Abstract
Background
Among individuals with schizophrenia, deficits in theory of mind (ToM) skills predict poor social functioning. Therefore, identifying the neural basis of ToM may assist the development of treatments that improve social outcomes. Despite growing evidence that the ventromedial prefrontal cortex (VMPFC) facilitates ToM skills among healthy individuals, methodological challenges, such as the influence of general cognitive deficits, have made it difficult to identify the relationship between ToM processing and VMPFC function in schizophrenia.
Methods
We used voxel-based morphometry (VBM) and a multi-method behavioral assessment of ToM processing, including performance-based (Recognition of Faux Pas Test), self-report (Interpersonal Reactivity Index, Perspective-Taking), and interview-rated (Quality of Life Scale–Empathy score) ToM assessments, to investigate whether ToM skills were related to VMPFC gray matter volume (GMV). Standardized neuropsychological measures were used to assess global cognition. 21 schizophrenia and 17 healthy control subjects participated.
Results
Between-group behavioral analyses showed that, as compared to healthy participants, schizophrenia participants had worse ToM performance and lower self-reported ToM processing in daily life. The between-group analysis of GMV showed that schizophrenia participants had less VMPFC GMV than healthy participants. Moreover, among schizophrenia participants, all three measures of ToM processing were associated with VMPFC GMV, such that worse ToM skills were related to less VMPFC GMV. This association remained strong for self-reported and interview-rated ToM skills even when controlling for the influence of global cognition.
Conclusions
The findings suggest that among individuals with schizophrenia, reduced VMPFC GMV is specifically associated with deficits using ToM skills to enhance social relationships.
Keywords: mentalizing, theory of mind, empathy, schizophrenia, social functioning, MRI
Introduction
Social dysfunction is a disabling clinical feature of schizophrenia that often persists despite treatment(1-2). Although tremendous resources are devoted to improving this aspect of illness, such efforts are hampered by limited knowledge regarding the underlying neural mechanisms that support social relationships. Identifying these mechanisms is necessary to develop targeted, effective treatments that improve social functioning among individuals with schizophrenia.
Successful social functioning depends on the capacity to understand how another person’s perspective influences their thoughts, feelings, and behavior. This capacity is operationalized as mentalizing or Theory of Mind (ToM) skills. Developing meaningful interpersonal relationships requires the use of ToM skills, such as perspective-taking, to empathize with others (i.e. cognitive empathy). These advanced ToM skills require the integration of cognitive and affective mentalizing, and can be assessed with behavioral tasks, self-report questionnaires, or interview-based instruments.
Individuals with schizophrenia have severe ToM deficits as demonstrated by poor behavioral performance on advanced ToM tasks, such as recognizing a social faux pas(3-11), as well as self-reports and close-other reports of deficient use of ToM skills, such as perspective-taking, to empathize with others(12-13). These impairments are observable in premorbid, active, and remitted stages of illness(3, 14-16), prospectively predict a schizophrenia diagnosis(17), and uniquely predict social functioning in schizophrenia patients(6, 18-20). These observations suggest that identifying the biological basis of ToM deficits may provide important information about neurocognitive processes for which remediation and treatment could have functional benefits.
Research in healthy individuals demonstrates that ToM skills are supported by a network of brain regions, including dorsal and ventral medial prefrontal cortex (DMPFC/VMPFC), superior temporal cortex(STC), posterior cingulate cortex(PCC), and temporal poles (21-24). Among these, VMPFC may provide the most crucial functions. Neuroimaging studies consistently demonstrate VMPFC activity during ToM tasks(23, 25-26), and VMPFC lesions result in ToM deficits, including the recognition of faux pas(27), as well as self-reports and close-other reports of diminished empathy and perspective-taking in social relationships(27-31).
Schizophrenia is associated with structural and functional abnormalities in the VMPFC(32-34), suggesting that VMPFC dysfunction could contribute to ToM deficits and subsequent consequences in social relationships. However, thus far, evidence for this brain-behavior association is inconclusive. Methodological shortcomings of both neural and behavioral assessments might obscure the underlying relationship between VMPFC and ToM skills.
Most neuroscience-based investigations of ToM processing in schizophrenia collect functional neuroimaging data during performance of a ToM task. Although several studies demonstrate the predicted pattern of less VMPFC activity in schizophrenia versus healthy participants(35), other studies using similar tasks show a different or opposite pattern(36-37). These findings highlight a methodological challenge of using fMRI to understand cognitive deficits in schizophrenia. Neural activity during task performance is influenced by attention and effort-- hypo-activity can reflect lack of attention and hyper-activity can reflect additional effort(38-39). These epiphenomena can obscure true brain-behavior relationships.
Alternatively, structural neural assessments, such as gray matter volume (GMV), are collected independent from task performance, so the neural measurement is not confounded by state effects. Nevertheless, identification of a reliable relationship between VMPFC structure and ToM depends on valid and specific behavioral assessments of ToM skills. This is a challenging requirement. Accuracy on performance-based ToM tasks is partially dependent on general cognitive skills, such as executive function(40), and can be influenced by state effects, such as attention or effort. Furthermore, while some research shows that poor performance on ToM tasks predicts social functioning(6), other studies show no relationship(41). This suggests that while performance-based measures may assess cognitive capacity for ToM, they do not account for the motivation or success in using these skills to enhance social relationships, which may be better evaluated via self-report and interview-based functional assessments. However, standard functional assessments of social relationships often encompass multiple subcomponents of social functioning into one overall functional outcome score. Although certain outcome variables, like marital or occupational status, may depend on ToM skills, they also depend on many other factors that have different neural and environmental influences. Therefore, identifying the neural basis of ToM in schizophrenia requires converging evidence from complementary neuroimaging and behavioral methods.
We address these methodological challenges by investigating the relationship between neural structure and three different behavioral assessments of ToM processing. First, we use optimized voxel-based morphometry (VBM) to investigate the relationship between VMPFC neural structure (i.e. gray matter volume (GMV)) and ToM processing among schizophrenia participants. Second, we use multiple measures of ToM processing, including behavioral performance on an advanced ToM task (Recognition of Faux Pas Test), self-reported tendency to engage in perspective-taking (Interpersonal Reactivity Index Perspective-Taking subscale), and an interview-based assessment of the capacity and tendency to consider the perspectives and emotions of others (Quality of Life Scale-Empathy score). Each measure assesses the ability to integrate both cognitive and affective components of ToM processing in the service of understanding others. Moreover, this multi-method approach addresses not only the cognitive capacity to understand the mental and emotional states of others but also the effectiveness in using that capacity to enhance relationships in daily life. Third, we investigate whether controlling for general cognitive performance influences the relationship between ToM processing and GMV in schizophrenia. Finally, we investigate between-group differences to replicate previously established deficits in schizophrenia and to identify whether the relationship between ToM and GMV is significantly different in schizophrenia than healthy participants. Given prior evidence that schizophrenia is associated with both VMPFC GM loss and ToM deficits on these specific measures, we expect that the relationship between ToM skills and VMPFC GMV will be stronger in schizophrenia.
Methods and Materials
Participants
Participants included 21 volunteers with schizophrenia or schizoaffective disorder and 17 healthy control subjects. Table S1 in Supplement 1 summarizes demographic data. Schizophrenia subjects were recruited from outpatient clinics and community mental health centers. Standardized diagnostic and clinical evaluations were performed by clinical psychology doctoral students and supervised by a clinical psychologist(M.F.) and psychiatrist(S.V.). Diagnosis was assessed with the Structured Clinical Interview for DSM-IV Disorders(42) and information from the subject’s caretaker, medical team, and medical record. Symptom severity was assessed with the Positive and Negative Syndrome Scale-Extended (PANSS-E)(43-44). Functioning was assessed with the Quality of Life Scale-Abbreviated(QLS)(45). IQ was assessed with the Wechsler Abbreviated Scale of Intelligence(WASI)(46). PANSS and QLS interviews were conducted by two assessment personnel; a consensus rating was reached for each item (intraclass correlation coefficients >0.85).
Inclusion criteria were: schizophrenia or schizoaffective disorder, age 18-60 years, primary English-speaker. Exclusion criteria were: neurological or major medical illness, substance dependence within six months, prior head injury.
Healthy participants were screened for psychiatric, neurological and general medical problems with self-report questionnaires and a structured clinical interview that assessed past and present psychiatric symptoms, psychological/psychiatric service-use, medication-use, academic history, and general health. Schizotypy was assessed with the Schizotypal Personality Questionnaire(SPQ)(47). Exclusion criteria were: psychotropic medication-use, past or present psychiatric or neurological disorder, prior head injury, SPQ>30. Screening was conducted by trained research staff and supervised by a clinical psychologist(C.H.). University of California, Berkeley and San Francisco ethical review boards approved the study. Participants gave written informed consent and received payment for participation.
