10.Giannoudis PV, Papakostidis C, Roberts C. A review of the management of open fractures of the tibia and femur. J Bone Joint Surg Br. 2006;88:281–289. doi: 10.1302/0301-620X.88B3.16465. [DOI] [PubMed] [Google Scholar]
- 11.Gustilo RB, Merkow RL, Templeman D. The management of open fractures. J Bone Joint Surg Am. 1990;72:299–304. [PubMed] [Google Scholar]
- 12.Gustilo RB, Anderson JT. Prevention of infection in the treatment of one thousand and twenty-five open fractures of long bones: retrospective and prospective analyses. J Bone Joint Surg Am. 1976;58:453–458. [PubMed] [Google Scholar]
- 13.Bednar DA, Parikh J. Effect of time delay from injury to primary management on the incidence of deep infection after open fractures of the lower extremities caused by blunt trauma in adults. J Orthop Trauma. 1993;7:532–535. doi: 10.1097/00005131-199312000-00008. [DOI] [PubMed] [Google Scholar]
- 14.Enninghorst N, McDougall D, Hunt JJ, Balogh ZJ. Open tibia fractures: timely debridement leaves injury severity as the only determinant of poor outcome. J Trauma. 2011;70:352–356. doi: 10.1097/TA.0b013e31820b4285. discussion 356–357. [DOI] [PubMed] [Google Scholar]
- 15.Busse JW, Jacobs CL, Swiontkowski MF, et al. Complex limb salvage or early amputation for severe lower-limb injury: a meta-analysis of observational studies. J Orthop Trauma. 2007;21:70–76. doi: 10.1097/BOT.0b013e31802cbc43. [DOI] [PubMed] [Google Scholar]
- 16.Namdari S, Baldwin KD, Matuszewski P, et al. Delay in surgical debridement of open tibia fractures: an analysis of national practice trends. J Orthop Trauma. 2011;25:140–144. doi: 10.1097/BOT.0b013e3181e3dff1. [DOI] [PubMed] [Google Scholar]
- 17. [Accessed: November 2011];Introduction to the HCUP Nationwide Inpatient Sample (NIS) 2009 http://www.hcup-us.ahrq.gov/db/nation/nis/NIS_2009_INTRODUCTION.pdf.
- 18.Chen MW, Narayan D. Economics of upper extremity replantation: national and local trends. Plast Reconstr Surg. 2009;124:2003–2011. doi: 10.1097/PRS.0b013e3181bf8008. [DOI] [PubMed] [Google Scholar]
- 19.Pacella SJ, Butz DA, Comstock MC, et al. Hospital volume outcome and discharge disposition of burn patients. Plast Reconstr Surg. 2006;117:1296–1305. doi: 10.1097/01.prs.0000204962.85336.51. [DOI] [PubMed] [Google Scholar]
- 20.Curtin CM, Gater DR, Chung KC. Upper extremity reconstruction in the tetraplegic population, a national epidemiologic study. J Hand Surg Am. 2005;30:94–99. doi: 10.1016/j.jhsa.2004.10.007. [DOI] [PubMed] [Google Scholar]
- 21.Juillard C, Lashoher A, Sewell CA, et al. A national analysis of the relationship between hospital volume, academic center status, and surgical outcomes for abdominal hysterectomy done for leiomyoma. J Am Coll Surg. 2009;208:599–606. doi: 10.1016/j.jamcollsurg.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 22.MacKenzie EJ, Sacco WJ. ICDMAP-90 Software: User's Guide. Baltimore, Maryland: Johns Hopkins University and Tri-Analytics, Inc.; 1998. pp. 1–28. [Google Scholar]
- 23.Chung KC, Shauver MJ, Saddawi-Konefka D, Haase SC. A decision analysis of amputation versus reconstruction for severe open tibial fracture from the physician and patient perspectives. Ann Plast Surg. 2011;66:185–191. doi: 10.1097/SAP.0b013e3181cbfcce. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Parrett BM, Matros E, Pribaz JJ, Orgill DP. Lower extremity trauma: trends in the management of soft-tissue reconstruction of open tibia-fibula fractures. Plast Reconstr Surg. 2006;117:1315–1322. doi: 10.1097/01.prs.0000204959.18136.36. [DOI] [PubMed] [Google Scholar]
- 25.Bosse MJ, MacKenzie EJ, Kellam JF, et al. An analysis of outcomes of reconstruction or amputation after leg-threatening injuries. New England Journal of Medicine. 2002;347:1924–1931. doi: 10.1056/NEJMoa012604. [DOI] [PubMed] [Google Scholar]
- 26.MacKenzie EJ, Bosse MJ, Pollak AN, et al. Long-term persistence of disability following severe lower-limb trauma. Results of a seven-year follow-up. J Bone Joint Surg Am. 2005;87:1801–1809. doi: 10.2106/JBJS.E.00032. [DOI] [PubMed] [Google Scholar]
- 27.Management of complex extremity trauma. [Accessed July 2011];American College of Surgeons Committee on Trauma. 2005 http://www.facs.org/trauma/publications/mancompexttrauma.pdf.
- 28.Ansari M, Shlipak MG, Heidenreich PA, et al. Improving guideline adherence: a randomized trial evaluating strategies to increase beta-blocker use in heart failure. Circulation. 2003;107:2799–2804. doi: 10.1161/01.CIR.0000070952.08969.5B. [DOI] [PubMed] [Google Scholar]
- 29.Prior M, Guerin M, Grimmer-Somers K. The effectiveness of clinical guideline implementation strategies--a synthesis of systematic review findings. J Eval Clin Pract. 2008;14:888–897. doi: 10.1111/j.1365-2753.2008.01014.x. [DOI] [PubMed] [Google Scholar]
- 30.Ly TV, Travison TG, Castillo RC, et al. Ability of lower-extremity injury severity scores to predict functional outcome after limb salvage. J Bone Joint Surg Am. 2008;90:1738–1743. doi: 10.2106/JBJS.G.00136. [DOI] [PMC free article] [PubMed] [Google Scholar]