Theory of Mind (ToM) Assessments ToM Performance: The Recognition of Faux Pas Test
The Recognition of Faux Pas Test(27, 48) (henceforth called “FP task”) was used to assess ToM performance. The FP task was chosen because performance depends on VMPFC structural integrity(27, 30-31). Schizophrenia patients have performance deficits(9, 11), and these deficits are correlated with VMPFC-mediated cognitive processes(9). The FP task assesses the ability to recognize and understand when someone unintentionally says or does something that hurts or offends another person. Successful performance requires the use of perspective-taking to understand the speaker’s knowledge and listener’s feelings. The original task was divided into two forms containing 10 social scenarios (5 scenarios contained a faux pas). (Two forms were created for later use in a treatment study; there were no performance differences between the two forms). The experimenter read each scenario out-loud. Participants referred to a printed copy, as necessary, to minimize memory demands.
Participants received a Faux Pas (FP) score for recognizing and understanding faux pas and a Content score for understanding story facts. Recommended scoring procedures were followed(27).
Example FP scenario:
Helen’s husband was throwing a surprise party for her birthday. He invited Sarah, a friend of Helen’s, and said, “Don’t tell anyone, especially Helen.” The day before the party, Helen was over at Sarah’s and Sarah spilled some coffee on a new dress that was hanging over her chair. “Oh!” said Sarah, “I was going to wear this to your party!” “What party?” said Helen. “Come on,” said Sarah, “Let’s go see if we can get the stain out.”
FP Question: Did anyone say something they shouldn’t have said or something awkward?
If “yes”, ask follow-up questions. If “no” skip to Content questions:
Who said something they shouldn’t have said or something awkward?
Why shouldn’t he/she have said it or why was it awkward?
Why do you think he/she said it?
Did Sarah remember that the party was a surprise party?
How do you think Helen felt?
Content questions:
In the story, who was the surprise party for?
What got spilled on the dress?
For FP scenarios, correct detection of faux pas and each follow-up question was worth 1 point each. For non-FP scenarios, correct rejection of faux pas was awarded 2 points and no follow-up questions were asked. Misidentification of a faux pas (when none had occurred) was awarded zero points and follow-up questions were asked but not scored. The FP Score included performance on all scenarios (FP+non-FP), excluding Content scores. Content scores included performance on content questions (1 point each) for all scenarios.
ToM Self-Report: Interpersonal Reactivity Index, Perspective-Taking Subscale
The Interpersonal Reactivity Index (IRI)(49-50) is a 28-item self-report questionnaire with 4 subscales assessing different components of empathy. The Perspective-Taking subscale assesses the tendency to use ToM skills (perspective-taking) in interpersonal relationships. VMPFC lesion patients demonstrate low Perspective-Taking scores(28, 51) and Perspective-Taking scores are correlated with FP task performance(30-31). Schizophrenia participants have lower than normal Perspective-Taking scores(13, 52), and their Perspective-Taking scores are correlated with performance on VMPFC-mediated cognitive processes(52). Example items (rated 0-4) include: “I try to look at everybody’s side of a disagreement before I make a decision,” and “When I’m upset at someone, I usually try to ‘put myself in his shoes’ for a while.” Item ratings are summed for each subscale. All subscales described in Supplement 1.
ToM Interview-Rated: Quality of Life Scale-Empathy Score
The Empathy score of the Quality of Life Scale–Abbreviated(45, 53) was used to assess interviewer-rated ToM skills. The QLS–Abbreviated is a 7-item semi-structured clinical interview to assess empathy, motivation, anhedonia, interpersonal relations (number of acquaintances, social initiative), occupational functioning, and environmental engagement. For each item, the participant is asked several questions by an interviewer who then determines a rating on a 0-6 scale. The Empathy score assesses the “capacity to regard and appreciate another person’s situation as different from his own – to appreciate different perspectives, affective states and points of view”(45). A 0 rating indicates “no capacity to consider the views and feelings of others;” a 6 rating indicates “spontaneously considers the other person’s situation in most instances, can intuit the other person’s affective responses, and uses this knowledge to adjust his own response”. The QLS was designed specifically for schizophrenia research, so this measure was not used with healthy participants.
Global-Cognition
Global-Cognition was assessed with the Measurement and Treatment Research to Improve Cognition in Schizophrenia (MATRICS) battery(54). All MATRICS-recommended cognitive domains were assessed except attention (due to soft-ware difficulties). Raw scores were converted to age-adjusted z-scores, and a Global-Cognition composite score was computed as the average z-score across all measures.
Magnetic Resonance Imaging
High resolution T1-weighted structural magnetic resonance (MR) images were acquired with a Varian INOVA 4T-scanner using an oblique-axial magnetization-prepared fast low-angle shot high-resolution (MPFLASH) sequence: [TR=9ms, TE=5ms, FOV=22.4cm×22.4cm×19.8cm, matrix size=256×256×128, resolution=0.875mm×0.875mm×1.55mm].
MR images were processed with voxel-based morphometry (VBM)(55) in Statistical Parametric Mapping (SPM8) using the recommended processing sequence(56). Images were reoriented to the intercommissural plane, segmented into gray and white matter (GM,WM) tissues, normalized, resliced (2×2×2mm3 voxels), modulated with Jacobian determinants, and smoothed 8mm full-width-at-half-maximum. Modulation was used to retain the same gray matter volume as the original (non-normalized) images(56-57). An 8mm smoothing kernel was used because larger kernels (10-12mm) can miss group differences in small structures, whereas smaller kernels (4-6mm) can produce false positive findings(32, 58). Normalized, modulated, smoothed images were submitted to group-level analyses.
Statistical Analyses
Between-Group Differences
Repeated Measures ANOVA and Independent Samples T-tests were used to test for differences between schizophrenia and healthy participants on behavioral ToM measures. Because these tests were conducted to replicate prior findings, results are considered significant at p<.05 (one-tailed).
Regional differences in GMV between schizophrenia and healthy participants were investigated across the whole-brain using a two sample t-test with total intracranial volume (TIV) and global signal intensity as nuisance variables(59-60). TIV (sum of GM, WM, and cerebral spinal fluid) was calculated on each subject and included as a nuisance variable at the second level. Variance in global signal intensity across scans was controlled for with the ANCOVA option for global normalization in the second-level model. The statistical threshold was p<.05, whole-brain Family Wise Error (FWE) correction, 20voxel/160mm extent.
Regression Analyses
Pearson bivariate correlations were used to examine relationships between behavioral variables.
To identify regions where GMV loss in schizophrenia was related to ToM skills, multiple regression analyses were conducted within the schizophrenia group. Separate multiple regressions were conducted for each ToM variable: FP Score; IRI Perspective-Taking; and QLS-Empathy. In each regression, the behavioral score was the covariate of interest predicting GMV while controlling for TIV and global signal intensity. The regression analysis for FP Score also controlled for Content Score. Regressions for FP Score and IRI Perspective-Taking were conducted among healthy participants. To verify that the findings in schizophrenia were not explained by variation in general cognition, each regression was conducted controlling for MATRICS Global-Cognition score. To identify whether the findings were specific to schizophrenia, we investigated the interaction between Group (SZ/HC) and ToM GMV correlation by conducting two ANOVA analyses: Group*FP Score and Group*IRI Perspective-Taking.
The statistical threshold was p<.001, uncorrected for multiple comparisons. A VMPFC region of interest ‘mask’ was created in WFU PickAtlas(61-62) with boundaries defined according to recent literature(25, 63-65) (Figure 1A). Small volume correction (FWE, p<.05) was conducted for right/left VMPFC.
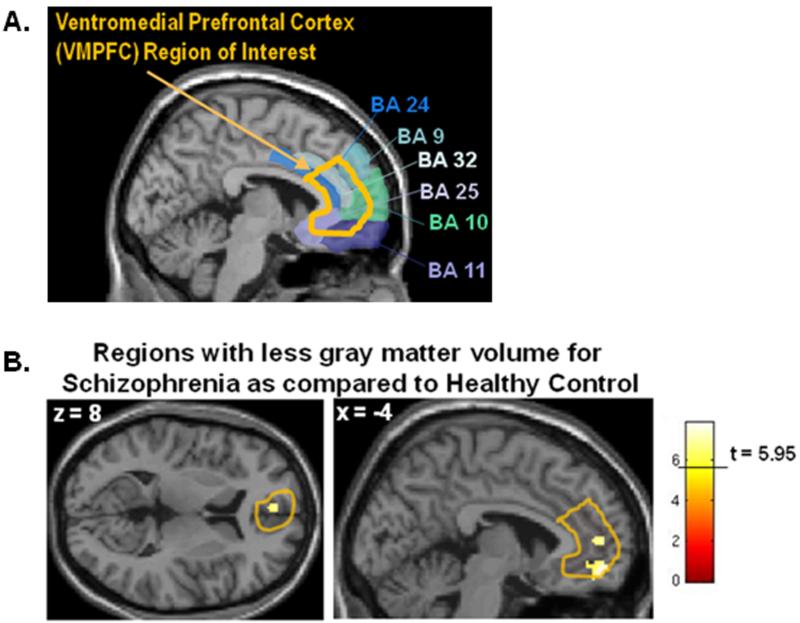
Figure 1.
A. The orange outline shows ventromedial prefrontal cortex (VMPFC) region of interest (ROI) mask. The VMPFC mask includes the anterior and ventral portions of the anterior cingulate as it wraps around the genu of the corpus collosum (Brodmann’s Areas (BA) 24, 25), extending anteriorly to include the cingulate sulcus and paracingulate gyri (BA 32), as well as the inferior, medial portions of the superior frontal gyrus (BA 9, 10, 11). The most superior portion of the ROI mask drawn here is also referred to as medial prefrontal cortex (MPFC) in the literature. Boundaries for Brodmann’s areas are taken from the MRIcron (http://www.cabiatl.com/mricro/mricron/index.html) Brodmann template.
B. Between group comparison of schizophrenia and healthy control participants. Yellow clusters are regions where schizophrenia participants show less gray matter than healthy control participants within the ventromedial prefrontal cortex (VMPFC) region of interest (ROI) mask (outlined in orange).
Results
Behavioral Results
Table S1 in Supplement 1 shows all behavioral results. Schizophrenia participants were significantly worse than healthy participants at understanding faux pas. Repeated measures ANOVA showed a significant Group (SZ/HC) by Question type (Faux Pas/Content) interaction, such that schizophrenia participants were significantly worse than healthy participants at understanding faux pas but not factual content [Reported as %Correct Mean(SD). Schizophrenia: FP=70(20), Content=93(12); Healthy: FP=94(9), Content: 96(6); Group*Question interaction: F=13.99, p=.001]. Schizophrenia participants also reported less perspective-taking (IRI Perspective-Taking) than healthy participants [Schizophrenia: Perspective-Taking=17.05(4.68), Healthy: Perspective-Taking =19.73(4.46), t=1.71, p=.048 (one-tailed)]. QLS-Empathy score was 4.14(1.11) for schizophrenia participants. These results are similar to previous findings on these measures(9, 13, 52).
Bivariate correlations were used to investigate whether the ToM measures were related to one another and/or to global-cognition among schizophrenia participants. There were no significant correlations between the three ToM measures among schizophrenia participants; however, IRI Perspective-Taking was related to FP Score at trend-level (r=.40, p=.08), and non-significantly to QLS-Empathy (r=.35, p=.1). These non-significant findings could be due to small sample size; power analyses on these data indicated that N=45 is necessary to show a significant relationship between these variables at p<.05 (two-tailed). There was no relationship between FP Score and QLS-Empathy (r=.004, p=.99). Global-cognition was significantly related to FP Score (r=.57, p=.007), but not IRI Perspective-Taking (r=.31, p=.18) or QLS-Empathy (r=−.11, p=.62). None of the ToM variables were related to symptom severity (PANSS Positive, Negative, and Disorganized subscales). Among healthy participants, FP Score was not related to IRI Perspective-Taking (r=−.37, p =.19). Table S2 in Supplement 1 shows correlations.
VBM Results
Gray Matter Volume (GMV) Differences Between Groups
Table 1 lists regions where schizophrenia participants showed less GMV than healthy participants. As expected, schizophrenia participants had significantly less VMPFC GMV than healthy participants (Figure 1B). These findings replicate research showing VMPFC GMV reductions in schizophrenia(32-34). Schizophrenia participants also had less GMV in the superior temporal gyrus(STG) and lateral prefrontal cortex(LPFC), which is consistent with prior findings(32-34).
Table 1.
Whole-brain analysis of between-group differences showing regions where schizophrenia participants have less gray matter volume (GMV) as compared to healthy control participants (threshold: p<.05, FWE with 20 voxel (160mm) cluster extent). Clusters within the ventromedial prefrontal cortex (VMPFC) region of interest are labeled as “VMPFC”.
| Anatomical Region | R/L | Brodmann’s Area |
Volume in voxels (mm) |
x | y | za | T value |
|---|---|---|---|---|---|---|---|
| Superior frontal gyrus/Supraorbital sulcus (VMPFC) |
L | 11 | 70 (560) | −4 | 54 | −12 | 7.85 |
| Inferior frontal gyrus - pars orbitalis | L | 47 | 86 (688) | −54 | 38 | −4 | 7.79 |
| Precentral gyrus | R | 4 | 46 (368) | 38 | −28 | 66 | 7.72 |
| Cerebellum | L | n/a | 46 (368) | −8 | −78 | −22 | 7.33 |
| Middle temporal gyrus | L | 21 | 70 (560) | −66 | −24 | −12 | 7.26 |
| Inferior temporal gyrus; posterior portion | L | 37 | 23 (184) | −54 | −58 | −18 | 7.23 |
| Superior temporal gyrus; anterior portion | R | 22 | 42 (336) | 68 | −4 | 6 | 7.08 |
| Precentral gyrus/rolandic operculum | R | 6 | 23 (184) | 62 | 10 | 12 | 6.99 |
| Superior frontal gyrus - medial portion | R | 32, 9 | 24 (192) | 4 | 50 | 32 | 6.95 |
| Anterior cingulate cortex (ACC) (VMPFC) | L | 10 | 20 (160) | −4 | 52 | 8 | 6.73 |
| Superior frontal gyrus - medial portion (VMPFC) | L | 32, 10 | 22 (176) | −2 | 56 | 22 | 6.66 |
Peak voxel x, y, z coordinates are in Montreal Neurological Institute (MNI) template space.
Relationship between ToM Skills and GMV
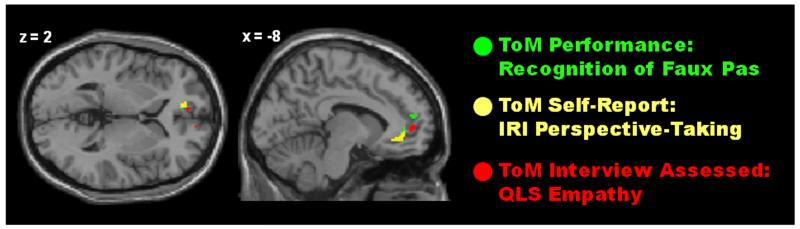
Among schizophrenia participants, three separate multiple regressions were conducted to investigate the relationship between our three ToM measures [Faux Pas Score; IRI Perspective-Taking; QLS-Empathy] and GMV. All three ToM measures were significantly associated with VMPFC GMV, such that better ToM skills were associated with higher GMV (Table 2, Figure 2). When controlling for Global-Cognition, self-reported IRI Perspective-Taking and interview-rated QLS Empathy were still significantly related to VMPFC GMV, but the relationship between FP task performance and VMPFC GMV was reduced just below statistical threshold (from p<.001 to p<.005) (Table 2, Table S4 in Supplement 1). The relationship between all three ToM measures and VMPFC GMV remained significant when controlling for age, medication, and illness duration (Tables S7-S9 in Supplement 1).
Table 2.
Regions across the whole brain showing a relationship between Theory of Mind (ToM) and gray matter volume (GMV) among schizophrenia participants. Clusters designated as “VMPFC” are within the ventromedial prefrontal cortex (VMPFC) region of interest. Small volume corrections (SVC) for multiple comparisons were applied to all clusters in the VMPFC and superior temporal cortex (STC). Symbols designate results after correcting for multiple comparisons and after controlling for global cognition.
| Anatomical Region | R/L | BA | Volume in voxels (mm) |
x | y | z a | T value |
|---|---|---|---|---|---|---|---|
| ToM Performance: Recognition of Faux Pas Test and GMV among schizophrenia participants | |||||||
|
| |||||||
| Superior frontal gyrus (a portion is within VMPFC) | R | 32, 9 | 43 (344) | 18 | 46 | 22 | 5.31 |
| Superior temporal gyrus* | R | 22 | 16 (128) | 66 | −34 | 14 | 5.20 |
| Superior temporal sulcus | L | 22 | 19 (152) | −52 | −8 | −12 | 4.86 |
| Middle cingulate/Supplementary motor cortex | R | 4, 23 | 15 (120) | 12 | −26 | 50 | 4.41 |
| Superior frontal gyrus; anterior, dorsal portion | R | 9 | 15 (120) | 16 | 44 | 48 | 4.36 |
| Superior parietal gyrus | R | 7 | 6 (48) | 30 | −74 | 52 | 4.24 |
| Anterior cingulate cortex (VMPFC) ∞ | L | 32, 10 | 3 (24) | −8 | 44 | 2 | 4.14 |
| Middle occipital gyrus | L | 19 | 9 (72) | −28 | −82 | 24 | 4.01 |
| Anterior cingulate/cingulate sulcus (VMPFC) ∞ | L | 32, 10 | 7 (56) | −8 | 52 | 16 | 3.96 |
| Superior frontal gyrus/superior orbital gyrus | L | 11 | 4 (32) | −14 | 56 | −6 | 3.96 |
| Anterior cingulate cortex (VMPFC) | R | 32, 10 | 7 (56) | 12 | 50 | 0 | 3.87 |
|
| |||||||
| ToM Self-report: Interpersonal Reactivity Index (IRI) Perspective-Taking and GMV among schizophrenia participants | |||||||
|
| |||||||
| Hippocampus | R | 20 | 87 (696) | 40 | −16 | −18 | 5.99 |
| Anterior cingulate cortex (VMPFC) * Ω Φ | L | 10 | 100 (800) | −10 | 44 | −2 | 5.46 |
| Supplementary motor area | L | 6 | 24 (192) | −16 | −12 | 62 | 5.05 |
| Superior temporal gyrus/Heschl’s gyrus | L | 48 | 12 (96) | −36 | −28 | 8 | 4.98 |
| Rolandic operculum/Insula (SRC) | L | 48 | 50 (400) | −40 | −14 | 20 | 4.97 |
| Middle occipital gyrus; posterior portion | R | 18 | 14 (112) | 26 | −98 | 2 | 4.65 |
| Precuneus | L | 31 | 14 (112) | −22 | −48 | 40 | 4.52 |
| Rolandic operculum/Insula (SRC) | R | 48 | 11 (88) | 40 | −14 | 18 | 4.36 |
| Middle frontal gyrus; anterior | L | 46 | 5 (40) | −32 | 42 | 20 | 4.23 |
| Middle occipital gyrus; posterior portion | R | 18 | 7 (56) | 34 | −84 | 4 | 4.2 |
| Posterior cingulate cortex | R | 17 | 5 (40) | 22 | −60 | 10 | 3.84 |
|
| |||||||
| ToM Interview-rated: Quality of Life Scale (QLS)-Empathy and GMV among schizophrenia participants | |||||||
|
| |||||||
| Superior frontal gyrus | R | 9 | 16 (128) | 18 | 60 | 36 | 6.42 |
| Middle frontal gyrus; anterior portion | R | 46 | 38 (304) | 26 | 52 | 22 | 5.90 |
| Anterior orbital gyrus | R | 11 | 18 (144) | 32 | 58 | −14 | 5.66 |
| Middle cingulate gyrus | R | 32 | 45 (360) | 12 | 14 | 42 | 5.59 |
| Precentral gyrus | L | 6 | 10 (80) | −36 | −18 | 66 | 5.05 |
| Middle cingulate gyrus (VMPFC) Ω | R | 32 | 24 (192) | 8 | 34 | 30 | 4.93 |
| Superior frontal gyrus- medial portion (VMPFC) Ω Φ | L | 10 | 29 (232) | −14 | 56 | 6 | 4.90 |
| Supplementary motor area | L | 6 | 6 (48) | −14 | 10 | 64 | 4.89 |
| Inferior frontal gyrus - triangularis | L | 45 | 8 (64) | −46 | 30 | 16 | 4.85 |
| Posterior insula/Rolandic operculum | R | 48 | 40 (320) | 34 | −28 | 26 | 4.69 |
| Anterior cingulate/cingulate sulcus (VMPFC) * Ω Φ | L | 10 | 23 (184) | −8 | 52 | 4 | 4.58 |
| Anterior insula (SRC) | R | 48 | 42 (336) | 26 | 28 | 0 | 4.54 |
| Posterior insula/Rolandic operculum | L | 48 | 26 (208) | −32 | −30 | 24 | 4.44 |
| Superior frontal gyrus; dorsal/anterior portion | L | 9 | 8 (64) | −22 | 44 | 32 | 4.43 |
| Orbital frontal gyrus; anterior portion | L | 11 | 16 (128) | −8 | 66 | −14 | 4.31 |
| Anterior cingulate/Supraorbital sulcus | R | 10, 11 | 9 (72) | 4 | 46 | −10 | 4.29 |
| Precentral gyrus | L | 6 | 11 (88) | −32 | −12 | 54 | 4.26 |
| Middle frontal gyrus | L | 46 | 7 (56) | −36 | 36 | 34 | 4.07 |
| Anterior cingulate cortex (VMPFC) Ω | R | 32 | 4 (32) | 8 | 44 | 8 | 3.82 |
| Middle frontal gyrus | L | 46 | 6 (48) | −32 | 44 | 24 | 3.78 |
| Superior frontal gyrus/cingulate sulcus (VMPFC) Ω Φ | R | 10 | 2 (16) | 10 | 58 | 4 | 3.70 |
Statistical threshold p<.001 (uncorrected); clusters not within VMPFC region of interest must exceed 5 voxels.
SRC = Somatosensory Related Cortices
Peak voxel x, y, z coordinates are in Montreal Neurological Institute (MNI) template space.
Without controlling for global cognition region is significant at p<.05, family wise error (FWE) with small volume correction using ‘masks’ made from WFU Pickatlas: VMPFC ROI (see Figure 1) and the superior temporal gyrus (anatomically defined)
When controlling for global cognition region is significant at p<.005 (uncorrected); x, y, z coordinates: −8,52,16; t=3.2, p=.003; −8,44,2; t=3.04, p=.004.
When controlling for global cognition, region is significant at p<.001 (uncorrected)
When controlling for global cognition, region is significant at p<.05, FWE with small volume correction
Figure 2.
Overlay of three separate regression analyses showing where Theory of Mind (ToM) skills are significantly related to gray matter volume (GMV) among schizophrenia participants. ToM is assessed by: 1) behavioral performance on the ToM task - The Recognition of Faux Pas Test (FP Score)(green); 2) self-reported ToM skills in daily life as measured by the questionnaire - Interpersonal Reactivity Index (IRI) Perspective-Taking subscale (yellow); and 3) an interview-based rating of the capacity to use ToM skills in the participant’s own interpersonal relationships, measured with the Quality of Life Scale (QLS) – Empathy score (red). The data show that, among schizophrenia participants, better ToM skills are related to more GMV. Data within the bilateral ventromedial prefrontal cortex (VMPFC) are displayed at threshold p<.001. Regressions are not controlling for global cognition.
Healthy participants also showed a relationship between ToM and VMPFC GMV (Table S10 in Supplement 1); however, it was relatively weak. FP Score correlated with VMPFC GMV in 2voxels and the IRI Perspective-Taking correlation was subthreshold(p=.002).
Between-Group Differences in the Relationship between ToM and GMV
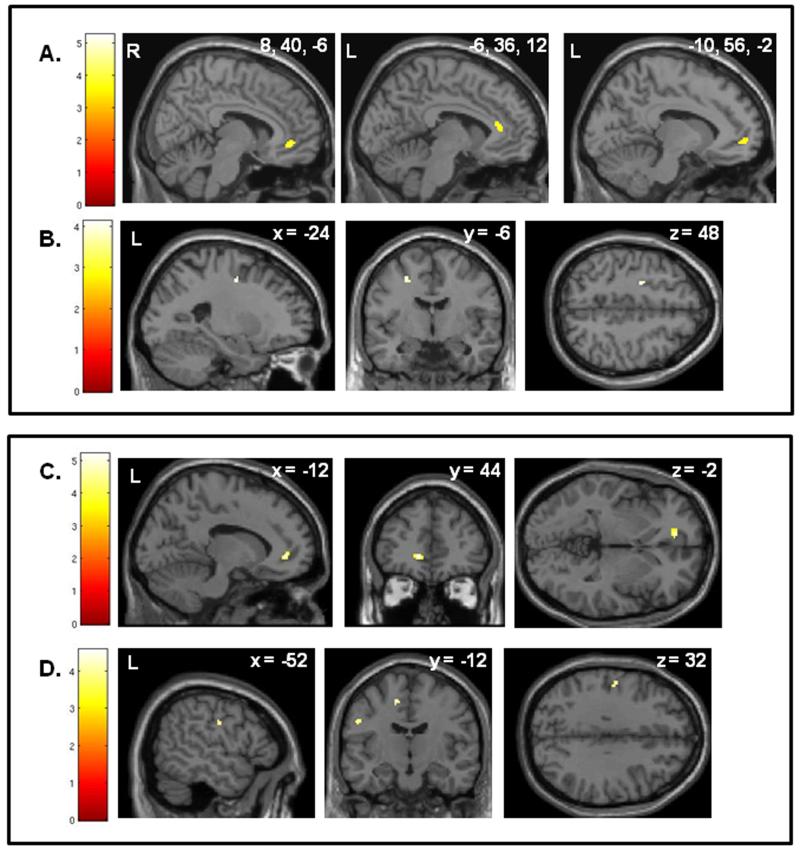
Group*ToM measure interaction analyses showed that the relationship between ToM and VMPFC GMV was stronger for schizophrenia participants than healthy participants (Table S11 in Supplement 1, Figure 3).
Figure 3.
Regions showing a significant interaction between Group (Schizophrenia/Healthy Control) and the relationship between Theory of Mind (ToM) and gray matter volume (GMV). The top panel (A & B) shows results for the performance-based ToM measure, The Recognition of Faux Pas Test, and the bottom panel (C & D) shows results for the self-reported ToM measure, IRI Perspective-Taking. Results for the Faux Pas task: A. Regions where the correlation between Faux Pas Score and GMV is stronger for schizophrenia (SZ) participants than healthy control (HC) participants. The results show that Faux Pas scores are more strongly related to VMPFC GMV (three separate clusters) among SZ participants than among HC participants. MNI x, y, z coordinates for the three separate clusters are: 8, 40, −6; −6, 36, 12; and −10, 56, −2. B. Regions where the correlation between Faux Pas Score and GMV is stronger for HC participants than SZ participants. The correlation between Faux Pas Scores and middle frontal sulcus GMV was stronger for HC than SZ participants. Results for IRI Perspective-Taking: C. Regions where the correlation between IRI Perspective-Taking score and GMV is stronger for schizophrenia (SZ) participants than healthy control (HC) participants. The results show that IRI Perspective-Taking scores are more strongly related to VMPFC GMV among SZ participants than among HC participants. D. Regions where the correlation between IRI Perspective-Taking score and GMV is stronger for HC participants than SZ participants. The correlation between IRI Perspective-Taking scores and postcentral gyrus GMV and was stronger for HC than SZ participants. Data shown at p<.001.
Discussion
Using a multi-method assessment of Theory of Mind (ToM) skills and optimized VBM analysis, we found that among schizophrenia patients, three different measures of advanced ToM skills were significantly related to ventromedial prefrontal cortex (VMPFC) gray matter volume (GMV): 1) behavioral performance in the ability to recognize and understand social faux pas; 2) self-reported tendency to engage in perspective-taking in daily life; and 3) an interview-based rating of the person’s capacity to understand different perspectives and affective states in their own social relationships. In addition, the relationship between ToM and VMPFC GMV was stronger for schizophrenia than healthy participants, suggesting a close link between the VMPFC GM loss characteristic of schizophrenia neuropathology and the ToM deficits associated with risk, manifestation, and severity of schizophrenia disorder. When controlling for global-cognition among schizophrenia participants, the relationship between Faux Pas (FP) task performance and VMPFC GMV was reduced to just under standard significance levels, but the relationship between self-reported IRI Perspective-Taking and interview-rated QLS-Empathy and VMPFC GMV remained strong. These results demonstrate that, in schizophrenia, GM loss in the VMPFC is particularly associated with deficits using ToM skills to enhance social relationships in daily life.
Our finding that global-cognition was positively correlated with ToM task performance, but not with self-report or interview-based ToM measures, suggests that the performance-based MATRICS global-cognition measure shares common ‘test-taking’ features with the FP task, including the ability to sustain attention and/or tolerate explicit performance assessments. This is consistent with results from the MATRICS committee who found higher associations between MATRICS cognitive scores and other performance-based measures as compared to interview-based measures(66). In the current study, the self-report and interview-based ToM measures showed no correlation with global-cognition, and instead demonstrated a strong and significant relationship with VMPFC even when controlling for general cognitive abilities.
These findings suggest that the qualitative ToM assessments used here (i.e. self-reported perspective-taking and interview-rated capacity for empathy) assess a fundamental construct related to VMPFC function. Importantly, both the self-report and interview-based ratings of ToM consider how a person sees themselves in relation to others and how successfully they use that information to enhance their social relationships. These processes require self-reflection and self-monitoring to understand how another person’s situation may be different from one’s own and to respond accordingly. Using the self as a reference for understanding others is a common psychological strategy(67) which may be closely aligned to VMPFC function.
A primary VMPFC function is to monitor internal, affective states and mediate the influence of those states on behavior(68). This facilitates the use of past emotional experience to guide behavior in multiple contexts. VMPFC may support ToM processing by facilitating the use of one’s own experience to understand the experience of others and guide behavior that enhances the social relationship(69). In support of this, VMPFC activity is associated with autobiographical memory retrieval(70), enhanced memory for self-relevant and self-generated words(25), and evaluation of similarity between self and others(71-72). Compared to healthy participants, schizophrenia participants have less VMPFC activity and worse memory for self-relevant and self-generated words(73-75). Among schizophrenia participants, less VMPFC GM is related to worse self-insight(76-77) and deficits understanding the emotions of others(65, 78). Taken together, the data indicate that, in schizophrenia, VMPFC structural and functional abnormalities are related to deficits monitoring and using information relevant to the self in the service of understanding others.
Our results also showed a relationship between ToM skills and GMV in other brain regions involved in ToM processing. Superior temporal cortex (STC), specifically superior temporal gyrus (STG), GMV was related to performance-based and self-reported ToM skills. STC is robustly related to ToM processing(21, 24). Initial data further indicates that STC activity during affective mentalizing is related to self-reported perspective-taking(79). STG GMV loss is a core feature of schizophrenia pathology(32, 34); reductions precede psychosis and continue throughout the early course of illness(80-81). FMRI research shows that STG GMV deficits in schizophrenia contribute to poor performance and abnormal activity (hypo-activity and hyper-activity) during ToM tasks(36). Thus, STG abnormalities may contribute to social dysfunction in schizophrenia and need further investigation. Self-reported and interview-based ToM showed a relationship with GMV in the insula and somatosensory-related cortex (SRC). These regions are involved in the experience, expression, and recognition of emotion(82-83). The current findings are consistent with research showing that SRC activity during affective mentalizing is related to self-reported empathy measured with the IRI(26). In addition, all three ToM measures showed a relationship with GMV in the dorsal and lateral (DL)PFC (BA 8, 9, 46). Schizophrenia is associated with DLPFC functional and structural abnormalities and related cognitive deficits(84). Although DLPFC is not identified as specific or necessary for ToM processing, DLPFC deficits in schizophrenia may contribute to difficulties using DLPFC-mediated cognitive skills, such as attention and memory, in the service of ToM reasoning. Consistent with this, DLPFC and VLPFC GM loss among schizophrenia participants is related to deficits identifying mental states (Mind in the Eyes task)(85) and detecting faux pas(86).
Overall, the current results show a robust relationship between GMV, particularly VMPFC GMV, and ToM skills. However, the direction of causation is not determined. Although evidence clearly shows that social deficits develop after VMPFC lesions(68), animal models also demonstrate that prolonged social isolation is related to progressive VMPFC GM loss(87). Therefore, VMPFC GM loss associated with schizophrenia neuropathology could cause poor ToM skills; but conversely, the social isolation experienced during progressive psychosis, and the loss of opportunities to employ perspective-taking, empathy, and other ToM skills, could cause VMPFC GM loss over time.
Ultimately, these issues have important implications for treatment development, since they suggest that the targeted practice of ToM skills could restore VMPFC function and possibly mitigate the progressive GM loss associated with illness. It is now abundantly clear that, in addition to targeting general cognitive abilities in schizophrenia, specific treatment interventions that focus on social cognition are necessary. As our data indicate, a focus on ecologically valid interpersonal cognitions and skills, such as perspective-taking, may be a high-yield approach that benefits patients behaviorally and addresses underlying compromises in VMPFC structure and function.
Although results for healthy participants are reported, the ability to interpret these ToM-GMV findings is limited. The ToM measures used here are particularly relevant for understanding ToM processing in schizophrenia, but less informative for understanding ToM in healthy adults (e.g. recognizing faux pas was too easy for them). Unfortunately, there are few behavioral tasks that are difficult enough to adequately measure high-end ToM skills in healthy individuals. This is a major challenge for the field and indicates the need for additional task development. Another study limitation is the small and heterogeneous schizophrenia sample; the group was predominantly male and included both schizophrenia and schizoaffective participants. Future research could investigate the influence of gender and mood on GMV-ToM relationships.
Supplementary Material
Acknowledgments
This work was supported by a NARSAD Young Investigator Award (C.I.H) and NIMH grants MH71746 (C.I.H.) and MH68725-02 (S.V.). The authors would like to thank Sara Verosky, Asako Miyakawa and Ori Elis for help with data collection and Mark D’Esposito and Robert T. Knight for neuroimaging support and guidance.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial Disclosures: Sophia Vinogradov is a paid consultant on an NIMH BRDG-SPAN grant to Brain Plasticity Inc. Christine Hooker, Melissa Fisher, Lori Bruce, and Sarah Hope Lincoln report no biomedical financial interests or potential conflicts of interest.
References
- 1.Green MF. Cognition, drug treatment, and functional outcome in schizophrenia: a tale of two transitions. The American journal of psychiatry. 2007;164:992–994. doi: 10.1176/ajp.2007.164.7.992. [DOI] [PubMed] [Google Scholar]
- 2.Swartz MS, Perkins DO, Stroup TS, Davis SM, Capuano G, Rosenheck RA, et al. Effects of antipsychotic medications on psychosocial functioning in patients with chronic schizophrenia: findings from the NIMH CATIE study. The American journal of psychiatry. 2007;164:428–436. doi: 10.1176/ajp.2007.164.3.428. [DOI] [PubMed] [Google Scholar]
- 3.Bora E, Yucel M, Pantelis C. Theory of mind impairment in schizophrenia: meta-analysis. Schizophr Res. 2009;109:1–9. doi: 10.1016/j.schres.2008.12.020. [DOI] [PubMed] [Google Scholar]
- 4.Bertrand MC, Sutton H, Achim AM, Malla AK, Lepage M. Social cognitive impairments in first episode psychosis. Schizophr Res. 2007;95:124–133. doi: 10.1016/j.schres.2007.05.033. [DOI] [PubMed] [Google Scholar]
- 5.Bonshtein U, Leiser D, Levine J. Naive theory impairment in schizophrenia: is it domain-specific? The Journal of nervous and mental disease. 2006;194:753–759. doi: 10.1097/01.nmd.0000243083.75008.ae. [DOI] [PubMed] [Google Scholar]
- 6.Brune M, Abdel-Hamid M, Lehmkamper C, Sonntag C. Mental state attribution, neurocognitive functioning, and psychopathology: what predicts poor social competence in schizophrenia best? Schizophr Res. 2007;92:151–159. doi: 10.1016/j.schres.2007.01.006. [DOI] [PubMed] [Google Scholar]
- 7.Corcoran R, Mercer G, Frith CD. Schizophrenia, symptomatology and social inference: investigating “theory of mind” in people with schizophrenia. Schizophr Res. 1995;17:5–13. doi: 10.1016/0920-9964(95)00024-g. [DOI] [PubMed] [Google Scholar]
- 8.Mo S, Su Y, Chan RC, Liu J. Comprehension of metaphor and irony in schizophrenia during remission: the role of theory of mind and IQ. Psychiatry research. 2008;157:21–29. doi: 10.1016/j.psychres.2006.04.002. [DOI] [PubMed] [Google Scholar]
- 9.Shur S, Shamay-Tsoory SG, Levkovitz Y. Integration of emotional and cognitive aspects of theory of mind in schizophrenia and its relation to prefrontal neurocognitive performance. Cogn Neuropsychiatry. 2008;13:472–490. doi: 10.1080/13546800802490034. [DOI] [PubMed] [Google Scholar]
- 10.Tsoi DT, Lee KH, Gee KA, Holden KL, Parks RW, Woodruff PW. Humour experience in schizophrenia: relationship with executive dysfunction and psychosocial impairment. Psychological medicine. 2008;38:801–810. doi: 10.1017/S0033291707002528. [DOI] [PubMed] [Google Scholar]
- 11.Zhu CY, Lee TM, Li XS, Jing SC, Wang YG, Wang K. Impairments of social cues recognition and social functioning in Chinese people with schizophrenia. Psychiatry and clinical neurosciences. 2007;61:149–158. doi: 10.1111/j.1440-1819.2007.01630.x. [DOI] [PubMed] [Google Scholar]
- 12.Bora E, Gokcen S, Veznedaroglu B. Empathic abilities in people with schizophrenia. Psychiatry research. 2008;160:23–29. doi: 10.1016/j.psychres.2007.05.017. [DOI] [PubMed] [Google Scholar]
- 13.Montag C, Heinz A, Kunz D, Gallinat J. Self-reported empathic abilities in schizophrenia. Schizophr Res. 2007;92:85–89. doi: 10.1016/j.schres.2007.01.024. [DOI] [PubMed] [Google Scholar]
- 14.Pickup GJ. Theory of mind and its relation to schizotypy. Cogn Neuropsychiatry. 2006;11:177–192. doi: 10.1080/13546800444000236. [DOI] [PubMed] [Google Scholar]
- 15.de Achávala D, Costanzoa EY, Villarreal M, Jáureguia IO, Chiodia A, Castro MN, et al. Emotion processing and theory of mind in schizophrenia patients and their unaffected first-degree relatives. Neuropsychologia. doi: 10.1016/j.neuropsychologia.2009.12.019. in press. [DOI] [PubMed] [Google Scholar]
- 16.Riveros R, Hurtado E, Escobar M, Ibanez A. Context-sensitive social cognition is impaired in schizophrenia patients and their healthy relatives. Schizophrenia research. doi: 10.1016/j.schres.2009.10.017. in press. [DOI] [PubMed] [Google Scholar]
- 17.Schiffman J, Lam CW, Jiwatram T, Ekstrom M, Sorensen H, Mednick S. Perspective-taking deficits in people with schizophrenia spectrum disorders: a prospective investigation. Psychological medicine. 2004;34:1581–1586. doi: 10.1017/s0033291704002703. [DOI] [PubMed] [Google Scholar]
- 18.Couture SM, Penn DL, Roberts DL. The Functional Significance of Social Cognition in Schizophrenia: A Review. Schizophrenia bulletin. 2006;32:S44–63. doi: 10.1093/schbul/sbl029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pijnenborg GH, Withaar FK, Evans JJ, van den Bosch RJ, Timmerman ME, Brouwer WH. The predictive value of measures of social cognition for community functioning in schizophrenia: implications for neuropsychological assessment. J Int Neuropsychol Soc. 2009;15:239–247. doi: 10.1017/S1355617709090341. [DOI] [PubMed] [Google Scholar]
- 20.Roncone R, Falloon IR, Mazza M, De Risio A, Pollice R, Necozione S, et al. Is theory of mind in schizophrenia more strongly associated with clinical and social functioning than with neurocognitive deficits? Psychopathology. 2002;35:280–288. doi: 10.1159/000067062. [DOI] [PubMed] [Google Scholar]
- 21.Carrington SJ, Bailey AJ. Are there theory of mind regions in the brain? A review of the neuroimaging literature. Human brain mapping. 2009;30:2313–2335. doi: 10.1002/hbm.20671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Frith CD, Frith U. The neural basis of mentalizing. Neuron. 2006;50:531–534. doi: 10.1016/j.neuron.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 23.Gallagher HL, Frith CD. Functional imaging of ‘theory of mind’. Trends in cognitive sciences. 2003;7:77–83. doi: 10.1016/s1364-6613(02)00025-6. [DOI] [PubMed] [Google Scholar]
- 24.Van Overwalle F, Baetens K. Understanding others’ actions and goals by mirror and mentalizing systems: a meta-analysis. NeuroImage. 2009;48:564–584. doi: 10.1016/j.neuroimage.2009.06.009. [DOI] [PubMed] [Google Scholar]
- 25.Amodio DM, Frith CD. Meeting of minds: the medial frontal cortex and social cognition. Nat Rev Neurosci. 2006;7:268–277. doi: 10.1038/nrn1884. [DOI] [PubMed] [Google Scholar]
- 26.Hooker CI, Verosky SC, Germine LT, Knight RT, D’Esposito M. Mentalizing about emotion and its relationship to empathy. Soc Cogn Affect Neurosci. 2008;3:204–217. doi: 10.1093/scan/nsn019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stone VE, Baron-Cohen S, Knight RT. Frontal lobe contributions to theory of mind. Journal of cognitive neuroscience. 1998;10:640–656. doi: 10.1162/089892998562942. [DOI] [PubMed] [Google Scholar]
- 28.Shamay-Tsoory SG, Aharon-Peretz J, Levkovitz Y. The neuroanatomical basis of affective mentalizing in schizophrenia: Comparison of patients with schizophrenia and patients with localized prefrontal lesions. Schizophr Res. 2007;90:274–283. doi: 10.1016/j.schres.2006.09.020. [DOI] [PubMed] [Google Scholar]
- 29.Shamay-Tsoory SG, Aharon-Peretz J. Dissociable prefrontal networks for cognitive and affective theory of mind: a lesion study. Neuropsychologia. 2007;45:3054–3067. doi: 10.1016/j.neuropsychologia.2007.05.021. [DOI] [PubMed] [Google Scholar]
- 30.Shamay-Tsoory SG, Tomer R, Berger BD, Aharon-Peretz J. Characterization of empathy deficits following prefrontal brain damage: the role of the right ventromedial prefrontal cortex. Journal of cognitive neuroscience. 2003;15:324–337. doi: 10.1162/089892903321593063. [DOI] [PubMed] [Google Scholar]
- 31.Shamay-Tsoory SG, Tomer R, Berger BD, Goldsher D, Aharon-Peretz J. Impaired “affective theory of mind” is associated with right ventromedial prefrontal damage. Cogn Behav Neurol. 2005;18:55–67. doi: 10.1097/01.wnn.0000152228.90129.99. [DOI] [PubMed] [Google Scholar]
- 32.Honea R, Crow TJ, Passingham D, Mackay CE. Regional deficits in brain volume in schizophrenia: a meta-analysis of voxel-based morphometry studies. The American journal of psychiatry. 2005;162:2233–2245. doi: 10.1176/appi.ajp.162.12.2233. [DOI] [PubMed] [Google Scholar]
- 33.Pomarol-Clotet E, Canales-Rodriguez EJ, Salvador R, Sarro S, Gomar JJ, Vila F, et al. Medial prefrontal cortex pathology in schizophrenia as revealed by convergent findings from multimodal imaging. Molecular psychiatry. doi: 10.1038/mp.2009.146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Williams LM. Voxel-based morphometry in schizophrenia: implications for neurodevelopmental connectivity models, cognition and affect. Expert review of neurotherapeutics. 2008;8:1049–1065. doi: 10.1586/14737175.8.7.1049. [DOI] [PubMed] [Google Scholar]
- 35.Brunet E, Sarfati Y, Hardy-Bayle MC, Decety J. Abnormalities of brain function during a nonverbal theory of mind task in schizophrenia. Neuropsychologia. 2003;41:1574–1582. doi: 10.1016/s0028-3932(03)00119-2. [DOI] [PubMed] [Google Scholar]
- 36.Benedetti F, Bernasconi A, Bosia M, Cavallaro R, Dallaspezia S, Falini A, et al. Functional and structural brain correlates of theory of mind and empathy deficits in schizophrenia. Schizophr Res. 2009;114:154–160. doi: 10.1016/j.schres.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 37.Marjoram D, Job DE, Whalley HC, Gountouna VE, McIntosh AM, Simonotto E, et al. A visual joke fMRI investigation into Theory of Mind and enhanced risk of schizophrenia. NeuroImage. 2006;31:1850–1858. doi: 10.1016/j.neuroimage.2006.02.011. [DOI] [PubMed] [Google Scholar]
- 38.Callicott JH, Bertolino A, Mattay VS, Langheim FJ, Duyn J, Coppola R, et al. Physiological dysfunction of the dorsolateral prefrontal cortex in schizophrenia revisited. Cereb Cortex. 2000;10:1078–1092. doi: 10.1093/cercor/10.11.1078. [DOI] [PubMed] [Google Scholar]
- 39.Callicott JH, Mattay VS, Verchinski BA, Marenco S, Egan MF, Weinberger DR. Complexity of prefrontal cortical dysfunction in schizophrenia: more than up or down. The American journal of psychiatry. 2003;160:2209–2215. doi: 10.1176/appi.ajp.160.12.2209. [DOI] [PubMed] [Google Scholar]
- 40.Pickup GJ. Relationship between Theory of Mind and executive function in schizophrenia: a systematic review. Psychopathology. 2008;41:206–213. doi: 10.1159/000125554. [DOI] [PubMed] [Google Scholar]
- 41.Ba MB, Zanello A, Varnier M, Koellner V, Merlo MC. Deficits in neurocognition, theory of mind, and social functioning in patients with schizophrenic disorders: are they related? The Journal of nervous and mental disease. 2008;196:153–156. doi: 10.1097/NMD.0b013e318162aa08. [DOI] [PubMed] [Google Scholar]
- 42.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version. Biometrics Research, New York State Psychiatric Institute; New York: 2002. Patient Edition. (SCID- I/P) [Google Scholar]
- 43.Kay SR, Opler LA, Fiszbein A. The positive and negative syndrome rating scale (PANSS) for schizophrenia. Schizophrenia bulletin. 1987;45:20–31. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- 44.Poole JH, Tobias FC, Vinogradov S. The functional relevance of affect recognition errors in schizophrenia. J Int Neuropsychol Soc. 2000;6:649–658. doi: 10.1017/s135561770066602x. [DOI] [PubMed] [Google Scholar]
- 45.Bilker WB, Brensinger C, Kurtz MM, Kohler C, Gur RC, Siegel SJ, et al. Development of an abbreviated schizophrenia quality of life scale using a new method. Neuropsychopharmacology. 2003;28:773–777. doi: 10.1038/sj.npp.1300093. [DOI] [PubMed] [Google Scholar]
- 46.Wechsler D. Wechsler Abbreviated Scale of Intelligence. The Psychological Corporation; San Antonio, TX: 1999. [Google Scholar]
- 47.Raine A. The SPQ: a scale for the assessment of schizotypal personality based on DSM-III-R criteria. Schizophrenia bulletin. 1991;17:555–564. doi: 10.1093/schbul/17.4.555. [DOI] [PubMed] [Google Scholar]
- 48.Baron-Cohen S, O’Riordan M, Stone V, Jones R, Plaisted K. Recognition of faux pas by normally developing children and children with Asperger syndrome or high-functioning autism. Journal of autism and developmental disorders. 1999;29:407–418. doi: 10.1023/a:1023035012436. [DOI] [PubMed] [Google Scholar]
- 49.Davis MH. Measuring individual differences in empathy: Evidence for a multidimensional approach. Journal of personality and social psychology. 1983;44:113–126. [Google Scholar]
- 50.Davis MH. Empathy: a social psychological approach. Westview Press; Boulder, CO: 1996. [Google Scholar]
- 51.Shamay-Tsoory SG, Tomer R, Goldsher D, Berger BD, Aharon-Peretz J. Impairment in cognitive and affective empathy in patients with brain lesions: anatomical and cognitive correlates. J Clin Exp Neuropsychol. 2004;26:1113–1127. doi: 10.1080/13803390490515531. [DOI] [PubMed] [Google Scholar]
- 52.Shamay-Tsoory SG, Shur S, Harari H, Levkovitz Y. Neurocognitive basis of impaired empathy in schizophrenia. Neuropsychology. 2007;21:431–438. doi: 10.1037/0894-4105.21.4.431. [DOI] [PubMed] [Google Scholar]
- 53.Heinrichs DW, Hanlon TE, Carpenter WT., Jr. The Quality of Life Scale: an instrument for rating the schizophrenic deficit syndrome. Schizophrenia bulletin. 1984;10:388–398. doi: 10.1093/schbul/10.3.388. [DOI] [PubMed] [Google Scholar]
- 54.Nuechterlein KH, Green MF, Kern RS, Baade LE, Barch DM, Cohen JD, et al. The MATRICS Consensus Cognitive Battery, Part 1: Test Selection, Reliability, and Validity. The American journal of psychiatry. 2008;165:203–213. doi: 10.1176/appi.ajp.2007.07010042. [DOI] [PubMed] [Google Scholar]
- 55.Ashburner J, Friston KJ. Voxel-based morphometry--the methods. NeuroImage. 2000;11:805–821. doi: 10.1006/nimg.2000.0582. [DOI] [PubMed] [Google Scholar]
- 56.Good CD, Johnsrude IS, Ashburner J, Henson RN, Friston KJ, Frackowiak RS. A voxel-based morphometric study of ageing in 465 normal adult human brains. NeuroImage. 2001;14:21–36. doi: 10.1006/nimg.2001.0786. [DOI] [PubMed] [Google Scholar]
- 57.Mechelli A, Price CJ, Friston KJ, Ashburner J. Voxel-Based Morphometry of the Human Brain: Methods and Applications. Current Medical Imaging Reviews. 2005:1. [Google Scholar]
- 58.White T, O’Leary D, Magnotta V, Arndt S, Flaum M, Andreasen NC. Anatomic and functional variability: the effects of filter size in group fMRI data analysis. NeuroImage. 2001;13:577–588. doi: 10.1006/nimg.2000.0716. [DOI] [PubMed] [Google Scholar]
- 59.Friston K, Holmes AP, Worsley K, Poline J-B, D FC, Frackowiak RSJ. Statistic parametric maps in functional imaging: A general linear approach. Human brain mapping. 1995;2:189–210. [Google Scholar]
- 60.Friston KJ, Frith CD, Liddle PF, Dolan RJ, Lammertsma AA, Frackowiak RS. The relationship between global and local changes in PET scans. J Cereb Blood Flow Metab. 1990;10:458–466. doi: 10.1038/jcbfm.1990.88. [DOI] [PubMed] [Google Scholar]
- 61.Maldjian JA, Laurienti PJ, Burdette JB, Kraft RA. An Automated Method for Neuroanatomic and Cytoarchitectonic Atlas-based Interrogation of fMRI Data Sets. NeuroImage. 2003;19:1233–1239. doi: 10.1016/s1053-8119(03)00169-1. [DOI] [PubMed] [Google Scholar]
- 62.Maldjian JA, Laurienti PJ, Burdette JH. Precentral gyrus discrepancy in electronic versions of the Talairach Atlas. NeuroImage. 2004;21:450–455. doi: 10.1016/j.neuroimage.2003.09.032. [DOI] [PubMed] [Google Scholar]
- 63.Fornito A, Yucel M, Dean B, Wood SJ, Pantelis C. Anatomical abnormalities of the anterior cingulate cortex in schizophrenia: bridging the gap between neuroimaging and neuropathology. Schizophrenia bulletin. 2009;35:973–993. doi: 10.1093/schbul/sbn025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Fornito A, Yung AR, Wood SJ, Phillips LJ, Nelson B, Cotton S, et al. Anatomic abnormalities of the anterior cingulate cortex before psychosis onset: an MRI study of ultra-high-risk individuals. Biological psychiatry. 2008;64:758–765. doi: 10.1016/j.biopsych.2008.05.032. [DOI] [PubMed] [Google Scholar]
- 65.Fujiwara H, Hirao K, Namiki C, Yamada M, Shimizu M, Fukuyama H, et al. Anterior cingulate pathology and social cognition in schizophrenia: a study of gray matter, white matter and sulcal morphometry. NeuroImage. 2007;36:1236–1245. doi: 10.1016/j.neuroimage.2007.03.068. [DOI] [PubMed] [Google Scholar]
- 66.Green MF, Nuechterlein KH, Kern RS, Baade LE, Fenton WS, Gold JM, et al. Functional Co-Primary Measures for Clinical Trials in Schizophrenia: Results From the MATRICS Psychometric and Standardization Study. The American journal of psychiatry. 2008;165:221–228. doi: 10.1176/appi.ajp.2007.07010089. [DOI] [PubMed] [Google Scholar]
- 67.Gordon RM. Folk psychology as simulation. Mind and Language. 1992:1. [Google Scholar]
- 68.Rudebeck PH, Bannerman DM, Rushworth MF. The contribution of distinct subregions of the ventromedial frontal cortex to emotion, social behavior, and decision making. Cognitive, affective & behavioral neuroscience. 2008;8:485–497. doi: 10.3758/CABN.8.4.485. [DOI] [PubMed] [Google Scholar]
- 69.van der Meer L, Costafreda S, Aleman A, David AS. Self-reflection and the brain: a theoretical review and meta-analysis of neuroimaging studies with implications for schizophrenia. Neuroscience and biobehavioral reviews. 34:935–946. doi: 10.1016/j.neubiorev.2009.12.004. [DOI] [PubMed] [Google Scholar]
- 70.Schacter DL, Addis DR, Buckner RL. Remembering the past to imagine the future: the prospective brain. Nat Rev Neurosci. 2007;8:657–661. doi: 10.1038/nrn2213. [DOI] [PubMed] [Google Scholar]
- 71.Mitchell JP, Banaji MR, Macrae CN. The link between social cognition and self-referential thought in the medial prefrontal cortex. Journal of cognitive neuroscience. 2005;17:1306–1315. doi: 10.1162/0898929055002418. [DOI] [PubMed] [Google Scholar]
- 72.Mitchell JP, Macrae CN, Banaji MR. Dissociable medial prefrontal contributions to judgments of similar and dissimilar others. Neuron. 2006;50:655–663. doi: 10.1016/j.neuron.2006.03.040. [DOI] [PubMed] [Google Scholar]
- 73.Fisher M, McCoy K, Poole JH, Vinogradov S. Self and other in schizophrenia: a cognitive neuroscience perspective. The American journal of psychiatry. 2008;165:1465–1472. doi: 10.1176/appi.ajp.2008.07111806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Harvey PO, Lee J, Horan WP, Ochsner K, Green MF. Do patients with schizophrenia benefit from a self-referential memory bias? Schizophr Res. 2011;127:171–177. doi: 10.1016/j.schres.2010.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Vinogradov S, Luks TL, Schulman BJ, Simpson GV. Deficit in a neural correlate of reality monitoring in schizophrenia patients. Cereb Cortex. 2008;18:2532–2539. doi: 10.1093/cercor/bhn028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Flashman LA, McAllister TW, Johnson SC, Rick JH, Green RL, Saykin AJ. Specific frontal lobe subregions correlated with unawareness of illness in schizophrenia: a preliminary study. The Journal of neuropsychiatry and clinical neurosciences. 2001;13:255–257. doi: 10.1176/jnp.13.2.255. [DOI] [PubMed] [Google Scholar]
- 77.Lee KH, Brown WH, Egleston PN, Green RD, Farrow TF, Hunter MD, et al. A functional magnetic resonance imaging study of social cognition in schizophrenia during an acute episode and after recovery. The American journal of psychiatry. 2006;163:1926–1933. doi: 10.1176/ajp.2006.163.11.1926. [DOI] [PubMed] [Google Scholar]
- 78.Yamada M, Hirao K, Namiki C, Hanakawa T, Fukuyama H, Hayashi T, et al. Social cognition and frontal lobe pathology in schizophrenia: a voxel-based morphometric study. NeuroImage. 2007;35:292–298. doi: 10.1016/j.neuroimage.2006.10.046. [DOI] [PubMed] [Google Scholar]
- 79.Hooker CI, Verosky SC, Germine LT, Knight RT, D’Esposito M. Neural activity during social signal perception correlates with self-reported empathy. Brain Res. 2010;1308:100–113. doi: 10.1016/j.brainres.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Kasai K, Shenton ME, Salisbury DF, Hirayasu Y, Lee CU, Ciszewski AA, et al. Progressive decrease of left superior temporal gyrus gray matter volume in patients with first-episode schizophrenia. The American journal of psychiatry. 2003;160:156–164. doi: 10.1176/appi.ajp.160.1.156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kasai K, Shenton ME, Salisbury DF, Hirayasu Y, Onitsuka T, Spencer MH, et al. Progressive decrease of left Heschl gyrus and planum temporale gray matter volume in first-episode schizophrenia: a longitudinal magnetic resonance imaging study. Archives of general psychiatry. 2003;60:766–775. doi: 10.1001/archpsyc.60.8.766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Adolphs R. The social brain: neural basis of social knowledge. Annu Rev Psychol. 2009;60:693–716. doi: 10.1146/annurev.psych.60.110707.163514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Adolphs R, Damasio H, Tranel D, Cooper G, Damasio AR. A role for somatosensory cortices in the visual recognition of emotion as revealed by three-dimensional lesion mapping. J Neurosci. 2000;20:2683–2690. doi: 10.1523/JNEUROSCI.20-07-02683.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Barch DM. The cognitive neuroscience of schizophrenia. Annual review of clinical psychology. 2005;1:321–353. doi: 10.1146/annurev.clinpsy.1.102803.143959. [DOI] [PubMed] [Google Scholar]
- 85.Hirao K, Miyata J, Fujiwara H, Yamada M, Namiki C, Shimizu M, et al. Theory of mind and frontal lobe pathology in schizophrenia: a voxel-based morphometry study. Schizophr Res. 2008;105:165–174. doi: 10.1016/j.schres.2008.07.021. [DOI] [PubMed] [Google Scholar]
- 86.Herold R, Feldmann A, Simon M, Tenyi T, Kover F, Nagy F, et al. Regional gray matter reduction and theory of mind deficit in the early phase of schizophrenia: a voxel-based morphometric study. Acta psychiatrica Scandinavica. 2009;119:199–208. doi: 10.1111/j.1600-0447.2008.01297.x. [DOI] [PubMed] [Google Scholar]
- 87.Schubert MI, Porkess MV, Dashdorj N, Fone KC, Auer DP. Effects of social isolation rearing on the limbic brain: a combined behavioral and magnetic resonance imaging volumetry study in rats. Neuroscience. 2009;159:21–30. doi: 10.1016/j.neuroscience.2008.12.019. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.